Immunology
Dr Ahmed Abdullah
Lecture 3
1
Immunology of blood transfusion
Objectives:
The main objectives of this lecture are:
1. Blood groups
2. Haemolytic transfusion reactions
3. Febrile non hemolytic transfusion reaction
4. Platelet transfusion reaction
5. Rhesus disease
6. Coombs tests
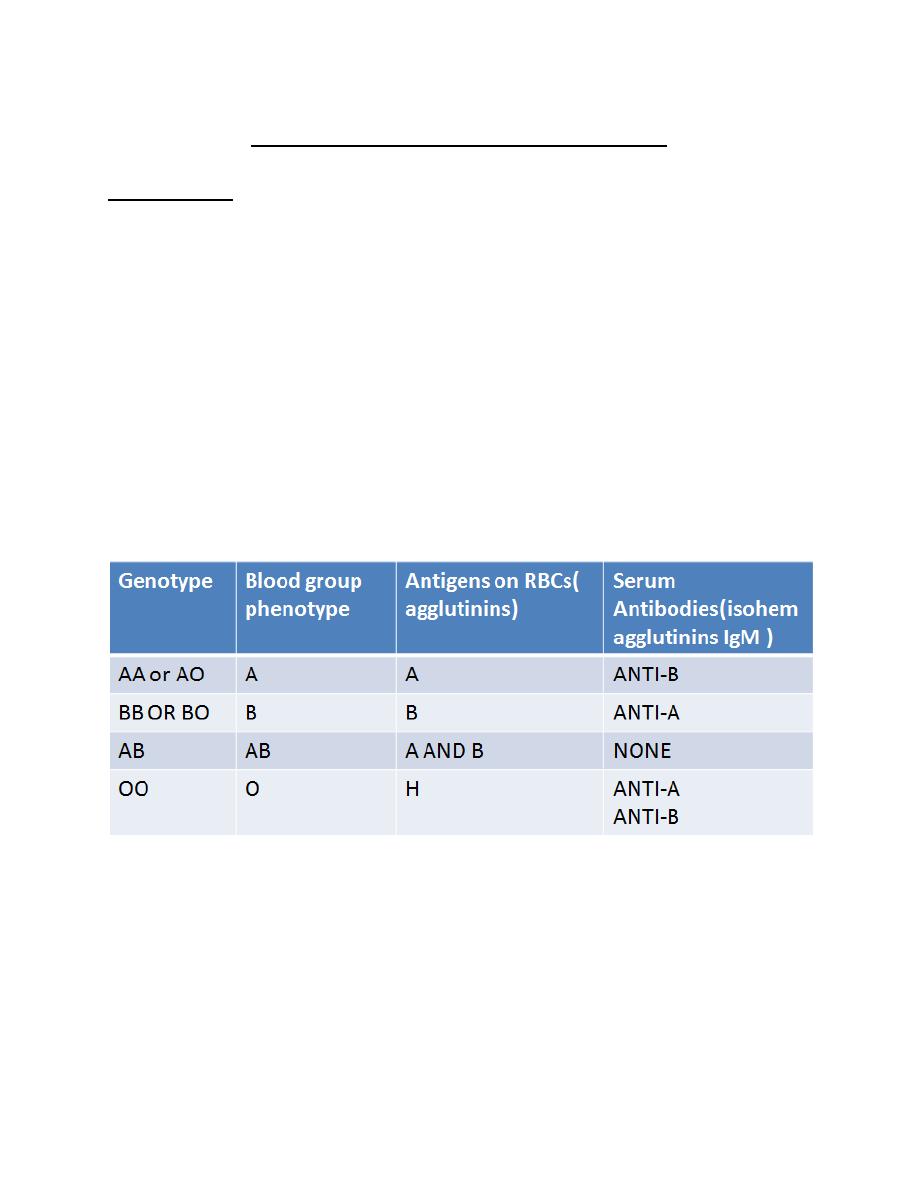
Blood groups:
ABH(ABO) (blood types A, B, AB, and O)
Rhesus (with Rh D-positive or Rh D-negative blood types).
Blood group antigens are either sugars or proteins.
Blood groups and Rh genes were inherited according to mendelian law.
Other blood grouping systems as MNS,Duffy, p1, Lutheran (LU), KELL, Jk
(Kidd blood group) and Lewis blood groups.

Immunology
Dr Ahmed Abdullah
Lecture 3
2
Haemolytic transfusion reaction: RBCs incompatibility
• Haemolytic transfusion reactions are reactions in which donor RBCs are
destroyed by antibodies in the recipient's circulation.
• They occur when Ag. Positive donor RBCs are transfused into a patient who
has performed Abs (isohemagglutinins) to that Ag. (Not matched blood
groups).
• The isohemagglutinins bind to RBCs activating the classical complement
system leading to lysis of RBCs.
Fig 2: Recognition of incompatible RBCs by isohaemagglutinins and activation of complement classical pathway (1).
• The donor RBCs may be destroyed immediately (a potentially serious
reaction) or may have a shortened survival time (milder reactions).
• Red blood cells incompatibility may also occur when antibodies from the
donor’s antibodies attack the patient’s RBC antigens. It is a minor problem
because of the small amount of antibody presents in the donated plasma,
which is further diluted on transfusion into the recipient's circulation.
*Acute haemolytic transfusion reaction
• It occurs within 24 hours of the transfusion and in most of cases occurs
during the transfusion.
Immunology
Dr Ahmed Abdullah
Lecture 3
3
Two types of Haemolysis occur in this reaction:
Acute intra vascular haemolysis:
• The most severe reaction
• The donor RBCs are destroyed by the recipient's antibodies while they are
still inside blood vessels.
• Strong activation of complement system, which lyses the donor RBCs.
• Anti-A and anti-B antibodies anti-Rh, ((other blood groups as Jk (Kidd blood
group) , P1blood group can induce intravascular haemolysis.
Acute extra vascular haemolytic reaction:
• The donor RBCs are removed from the circulation by macrophages in the
spleen and liver.
• Antibodies directed at antigens of the Rh blood group, ABO, Duffy, and
Kidd blood groups mediate this type of RBC removal.
• Less severe than the intravascular reaction
*Delayed haemolytic transfusion reaction
• Occurs as soon as one day or as late as 14 days after a blood transfusion.
• It occurs with estimates of approximately 1:2500 of transfusions but is
found more frequently in sickle cell patients who have received frequent
blood transfusions.
• The donor RBCs are destroyed by the recipient's antibodies, but the
haemolysis is "delayed" because the antibodies are only present in low
amounts initially.
• Usually, this type of reaction is extravascular much less severe than acute
haemolytic reactions.

Immunology
Dr Ahmed Abdullah
Lecture 3
4
• This type of transfusion reaction is associated with antibodies that target
the Kidd, Duffy, Kell and MNS antigens.
Febrile non-haemolytic transfusion reaction (FNHTR):
• The most common transfusion reaction is a fever without signs of
haemolysis.
• This is called febrile non-haemolytic transfusion reaction (FNHTR).
• Most cases are mild; the patients may describe feeling hot and cold, their
temperatures rise by at least 1°C, and they may have rigors.
• FNHTR is only diagnosed when other potentially dangerous causes of
transfusion reactions are excluded.
• The cause is thought to be the patient's preformed antibodies attacking
transfused WBCs, binding to their HLA antigens.
• Another factor might be that during the storage of blood units, WBCs and
platelets release cytokines that may provoke a fever when the unit of blood
is transfused into a patient.
• Patients who receive multiple transfusions may be given an anti-pyretics
before the transfusion to lessen fever symptoms or WBC may be removed
from the given blood.
Immunological complications of platelets transfusion
The serious risks of platelet transfusion include viral transmission, bacterial
sepsis, and acute lung injury.
Less serious adverse effects include allergic and non-hemolytic febrile
reactions.
Rare hemolytic reactions have occurred due to a common policy of
platelets transfusion without regard to ABO type.

Immunology
Dr Ahmed Abdullah
Lecture 3
5
Platelet-derived lipids are implicated in transfusion-related acute lung
injury after transfusion.
The platelets are regarded as immune cells releasing IL-6, IL-27 and sCD40L,
which are closely linked to febrile reactions.
Platelet transfusions are pro-inflammatory, and may be pro-thrombotic.
Post transfusion purpura (PTP) is a thrombocytopenia (low number of
platelets) that occurs 5 to 10 days after a platelets transfusion:
• Patients are at risk of bleeding, and bleeding into the skin causes a purplish
discoloration of the skin known as purpura.
• The platelet antigen HPA-1a appears to be most frequently targeted Ag.
Blood type and cross match
• To avoid a transfusion reaction, donated blood must be compatible with
the blood of the recipient.
• Before blood transfusion, two blood tests known as a "type and cross
match" should be done.
• First, the recipient's blood type is determined, i.e., their ABO type and Rh D
status.
• In theory, once the recipient's blood type is known, a transfusion of
Compatible blood can be given. However, donor blood may still be
incompatible because it contains other antigens that are not routinely
typed but may still cause a problem if the recipient's serum contains
antibodies that will target them. Therefore, a "cross match" is done to
ensure that the donor RBCs actually do match against the recipient's serum.
Immunology
Dr Ahmed Abdullah
Lecture 3
6
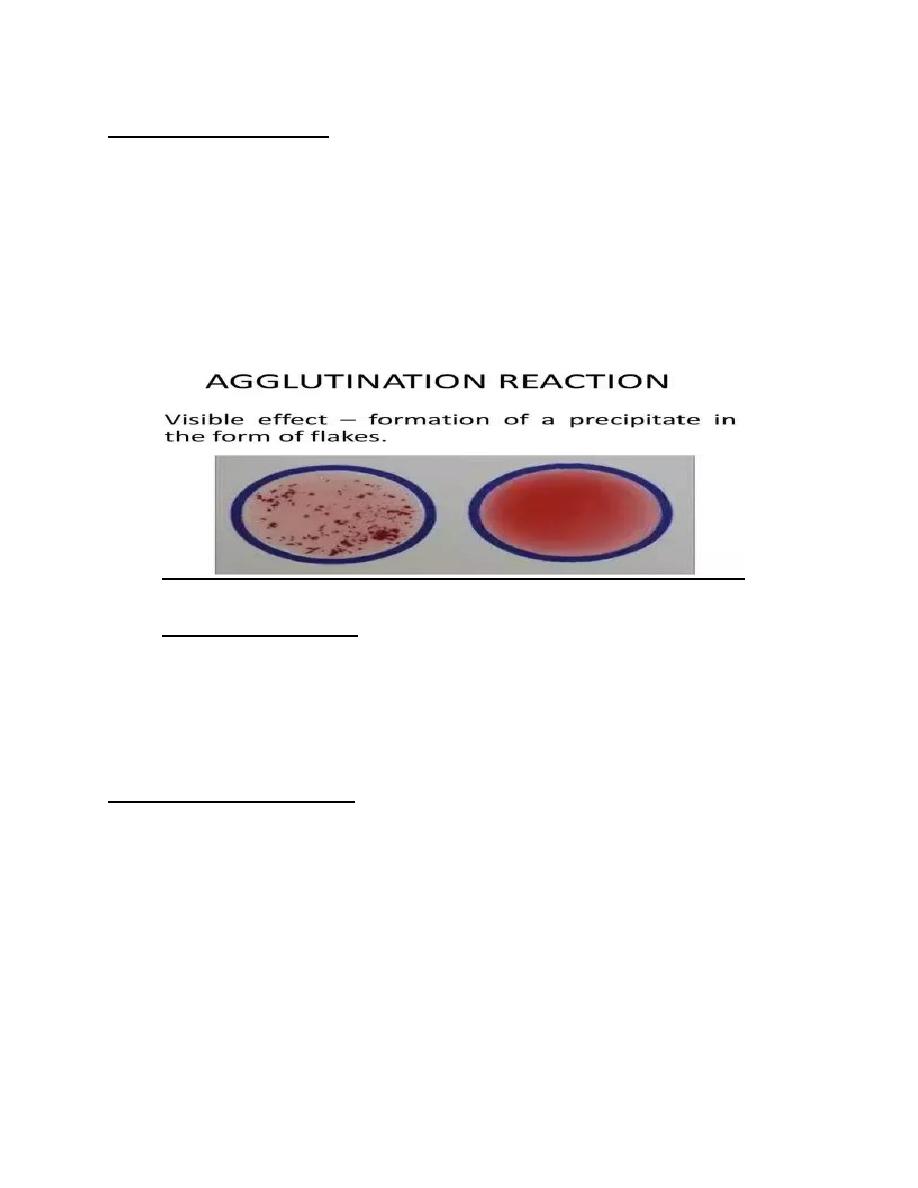
Procedure of cross match:
To perform a cross match:
• Recipient's serum is mixed with donor RBCs.
• The mixture is then examined under a microscope.
• If the proposed transfusion is incompatible, the donor RBCs are
agglutinated by antibodies in the recipient's serum.
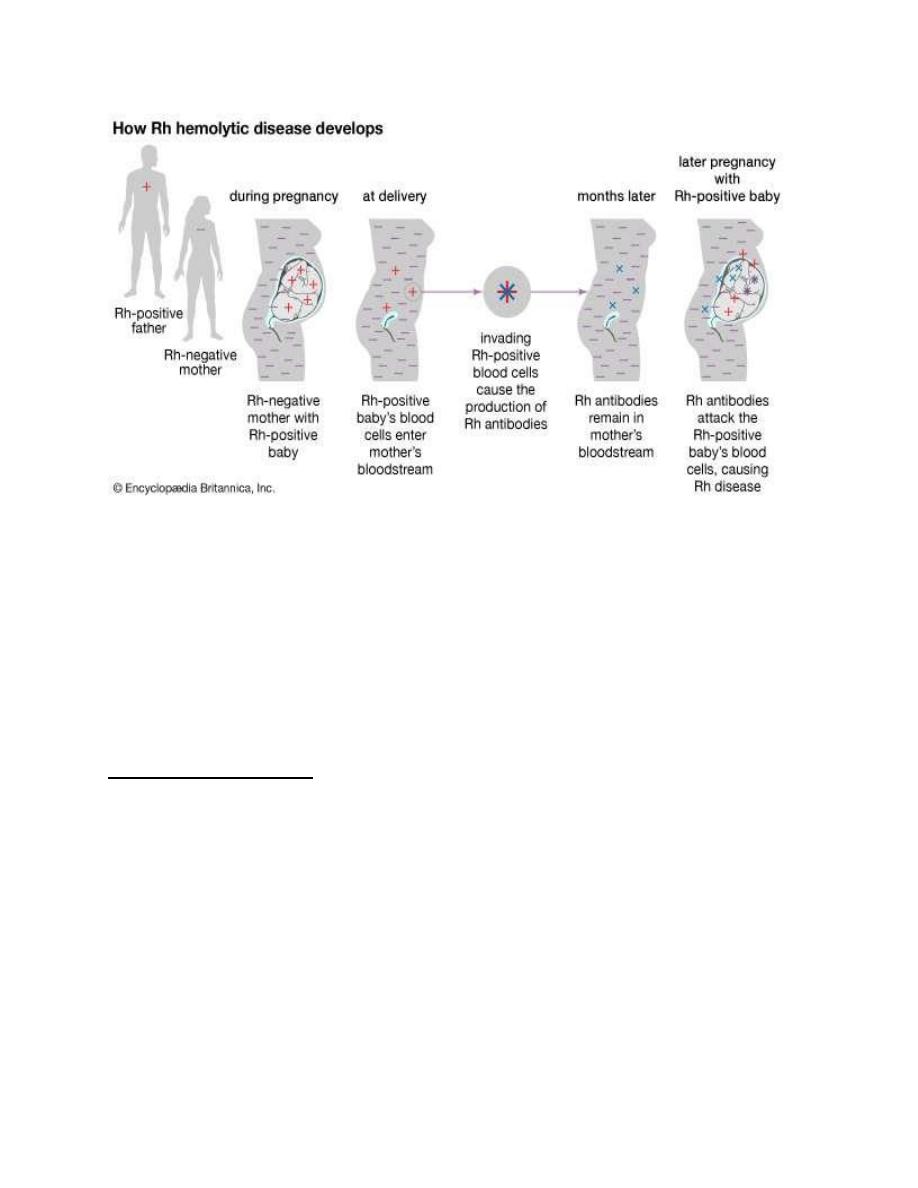
Rhesus disease:
• Rhesus disease is a condition where antibodies in a pregnant woman's
blood destroy her baby's blood cells.
• It is also known as haemolytic disease of the fetus and newborn (HDFN).
What causes rhesus disease?
Immunology
Dr Ahmed Abdullah
Lecture 3
7
Rhesus disease
(2)
Preventing rhesus disease
• Rhesus disease can be prevented by injection of non sensetized Rh negative
mother with anti-D immunoglobulins.
• This can help to avoid the process of sensitization of mother immune
system to Rh
+
RBCs.
Anti-D immunoglobulin:
• The anti-D immunoglobulin neutralizes any RhD positive antigens that may
have entered the mother’s blood during pregnancy.
If the antigens have been neutralized, the mother’s blood won't produce
antibodies.
• Anti-D immunoglobulin is administered routinely during the third trimester
of pregnancy if mother’s blood type is RhD negative.
• This is because it's likely that small amounts of blood from baby will pass
into maternal blood during this time.
Immunology
Dr Ahmed Abdullah
Lecture 3
8
• This routine administration of anti-D immunoglobulin is called routine
antenatal anti-D prophylaxis, or RAADP.
There are currently two protocols for RAADP:
One-dose treatment: between weeks 28 to 30 of pregnancy
Two-dose treatment: Mother receives two injections; 1
st
at 28th week and
the other during the 34th week of pregnancy.
RAADP is recommended for all pregnant RhD negative women who are not
sensitized to the RhD antigen, even if previously had an injection of anti-D
immunoglobulin because RAADP does not offer lifelong immunity.
RAADP won't work if mother is already sensitized.
Anti-D immunoglobulin after birth:
• If mother is RhD negative and baby is RhD positive, and the mother isn’t
already been sensitized, she should receive an injection of anti-D
immunoglobulin within 72 hours of giving birth.
• The injection will neutralize any RhD positive blood cells that may have
crossed over into maternal blood stream during the delivery.
• This means maternal blood won't have a chance to produce antibodies and
will significantly decrease the risk of next baby having rhesus disease.
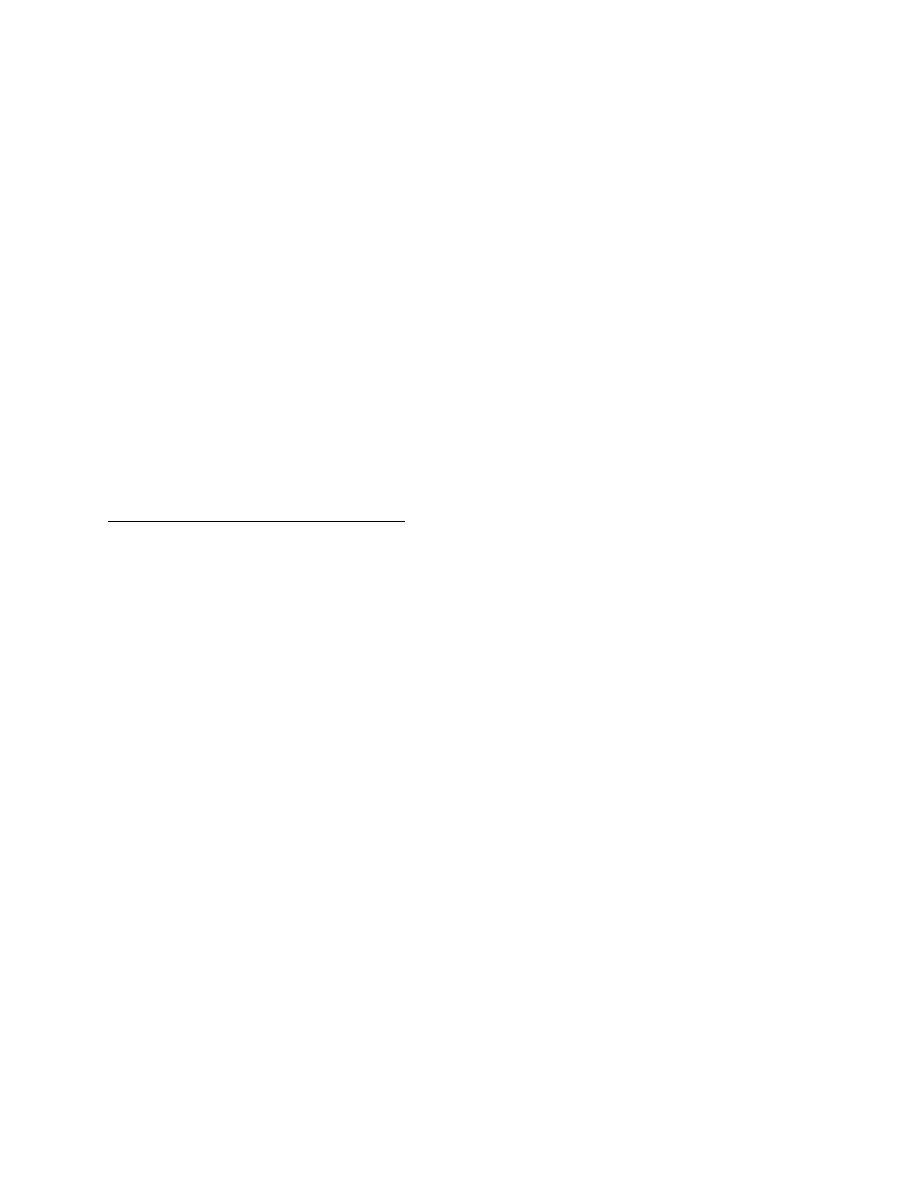
Direct coombs test:
• This test is used to detect whether the fetus has hemolytic condition due to
Rhesus disease or not.
• Fetal sample of RBCs from affected infant to which maternal anti-D
Abs(IgG) are bound + externally added anti-IgG antibodies leads to
agglutination means positive result.
Immunology
Dr Ahmed Abdullah
Lecture 3
9
(3)
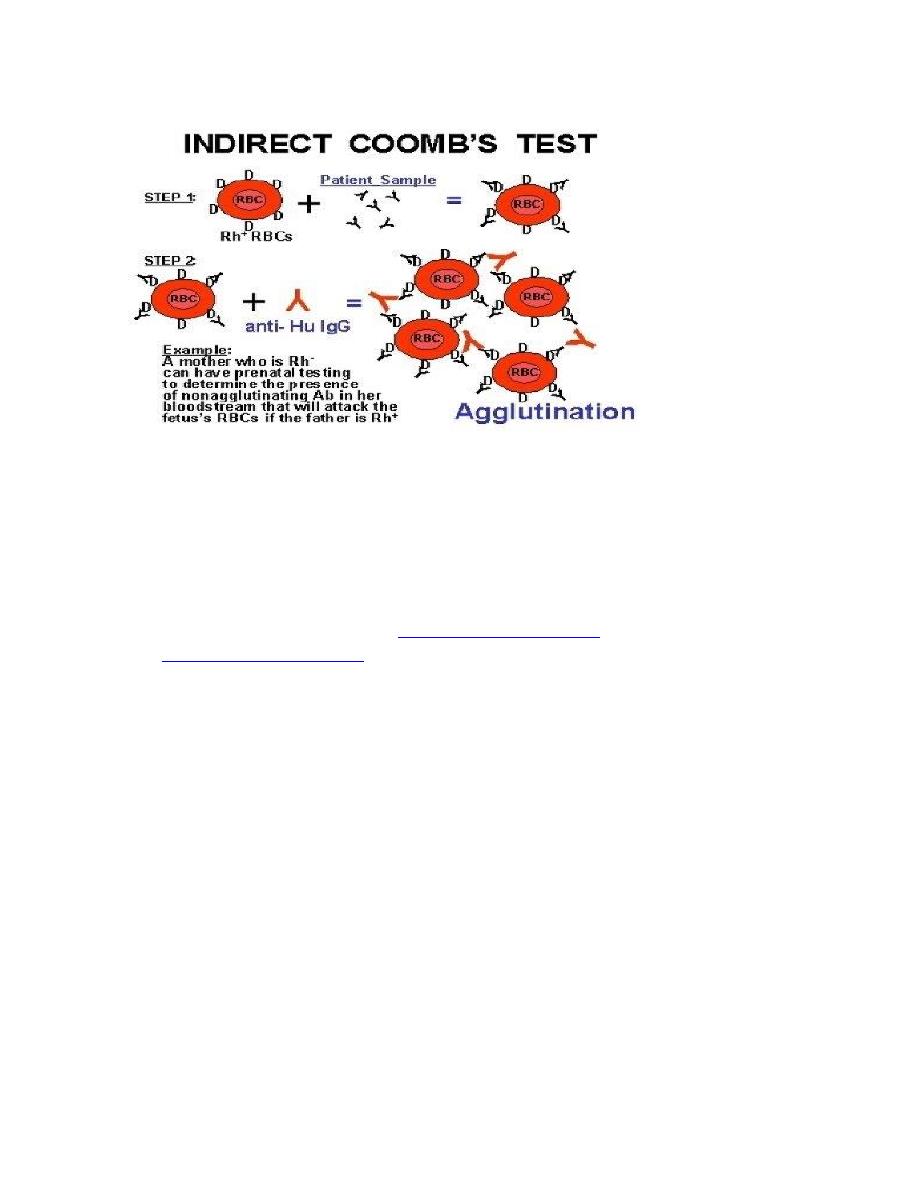
Indirect Coombs test:
• This is an immunological test can be used to detect whether Rh-negative
mother is sensitized or not.
• Maternal serum (which may contain maternal anti-D antibodies (IgG)+ Rh-
positive RBCs+ Anti-IgG antibodies leads to agglutination means that the
mother is sensitized.
Immunology
Dr Ahmed Abdullah
Lecture 3
10
(3)
References:
1. Sharp J, Whitley P, Cunnion K and Krishna N (2014).
Peptide inhibitor of complement
C1, a novel suppressor of classical pathway activation: mechanistic studies and clinical
potential. Front. Immunol.
2.
Encyclopedia Botanica, inc.
3. Bioscience notes, direct coombs test.
4. Kuby immunology 8th edition
