
Streptococcus and Enterococcus:
Objectives
The objective of this lecture are to know
1. general characters of family streptococci
2. classification of streptococci
3. beta hemolytic streptococci and their virulence factors disease
caused by them and main feature used for identification
General characteristics
They member of family streptococcacea
The Streptococcaceae consist of a large family of medically important
species, including Streptococcus spp. and Enterococcus spp.
They are
Catalase negative
Cytochrome enzyme (oxidase) negative, which differentiated them
from other micrococal and staphylococci.
Elongated cocci (more than spherical) arranged in chains when
grown in broth.
Facultative anaerobic
Fastidious (require special condition and enriched media) and some
spp are capnophilic (require CO2 for growth).
Genus Streptococci
Classification
schemes
:
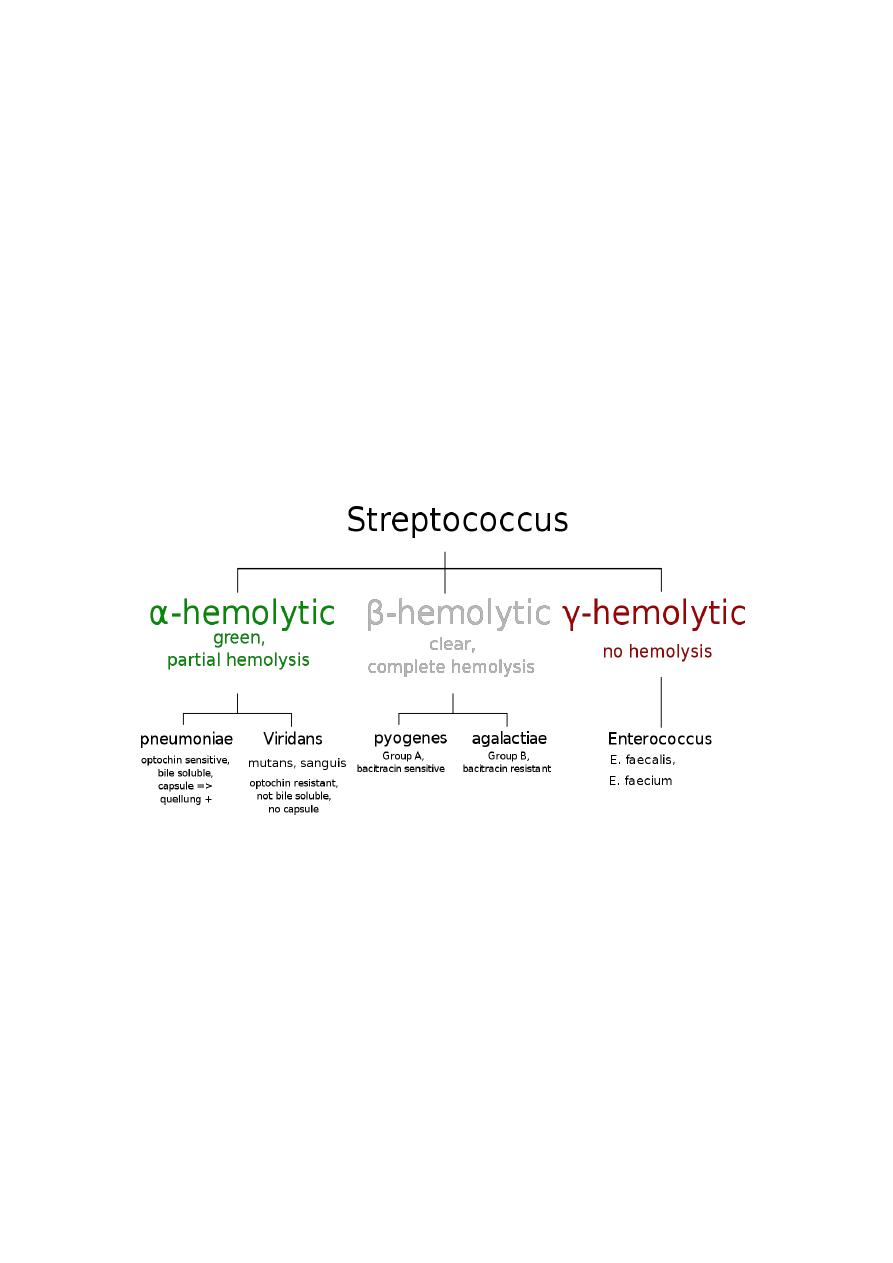
Four commonly used classification schemes are:
i.
Hemolytic pattern on sheep blood agar (SBA).
There are 3 type of hemolytic pattern:
1. Alpha α-hemolysis partial hemolysis greenish discoloration
around the colony (AH) Streptococcus pneumoniae , viridans
streptococci.
2. Beta hemolysis clear zone around the colony (BH) e.g.
Streptococcus pyogenes and Streptococcus agalactiae.
3. Non haemolytic no change in the medium e.g. Enterococcus
feacalis
ii.
Serological grouping (
Lancefield groups) On the basis of group
specific antigens in the cell wall, streptococci are divided into
20serological groups from A-H and K-V (without I and J). These
are known as
Lancefield groups. Groups A, B, C, D, and G are most
commonly found associated with human infections.
The antigen detected in Lancefield grouping include either cell
wall polysaccharide (C CHO) (A,B,C,F & G human groups) or
on lipotiechoic acid in group D & Enterococci. Viridians
streptococci do not posses any of the recognized Lancefield
grouping antigens.
iii.
Physiological characteristics.
iv.
Biochemical characteristics.
I.
Beta hemolytic streptococci
A. Streptococcus group A (S. pyogenes):
It colonizes the skin and upper respiratory tract of humans making
these sites the primary sources of transmission; carried on nasal,
pharyngeal, and sometimes anal mucosa; presence in specimens is almost
always considered clinically significant. It is transmitted either by direct
contact or aerosolized infection
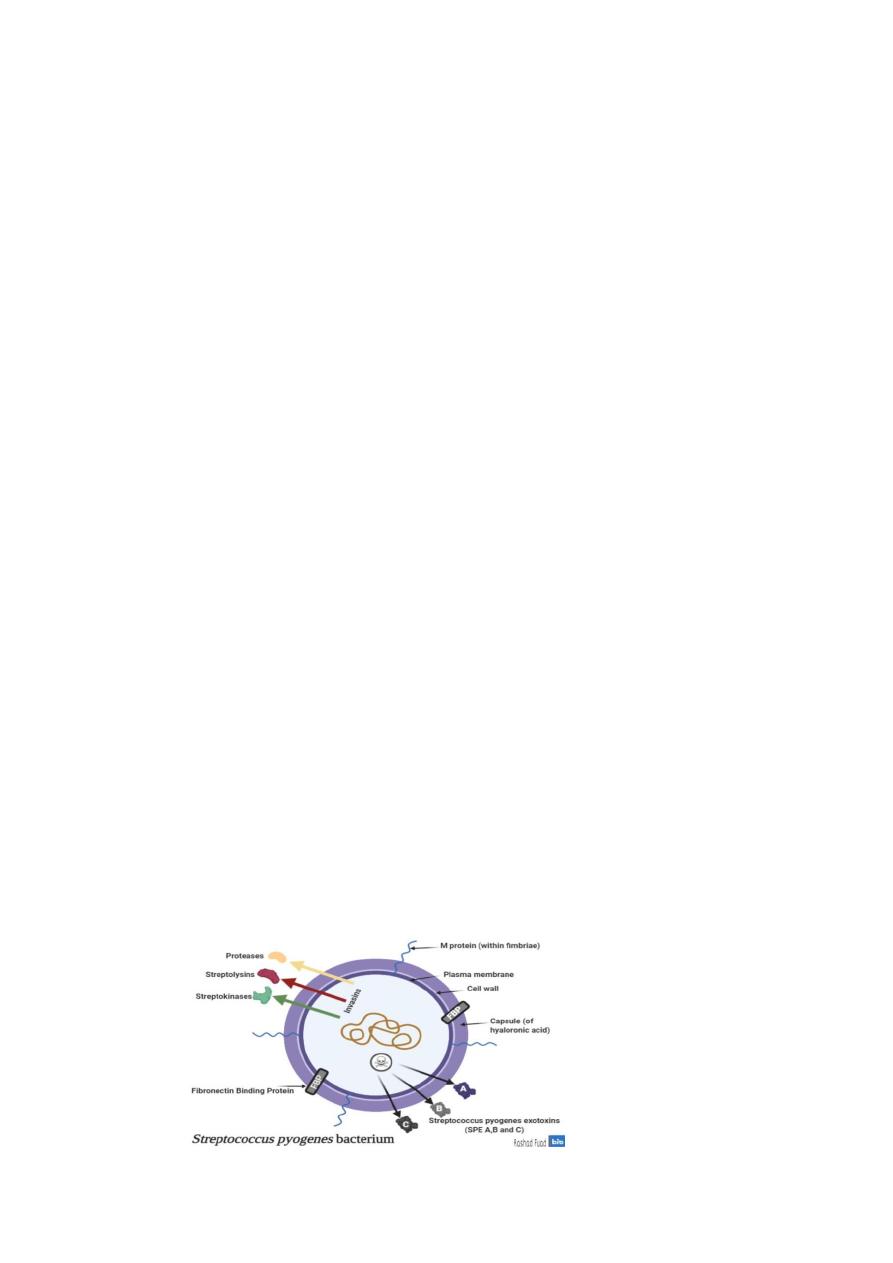
Virulence factors:
1. M- protein: is the best defined virulence factor. There are more than
80 serotype of M protein. It plays a role in resistance to phagocytosis
and adherence of mo to mucosal cells.
Resistance to infection with
S. pyogenes appears to be related to the presence of type-specific
antibodies to the M protein.
2. Fibronectin binding proteins (FBPs): these proteins play a role in
adherence of mo to keratinocyte.
3. Capsule: which is composed of hyaluronic acid it is
indistinguishable from the ground substance of connective tissue
which explain it is lack of immunogensity.
4. Streptolysin : Streptolysin O SLO (O2 labile and highly antigenic)
& Streptolysin S SLS (O2 stable and non antigenic).
ASO Test
antistreptolysin
O (ASO) antibodies appears in sera
following streptococcal infection. An ASO titer
in excess of 200
units/mL is considered
significant and suggests either recent or
recurrent
infection with streptococci.
5. Streptococcal pyrogenic exotoxin (SPE A , B & C): responsible for
the rash of scarlet fever and pathogenesis in streptococcal toxic
shock syndrome, SPE A & C act as superantigens that cause
hypotension and shock.
6. Other immunological active substances are:
a. hyaluronidase deploymerizes connective tissue
b. streptokinase hydrolyse fibrin clot
c. deoxy ribonucleases (DNAase used in debridement)
d. SIC protein that inhibits complements.

Clinical significant
:
Human is the natural reservoir of S. pyogenes transmitted from person to
person. It causes the following diseases
I.
Suppurative infection
1.
Streptococcal pharyngitis and tonsillitis is most common
infection caused by S. pyogenes children (5-15 years).
2.
Pyodermal infection including
a.
Impetigo: local infection of superficial layers of skin, especially in
children. It consists of superficial vesicles that break down and
eroded areas whose denuded surface is covered with pus and later is
encrusted. It spreads by continuity and is highly communicable.
b.
Erysiplus: results with massive brawny edema and a rapidly
advancing margin of infection.
c.
Cellulitis: Streptococcal cellulitis is an acute, rapidly spreading
infection of the skin and subcutaneous tissues.
3.
Scarlet fever: which is red spreading rash caused by SPE A it
commonly affects children. Signs and symptoms include sore throat, fever,
and a characteristic red rash followed by desquamated skin.
4.
Necrotizing fasciitis: this is an infection of the subcutaneous tissues
and fascia. There is extensive and very rapidly spreading necrosis of the
skin and subcutaneous tissues. It is called “flesh-eating bacteria.”
5.
Streptococcal toxic shock syndrome: resemble staphylococcal toxic
shock syndrome.
II.
Non suppurative sequelae Post streptococcal diseases :
1. Rheumatic fever (after pharyngitis): This is the most serious
sequelae of S pyogenes because it results in damage to heart muscle
and valves. Certain strains of group A streptococci contain cell
membrane antigens that cross-react with human heart tissue
antigens. Sera from patients with rheumatic fever contain antibodies
to these antigens.
Typical symptoms and signs of rheumatic fever
include fever, malaise, a migratory non suppurative polyarthritis,
and evidence of inflammation of all parts of the heart (endocardium,
myocardium, pericardium).

Pathogenesis
The pathogenesis of rheumatic fever is poorly understood. The disease is
autoimmune in nature and is believed to result from the production of
antibodies that cross react components of the bacteria and host tissues. A
common cross-reacting antigen may exist in some group a streptococci
and heart, therefore, antibodies produced in response to the streptococcal
infection could cross-react with myocardial and heart value tissues,
causing cellular destruction.
2.
Acute Poststreptococcal Glomerulonephritis
(AGN)
In contrast to rheumatic fever, which occurs only after pharyngitis, AGN
may be seen after either a pharyngeal or a cutaneous infection. Specific
nephrogenic strains of group A streptococci are associated with this
disease. AGN is most often seen in children
Pathogenesis
1. Immune complex deposition in the glomeruli.
2. Reaction of antibodies cross-reactive with streptococcal and
glomerular antigen.
3. Alterations of glomerular tissues by streptococcal products such as
streptokinase.
4. Direct complement activation by streptococcal components that have a
direct affinity for glomerular tissues.
Identification of group A
1. gram stain
Gram stain will reveal gram positive cocci with some
short chains
2.
Culture colonies of S. pyogenes on SBA are small, transparent, and
smooth with a well-defined area of β-hemolysis.
3.
biochemical
a)
hydrolyze PYR (positive )
b) CAMP test negative
c) bacitracin sensitive

Treatment
of streptococcal infection
Penicillin is the drug of choice; erythromycin is alternative in allergic
patients. Routine antibiotic susceptibility testing for Beta haemolytic is not
required (sensitive to penicillin).
B. Group B streptococci (S. agalactiae):
It is a part of Normal microbiota female genital tract and lower
gastrointestinal tract and occasional colonizer of upper respiratory tract. It
gets transmitted by
:
gaining access to sterile site(s) Probable Direct
contact: person to person from mother in utero or during delivery; or
nosocomial transmission by unwashed hands of mother or health care
personnel
Virulence factors:
The capsule is important virulence of group B it prevent phagocytosis.
Clinical infection:
S. agalactiae cause invasive disease in newborn in the form of two clinical
syndromes:
1. Early onset appear(less than 7 days old) 80% of clinical case of new
born in the form of bactermia , pneumonia and meningitis.
2. Late onset infection occurs between 1 week- 3month mainly in the
form of meningitis.
Infections in adults usually involve postpartum infections such as
endometritis, which can lead to pelvic abscesses and septic shock; or
bacteremia or arthritis etc.
Identification of group B :
1. gram positive chain of cocci
2. culture beta hemolytic small colonies on sheep blood agar
3. biochemical reaction
a. CAMP reaction positive (Christie, Atkins and Munch-Peterson),
which can be demonstratedas an accentuated zone of hemolysis
(arrowhead shaped area of enhanced hemolysis) when S.agalactiae
is inoculated perpendicular to a streak of Staph. aureus grown on
blood agar .
b. bacitracin resistance
c. hippurate hydrolysis positive
The treatment of choice is ampicillin +aminoglycoside.
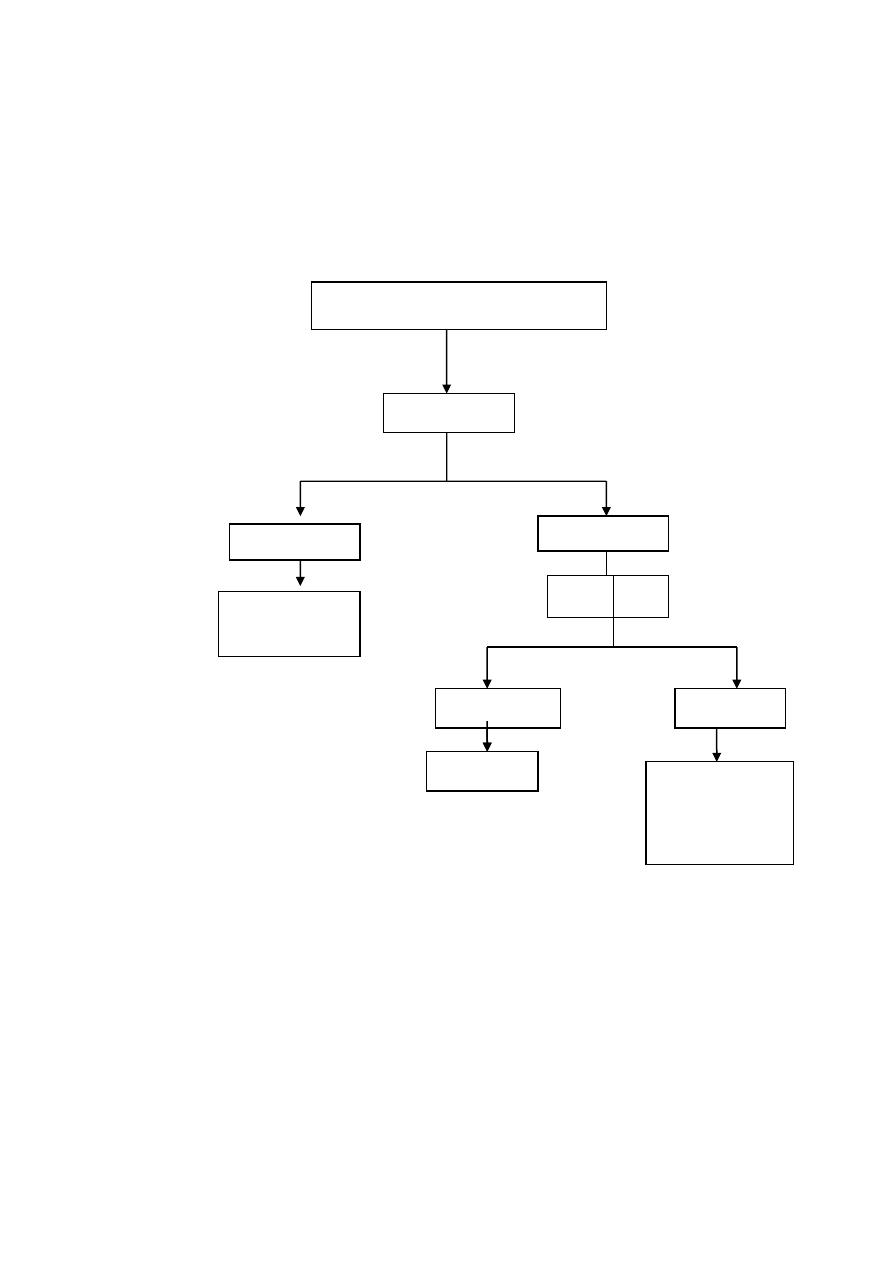
Beta Hemolytic streptococci
Bacitracin
susceptible
resistant
group A
streptococci
CAMP
test
Positive
Negative
Group B
non group A
non group B
