Streptococcus and Enterococci
lec 2
د.اسماء زكي شيتاوي
Objectives:
1. to understand the alpla hemolytic streptococci and their main
virulence factors , infection caused by this groups and their
identification
2. to understand non hemolytic streptococci and enterococci their
main virulence factors , infection caused by this groups and their
identification
Alpha hemolytic streptococci
a. Viridans streptococci: The term viridis means “green.” (Latin for
“green”) because many of these bacteria produce a green pigment
on blood agar media
1. They are constituents of the normal flora of the URT , female genital
tract and GIT.
2. Many spp are α hemolytic and few spp are non- hemolytic and very
rarely beta hemolytic.
3. They do not possess any recognized Lancefield grouping antigen
lack of C CHO
4. Virulence factors
Generally considered to be of low virulence;
production of extracellular complex polysaccharides (e.g., glucans
and dextrans) enhance attachment to host cell surfaces, such as
cardiac endothelial cells or tooth surfaces in the case of dental caries.
5. Clinical infection: It is the most common cause of subacute
bacterial endocarditis, bacterimia, gingivitis and dental caries,
abscess formation
6. Viridians are general susceptible to penicillin, over the last 2 decade
there is increase resistance to penicillin, cephalosporin and
aminoglycoside. Accurate susceptibility to penicillin is required to
viridians when isolated from serious infection.

Identification:
✓ stain gram positive chain of streptococci
✓ culture alpha hemolysis (green color around the growth)
✓ biochemical
• optochin resistance
• bile insoluble
• lack of capsule
b. Streptococcus pneumonia:
It colonizes the nasopharynx it is transmitted by direct contact from
person to person
Virulence factor:
1. Capsular polysaccharide is main virulence factor by which the mo
resists opsonization and phagocytosis. There are at least 90
capsular types, 23 of these type accounts for over 88% of
pneumoncoccal meningitis and bacterimia.
2. Several toxin produced include hemolysin, IgA1 proteases,
neuraminidase , hyaluronidases, pneumolysin, teichoic acid and
lipotiechoic acid.
Clinical infection:
The organism may harmlessly inhabit the upper respiratory tract with
a 5% to 75% carriage rate in humans.
S. pneumoniae is capable of spreading to the lungs, paranasal sinuses,
and middle ear. In addition, this organism accesses the bloodstream and
the meninges to cause acute, purulent, and often life-threatening
infections
.
So it causes pneumonia (2ry pneumonia), otitis media (recurrent
infection in children under 3years of age) ,sinusitis , meningitis 2ry to
otitis media affect all age group and bactermia.
Identification :
✓ Gram stain gram positive diplococcic (pairs of cocci)
✓ Culture alpha hemolysis on blood agar

✓ biochemical activity
• optochin sensitive
• bile soluble
• capsulated microorganism(capsule swelling test is
positive)
Antimicrobial resistance:
Over the last three decades S pneumoniae have become increasingly
resistant to penicillin and generally treat with erythromycin.
α hemolysiss
optochin
sensetivity +bile
soblubility
susceptible + bile
solable
s
.
pneumoniae
resistance +bile
insolable
bile esculin
positive
enterococci or gp
D
negative =
viridans
Non hemolytic streptococci (gamma hemolytic)
Group D
They are mainly non hemolytic but could be alpha may cause UTI or
endocarditis
Identification
Gram stain gram positive chain
Culture alpha or non- hemolytic mainly non
Biochemical:
• growth at 6.5% negative.
• growth in bile negative.
• growth at 45 C negative.
• sensitive to penicillin
Genus Enterococcus:
1. Enterococcus microscopic morphology is similar to streptococci on
Gram stain. Enterococcus species, previously classified as group D
streptococci until 1984.
2. These mo are normal residents of GIT and in lower number of the
vagina and male urethra.
3. E. feacalis is the most common isolate being associated with 80-
90% of human enterococcal infection. E. faecium ranks second and
is isolated from 10-15% of infection.
4. It is the second most common cause of nosocomial UTI and wound
infection and the third most common cause of bacterimia.
5. The ability of enterococci to hydrolyse esculin differentiated it
from non-hemolytic or alpha hemolytic streptococci other than gp
D.
6. Isolates that fit the criteria for diagnosis of enterococci ( bile
esculin +, PYR +, growth at 6.5% NaCl growth at 10- 45 C).
7. E.faecalis differentiated from faecium) by hippurate hydrolysis
( faecalis + faecium _-) .

8. They are generally resistant to penicillin and cephalosporin. Also
resistant to aminoglycoside and now emergence of vancomycin
resistance.
Biochemical
• growth at 6.5% positive .
• growth in bile positive
• growth at 45 C positive .
• resistance to penicillin .
• bile esculin hydrolysis is positive
Laboratory diagnosis of Streptococci:
I.
Direct detection:
1.
Gram stain of clinical specimen show gram positive cocci arranged
in chains or pairs.
2.
Direct detection of Antigen of group A, B and pneumococcal
capsular Antigen by slide agglutination or latex or Enzyme immunoassay.
3.
Quelling reaction for capsular type of pneumococcus seldom used.
4.
DNA probe has been used for direct detection of gp A.
II.
Culture:
1. Sheep blood agar 5% is suitable media for isolation where we can
evaluate hemolysis. Group A, B, C, F and G Beta hemolytic
(hemolysis is enhanced under anaerobic condition e.g inoculation
by stabbing inside the media ), while majority of group D and
enterococci are either non hemolytic or AH.
S. pneumoniae Surrounded with intense green AH. Viridans
streptococci are AH or NH.
2. Other media used Columbia base medium. The colonies are then
tested for catalase and oxidase (both are negative).
III.
Biochemical activities:
Presumptive identification can be accomplished using few biochemical
tests which are selected depending on the hemolytic pattern.
1. Bacitracin susceptibility : This test used to identify Beta Haemolytic
gp A (Streptococcus pyogens) which sensitive to Bacitracin while
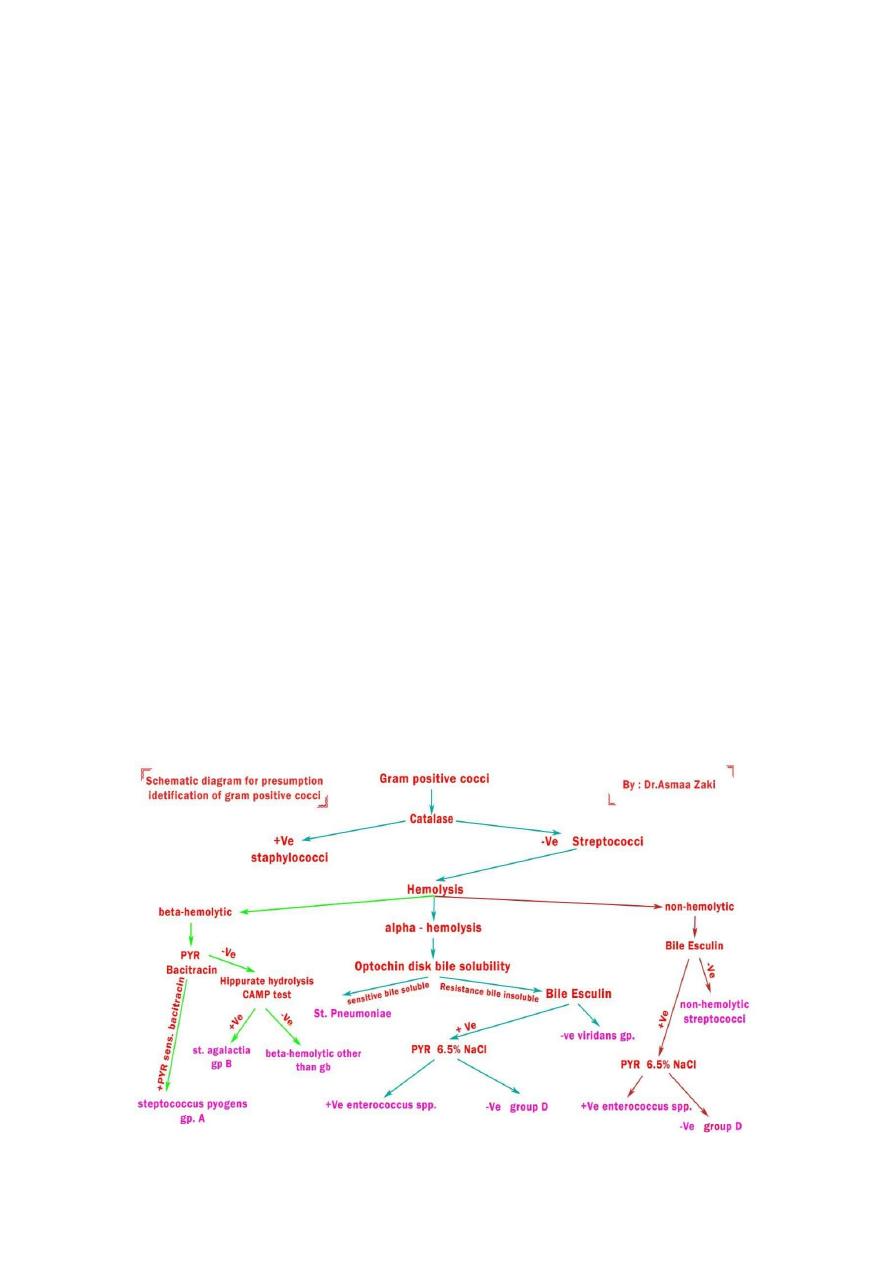
Beta hemolytic gp B is resistant (S. agalactiae). Bacitacin disk
contain 0.04 unit of bacitracin any zone of inhibition considered
sensitive. .
2. CAMP test used to differentiate gp B from other Beta haemolytic
streptococci. Arrowhead shaped area of enhanced hemolysis are
formed when 2 streak Staph aureus and gp B streptococci approach
each other.
3. Hippurate hydrolysis : differentiate agalactia (+) from other beta
hemolytic strep. Some isolates of gp D give +ve hippurate hydrolysis
but are not BH.
4. PYR hydrolysis (pyrrolidonyl aminopeptidase) to identify gp A.
5. Bile esculin hydrolysis to differentiate gp D & Enterococcus from
other Strep (viridans gp) .
6. Salt tolerance test : to differentiate gram positive cocci that grow
6.5% (enterococci) from those inhibited by it ( gp D).
7. Optochin Susceptibility and bile solubility: used to differentiate S.
pneumoniae from viridians gp.
