Parasitology
Notes…
1
Parasitology Lecture.2 & 3 (Protozoa Entamoeba Histolytica)
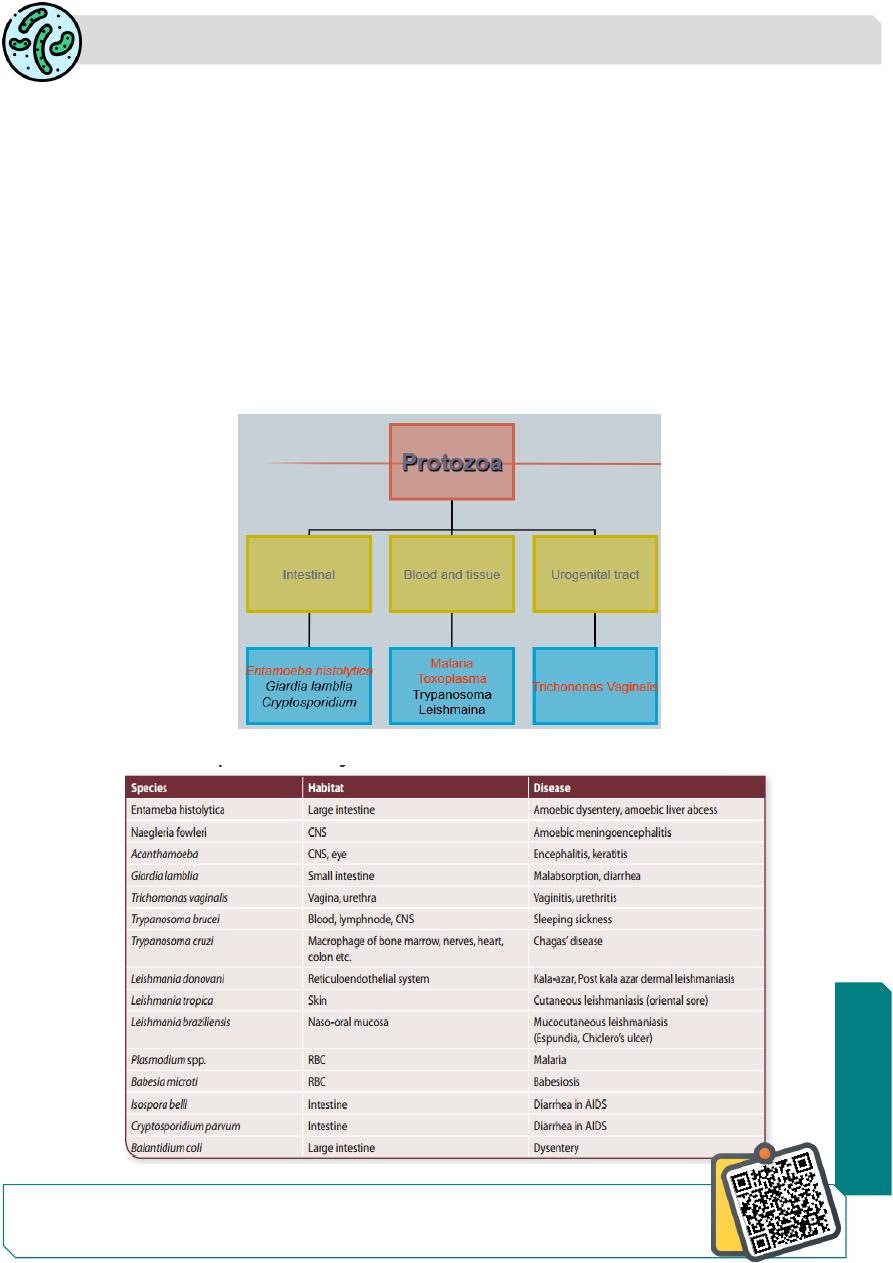
Protozoa
-Single-celled eukaryotic microorganisms.
-Protozoa(Greek protos:first: zoon: animal)
-The single protozoal cell performs all functions.
Most of the protozoa are nonpathogenic but few may cause major diseases such as
malaria, leishmaniasis,
-Protozoa like Cryptosporidium parvum,Toxoplasma gondii are being recognized as
opportunistic pathogens in patients affected with (HIV) and in those with
immunosuppressive therapy.
-Protozoa exhibit wide range of size (1–150 µm), shape, and structure
Principal Protozoan Pathogen of Man
N
eed S
om
e H
el
p?

Parasitology
Notes…
2
Amoebae are structurally simple protozoans which have no fixed shape.
classified under
Phylum: Sarcomastigophora,
Subphylum: Sarcodina,
Superclass: Rhizopoda
Order: Amoebida.
The cytoplasm of amoeba is bounded by a membrane and can be differentiated into an
outer ectoplasm and inner endoplasm.
Pseudopodia are formed by the amoeba by thrusting out ectoplasm, followed by
endoplasm.
These are employed for locomotion and engulfment of food by phagocytosis.
Classification of Amoebae
Entamoeba Histolytica
Epidemiology :
E. histolyticais worldwide in prevalence
The incidence of Amebiasis is common & high in tropical & subtropical areas. It has
been found wherever sanitation is poor in all climatic zones
It has been reported that about 10% of world population and 50% of developing countries
may be infected with the parasite.
The infection about 1% of Americans being reported, While the majority of infected
humans (80–95%) are Asymptomatic.
invasive amoebiasis causes disabling illness in an estimated 50 million of people and
causes 50,000 deaths annually amoebiasis is the third parasitic cause of mortality after
malaria and schistosomiasis
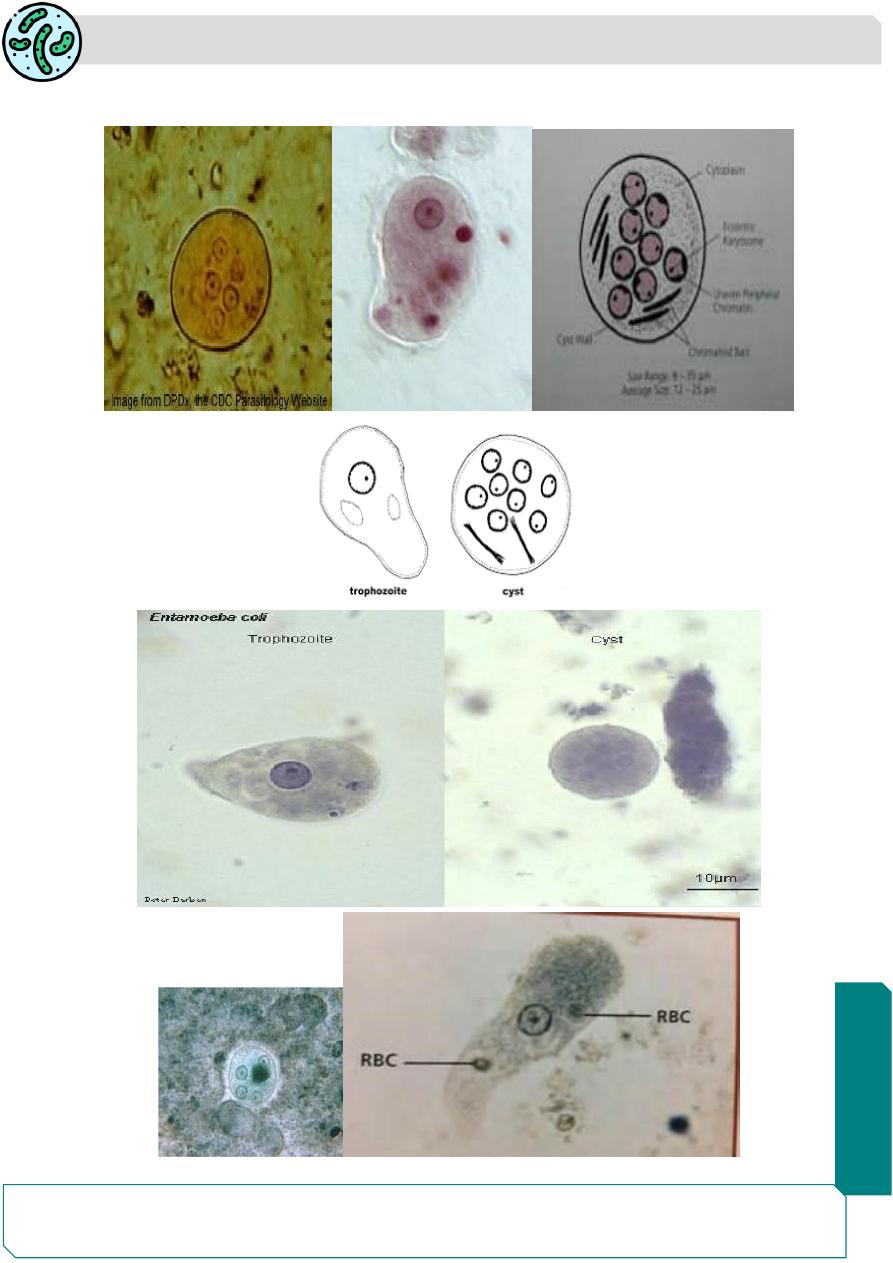
Morphology
E. histolytica occurs in 3 forms .
Trophozoite
Precyst
Cyst.
Parasitology
Notes…
3
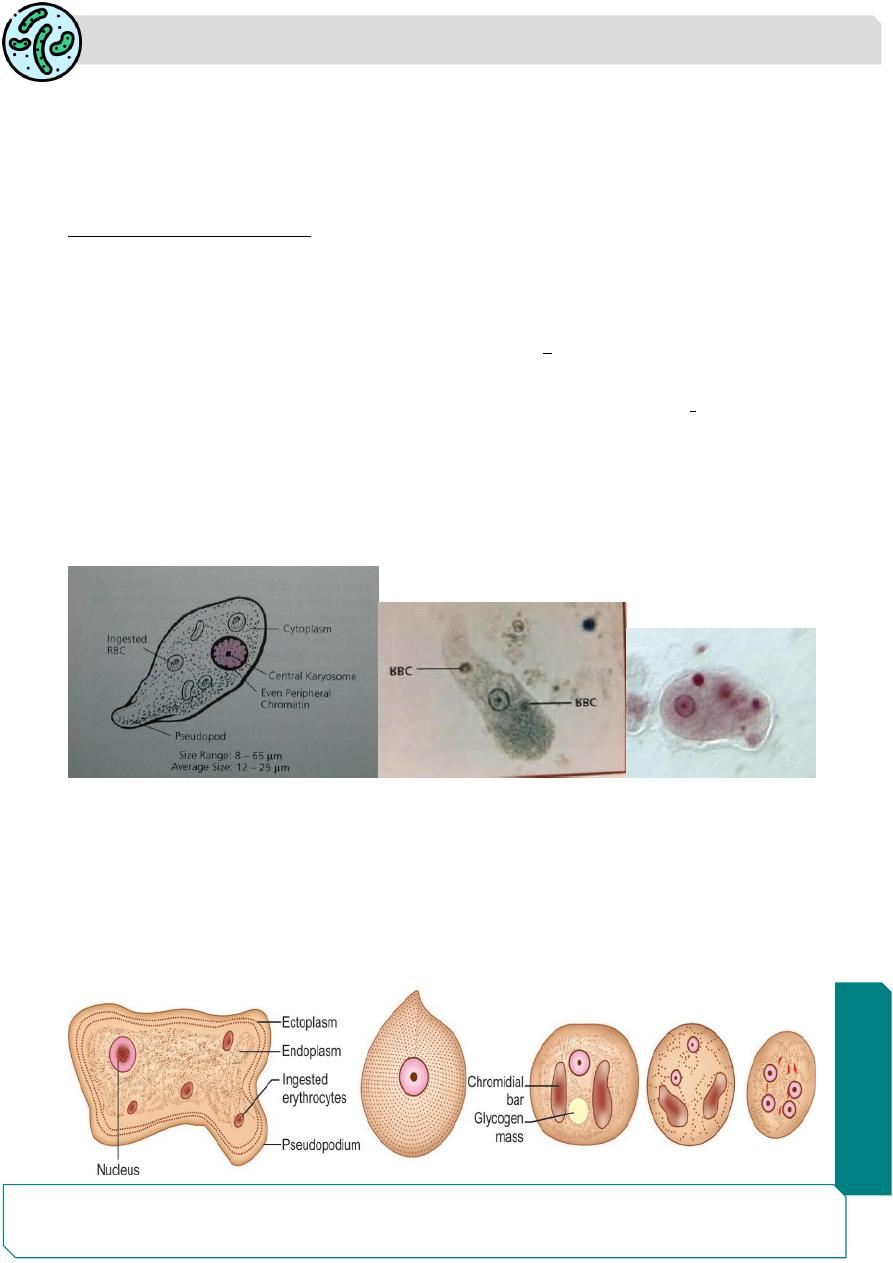
Trophozoite
Trophozoite is the vegetative or growing stage of the parasite .
It is the only form present in tissues and in intestine
The parasite, as it occurs free in the lumen as a commensal is generally smaller in size,
about 15–20 µm and has been called the minuta form
Morphology ( Trophozoite ):
1- It is irregular in shape and varies in size (12-60 µm),actively motile in freshly passed
dysenteric stools.
2- Large finger – like pseudopodia
3- the Cytoplasm: is differentiated into outer Clear ectoplasm ,inner endoplasm is
granular and may contain RBCs,food vacuols,granules.
4- It has one nucleus, is spherical 4–6 µm in size contain small central karyosome and
fine chromatin granules arranged regularly beneath nuclear membrane.
The trophozoites divide by binary fissionin every 8 hours.
Trophozoites survive upto 5 hours at 37°C and are killed by drying, heat, and chemical
sterilization.
Therefore, the infection is not transmitted by trophozoites
Precystic Stage
Trophozoites undergo encystment in the intestinal lumen.
Encystment does not occur in the tissues
Before encystment, the trophozoite extrudes its food vacuoles and becomes round or
oval, about 10–20µm in size.
the precystic stage of the parasite contains a large glycogen vacuole and two chro-matid
bars. then secretes a highly retractile cyst wall around it and becomes cyst.
Parasitology
Notes…
4
Cystic Stage
The cyst is spherical in shape about 10–20 µm in size.
The early precystic stage contains a single nucleus and two other structures—a mass
of glycogen and two chromatoid bodies .
As the cyst matures, the glycogen mass and chromidial bars disappear and the nucleus
undergoes 2 successive mitotic divisions to form 2 and then 4 nuclei ,The mature cyst is,
thus quadrinucleate.
The cyst wall is a highly retractile membrane, which makes it highly resistant to gastric
juice and unfavorable environmental conditions
Morphology ( mature cyst) :
1- Small in size (10 – 20 µm) , spherical or oval in shape, thick wall about 0.5 micron
.containing 1 - 4 nuclei ,vacuoles,glycogen . Each nucleus contain similar nuclear
morphology like the trophozoite.
Transmision of amoebiasis occur through:
1. Mature cyst is the main sours of the infection which passes with the feces of chronic
patients or asymptomatic carrier .
2. Human being acquire the infection via contamination of food, drinks, vegetables or
hands with infective cysts especially in resturants .
3. Flies (House fly) play an important roles in transmission of these cysts to the food of
human .
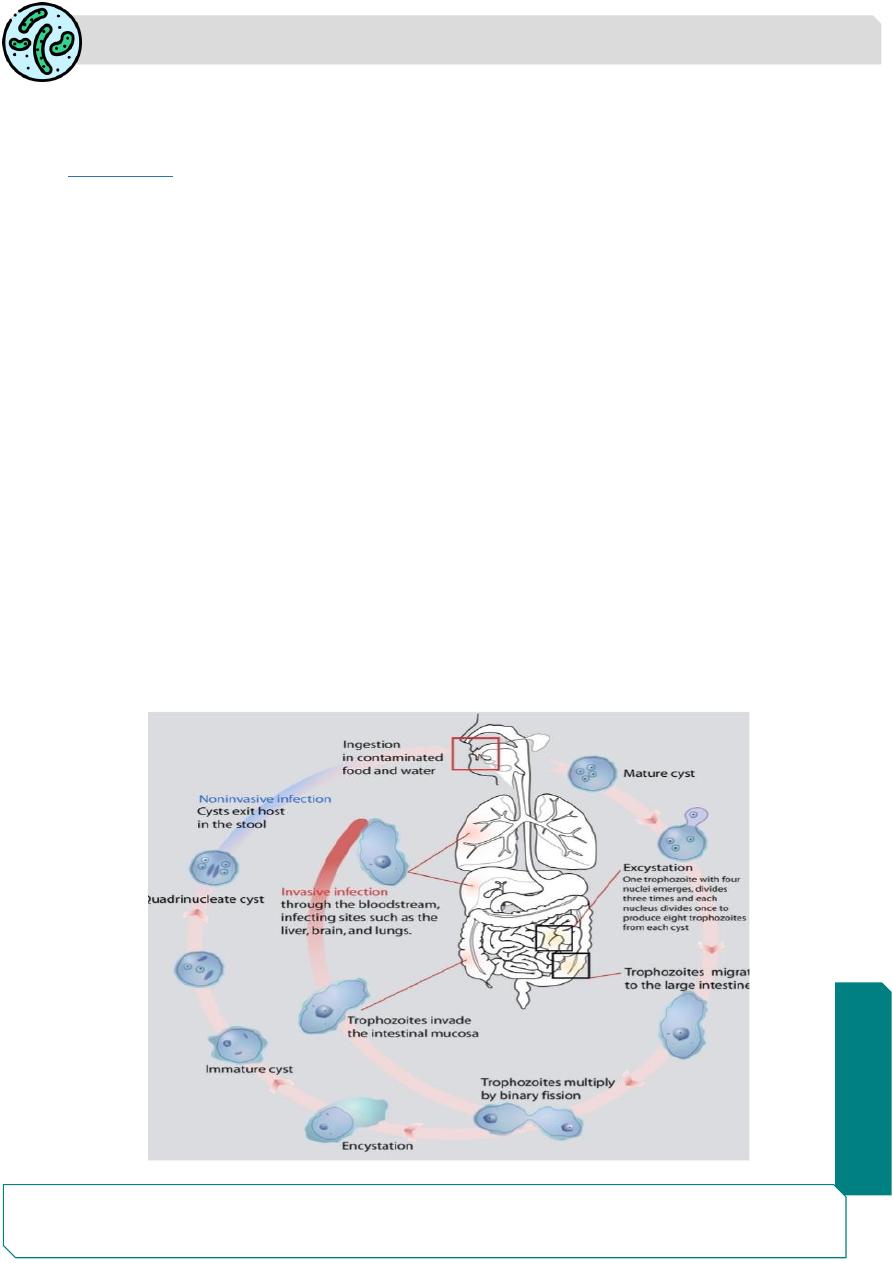
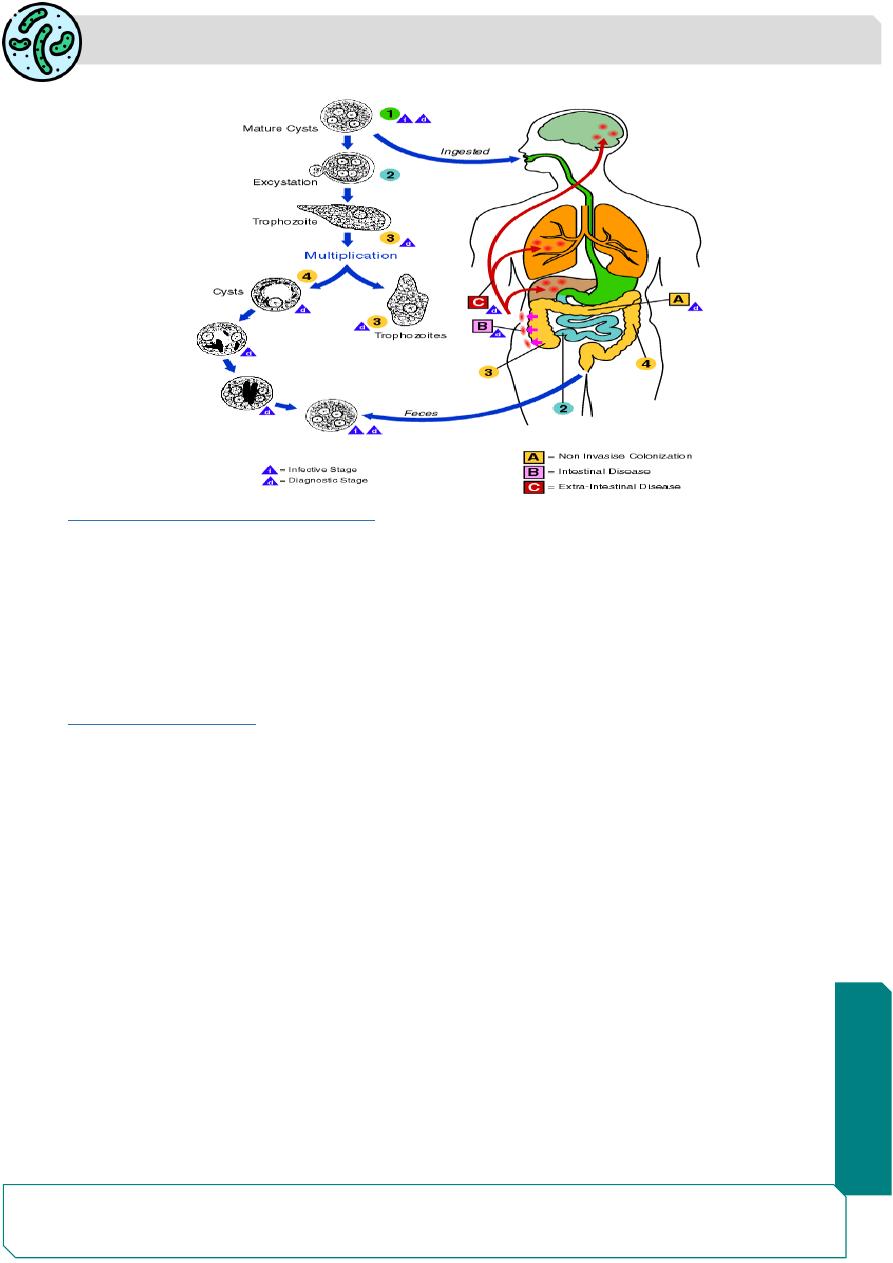
Life Cycle
life cycle only in one host
Infective form: Mature quadrinucleate cyst .
The cysts can remain viable under moist conditions for about 10 days.
E. histolytica causes intestinal and extraintestinal amoebiasis.
Parasitology
Notes…
5
Incubation period ranges from 4 days - 4 months.
As the cyst wall is resistant to action of gastric juice, the cysts pass through the stomach
undamaged and enter the small intestine.
Excystation:
When the cyst reaches caecum or lower part of the ileum, due to the alkaline medium,
the cyst wall is damaged by trypsin, leading to excystation after excystation the
cytoplasm gets detached from the cyst wall through which (4amoeba) quadrinucleate
amoeba is liberated into metacystic trophozoites:
The nuclei in the metacyst trophozoites immediately undergo division to form 8 nuclei,
each of which gets surrounded by its own cytoplasm to become 8 small amoeba or
metacystic trophozoites.
The optimal habitat for the metacystic trophozoite is the submucosal tissue of caecum
and colon and grow by binary fission
Some develop into precystic forms and cysts, which are passed in feces to repeat the
cycle .
In most of the cases, E. histolytica remains as a commensal in the large intestine without
causing any ill effects. Such persons become carriers or asymptomatic
Sometimes, the infection may be activated and clinical disease ensues
In some patients the trophozoites invade the intestinal mucosa and cause intestinal
disease or developed perforated ulcer .
the trophozoites migrate through the blood stream to invade the extra intestinal organs
such as the liver, brain, and lungs and it will cause amoebic infection in these organs.
Parasitology
Notes…
6
Life cycle of E. histolytica:
Pathogenesis and Clinical Features
E. histolytica causes intestinal and extraintestinal amoebiasis.
Incubation period ranges from 4 days to 4 months. Pathogenesis depend on
1- The resistance of the host .
2- The number of the amebas.
3- Presence of pathogenic bacteria.
4.Presence of physical & chemical injury of the mucosa
Intestinal Amoebiasis
The lumen-dwelling amoebae do not cause any illness
Amoebiasis occure only when they invade the intestinal tissues in about 10% of cases of
infection, the remaining 90% being asymptomatic .
The metacystic trophozoites penetrate the columnar epithelial cells in the crypts the
colon.
Penetration of the amoeba is facilitated by the motility of the trophozoites and the tissue
lytic enzyme,which damages the mucosal epithelium.lead to form ulcers with pinhead
center and raised edges.
Sometimes, the invasion remains superficial and heals spontaneously.
More often, the amoeba penetrates to submucosal layer and multiplies rapidly, causing
abscess then breaks down to form an ulcer.
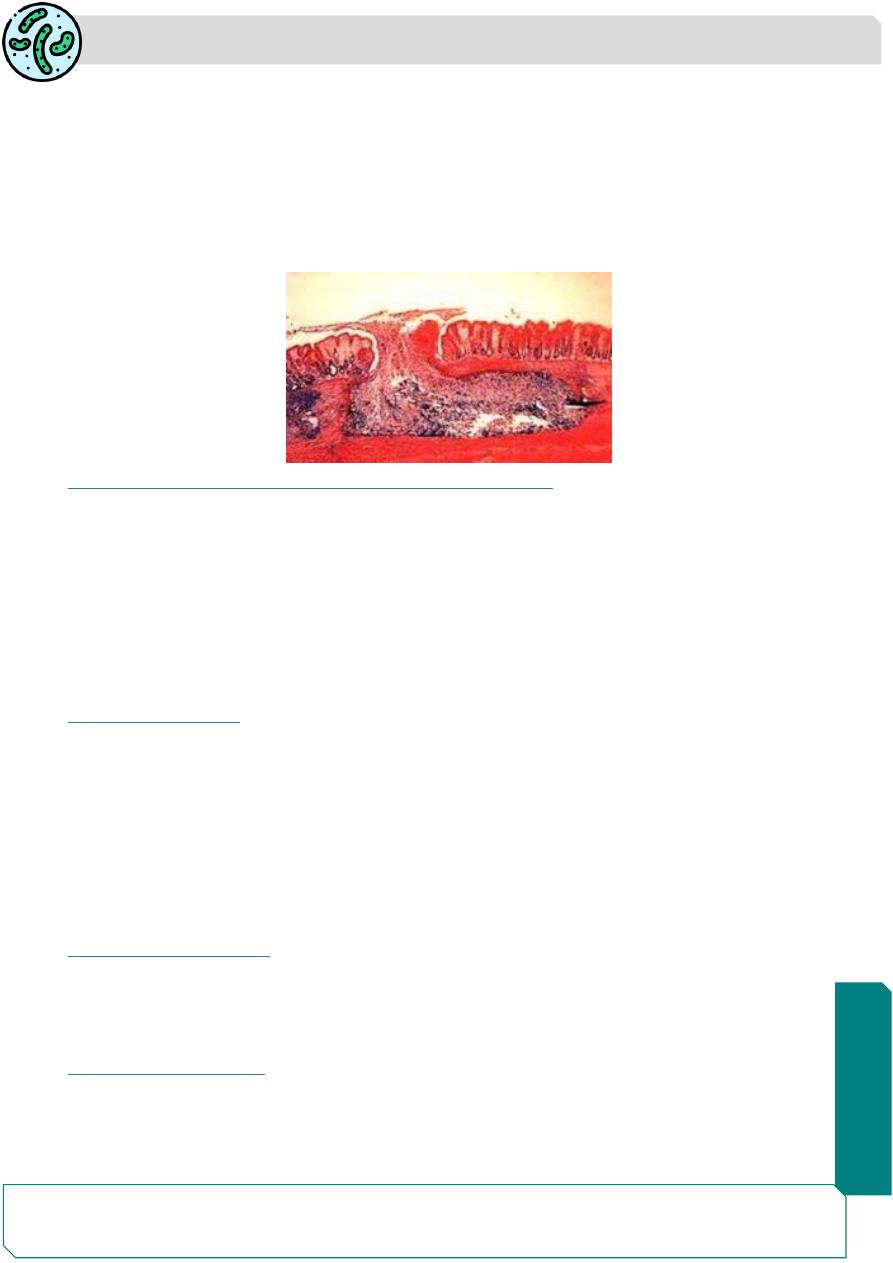
The typical amoebic ulcer is flaskshaped in cross section, with mouth and neck being
narrow and large rounded base .
Parasitology
Notes…
7
The amoebas usually found on the floor of the base of ulcer the ulcers may involve
the muscular and serous coats of the colon, causing perforation, hemorrhage and
peritonitis.
The superficial lesions generally heal without scarring, but the deep ulcers form scars
which may lead to strictures, partial obstruction .
chronic ulcer lead to amoebic granuloma or amoeboma may be mistaken for are
malignant tumor .
E. histolytica in the large intestine ( Flask shape ulcer )
Clinical Features of Intestinal Amoebiasis
The majority of infections with
E.histolytica
show 90% a symptoms or show symptoms
which varies from mild to intense and long lasting general discomfort, loss of appetite,
and weight loss with general malaise. Symptoms may develop within 4 days of exposure,
may occur up to a year later, or may never occur.
Amoebic dysentery(Bloody diarrhea), abdominal cramps, nausea and vomiting, and an
urgent desire to defecate
Hepatic Amoebiasis
about 2–10% of the individuals infected with E. histolytica suffer from hepatic
complications.
The history of amoebic dysentery is absent in more than 50% of cases.
Several patients with amoebic colitis develop an enlarged tender liver without detectable
impairment of liver function or fever
The incidence of liver abscess is less common in women and rare in children under 10
years of age
Pulmonary Amoebiasis
Very rarely, primary amoebiasis of the lung may occur by liver direct hematogenous
spread from the colon bypassing the The patient presents with severe pleuritic chest
pain, dyspnea, and non-productive cough..
Metastatic Amoebiasis
Involvement of distant organs is by hematogenous spread and through lymphatics.
Abscesses in kidney, brain, spleen, and adrenals have been noticed.
Spread to brain leads to severe destruction of brain tissue and is fatal.
Parasitology
Notes…
8
Cutaneous Amoebiasis
It occurs by direct extension around anus, colostomy site,
Genitourinary Amoebiasis
Amoebiasis which is acquired through anal intercourse.
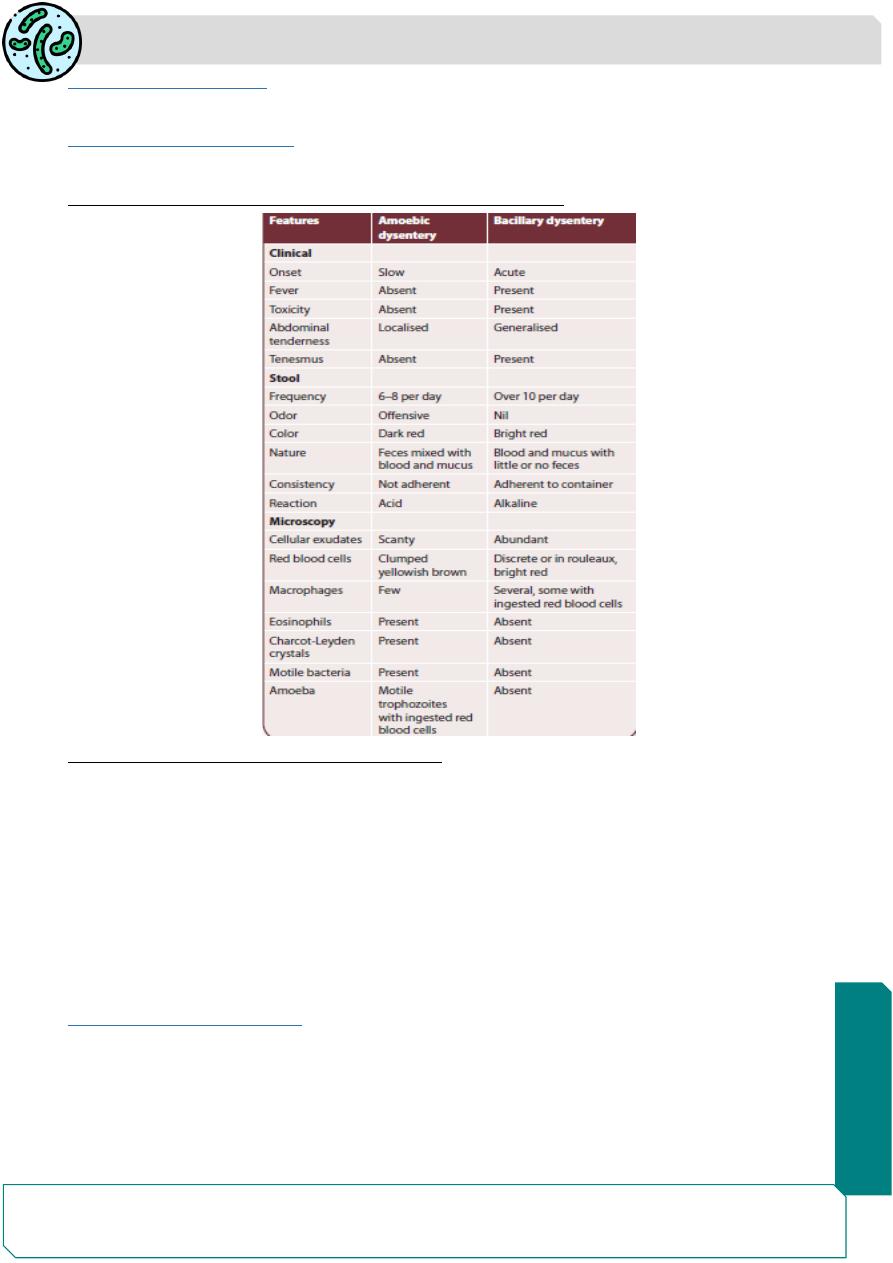
Differential Features of Amoebic and Bacillary Dysentery
The complications of intestinal amoebiasis:
1- Appendicitis .
2- Intestinal perforation .
3- Hemorrhage .
4- Liver abscess.
5- Ameboma (Granulomas)
6-Fulminant amoebic colitis
7-Toxic megacolon
8-Perianal ulceration
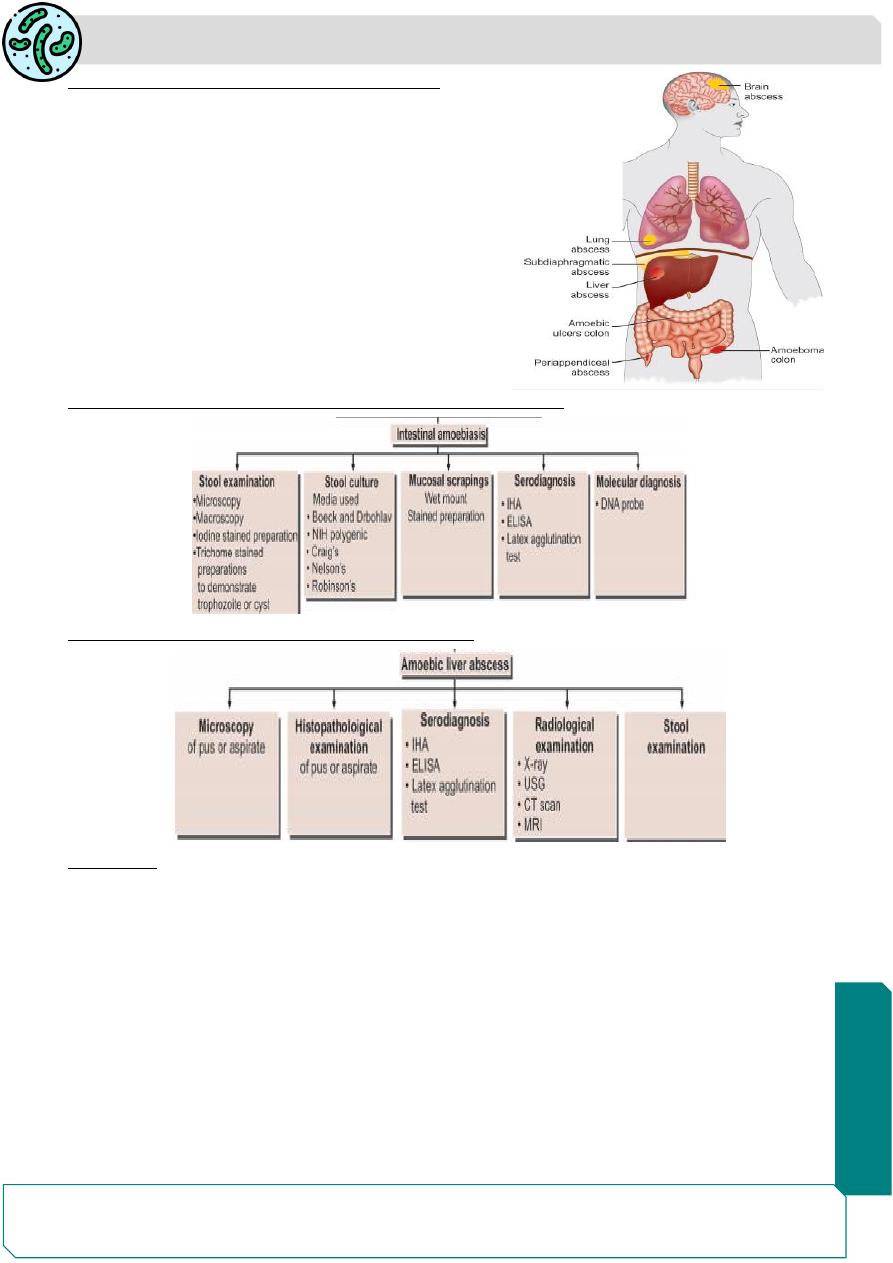
Extraintestinal Amoebiasis
The metastasis of amoeba usually via blood streem or by direct extension after
intestinal perforation to the peritonium.
The amoeba may cause local abcsess or peritonitis or migrate to the liver which is the
most commonly affected than other organs e.g, lungs, perianal skin and brain.
Parasitology
Notes…
9
Complication of extraintestinal amoebiasis
1. Amoebic hepatitis
2. Amoebic liver abscess
3. Amoebic appendicitis and peritonitis
4. Pulmonary amoebiasis
5. Cerebral amoebiasis ,Splenic abscess
6. Cutaneous amoebiasis
7. Genitourinary amoebiasis
Laboratory diagnosis of intestinal Entamoeba histolytica
Laboratory diagnosis of amoebic liver abscess
Treatment
Three classes of drug are used in the treatment of amoebiasis.
1-Luminal amoebicides: paromomycin30 mg/kg 4 times a day or tetracycline iodoquinol
650 mg orally ,three times day for 20) act in the intestinal lumen but not in tissues.
2-Tissue amoebicides: Emetine, chloroquine, etc. are effective in systemic infection, but
less effective in the intestine.
3-Both luminal and tissue amoebicides: Metronidazole( 750 mg three times a day, orally
or IV for 7 days) tinidazole 2 g/day orally for 3 days) and or nidazole act on both sites
and are the drug of choice for treating amoebic colitis and amoebic liver abscess.
Patients should remain in bed rest with oral rehydration and electrolyte replacement
should be done

Parasitology
Notes…
10
Prevention & Control :
1- All human infections should be treated
2- A symptomatic carriers should be treated especially those working in resturants
.
3- Effective enviromental sanitation is necessary to prevent water ,food , and vegitable
contamination, e.g. Sewage disposal should be treated with chemical before used as
fertiliser in gardens.
4- Chlorination & filtered water supply are important to kill the
E.histolytica
5- Insects should be controlled by insecticides.
6- Uncooked vegetables should be washed with running water. .
NON PATHOGENIC AMOEBA
These parasites are commensals none pathogenic but they are important because they
may be confused with
E.histolytica
.
The most none pathogenic amoebas affecting human being are:
1- E.coli. 2- E.gingivalis . 3- Dientamoeba fraglis. 4- Endolimax nana .
5- Iodoamoeba butschlii .
6- Other amoebas infecting human are morphologically very simillar to E.histolytica e.g,
E.hartmanni and E.dispar .
7- Free living amoebas are Negleria ,Acanthamoeba are accidental parasites of human
being .
The majority of these amoeba are non-pathogenic commensal parasites or only cause
mild infection.
Entamoeba. coli
It is worldwide in distribution and a nonpathogenic commensal intestinal amoeba .
life cycle only in one host
Infective form: Mature cyst
It is a parasite of the large intestine .
the
E. coli
medical importance because it may be mistaken for
E.histolytica
.
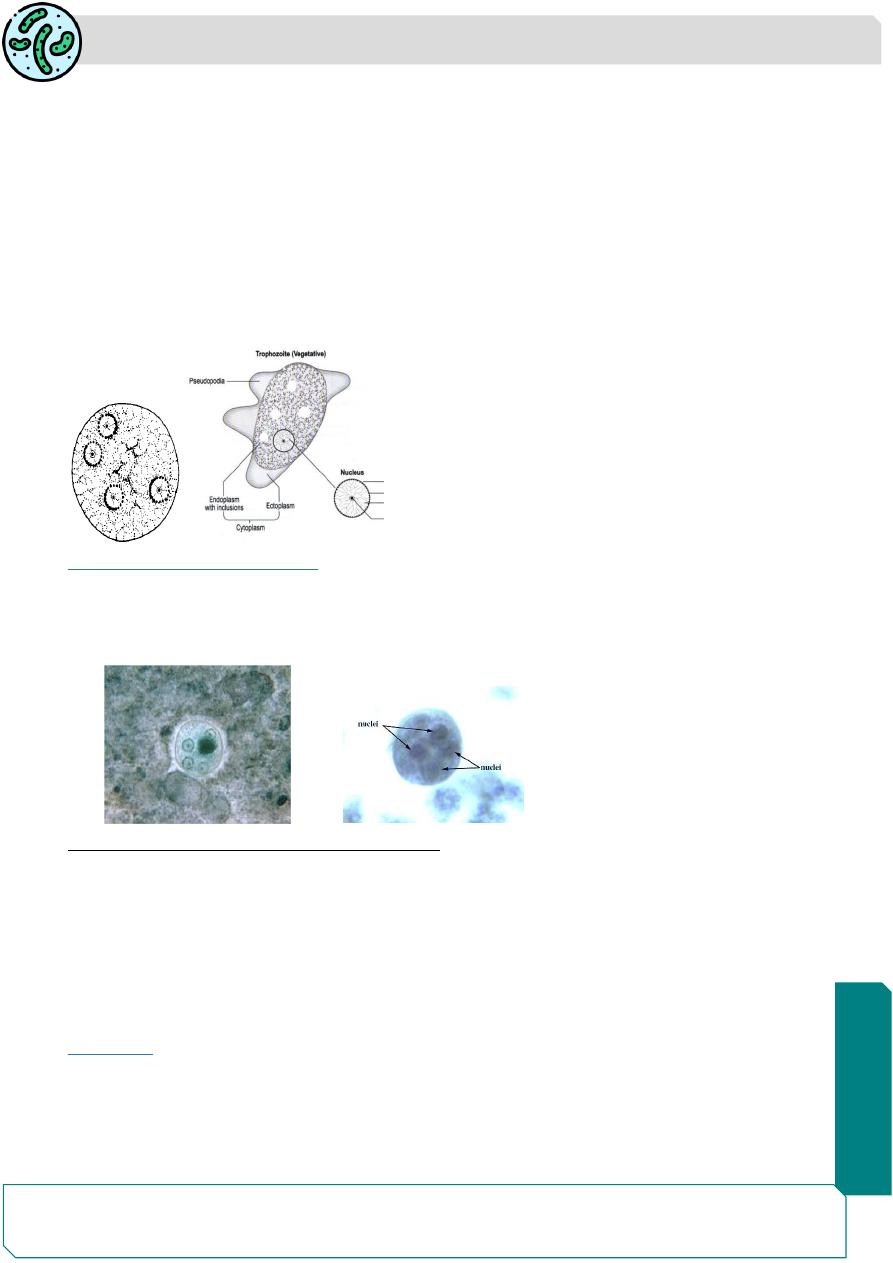
It has two stages (trophozoite& cyst).
The important morphological features are.
trophozoite
It is larger than E. histolytica about 20–50 µm with sluggish motility and
contains ingested bacteria but no red blood cells
The ectoplasm is not clear and it has small pseudopodia.
It has one nucleus contain large eccentric karyosome, and large chromatin granules
arranged irregularly beneath nuclear membrane
Cysts
are large oval in shap , 10–30 µm in size, with a prominent glycogen mass in the
early stage.
The chromatoid bodies are splinter like and irregular. The mature cyst has 8 nuclei.
Parasitology
Notes…
11
The life cycle is the same as in E.histolytica except that it remains a luminal commensal
without tissue invasion and is nonpathogenic
Parasitology
Notes…
12
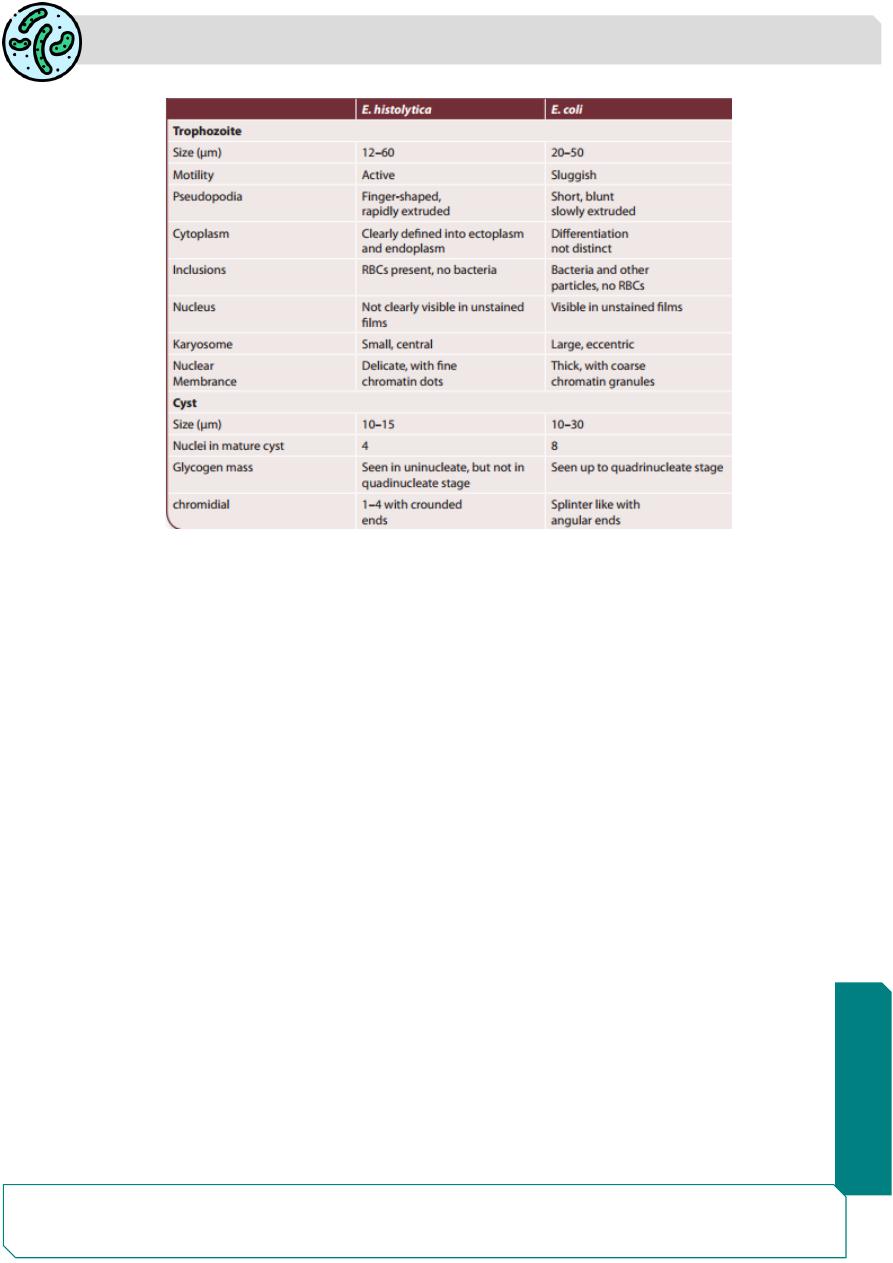
Difference between E.histolytica and E coli
