
Parasitology
Notes…
1
Malaria Lec.3
Pathogenesis and Clinical Features
Clinical manifestations in malaria are caused by products of erythrocytic schizogony and
the host's reaction to them.
The disease process in malaria occurs due to:
I.
the local or systemic response of the host to parasite antigens.
II.
tissue hypoxia caused by reduced oxygen delivery because of obstruction of blood
flow by the parasitized erythrocytes.
Liver is enlarged and congested. Kupffer cells are
increased and filled with parasites.
Spleen is soft, moderately enlarged and congested
in acute infection. In chronic cases, spleen is hard.
Kidneys are enlarged and congested.
The brain in P. falciparum infection is congested.
Anemia: After few paroxysms of fever, normocytic
and normochromic anemia develops.
Clinical Features of Benign Malaria
It is characterized by a triad of febrile paroxysm, anemia and splenomegaly.
Febrile paroxysm
❖ Fever comes intermittently depending on the species. It occurs every fourth day (72
hour cycle for P. malariae) and every third day (48 hour cycle for other three
species)
Paroxysm corresponds to the release of the successive broods of merozoites into
the bloodstream, at the end of RBC cycle.
The paroxysm usually begins in the early afternoon and lasts for 8-12 hours.
❖ Each paroxysm of fever is
comprised of three stages:
1. Cold stage: The patient feels intense cold with chill and rigor along with lassitude,
headache and nausea. This stage lasts for 15 minutes to 1 hour.
2. Hot stage: The patient feels intensely hot. The temperature mounts to 39
–41 °C or
higher. Headache persists but nausea commonly diminishes. This stage lasts for
2-6 hours.
3. Sweating stage: Fever comes down with profuse sweating. Skin becomes cold
and moist. Patient feels relieved and often asleep. This stage lasts for 2
–4 hours.
N
eed S
om
e H
el
p?
Parasitology
Notes…
2
Anemia
After a few paroxysms of fever,the patient develops a normocytic
normochromic anemia. Various factors can attribute to the development of
anemia such as:
1. Parasite induced RBC destruction
—Lysis of RBC due to release of merozoites.
2. Splenic removal of both infected RBC and uninfected RBC coated with immune
complexes.
3. Bone marrow suppression leading to decrease RBC production.
4. Increased fragility of RBCs.
5. Autoimmune lysis of coated RBCs.
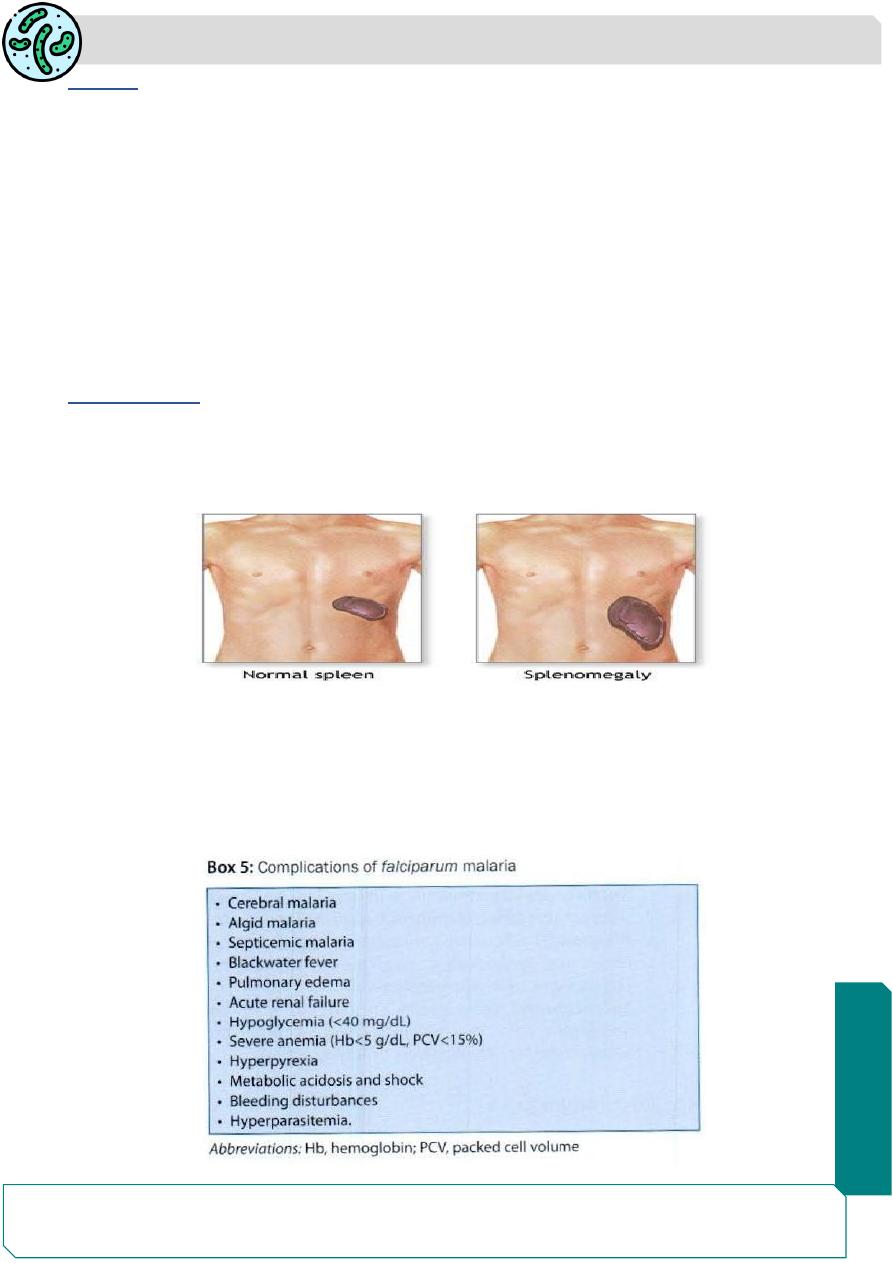
Splenomegaly
After a few weeks of febrile paroxysms, spleen gets enlarged and becomes
palpable. Splenomegaly is due to massive proliferation of macrophages that engulf
parasitized and non-parasitized coated RBCs.
Clinical Features of Malignant Tertian Malaria
The most serious and fatal type of malaria is malignant tertian malaria caused by
P. falciparum. Falciparum malaria
if not treated timely or adequately, severe life-
threatening
complications may develop. In severe falciparum malaria, parasitic load
is very high. it invades erythrocytes of all ages (old and young).
Parasitology
Notes…
3
1
. Cerebral malaria:
Occurs due to plugging of brain capillaries by the rosettes of sequestered
parasitized RBCs leading to vascular
occlusion and cerebral anoxia.
Cerebral malaria manifests as diffuse symmetric encephalopathy characterized by
generalized convulsion
in 10% of adults and up to 50% of children.
Other defects are retinal hemorrhages, neurologic sequelae, repeated seizures,
and rarely deep coma.
High mortality rate 20% among adults. and more than 15% among children.
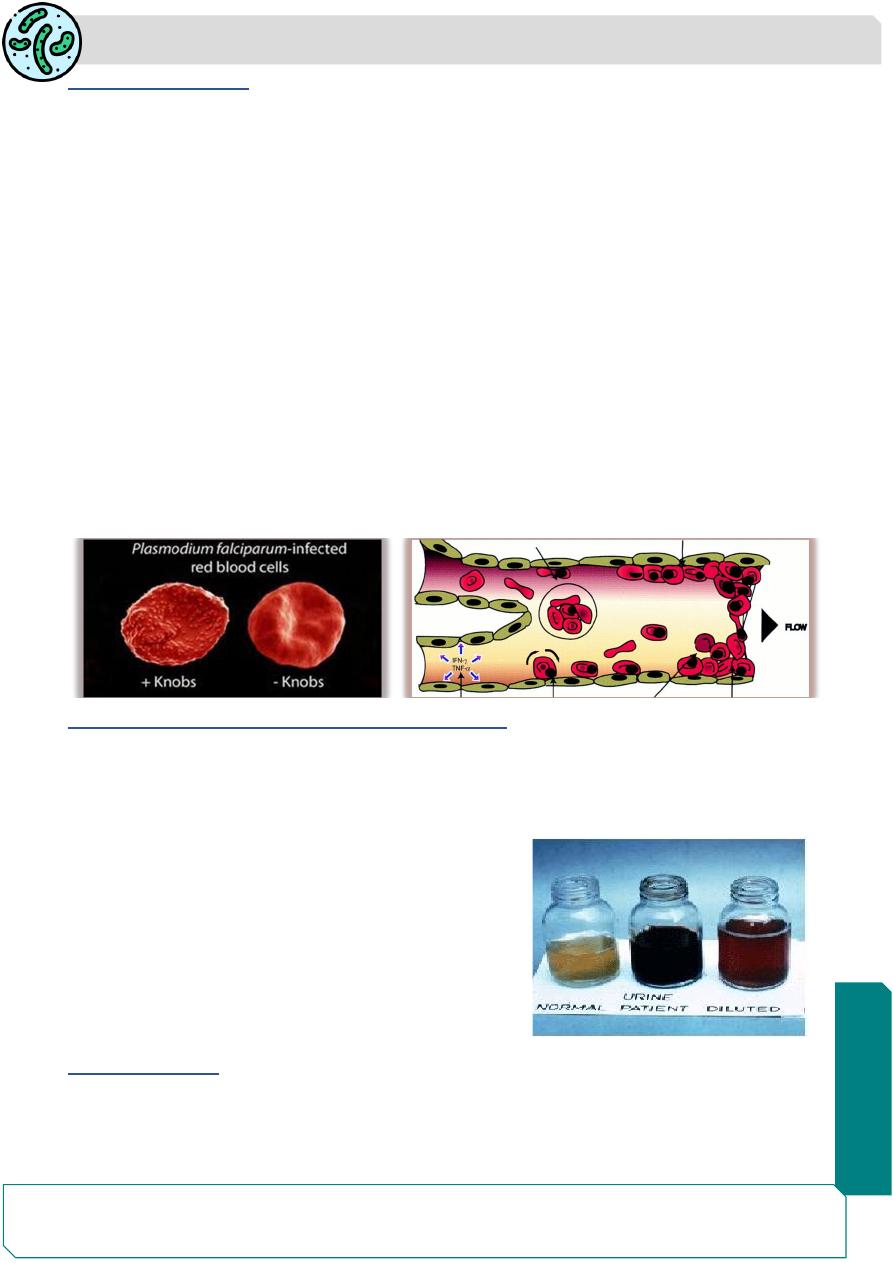
Soon after invasion of the RBC, the trophozoite produce protein that is deposited
in the erythrocyte surface membrane to form knob-like deformities, This knob
produces specific adhesive proteins [Plasmodium falciparum erythrocyte
membrane protein-I (PfEMP-1)]. which promote aggregation of infected RBCs to
other noninfected RBCs and to capillary endothelial cells.
These sequestrated RBCs cause capillary plugging of cerebral microvasculature,
which results in anoxia, ischemia and hemorrhage in brain.
2. Black-water fever (malarial hemoglobinuria) :
this syndrome is sometimes seen in falciparum malaria, particularly in patients, who
have experienced repeated past infections and inadequate treatment with quinine.
Clinical manifestations include: fever, hemoglobinuria (black colored urine),
bilious vomiting and prostration.
The pathogenesis is believed to be massive
intravascular hemolysis caused by anti-
erythrocyte antibodies, leading to massive
absorption of hemoglobin by the renal
tubules. It may leads to renal failure and
collapse.
3. Algid malaria:
This syndrome is characterized by peripheral circulatory failure, rapid thready pulse with
low blood pressure and cold clammy skin.

Parasitology
Notes…
4
4. Septicemic malaria:
It is characterized by high continuous fever with dissemination of the parasite to various
organs, leading to multiorgan failure. Death occurs in 80% of the cases.
Chronic Complications of Malaria:
1.
Tropical Splenomegaly Syndrome (hyper-reactive malarial splenomegaly):
condition seen in people of malaria in endemic areas, it happens from abnormal
immunological response to
repeated malaria infection.
Tropical splenomegaly syndrome is characterized by high level of immunoglobulin M
(IgM), decreased C3 and massive splenomegaly.
2.
Quartan malarial nephropathy
It is a chronic complication seen with P. malariae (and possibly with other malarial
species). It occurs due to injury to the renal glomeruli by the immune complexes, resulting
in nephrotic syndrome.
Merozoite-induced Malaria
Natural malaria is sporozoite-induced, the infection being transmitted by sporozoites
introduced through the bite of vector mosquitoes. Injection of merozoites can lead to direct
infection of red cells and erythrocytic schizogony with clinical illness. Such merozoite-
induced malaria may occur in the following situations:
A. Transfusion malaria: Blood transfusion can accidentally transmit malaria; if the
donor is infected with malaria. The parasites may remain viable in blood bank for
1-2 weeks. Pre-erythrocytic schizogony and hypnozoites are absent. Relapse
does not occur and incubation period is short.
B. Congenital malaria: where the parasite is transmitted transplacentally from mother
to fetus.
C. Renal transplantation may lead to malaria if the donor had parasitemia.
D. Shared syringes among drug addicts may be responsible.
Mixed Infections Pathogenesis
In endemic areas it is not uncommon to find mixed infections with two or more species
of malaria parasites in the same individual. Mixed infection with P. vivax and P.
falciparum is the most common combination with a tendency for one or the other to
predominate. The clinical picture may be atypical with bouts of fever occurring daily.

Parasitology
Notes…
5
Laboratory Diagnosis
1. Microscopic examination
Peripheral Blood Smear: the simple and gold standard confirmatory test for the
detection of malarial parasites.
Thin smears:
The amount of blood in thin smear is about 1-
1.5 μL and spread over the
slide by a second slide held at an angle of 45° such that a tail is formed. Thins smears
are stained by Leishman, Giemsa, or Field’s stain. They are used for determining the
species of plasmodium.
Thick smears:
In a thick film, usually three drops of blood are spread over a small area.
The amount of blood in a thick smear is 3-
4 μL. Thick film is more suitable for rapid
detection of malarial parasite, particularly when they are few. thick film is more sensitive
than thin film because it concentrates 20- 30 layers of blood cells in a small area.
• Thin film is examined first at the tail end and if parasites are found, there is no need
for examining thick film.
• It is recommended that 200 oil immersion fields should be examined before the smears
are considered as negative.
2. Quantitative Buffy Coat, and immuno-Fluorescence microscope:
The nucleus of the parasite is detected by acridin-orange stains and appears as
fluorescing greenish-yellow against red back ground.
The advantage of this test is that it is faster. The disadvantage is that it is less
sensitive than thick film and is expensive.

Parasitology
Notes…
6
3. Serodiagnosis
it is not helpful in clinical diagnosis because it will not differentiate between an active and
past infection. The tests used are indirect hemagglutination (IHA), indirect fluorescent
antibody (IFA) test and enzyme-linked immunosorbent assay (ELISA).
4. Rapid antigen detection tests (RDTS) :
Rapid diagnostic test are based on the detection of antigens using
immunochromatographic methods.
5. Parasite-F test:
This test is based on detection of histidine rich protein-2 (HRP-2) antigen produced by the
asexual stages of P. falciparum expressed on the surface of red cells.
6. Culture of malaria parasite:
RPMl1640 Culture of plasmodia provides a source of the parasites for study of their
antigenic structure, in seroepidemiologic surveys, drug sensitivity tests .
7. Molecular Diagnosis:
nucleic acid probe and PCR.
Summary
Benign Malaria characterized by a triad of febrile paroxysm, anemia and
splenomegaly.
Cerebral malaria and Black-water fever are complication of P. falciparum malaria.
Thin and thick blood smears are the simplest and gold slandered methods for the
diagnosis of malaria.
