Parasitology
Notes…
1
Malaria Lec.4
Treatment of Uncomplicated Malaria
Positive P. vivax, P. ovale and P. malariae cases are treated with chloroquine 25
mg/kg divided over 3 days Or hydroxycholraquine.
Primaquine is used to eliminate the exo-erythrocytic phase (hypnozoites), so it is
used for prevention of relapse, primaquine is given in a dose of 0.25 mg/ kg daily
for 14 days.
In case of chloroquine resistance: Quinine is given in a dose of 600 mg 8 hourly
for 7 days along with doxycycline 100 mg/ day.
Treatment of Complicated (Falciparum) Malaria
Due to emergence of drug resistance of falciparum malaria, artemisinin-based
combination therapy (ACT) (artemisinin + sulfadoxine- pyrimethamine) should
be given to all microscopically positive falciparum cases for 3 days. This is
accompanied by single dose of primaquine 45 mg (0. 75 mg/kg) on day 2 as
gametocidal drug.
Immunity
Immunity in malaria could be of two types:
(1) innate immunity
(2) acquired immunity.
Innate Immunity :
This could be due to various factors:
1) Age of red blood cells: P. falciparum attacks RBCs of any age, P. vivax and P. ovale
attack the young RBCs and reticulocytes where as P. malariae attacks older RBCs
2) Duffy negative red blood cells: Duffy blood
group antigens present on RBC
membrane
act as receptors for P. vivax. So, people with Duffy negative RBCs (West
Africans Black people ) are
resistant to vivax malaria.
N
eed S
om
e H
el
p?

Parasitology
Notes…
2
3) Nature of hemoglobin: Sickle cell disease, hemoglobin C and E, fetal hemoglobin
and
thalassemia hemoglobin are resistance to falciparum malaria
4) Red blood cells with glucose-6-phosphate
dehydrogenase (G6PD) deficiency
are
resistant to falciparum malaria.
5) Human leukocyte antigen-HLA-B53: protect from cerebral malaria.
6) nutritional status: Patients with iron deficiency are relatively resistant to malaria.
7) Pregnancy: Falciparum malaria is more severe in pregnancy, particularly in
primigravida and may be enhanced by iron supplementation.
8) Splenectomy: The spleen appears to play an important role in immunity against
malaria. Splenectomy enhances susceptibility to malaria.
Acquired immunity
I.
Humoral immunity: Circulating antibodies against asexual forms give protection
by inhibiting red cell invasion and antibodies against sexual forms reduce
transmission of malaria parasite.
II.
Cellular immunity: Sensitized T cells release cytokines that regulate macrophage
activation and stimulate B cells to produce antibodies. The activated macrophages
inside liver, spleen and bone marrow phagocytose both parasitized and non-
parasitized RBCs.
Protective immunity against malaria is species specific, stage specific and strain
specific.
Immune defense of the host is sufficient to resist further infection but insufficient to
destroy the parasite. Immunity lasts till the original infection remains active and
prevents further infection. This is called as infection immunity or premunition or
concomitant immunity or incomplete immunity.
Prevention and Control
1. Chemoprophylaxis
For travelers visiting endemic areas, chemoprophylaxis provides effective protection. The
drugs recommended are proguanil, chloroquine or mefloquine weekly or doxycycline
daily. Prophylaxis should begin 1 week before travelling and be continued while in the
endemic area and for 4
–6 weeks after departure from endemic area.
2. Vector Control Strategies
(a) Insecticide residual spraying (IRS): The spraying of
the indoor surfaces of house with residual insecticides such
as DDT, malathion.
(b) Insecticide treated bed nets (ITN)
Parasitology
Notes…
3
(c) Use of repellants, protective clothing, and screening of
house.
(d) Anti-larval Measures: oiling collection of standing water or
dusting them with Paris green.
3.Malaria Vaccine
i.
SPf66 (a cocktail of four antigens, three asexual blood stage antigens + sporozoite
of Pf) was tested extensively in endemic areas in the 1990s, but clinical trials
showed it to be insufficiently effective.
ii.
Merozoite surface protein 1 (MSP 1), MSP2, MSP 13 and ring-infected
erythrocyte surface antigens (RESAs) have also been in insufficient on their own.
iii.
RTS,S/ASO1 (mosquirix): 2021 was engineered using genes from the outer
protein of P. falciparam and a portion of hepatitis B virus, plus a chemical adjuvant
(ASOl) to boost immune response.
➢ Mosquirix,is not just a first for malaria
— it is the first developed for any parasitic
disease.
➢ The World Health Organization (WHO) is recommending widespread use of the
RTS,S/AS01 (RTS,S) malaria vaccine in 2021 among children in sub-Saharan
Africa and in other regions with moderate to high P. falciparum malaria
transmission.
➢ RTS,S/AS01 malaria vaccine should be provided in a schedule of 4 doses in
children from 5 months of age for the reduction of malaria disease and burden.
➢ Mosquirix prevents 4 in 10 cases of malaria.
Malaria in Iraq
At 1957 malaria constituted about 20 % of infectious disease that was common in
Iraq at that period. Malaria is common in parts of north and south of Iraq where
Marshes are common.
Parasitology
Notes…
4
At 1994 – 1995 an outbreak occurred and about 100 thousand cases were reported.
The last 2 malaria cases were reported in Iraq in 2008.
In 2014, 2 imported cases of malaria were diagnosed in Iraq among non-national
individuals.
In 2015, another 2 imported cases were reported; one was national and one non-
national.
In 2018, another imported cases were reported among non-national individual.
According to the latest WHO data published in 2018 Malaria Deaths in Iraq reached
0.00% of total deaths.
Currently, Iraq is developing a national strategy of malaria for 2016–2020.
The main priorities for keeping the country malaria-free include:
1. Strengthening disease surveillance.
2. Use of appropriate vector control interventions when needed.
3. Provision of free diagnostics and antimalarial medicines, including rapid diagnostic
tests for areas where malaria microscopy of assured quality is not available.
4. Human resource development, particularly training courses for physicians and
laboratory technicians on malaria treatment and diagnosis.
BABESIA SPECIES
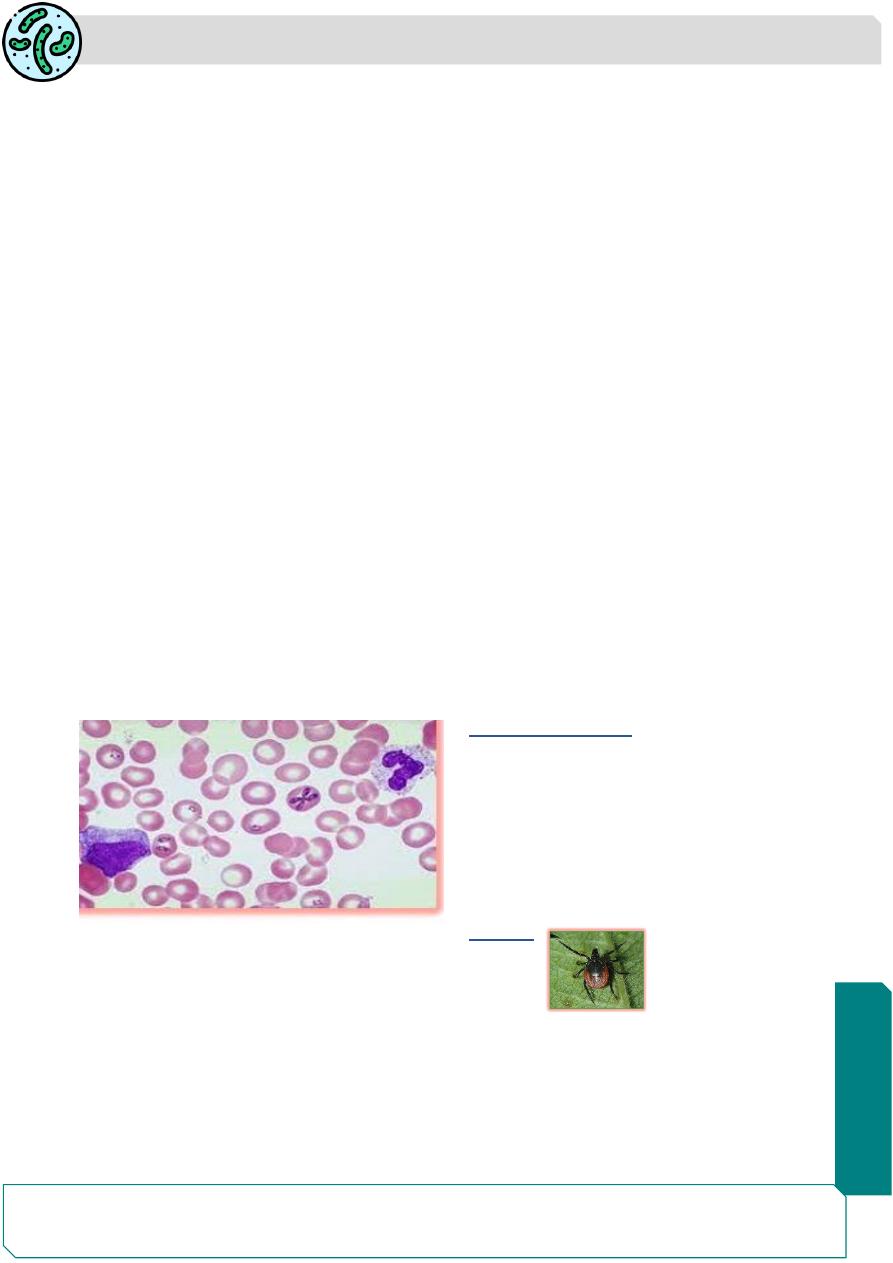
Babesia is intra-erythrocytic sporozoan parasites that morphologically resemble
Plasmodium and cause tick-borne malaria-like illness.
The parasite is present in erythrocytes and resembles the ring stage of P.
falciparum.
CLASSIFICATION
Order: Piroplasmida
Family: Babesiidae
Species: Medically important Babesia
species are:
• B. microti (rodent strain)
• B bovis ( cattle strain)
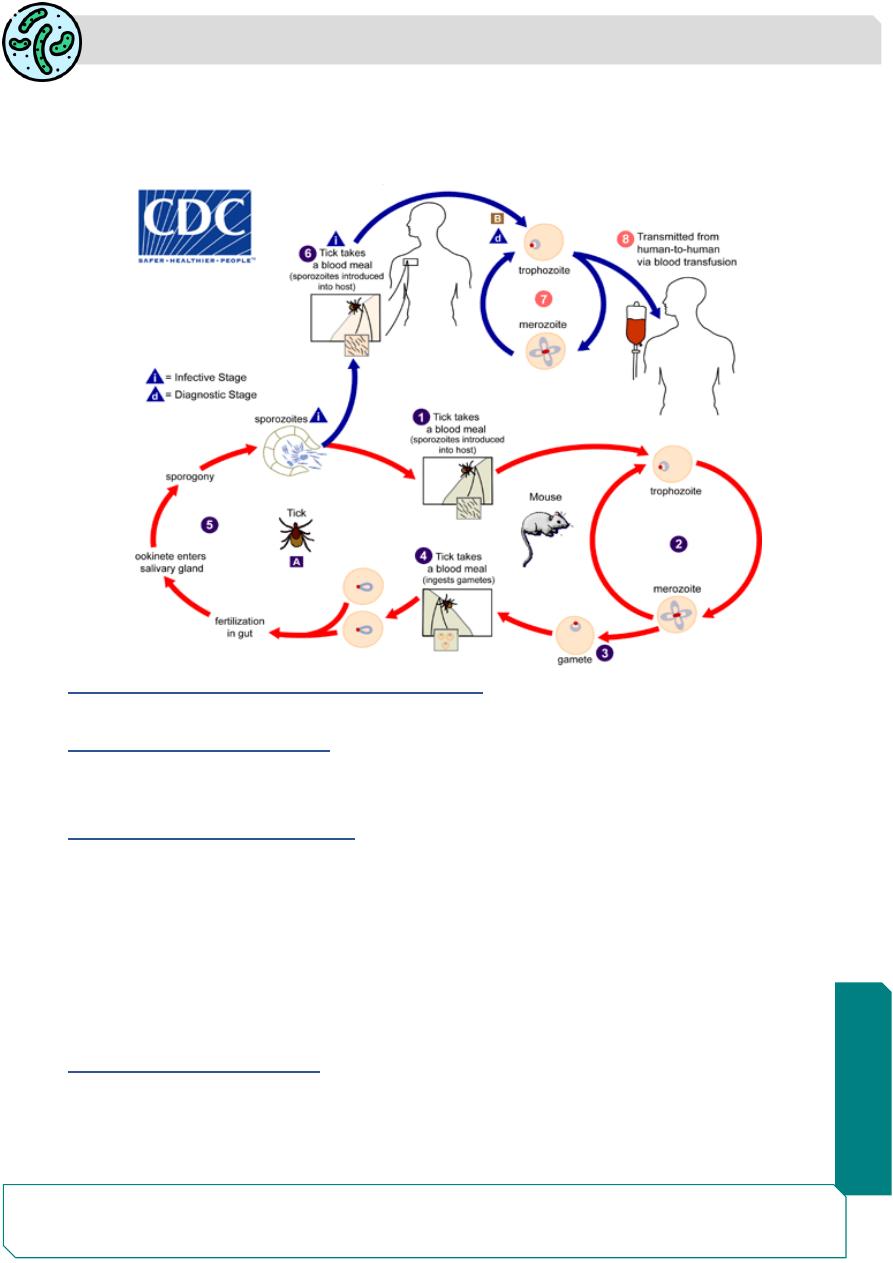
LIFE CYCLE
Definitive Host: Ixodid ticks.
Intermediate Host: Man or other mammals.
Infective Form: Sporozoites are the infective form for humans.
Mode of Transmission: Infection in vertebrate occurs through bite of the of Ixodid ticks.
➢ Sporozoites in the salivary glands of tick are introduced into man through the bite
of infected ticks.
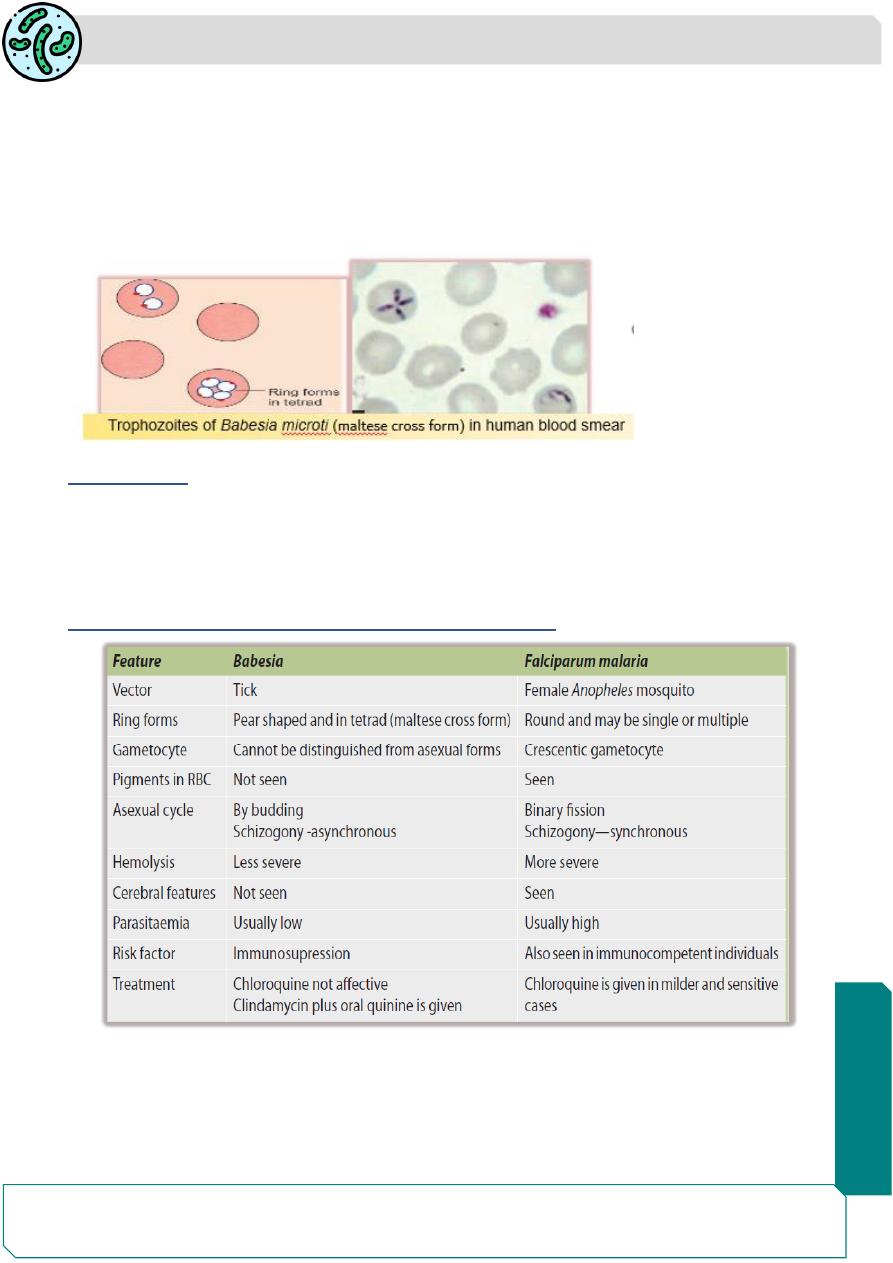
Sporozoites invade the RBCs and multiply asexually to form trophozoites (ring
forms in tetrad called as Maltese cross form
(.
Parasitology
Notes…
5
Newly formed trophozoites are released by rupturing erythrocytes and invade new
erythrocytes.
Ticks become infected by feeding the host blood, sporozoites formed in the ticks
and infect human.
PATHOGENICITY AND CLINICAL FEATURES
The incubation period varies from 1 to 6 weeks.
Mild Babesia microti illness:
It is characterized by malaise, fatigue, weakness and fever. Later on the patient develops
chills, sweats, headache, myalgia, anorexia, dry cough, arthralgia and nausea.
Severe Babesia microti illness:
Seen when parasitemia exceeds more than 4%.
Predisposing factors include: more than 50 years of age, male, splenectomy,
HIV/AIDS, malignancy, and immunosuppression.
Patient presents as severe anemia (hemoglobin level < 10 g/dL).
Complications may occur like: acute respiratory distress syndrome, disseminated
intravascular coagulation, congestive heart failure, renal failure and splenic infarcts
and rupture.
LABORATORY DIAGNOSIS
1) Peripheral Blood microscopy: Diagnostic feature is the demonstration of two or four
rings inside the RBCs (called as maltese cross forms) in the Giemsa stained thick
and thin blood smear. It is often confused with the multiple ring forms of P.
Parasitology
Notes…
6
falciparum. But can be differentiated by lack of pigments, lack of crescentic
gametocytes, and the presence of pear shaped rings.
2) Serology: It is useful to confirm the diagnosis: Indirect fluorescent antibody (IFA)
test.
3) Polymerase Chain Reaction.
4) Animal inoculation.
TREATMENT
B. microti infection is mild and self-limiting.
In acute severe cases chemotherapy is required:
Atovaquone along with azithromycin for a period of 7- 10 days is effective.
Alternatively, clindamycin along with quinine may be given intravenously.
Differences between Babesia and falciparum malaria
Summary
P. vivax, P. ovale and P. malariae cases are treated with chloroquine.
artemisinin-based combination therapy is used to treat P. falciparum malaria.
Babesia is intra-erythrocytic sporozoan parasites that morphologically resemble
Plasmodium.
