College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 1
Visceral leishmaniasis (Black fever, Dumdum fever)
Objectives:
Visceral leishmaniasis
o Have an idea about history of Visceral leishmaniasis
o Pathogenesis
o Clinical features
o Diagnosis
o Treatment
o Prevention and control
Leishmaniasis in Iraq
In 1900 Sir William Leishman from Scotland discovered Leishman Donavani bodies in a
postmortem spleen smear of a soldier who died due to fever at Dum Dum, India.
The disease was known locally as Dum-Dum fever or Kal azar.
Sir William Leishman
An Irish physician Charles Donavan also recognized the symptoms in other Kala-azar patients
and published his discovery a few weeks after examining the parasite using Leishman
,
s stain,
So the parasite named Leishmania and the amastigote forms named Leishman Dnoavan bodies.
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 2
Pathogeneses:
L. donovani causes VL or kala-azar.
• Kala-azar is a reticuloendotheliosis resulting from the invasion of reticuloendothelial
system by L. donovani.
• The parasitized macrophages disseminate the infection to all parts of the body.
• Three major surface membrane proteins of Leishmania: (1) gp63, (2) lipophosphoglycan
(LPG) and (3) glycosylphosphatidyl inositols (GPIs) give protection against hydrolytic
enzymes of macrophage phagolysosome.
• In the spleen, liver and particularly bone marrow, the amastigotes multiply enormously
in the macrophages leading to "blockade" of the reticuloendothelial system, that causes
marked proliferation and destruction of reticuloendothelia tissue in these organs.
Splenic changes:
• The spleen is the most affected organ.
• It is grossly enlarged and the capsule is thickened due to perisplenitis.
• Spleen is soft, friable and easily ruptures due to absence of fibrosis.
• The cut section is red or chocolate in color due to the dilated and engorged vascular
spaces.
• Microscopically, the reticulum cells are greatly increased in numbers and are loaded
with LD bodies.
• Lymphocytic infiltration is scanty, but plasma cells are numerous
Liver changes:
• The liver is enlarged.
• The Kupffer cells and vascular endothelial cells are heavily parasitized, but the
hepatocytes are not affected.
• Prothrombin production is commonly decreased.
• The sinusoidal capillaries are dilated and engorged.
• Some degree of fatty degeneration is seen.
• The cut surface may show a "nutmeg" appearance.
Nutmeg
Bone marrow and blood:
• The bone marrow is heavily infiltrated with parasirized macrophages, which may crowd
the hematopoielic tissues.
• Severe anemia with haemoglobin levels of 5-10 g/Dl may occur in kala-azar, as a result
of:
Infiltration of the bone marrow and marrow suppression by cytokines.
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 3
The increased destruction of erythrocytes due to hypersplenism.
Autoantibodies to red cells may contribute to hemolysis .
Hemorrage
• Auto immune Leukopenia , neutropenia and thrombocytopenia
• Pancytopenia observed in kala-azar.
Ecological types:
Indian visceral leishmaniasis: Caused by L. donovani
• It produces the anthroponotic disease kala-azar and its sequel Post-kala-azar dermal
leishmaniasis (PKDL).
• The disease is not zoonotic; human beings are the only host and reservoir.
• Vector is the sandfly, P. argentipes.
Mediterranean leishmaniasis: Middle Eastern
• Leishmaniasis caused by L. donovani infantum affecting mostly young children.
• It is a zoonotic disease; the reservoir being dogs and wild canines .
• Vectors are P. pernicious and P. papatasii.
American (New World) visceral leishmaniasis: Caused by L. chagasi.
• It presents in most parts of Latin America and resembles the disease caused by L.
infantum.
• The main vector is L. longipalpis
Clinical features of kala-azar:
• The onset is typically insidious.
• High-grade fever which has twice daily spikes or intermittent or less commonly
continuous.
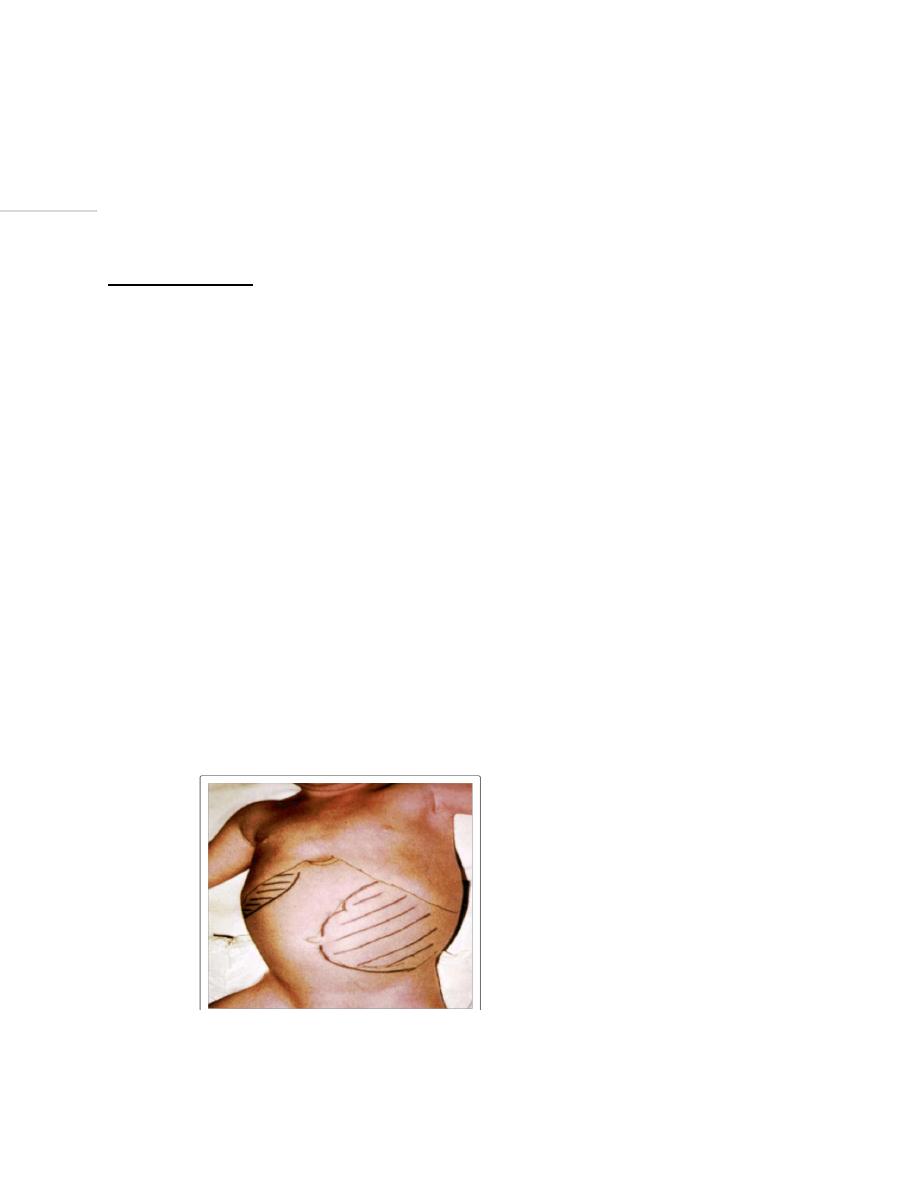
• Progressive, massive, Soft, non tender splenomegaly that starts early.
• Moderate hepatomegaly
Hepato splenomegally in patient with Kala azar. (1)
• Lymphadenopathy is common in most endemic areas.

College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 4
• Skin becomes dry, rough and darkly pigmented (hence, the name kala-azar).
• The hair becomes thin and brittle.
• Cachexia , emaciation and loss of weight .
• Hematological abnormalities:
1. Anemia always presents and is usually severe
2. Leukopenia
3. Thrombocytopenia is associated with epistaxis, gum bleeding gastrointestinal (GI)
bleeding.
4. Pancytopenia
• Ascites and oedema may occur due to hypo albuminemia.
• Renal impairment is also common.
• Secondary infections such as herpes, measles, pneumonia, tuberculosis, bacillary
dysentery may occur.
• Most untreated patients die in about 2 years.
Diagnosis:
Microscopic examination:
• In Kala azar :Detection of amastigotes (LD bodies(Leishman-Donovan) in Giemsa stained
smear of bone marrow, lymph nodes or liver.
• In cutaneous or mucocutaneous leishmaniasis: The amastigotes are found in the
scraping of cutaneous or mucosal ulcerations (especially scraping of the borders) as well
as in non-ulcerated lesions.
• Biopsy should be obtained from the active border of the skin and mucous lesions.
Examination of smear:
• It reveals the amastigote stage in free form or inside monocytes or less frequently in
polymorphonuclear cells.
• Number of amastigotes ranges from 2 to 20 in a single cell.
Amastigote stage in smear(2)
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 5
Cultivation of aspirates:
NNN (Novy- MacNeal-Nicolle) medium:
• Cultured in an incubator for a week.
• The incubation is under anaerobic conditions at 24-26
o
C
• Promastigotes are the parasite forms that grow in culture .
Cell culture of monocytes using RPMI-1640 or Medium-199
• Incubation at 37
o
C
• The stage found will be amastigotes.
Note : Both techniques (microscopic exam and culture) have a sensitivity of 85%.
Serology :
Detection of specific anti-leishmanial antibodies:
• IFAT (indirect immunofluorescent antibody test)
• DAT (Direct agglutination test)
• ELISA (enzyme linked immunosorbent assay): Determination of serum anti-Leishmania
Abs used with a sensitivity of 90 to 100%.
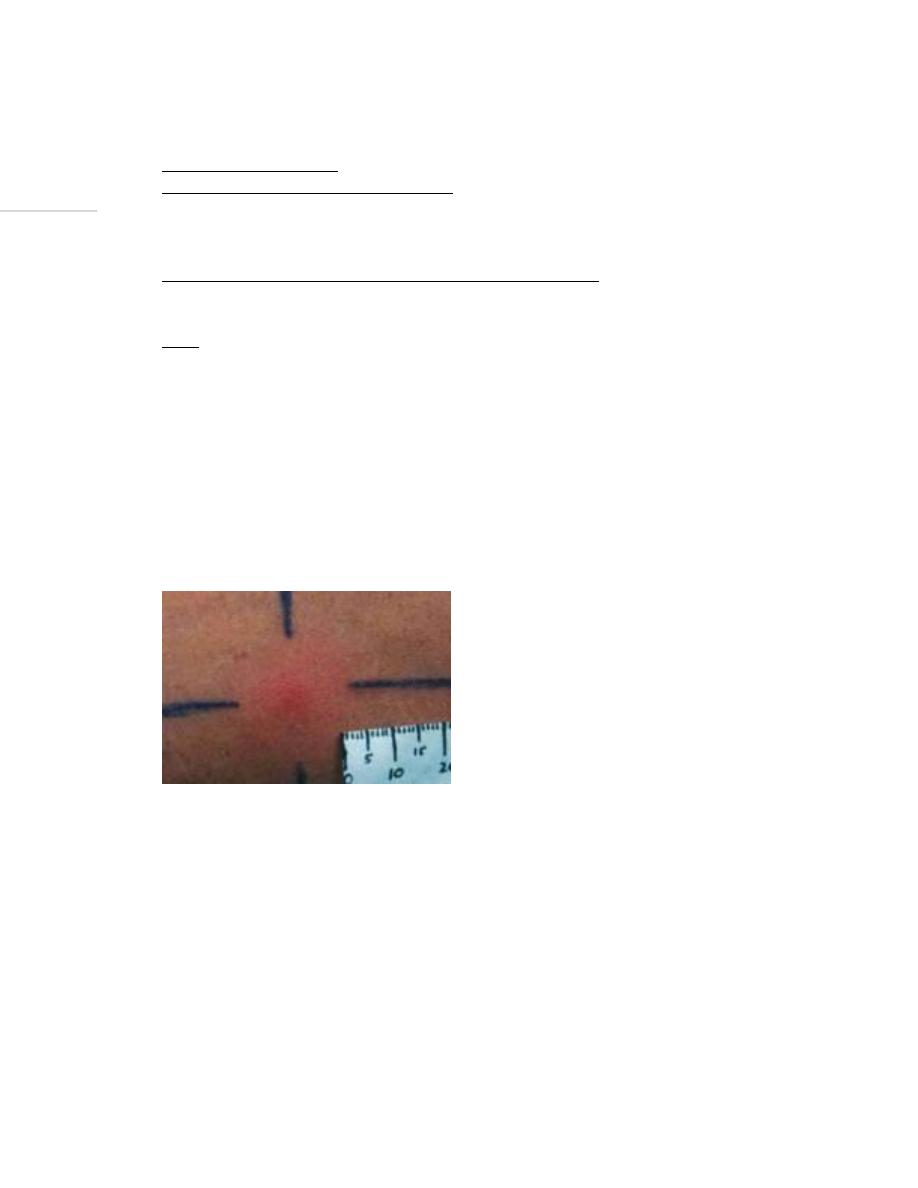
Leishmanin skin test (Montenegro test):
The Montenegro skin test is a tool for determining the degree of exposure and
immunity to the parasite depending on development of delayed hypersensitivity(DHSR).
Intradermal injection at forearm by 0.1 ml suspension of killed promasitigote.
Positive result is indicated by an induration of 5mm or more in 48-72 hours.
A positive leishman skin test(3)
It is positive in cutaneous leishmaniasis.
A positive test supports the diagnosis especially when the patient does not live in
endemic areas, but a negative test does not exclude it.
In active visceral leishmaniasis, the test is almost always negative and a positive result
usually appears 2–24 months after clinical recovery. Thus this test has no role in the
diagnosis of the acute disease.
Molecular method: PCR polymerase chain reaction is the most sensitive and specific
diagnostic method.
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 6
Treatment:
• In general, all clinically manifest cases of visceral leishmaniasis and mucosal
leishmaniasis should be treated.
• Not all cases of cutaneous leishmaniasis require treatment.
Some drugs used for treatment:
1- Sodium stibogluconate (Pentostam): highly effective therapy for visceral
leishmaniasis.
2- Amphotericine B approved for treatment of visceral leishmaniasis.
3. other treatments as Pentamidine and paromomycin also used.
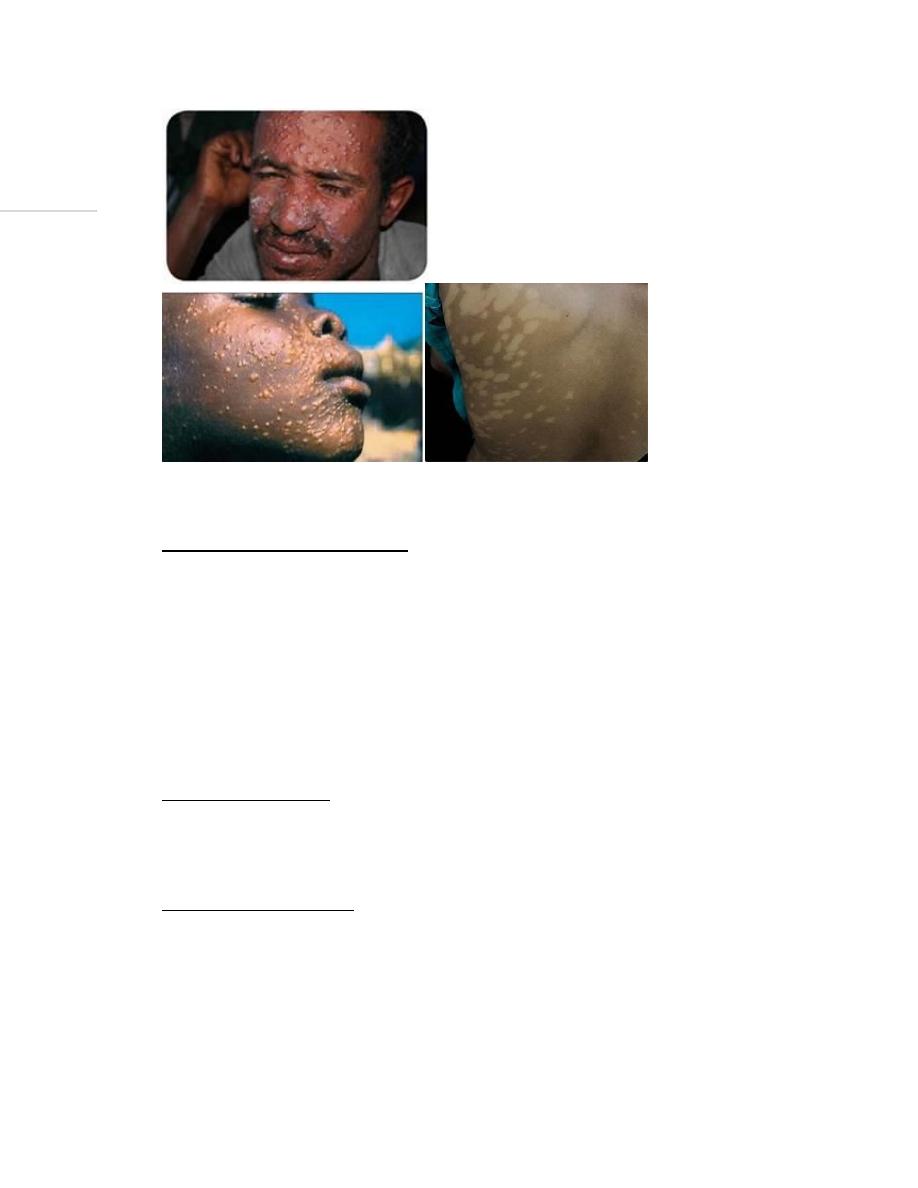
Post-kala-azar dermal leishmaniasis
PKDL
Post-kala-azar dermal leishmaniasis (PKDL) is a complication of visceral leishmaniasis
(VL) in areas where Leishmania donovani is endemic.
It is characterized by:
• Hypopigmented macular rash
• Maculopapular rash
• Nodular rash.
• It usually occurs in patients who have recovered from VL .
• It usually appears 6 months to 1 or more years after apparent cure of the disease but
may occur earlier or even concurrently with visceral leishmaniasis.
• It has important role in maintaining and transmission of the disease acting as a reservoir
for parasites.
Diagnosis of post-kala-azar dermal leishmaniasis:
• The nodular lesions are biopsied and amastigote forms are demonstrated in stained
sections.
• The biopsy material can be cultured or animal inoculation can be done.
• lmmunodiagnosis has no role in the diagnosis of PKDL.
Treatment of post-kala-azar dermal leishmaniasis:
• Liposomal amphotericin-8 (AmBisome) or sodium stibogluconate (SSG).
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 7
Maculopapular and anodular PKDL(4)
Prevention of leishmaniasis:
• Prevention involves protection from sandfly bites by using netting, window screens,
protective clothing, and insect repellents.
Leishmaniasis in Iraq:
Leishmaniasis is widespread in Iraq.
• Cutaneous leishmaniasis accounts for 2/3 of cases and visceral leishmaniasis accounts
for 1/3.
• The peak transmission season typically begins in May.
• Maximum number of cases of Leishmaniasis were reported in 1992 and it was 45.5
cases per 100,000 of population
Visceral leishmaniasis:
• Is generally found in central and southeastern parts of Iraq.
• L. donovani and L. Infantum are the causative agents, with 90% of the cases reported in
children under five years of age.
• It spreads through the Phlebotomus alexandri species of sandfly.
Cutaneous Leishmaniasis:
• Is quite prevalent in the entire country.
• Mainly caused by L. major and L. tropica.
• It is spread by Phlebotomus sergenti and P. papatasi species of sandfly.
Hypo pigmented macular PKDL (4)
College of Medicine University of Mosul /Department of: Microbiology
Subject: Parasitology Stage: 3
rd
2021-2022
Lecturer: Dr.Ahmed Alharbi Date: 22/11/2021 No.3
Page | 8
Summary of leishmaniasis:
Leishmania parasite is a hemoflagellate
Transmitted by Sandfly
Causes cutaneous, mucocutaneous and visceral diseases
Diagnosed by microscopy, culture, serology or by molecular techniques
Treatment is important for mucocutaneous, visceral and severe cutaneous
diseases.
Prevention by preventing sandfly from taking blood meal from victims.
References:
1. Mans, Dennis & Kent, Alida & Hu, Ricardo & Schallig, Henk. (2017). Epidemiological,
biological and clinical aspects of leishmaniasis with special emphasis on busi yasi in
Suriname. J Clin Exp Dermatol Res. 8:2. 10.4172/2155-9554.1000388.
Encyclopedia of Microbiology (Third Edition)
, 2009
3. Escholarship.org
4. WHO, Drugline.org and Parasites and vectors.biomedcentral.com
5. BURTON J. Bogitsh,Clint E. Carter, and Thomas N. Oeltmann, 2013, Human parasitology
4
th
edition, USA and UK, Elsevier.
6. CDC.gov
7. Paniker J CK , 2018, Paniker
,
s textbook of medical parasitology, 8
th
edition, Newdelhi,
London , Panama, JAYPEE.
8. World health organisation. Photos on leishmaniasis
9. Zeibig A. Elizabeth, 2013, Clinical parasitology, USA, Elsevier
10. Garcia Lynne.Diagnostic medical parasitology.Washington DC.ASM Press.5
th
edition.2007
