Parasitology
Notes…
1
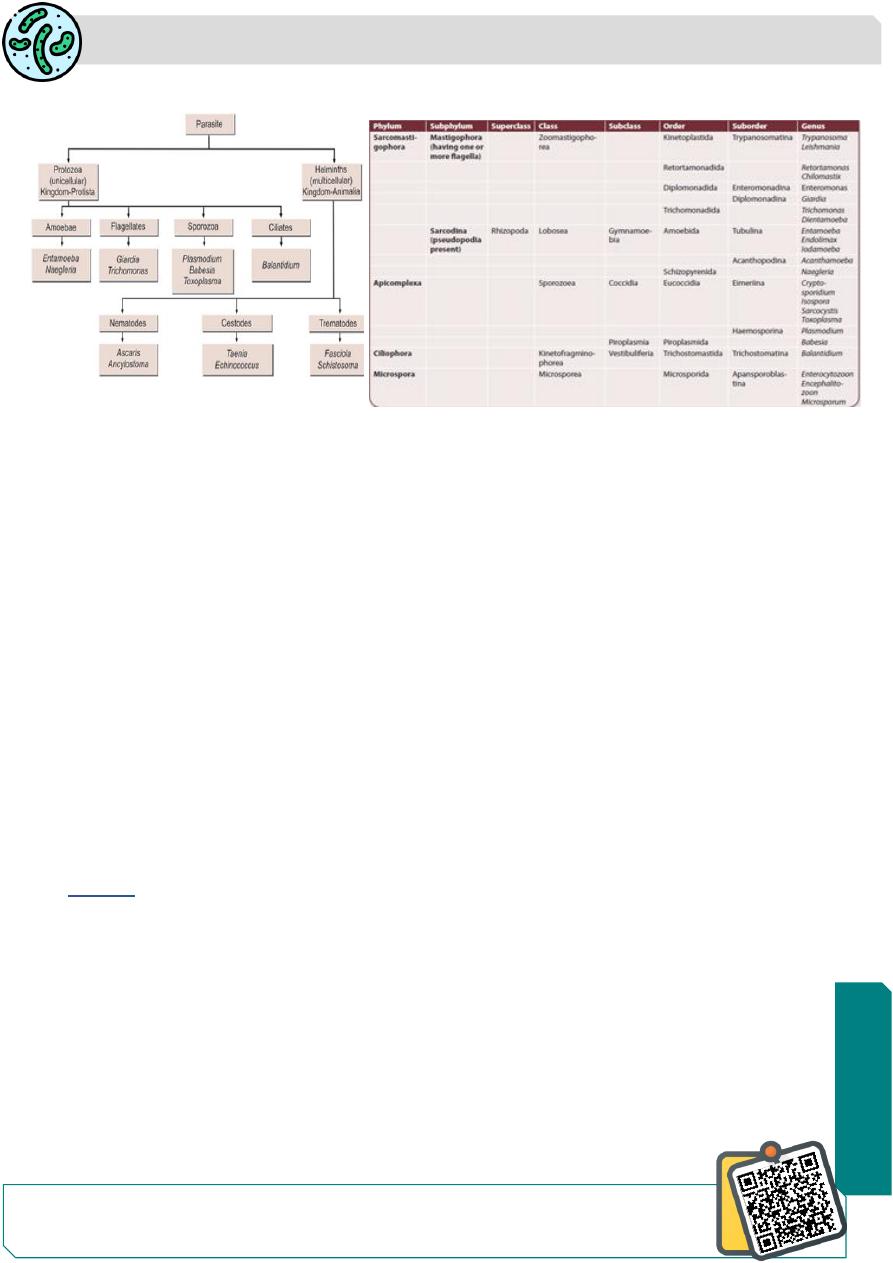
Toxoplasma
The coccidia are unicellular protozoa and belong to the
Phylum Apicomplexa Class sporazoea subclass cocccidia
They live intracellularly, at least during a part of their life cycle and at some stage in their
life cycle, they possess a structure called the
apical complex
.
All coccidian have a sexual sporogonic phase and an asexual schizogonic phase.
Many of them also show an alteration of hosts; a
definitive host and an intermediate host
Toxoplasma Gondii
Toxoplasma gondii is an obligate intracellular coccidian parasite.
Toxoplasmosis is a zoonotic infection of humans and animals, caused by the
opportunistic protozoan (Toxoplasma gondii), a parasite belonging
phylum Apicomplexa
Class sporazoea
subclass cocccidia .
History
The first described in 1908 by Nicolle and Manceaux in a small North
American rodent
called gondii.
Its importance as a human pathogen was recognized much later, when Janku in 1923
observed the cyst in the retina of a child with hydrocephalus
The discovery of the life cycle of the parasite has been completed only in 1970 when
domestic cats were recognized as the definitive hosts.
In 1980 T.gondii was regarded as important opportunistic infection in immune
compromised subjects
N
eed
S
ome
H
el
p?

Parasitology
Notes…
2
The name Toxoplasma is derived from the Greek word ‘Toxon’ meaning arc or brow
referring to the curved shape of the trophozoite
Geographic Distribution:
toxoplasmosis is one of the most common human infections throughout the world.
It has been estimated that 30% of the world population has been infected .
prevalence depends on the locale and the age of the population.
Generally, hot arid climatic conditions are associated with a low prevalence of infection.
In the United States and most European countries, the seroprevalence increases with age
in the United States, 5
–30% of individuals 10–20 years old
and 10
–65% of those >50 years old .
A high prevalence of infection in China 15% , 20% in UK
in France(50-75%) has been related to a preference for eating raw or undercooked
meat.
while a high prevalence in Central America has been related to the frequency of stray cats
in a climate favoring survival of oocysts and soil exposure
prevalence of T. gondii total Abs among young women attending the public health
laboratory in Mosul was around 50% with only 10% positive IgM anti-Toxoplasma Abs.
48% of Patients with Leukemia in Mosul showed presence of anti-T.gondii Abs in their
sera and 28% of them were positive for IgM Abs.
seroprevalence in Ramadi show (wives 30.7%), while 13.1% in husbands only.
in Duhok showed 59% of pregnant ladies with bad obstetric history (abortion, or dead
fetus)
anti- Toxoplasma Abs by latex agglutination test and IgM Abs were found in 1% of them
Morphology
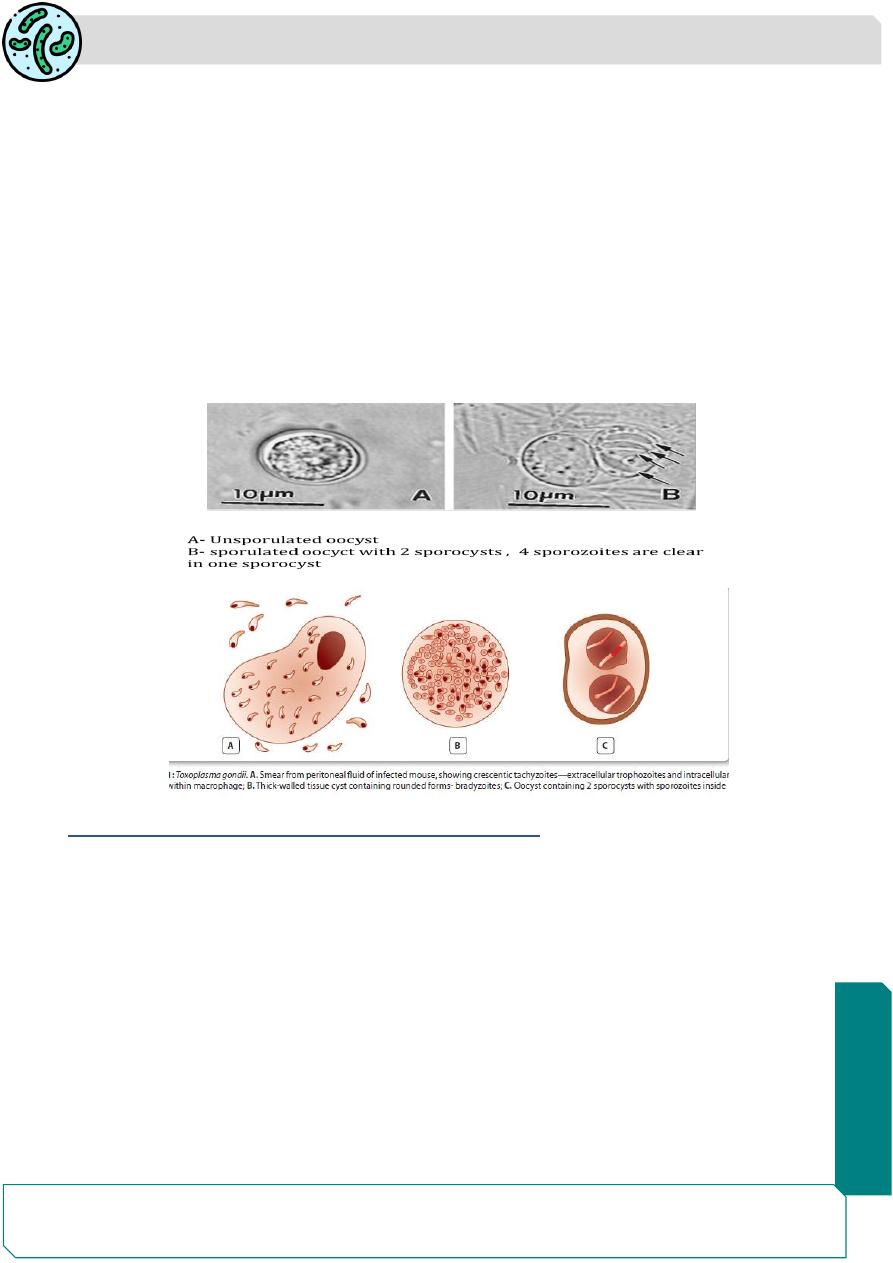
T. gondii occurs in 3 forms :
€ Trophozoite
€ Tissue cyst
€ Oocyst.
The trophozoite and tissue cyst represent stages in asexual
multiplication (schizogony),
while the the oocyst is formed by sexual reproduction (gmaetogony or sporogony).

Parasitology
Notes…
3
All 3 forms occur in domestic cats and other felines, which are the definitive hosts and
support both schizogony and gametogony.
Only the asexual forms, trophozoites and tissue cysts are present in other animals,
including humans and birds, which are the intermediate hosts.
All the 3 forms are infectious to man.
Trophozoites (Tachyzoites)
The trophozoite is crescent shaped, 3
–7 μm in length with one end
pointed and the other end rounded
The nucleus is ovoid and is situated at the blunt end of the parasite
Electron microscopy reveals an apical complex at the pointed end
The trophzoite stains well with Giemsa stain, the cytoplasm
appearing blue and the nucleus red .
The actively multiplying trophozoite is seen intracellularly in various tissues during early
acute infection
Extracellular trophozoites can also be seen in impression smears
It can invade any nucleated cell and replicate within cytoplasmic vacuoles by a process
called endogony (internal budding), where in 2 daughter trophozites are formed, each
surrounded by a membrane, while still within the parent cell.
When the host cell becomes distended with the parasite, it, releasing
disintegrates,
releasing the trophozoites that infect other cells
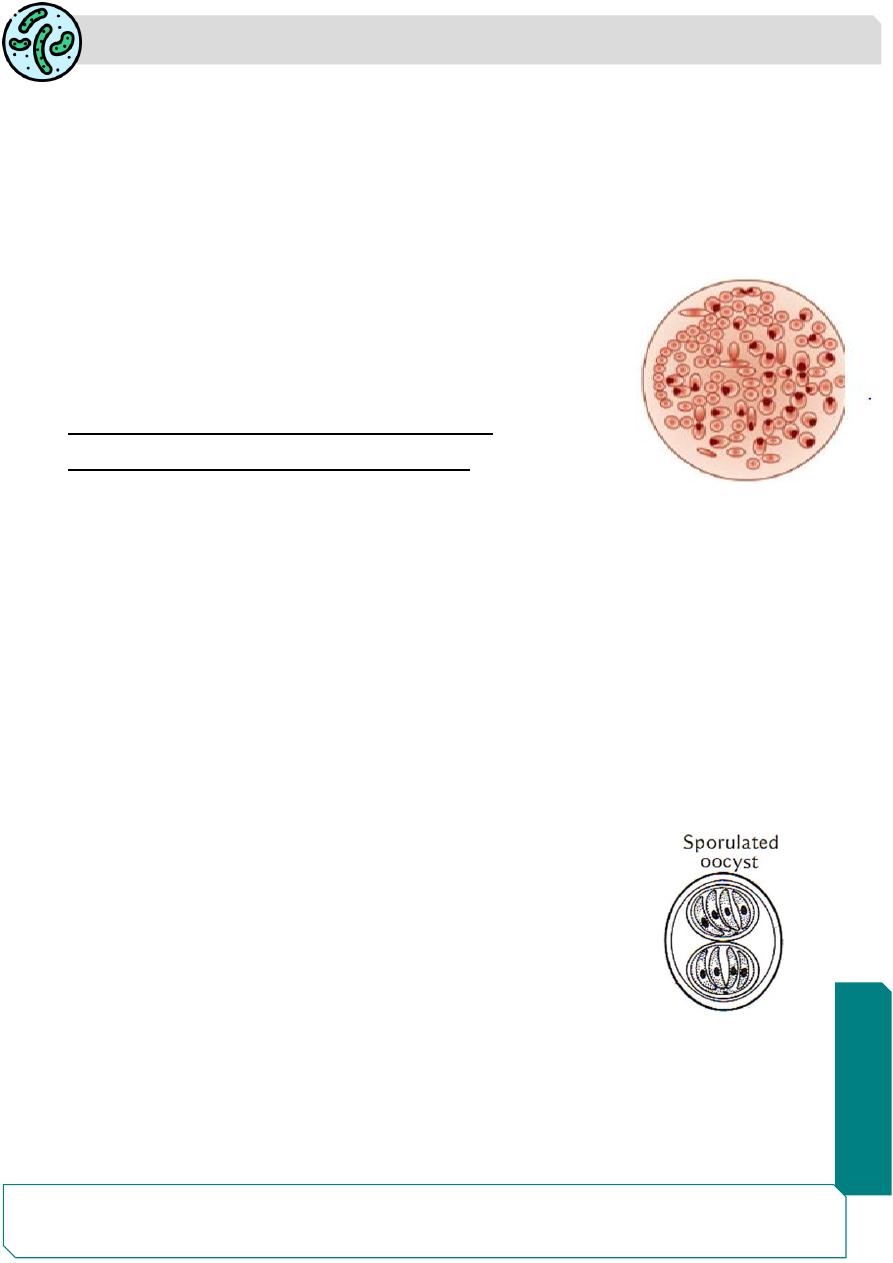
During acute infection, the proliferating trophozoites within host cell may appear rounded
and enclosed by the host cell membrane. This is, called pseudocyst or colony and can be
differentiated from tissue cysts by staining reactions.
The rapidly proliferating trophozoites in acute infection are called tachyzoites
The trophozoites are susceptible to drying, freezethawing
Parasitology
Notes…
4
Tissue cyst (bradyzoite)
Tissue cysts are the resting form of the parasite.
They are found during chronic stage of the infection and can be found in the brain (most
common site), skeletal muscles, and various other organs.
The tissue cyst is round or oval, 10
–20 μm in size and contains numerous bradyzoites.
The cyst wall is eosionophilic stains weakly and the parasites inside are stained deeply
with silver,
In contrast to the pseudocyst with periodic acid Schiff (PAS) stain,
The slowly multiplying parasites within the cyst are called
bradyzoite
Bradyzoites: Similar to tachyzoites in morphology
Cysts remain viable in tissue for several years.
In immunocompetent hosts, the cysts remain silent, but in the immunodeficient subjects,
they may get reactivated, leading to clinical disease.
when the raw or undercooked meat containing the cysts is eaten, infection occurs.
The cyst wall is disrupted by peptic or tryptic digestion and the released parasites initiate
infection by invading intestinal epithelial cells.
They reach various tissues and organs through blood and lymphatic dissemination.
Cysts are susceptible to freezing, and thawing, and heat above 60°C.
Oocyst
Oocysts develop only in definitive hosts
– in the intestine of cats and other felines but not
in humans.
It is oval in shape and measures 10
–12 μm in diameter.
Each cyst is surrounded by a thick resistant wall.
The oocysts is formed by sexual reproduction (gametogony).
Cats shed millions of oocysts per day in feces for about 2 weeks
during the primary infection.
The freshly passed oocyst is not infectious.
They undergo sporulation in the soil with formation of 2 sporocysts, each containing 4
sporozoites with in several days to several weeks the sporulated oocyst is become
infective.
Parasitology
Notes…
5
Oocyst is very resistant to environmental conditons and can remain infective in soil for
about 3 years
When the infective oocyst is ingested, it releases sporozoites in the intestine, which
initiates infection. The incubation period ranges from 5- 24 days. If the cat ingest infective
oocyst and initiate intestinal infection, the animal will pass oocyst within 21-24 days
If the cat feed in its tissue cysts, the oocyst will appear in the cat's feces within 5- 10 days
During acute infections, cats excrete unsporulated oocysts (noninfectious) in their feces
,after several days to several weeks, depending on environmental conditions.
the oocysts sporulate and become infectious. Under favorable conditions (i.e., in warm,
moist soil)
Risk factors for T. gondii infection in human being:
1-having poor hand hygiene.
2- seropositive cats in farming areas
3-cleaning the cat litter box .
4- eating raw or undercooked pork, beef.
5- gardening .
6- eating raw or unwashed vegetables or fruits.
7- contact with soil .
8-infrequent washing of kitchen knifes .
9-butchers do not always wear gloves during work when handling raw meat

Parasitology
Notes…
6
Source of infection
Domestic cats : reservoir source of infection.
Cat feces is the chief source of infection.
All the 3 forms are infectious to man (Tachyzoite, mature oocyst and tissue cyst are the
infective stage).
Transmission:
T. gondii infection usually is transmitted from infected cat and domestic animals to man
(zooontic infection).
There are several transmission ways
1-Oral transmission:
T. gondii infection is acquired by eating raw or undercooked meat
(chicken, pork and goat meat) containing the tissue cyst or ingesting food ,water
vegetables and fruits contaminated with mature oocysts form in cat feces
2-Congenital transmission:
the infection is transmitted from the infected pregnant
mother to the fetus, by the tachyzoits passing through the placenta.
The prevalence of T. gondii infection in pregnant women 25% in China, Austra (35%) ,
France (43%) and Brazil (53%)
3-Other modes of transmission:
laboratory infection is caused by accidental self-
inoculation of tachyzoites, It is less common.
The infection may be transmitted by blood transfusion, unpasteurised milk, and organ
transplantation

Parasitology
Notes…
7
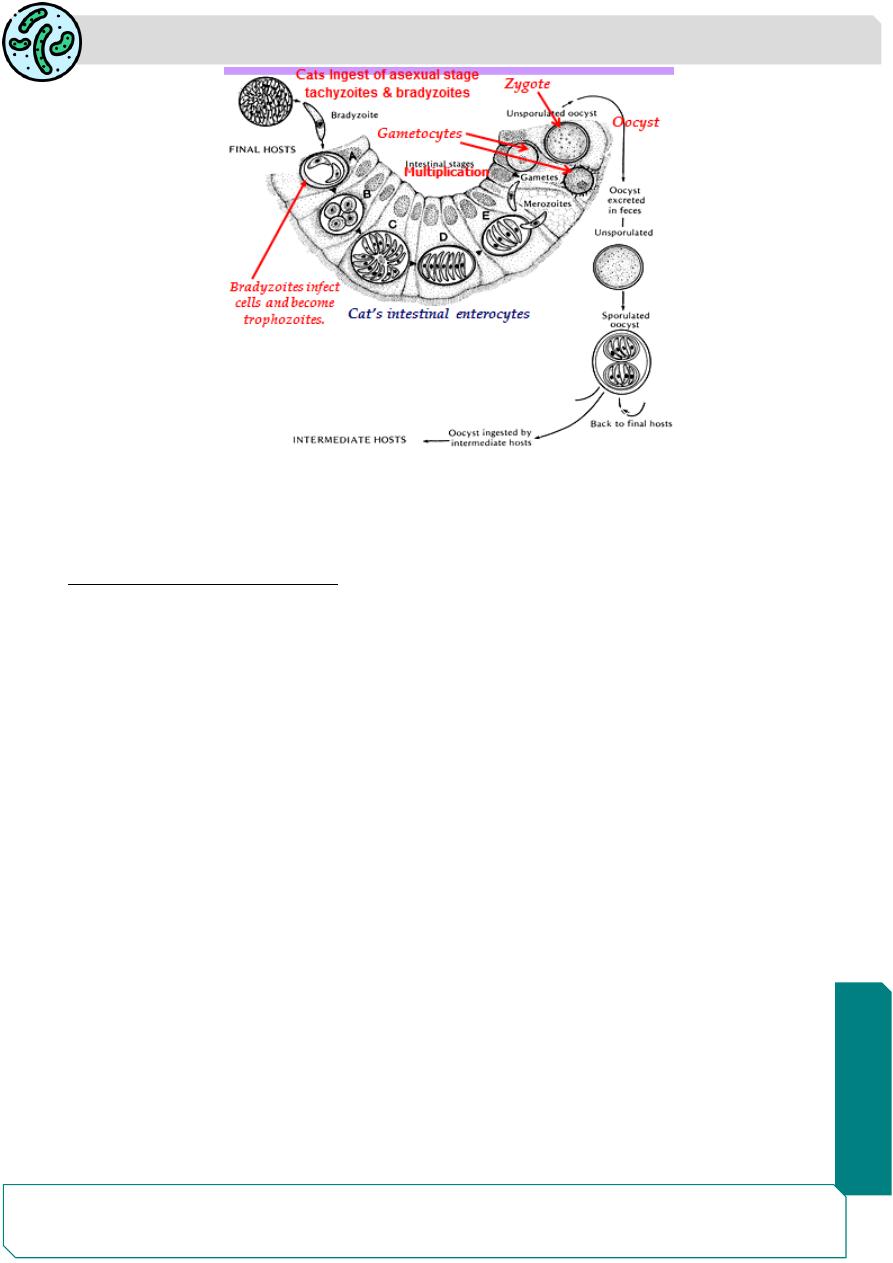
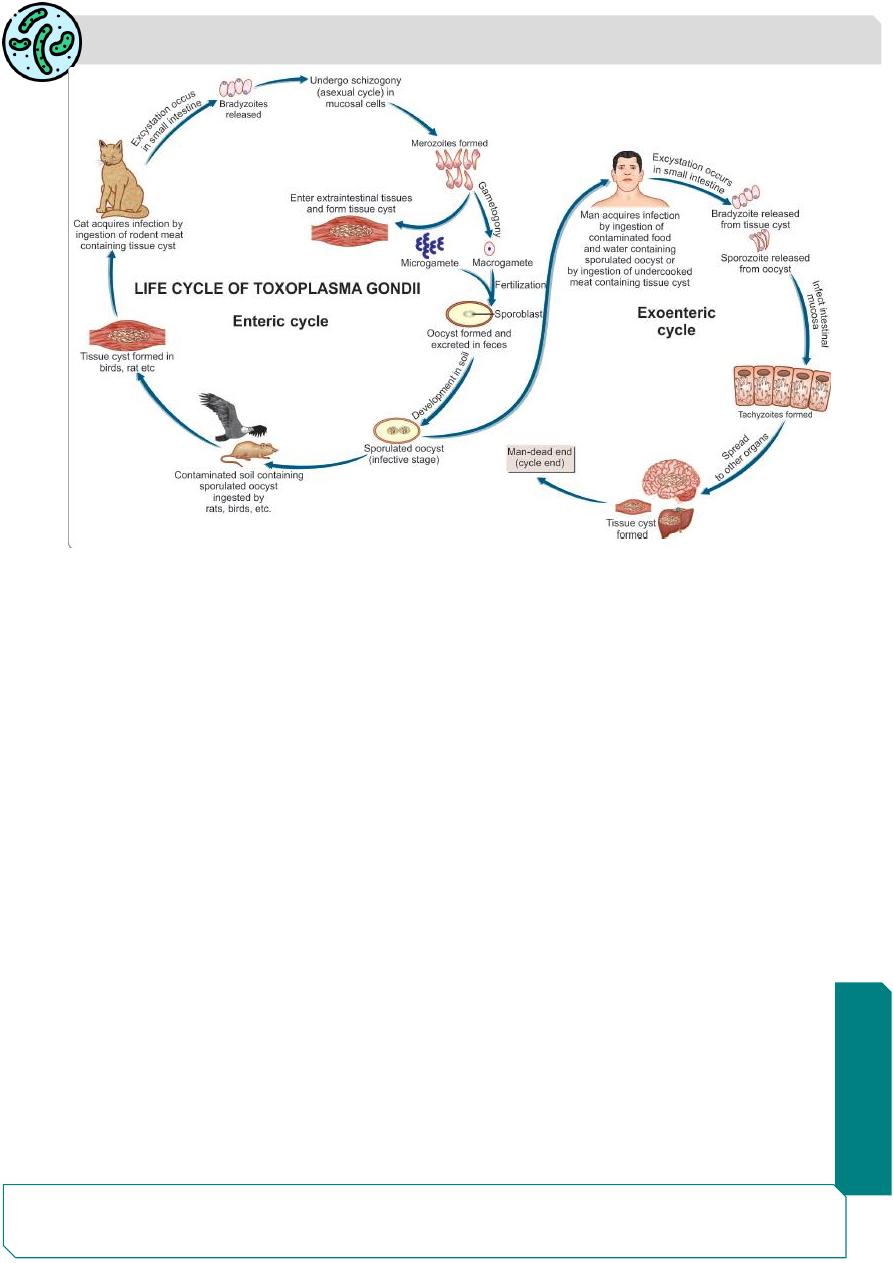
Life Cycle
T. gondii completes its life cycle in 2 hosts .
The widest range of hosts spread over 200 species of birds, reptiles, and mammals,
including humans
Definitive host:
Cats and other felines, in which both sexual and asexual cycle takes place.
Intermediate hosts:
Man and other mammals, in which only the asexual cycle takes place.
T. gondii has 2 types of life cycles:
€ Enteric cycle
€ Exoentric cycle.
Enteric cycle
Enteric cycle occurs in cat and other definitive hosts .
Both sexual reproduction (gametogony) and asexual reproduction (schizogony) occur
within the mucoscal epithelial cells of the small intestine of the cat.
Cat acquires infection by ingestion of tissue cysts in the meat of rats and other animals or
by ingestion of oocysts passed in its feces.
The bradyzoites are released in the small intestine and they undergo asexual
multiplication (schizogony) leading to formation of merozoites
Some merozoites enter extraintestinal tissues resulting in the formation of tissue cysts in
other organs of the body.
Other merozoites transform into male and female gametocytes and sexual cycle
(gametogony) begins, with the formation of microgamete and macrogamete.
A macrogamete is fertilized by motile microgamete resulting in the formation of an oocyst,
which passes through maturation stages (sporulation) in the soil after being excreted from
host through feces with in few days or weeks.
A mature oocyst containing 8 sporozoites is the infective form which may be ingested by
cats or other mammals to repeat the cycle
Parasitology
Notes…
8
Exoenteric cycle
Exoenteric cycle asexual cycle occurs in humans, mice, rats, sheep, cattle, pigs and birds
, which are the intermediate hosts.
Humans acquire infection after:
1-Eating uncooked or undercooked infected meat,particularly lamb and pork containing
tissue cysts
2-Ingestion of mature oocysts through food, water, or fingers flies)
)contaminated with
cat feces directly or indirectly
3-Intrauterine infection from mother to fetus (congenital toxoplasmosis)€ €
4-Blood transfusion or transplantation from infected donors.
5- laboratory infected after contact with contaminated needles or glassware or with
infected tissue.
Sporozoites from the oocysts and bradyzoites from the tissue cysts enter into the intestinal
mucosa and multiply asexually and tachyzoites are formed (endodyogeny).
Tachyzoites continue to multiply and spread by lymphatic system and blood.
Some tachyzoites also spread to distant extraintestinal organs like brain, eye, liver,
spleen, lung, and skeletal muscles and form tissue cysts.
The slowly multiplying forms inside the tissue cysts are known as bradyzoites, which
remain viable for years.
The dormant bradyzoites inside the cyst may be reactived in immune suppression causing
renewed infection in the
host.
Human infection is a dead end for the parasite
Parasitology
Notes…
9
Pathogenicity and Clinical Features
The outcome of Toxoplasma infection depends on the immune status of the infected
person and the strain of the parasite.
T. gondii is found inside the reticuloendothelial cells and many other nucleated cells of
the host.
The disease (toxoplasmosis) occur in the immunocompetent hosts or in the
immuno- compromised hosts.
The rate of the organ or tissue to get parasite infection depends on
1- Vascular supply
2-Immunity (local and general)
3- The regenerative ability of the host cells.
Toxoplasmosis has acquired great importance as one of the major fatal
complications in acquired immunodeficiency syndrome (AIDS).
-Most human infections are asymptomatic (90%).
-Clinical toxoplamosis may be congenital or acquired (10% )
In the acute infection, the proliferation of tachyzoites in the gastro-intestinal tract as well
as in the extra-intestinal sites, cause disruption and death of cells, resulting in the foci of
necrosis, surrounded by an intense mononuclear cell reaction.

Parasitology
Notes…
10
The development of both the humoral and cell mediated immunities in the
immunocompetent hosts, resolve the acute infection and associated with the
disappearance of tachyzoites from various tissues, especially from the extra-neural
tissues and the formation of tissue cysts.
The tachyzoites may persist in the (CNS) and even in the eye due to the absence of
circulating antibodies in the tissue
In the immunodeficient hosts and even some apparently normal hosts, the acute infection
does not resolve but progress to cause
severe necrotising lesions such as acute
necrotising encephalitis, pneumonitis and myocarditis, even death .
The presence of cysts in many organs through out the life of the host is probably lead to
clinicle feature of the infection.
In chronic infection, these cysts remain in a viable latent form and retain their potential for
reactivation. Reactivation of chronic infection possibly results from the rupture of cysts.
this causes recurrent parasitaemia frequently seen in some asymptomatic patients with
chronic infection
Rupture of cyst also liberates many tachyzoites, which cause toxoplasmosis in the
immunodeficient hosts or adults suffering from congenital toxoplasmosis.
The heart, liver, kidney and various other organs
in the immunocompetent hosts or
immunodeficient hosts are involved in disseminated toxoplasmosis.
These organs show areas of necrosis with or without inflammatory cells and the presence
of tachyzoites and cysts.
Toxoplasmosis in man occurs as congenital, acquired, ocular infections in the
immunocompetent hosts or an infection in the immunocompromised host
The most common manifestation
of acute toxoplasmosis is cervical lymphadenopathy.
The nodes may be single or multiple, are usually not tender lymphadenopathy occurs in
20
–30% of symptomatic patients. Between 20-40% of patients with lymphadenopathy
also have headache, malaise, fatigue, and fever .
A smaller proportion of symptomatic individuals have myalgia, sore throat, abdominal
pain, maculopapular rash, meningoencephalitis, and confusion.
Rare complications associated with pneumonia, myocarditis, encephalopathy,
pericarditis, and polymyositis.
Signs and symptoms associated with acute infection usually resolve within several weeks.

Parasitology
Notes…
11
Congenital toxoplasmosis
Congenital toxoplasmosis results from an acute primary infection acquired by the mother
during pregnancy (20%) of women infected with T. gondii develop clinical signs of
infection
Congenital toxoplasmosis occurs approximately (20%) of infants born to pregnant
women, who acquire the infection during first trimester of pregnancy.
Most infected newborns are asymptomatic at birth , Some develop clinical manifestations
of toxoplasmosis weeks, months, and even years after birth
Congenital infection lead to a wide variety of manifestations in the fetus and infant
including spontaneous abortion, still-birth, a newborn with classic signs of congenial
toxoplasmosis such as hydrocephalus or microcephalus, cerebral calcifications and
retinochoroiditis
Women with documented acute toxoplasmosis should be counseled to use appropriate
measures to prevent pregnancy for 6 months after infection.
T. gondii infection in pregnant women may cause poor obstetric outcomes such as
spontaneous abortion, hydatidiform mole, and sterility
In pregnancy, if the mother becomes infected during the first trimester, the incidence of
transplacental infection is lowest (20%), but the disease in the neonate is most severe.
If maternal infection occurs during the third trimester, the incidence of transplacental
infection is greatest (65%), but the infant is usually asymptomatic at birth.
Infection of the fetus during last trimester of pregnancy, is more likely to be mild or
asymptomatic at birth.
the severity of fetal damage is highest, when infection is transmitted in early pregnancy
chronic infection, the tissue cyst may be reactivated during pregnancy and liberate
trophozoites, which may infect the fetus
The risk of fetal infection rises with progress of gestation; from 20% in first trimester to
65% in the third trimester.
Acquired toxoplasmosis
Acquired infection with Toxoplasma in immunocompetent persons is generally an
asymptomatic infection (90%).
However, 10-20% of patients with acute infection may develop cervical lymphadenopathy
and/or a flu-like illness. Fever, headache, myalgia, and splenomegaly are often present.
Parasitology
Notes…
12
Rare cases of human gastrointestinal tract infection with T. gondii have presented as
ulcerations in the mucosa
The clinical course is benign and self-limited; symptoms usually resolve within a few
months to a year
Immunodeficient patients often have central nervous system (CNS) disease but may have
chorioretinitis , or pneumonitis .
In patients with AIDS, toxoplasmic encephalitis is the most common cause of
intracerebral mass lesions duto reactivation of chronic infection.
Toxoplasmosis in patients being treated with immunosuppressive drugs may be due to
either newly acquired or reactivated latent infection
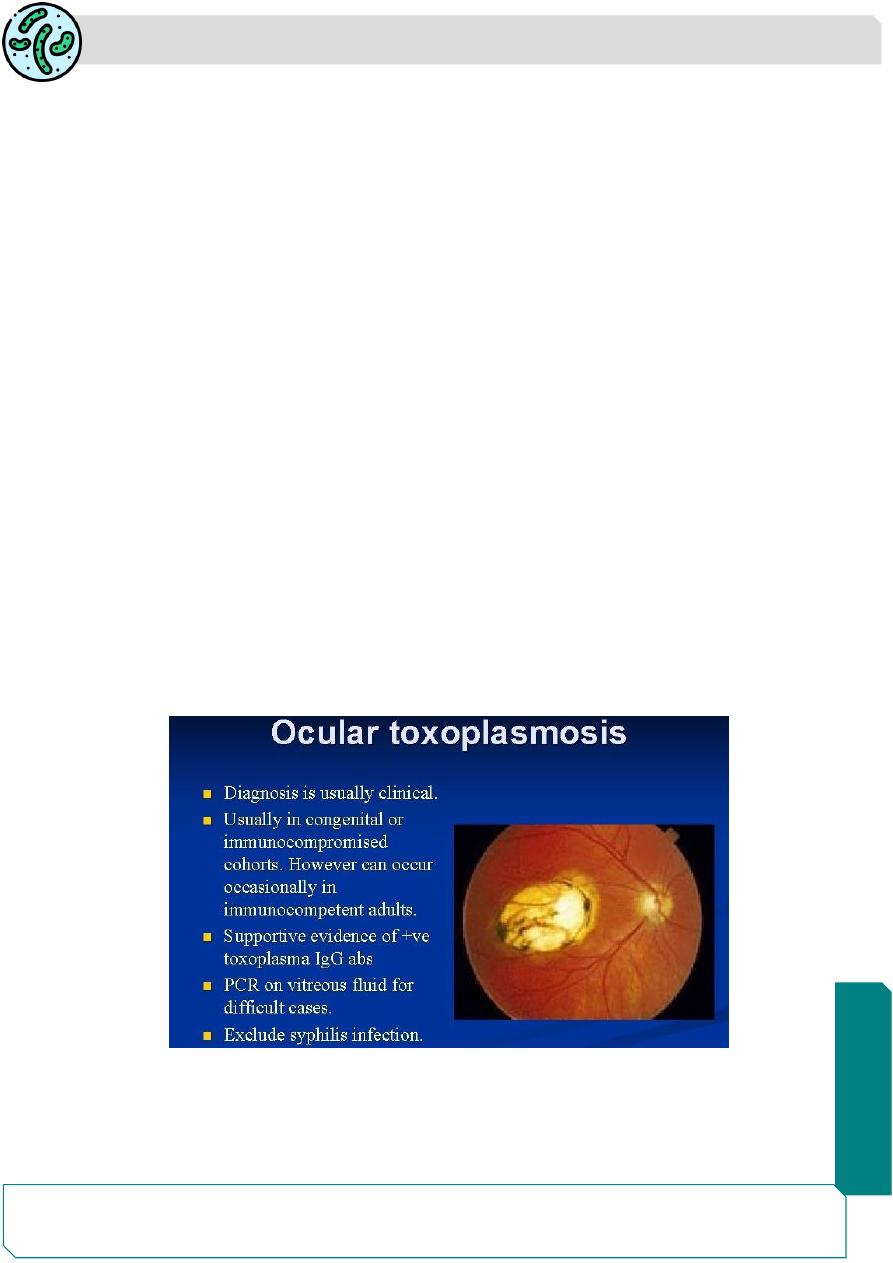
Occular Toxoplasmosis
Acute infection of eye begins as single or multiple foci of necrosis of retina .
Infection with T. gondii is estimated to cause 35% of all cases of chorioretinitis in the
United States and Europe.
Both the tachyzoites and tissue cysts are found in the retinal lesions.
Ocular manifestations of congenital toxplasmosis in the new born infants often
asymptomatic until the second or third decade of life.
when lesions develop in the eye. Unilateral chorioretinitis with photophobia blurred vision
and pain in the eye are the frequent clinical manifestation

Parasitology
Notes…
13
Infection In the Immunocompromised host
All types of T. gondii infections that occur in the immunocompetent hosts, are also seen
in the immunocompromised hosts.
The infection is more serious in immunosuppressed patients receiving immuno-
suppressive therapy for malignancy or persons receiving organ transplantations drugs
and AIDS.
toxoplasmic encephalitis is one of the most commonly recognized manifestation of the
infection in patients with AIDS.
the disease progresses rapidly and death is the frequent out come of the condition.
The signs and symptoms of acute toxoplasmosis in immunocompromised patients
principally involve the CNS .
More than 50% of patients with clinical manifestations have intracerebral involvement.
Clinical findings at presentation range from nonfocal to focal dysfunction.
CNS findings include encephalopathy, meningoencephalitis, and mass lesions.
Patients may present with altered mental status (75%), fever (7o%), seizures (33%),
headaches (56%), and focal neurologic findings (60%).
Laboratory Diagnosis
The diagnosis of acute toxoplasmosis is made mainly by demonstration of trophozoites
and cysts in tissue and body fluids .
Microscopy
Tachyzoites and tissue cysts can be detected in various specimens like blood, sputum,
bone marrow aspirate, cerebrospinal fluid (CSF), aminiotic fluid, and biopsy material from
lymphnode, spleen, and brain.
Smear made from above specimens is stained by Giemsa, PAS, or Gomori methanamine
silver (GMS) stain
Tachyzoites appear as crescent-shaped structures with blue cytoplasm and dark nucleus
Tachyzoites or cyst can also be demonstrated effectively by fluroscent conjugated
antibody technique in tissue biopsy or impression smear.
Presence of only tissue cysts does not differentiate between active and chronic infection.
The presence of cysts in placenta or tissues of newborn establishes congenital
toxoplasma infection

Parasitology
Notes…
14
Animal Inoculation
Toxoplasma can be isolated by inoculating body fluids,
blood, or tissue specimes by intraperitoneal inoculation in mice or in tissue culture.
Mice should be examined for Toxoplasma in their peritoneal exudate after 7
–10 days of
inoculation.
Serodiagnosis
is the main stay for diagnosis of toxoplasmosis.
Antibody detection
Diagnosis of acute infection with T. gondii can be made by detection
of IgM and IgG antibodies.
Tests include:
€ € Enzyme-linked immunosorbent assay (ELISA)
€ € Indirect fluroscent antibody test (IFAT)
€ € Latex agglutination test
Sabin-Feldman dye test
Positive IgG can be detected as early as 2
–3 weeks after infection. Peak level of antibody
is observed in blood 4
–8 weeks after infection
A positive IgM antibody titer indicates an early primary infection.
The serum IgM titer can be measured by double sandwich IgM ELISA , more specific and
sensitive.
Negative IgM titer and postive IgG titer indicate distant infection.
Double sandwich IgA-ELISA test is used for detecting congenital infection in newborns
IgG antibodies :
The IgG for usually appear within 2 weeks of the infection and peak within 1-2
months.However, they decline over months to years .
IgG antibodies avidity testing can be usefull in difficult cases during pregnancy for
establishing when infection may have occurred
IgM antibodies can be detected as early as one week after the primary infection, peak
within 2-4 weeks, then drop to below the detection limit within a few weeks
The detection of both T. gondii-specific IgM and IgA antibodies after birth confirms the
diagnosis of congenital Toxoplasmosis ,because both of them can not cross the placenta
Serologic diagnosis in congenital toxoplasmosis based on the persistence of IgG
antibody or a positive IgM titer after the first week of life (a time frame that excludes
placental leak).

Parasitology
Notes…
15
The IgG determination should be repeated every 2 months.
An increase in IgM beyond the first week of life is indicative of acute infection.
Up to 25% of infected newborns may be seronegative and have normal routine physical
examinations
Antigen detection
Detection of antigen by ELISA indicates recent Toxoplasma infection.
In AIDS and other immonocompromised patients, antigen detection is very useful.
Detection of antigen in amniotic fluid is helpful to diagnose congenital toxoplasmosis
Skin test of Frenkel
Diluted toxoplasmin is injected intradermally and delayed positive
reaction appears after 48 hours. This test is not very reliable for diagnosis of toxoplasma
Molecular Methods
DNA hybridization techniques and polymerase chain reaction (PCR)
are increasingly used to detect Toxoplasma from different tissues and body fluids.
T. gondii can be detected by PCR of the aminiotic fluid in case of congenital
toxoplasmosis.
Imaging
Magnetic resonance imaging (MRI) and computed tomography (CT) scan are
used to diagnose toxoplasmosis with (CNS) involvement.
Ultrasonography (USG) of the fetus in utero at 20
–24 weeks of pregnancy is useful for
diagnosis of congenital toxoplasmosis.
Sabin-Feldman dye test.
the first serological method to be described by Sabin and
Feldman (1948) to detect circulating antibodies in toxoplasmosis
Dye test is a highly sensitive and specific test with no false positives reported.
it is now used only in a reference laboratory as a reference serological test.

Parasitology
Notes…
16
Treatment
Congenital Toxoplasmosis
Neonates with congenital infection are treated with oral
pyrimethamine (1 mg/kg) daily and sulfadiazine (100 mg/ kg) with folinic acid for 1 year.
Systemic corticostoriod may be added to reduce chorioretinitis
Immunocompetent Patients and older children
, who have only lymphadenopathy, do
not require specific therapy unless they have persistent, severe symptoms
Patients with ocular toxoplasmosis are treated for 1 month with pyrimethamine plus either
sulfadiazine or clindamycin
Prophylaxis and control
1-
Individuals at risk, particularly pregnant women, children, and immunocompromised
persons should avoid contact with cat and its feces.
2-
Proper cooking of meat (Meat cooked to 50-60 Cº for 4
– 6 minutes or freezing at – 20
Cº for 48 hours)
3-
Proper washing of hands and washing of vegetables and fruits before eating.
4-
Blood or blood products from seropositive persons should not be given and screening
for T. gondii antibody should be done in all blood banks. The seroprevalence of T. gondii
in blood donors in China
((20%) in Egypt (59%) and Malaysia (28%)
5-
It is difficult to control toxoplasmosis because of wide range of animal reservoirs.
6-
Some occupations required people to have contact with animals and meats and these
frequently possess higher risk of infection with the parasite need education ,such as dairy
& slaughterhouse & meat-processing workers, veterinarians, meat sellers and cooks.
7-
Detection of antibodies is very important for pregnant women and women of child-
bearing age.
This is an effective way to find the infection, and then to provide treatment. It is also an
efficient way to stop congenital toxoplasmosis in newborns
Currently, there is no effective vaccnine available for humans. a genetically
engineered vaccine is under development for use in cats
