
Introduction to the clinical Medicine
Clinical Methods
Objectives
1- Define clinical methods
2- Steps in making diagnosis
3- Understand the steps of history taking ?
4- Understand how to analyse pain ?
5- Able to list the important symptoms of the different systems.
6-Able to understand the steps of general physical examination
Definition: Is the term used to describe a properly organized
approach to the patient and to his or her disease .
Diagnosis: should precede treatment whenever possible, but the
main aim of the doctor is to help the patient and family manage the
problems caused by a disease, where possible, offer treatment, cure
or prevention.
Diagnosis :
There are two main steps in making a diagnosis:
1. The first is to establish the clinical features by history – taking,
physical examination and investigation. (database).
2. The second is the interpretation of these data if possible, in terms
of disordered function and structure, that is pathology. (pathology
can mean disease or social pathology).
Communication: The art of history-taking
Headings to be used in history taking
•
Preliminary data (name, age, sex, occupation, address, religion,
marital status, date of admission and date of examination).
•
Presenting (chief) complaint and its duration:
•
History of present illness.
•
Menstrual history.
•
Medication: drugs, blood transfusion and vaccination.

•
History of previous illness.
•
Socio-economic history.
•
Family history.
•
Personal history.
Presenting (chief) complaint
•
Simply it means the problem which made the patient seek
medical help. Some patients have more than one main
complaint and a few particularly the neurotic have so many
that is impossible to identify a single chief complaint. For these
patients, the presenting complaints themselves represent the
problem, rather than the underlying disease.
Duration of the illness
•
The duration of symptomatic events is especially important
since the chronology of the illness will provide valuable clues to
the pathological process underlying it. The question of duration
may be difficult as many people especially elderly often find
difficult to remember the duration of their illness.
•
Most patients with long standing symptoms tend to date them
by events or seasons rather than by years, even though there is
no causal relationship.
History of present illness
•
Ask the patient to tell you the story of the illness from the
beginning.
•
Ideally you should allow this to continue without interruption,
except in certain circumstances.
•
Always begin by talking with the patient, excluding others,
however you may find it helpful to seek clarification or even an
alternative or objective view of the history from the relative or
friend.
•
When the patient has given you an initial description of his/her
symptoms, suggest that you would like to find out more about
certain aspects.
•
Some patients have symptoms which come and go, and it is
then important to try to find out whether the relapses and
remissions are related in any way to times, seasons or events in
the patient life.
•
Present history should contain the following: onset of the
illness (which may not be the same as chief complaint onset
especially in those with chronic illnesses like IHD and diabetes
mellitus), course of the illness, reason for presentation then
analysis of chief complaint and lastly review of other systems.
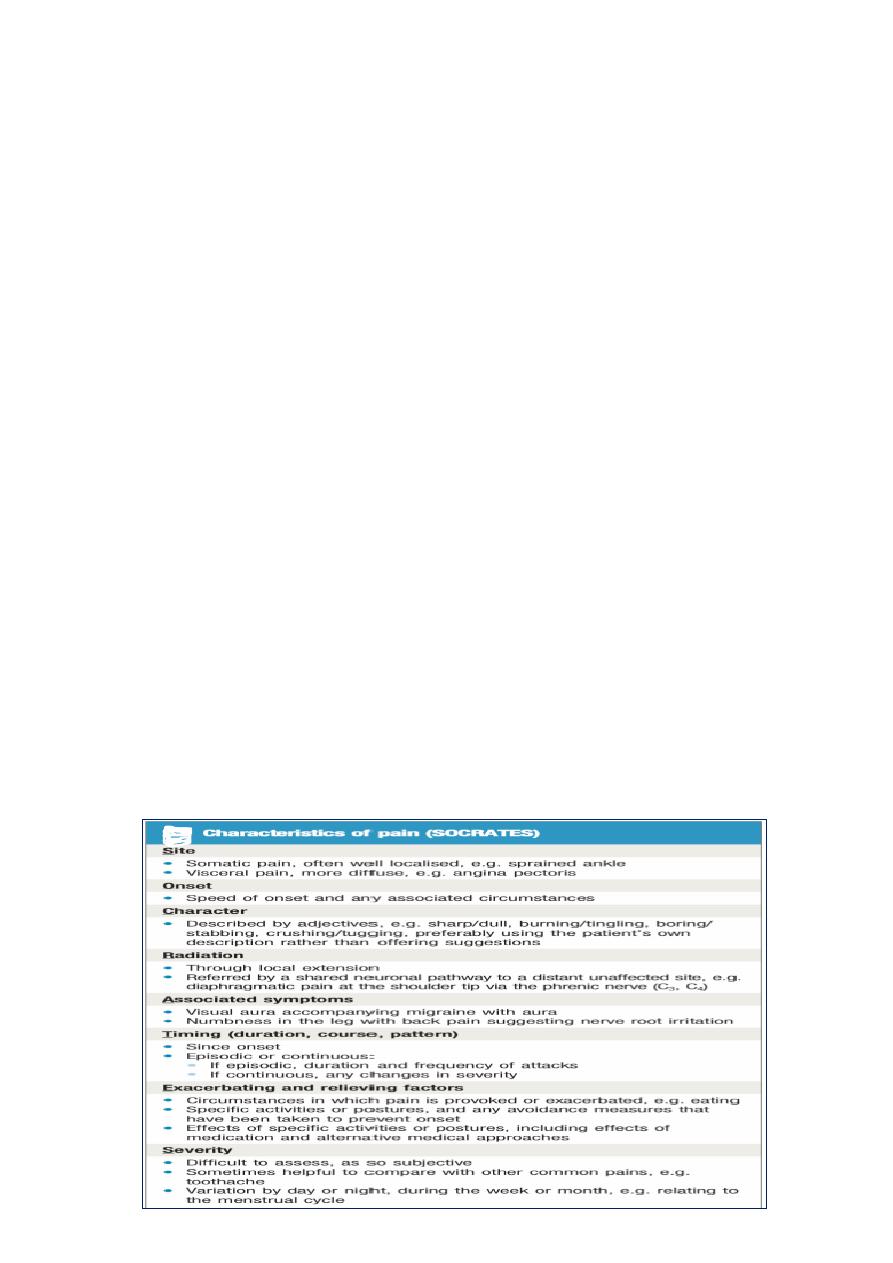
Analysis of pain as a symptom
•
When did it start? What was the first thing noticed? Progress
since then. Ever had it before?
SOCRATES
’ questions:
•
S
ite;
•
O
nset (gradual, sudden);
•
C
haracter;
•
R
adiation;
•
A
ssociations (e.g nausea, sweating);
•
T
iming of pain/duration;
•
E
xacerbating and alleviating factors;
•
S
everity (e.g scale of 1–10, compared with worst ever previous
pain).

History of (past) previous illness
•
Should include all important medical illnesses e. g. IHD,
connective tissue disorders, DM, tuberculosis, valvular
diseases, renal or liver diseases and questions about common
infectious diseases during early childhood……..etc.
•
Past surgical history: Operations and injuries.
•
Beware of accepting ready-made diagnosis.
•
In some cases, it may be necessary to communicate with
doctors or hospitals that have treated the patient in the past.
Menstrual history
•
In the majority of women menstruation occurs about every 28
days.
•
Ask at what age menstruation began and if menstruation has
ceased, ask when this occurred. (the menopause usually occurs
toward the end of the fifth decade).
•
Questions about the amount of blood loss and the duration of
menses, it is probably abnormal if it lasts for fewer than 2 or
more than 8 days.
•
Ask about premenstrual tension and about presence or
absence of pain with periods.
•
Ask about contraceptives, obstetric and gynecological history.
Treatment history (Medical and surgical)
•
Details of drugs taken, including analgesic, oral contraceptive,
psychotropic drugs, and of surgery, radiotherapy and
psychotherapy are all important.
•
Adverse drug reactions.
•
Knowledge of current therapy also necessary to avoid drug
interaction.
•
May be a clue for diagnosis of past illnesses.

Family history
•
Patient position in the family and the ages of children if any.
•
Record state of health , similar condition in the family, other
important illnesses and the cause of death of immediate
relatives.
•
Family tree study for genetic factor in cases of hereditary
diseases.
Social history
•
The patient’s physical and emotional environment, including
their surroundings at home and work, and their habits and
mental attitude to life and to work are essential components of
the history that assessing the effect of illness on the patients
and on their family .
Also important to ask about the following:
1. Domestic and marital relationship.
2. Home surroundings
3. Diet and use of alcohol and tobacco.
4. Travel abroad
Occupation history
1.
I
s the job dusty, and if so what tools make the dust?
2. Are there fumes, or vapours, and if so what are the chemical
substances involved?
3. Is a hood installed over the bench, and is it connected to a
suction system?
4. Is protective clothing provided?
5. Is a special suit and goggles required and why?
6. Has any similar illness affected a fellow employee?

Review of systems
1. General: weight, sleep and energy.
2. GIT, abdomen and pelvis:
Upper GIT: pain, appetite, vomiting, flatulence, water brash,
heartburn, dysphagia and other symptoms.
Lower GIT: diarrhea, constipation, pain
Liver and gallbladder: jaundice, pain
3. Genital system: impotence, Sexually Transmitted Diseases(STDs),
problems of infertility.
4. cardiovascular system: dyspnea, pain or tightness, palpitation,
cough, oedema, other symptoms.
1- Cardiorespiratory symptoms
•Chest pain .
•Exertional dyspnoea (=breathlessness): quantify exercise tolerance
and how it has changed, eg stairs climbed, or distance walked,
before onset of breathlessness.
•Paroxysmal nocturnal dyspnoea (PND). Orthopnoea, ie
breathlessness on lying flat (a symptom of left ventricular failure):
quantify in terms of number of pillows the patient must sleep on to
prevent dyspnea.
•Oedema: ankles, legs, lower back (dependent areas).
•Palpitations (awareness of heartbeats): can they tap out the
rhythm?
•Cough: sputum, haemoptysis (coughing up blood).
•Wheeze.
5. The blood: Lassitude, dyspnea, infections, blood loss, skin
problems, diet, past history, drug history, occupational history,
lymph glands enlargment.
6. Respiratory system: cough, sputum, breathing, wheeze, chest pain
7. Urinary system: Systems suggestive of renal failure, urine,
8. Skin diseases.
9. Nervous system: Stroke, epilepsy, common neurological
stmptoms.

10. Locomotor system
Physical examination (general)
•
Mental and emotional state.
•
Physical attitude.
•
Gait
•
Physique
: short, tall, muscular, fat, thin
•
Face
: Expression, hypothyroidism, thyrotoxicosis, nerve
palsy, acromegaly, others.
•
Skin
: pallor, yellow, cyanosis, oedema
•
Hands
: shake, shape, joint, nail, finger
•
Feet
: ulcers, oedema, ischemia
•
Neck
: lymph nodes, thyroid, carotid
•
Breasts
: redness, ulcer, dimpling, nipple discharge,
palpate for masses esp. for older than 35 year
•
Axillae
: For lymph nodes
•
Temperature
: Normal 36.8-37.2 C
•
Respiration
: Normal rate in adult 14-18 respiration/min.,
wheeze, stridor, cheyne-stokes respiration
•
Odours
: of alcohol, diabetic KA, uraemia, liver failure,
bad dental hygeine.
Schema for routine examination
•
General appearance
•
Hair
•
Eyes
•
Face
•
Mouth and pharynx
•
Neck
•
Upper limbs
•
Thorax (lung, heart): Ant, Lat, Post.
•
Abdomen
•
Lower limbs
•
Examination of excreta.

