Medicine
Notes…
1
Lecture.5 PRESENTING PROBLEMS In GASTROINTESTINAL DISEASE
Dysphagia
Dysphagia is defined as difficulty in swallowing.
It may coexist with heartburn or vomiting but should be distinguished
from both globus sensation (in which anxious people feel a lump in the throat without
organic cause) and odynophagia (pain during swallowing, usually from gastro-esophageal
reflux or candidiasis).
Dysphagia can occur due to problems in the oropharynx or esophagus.
➢ Oropharyngeal disorders affect the initiation of swallowing at the pharynx and upper
esophageal sphincter.
➢ The patient has difficulty initiating swallowing and complains of choking, nasal
regurgitation or tracheal aspiration. Drooling, dysarthria, hoarseness and cranial
nerve or other neurological signs may be present.
➢ Esophageal dysphagia disorders cause dysphagia by obstructing the lumen or by
affecting motility. Patients with esophageal disease complain of food ‘sticking’ after
swallowing.
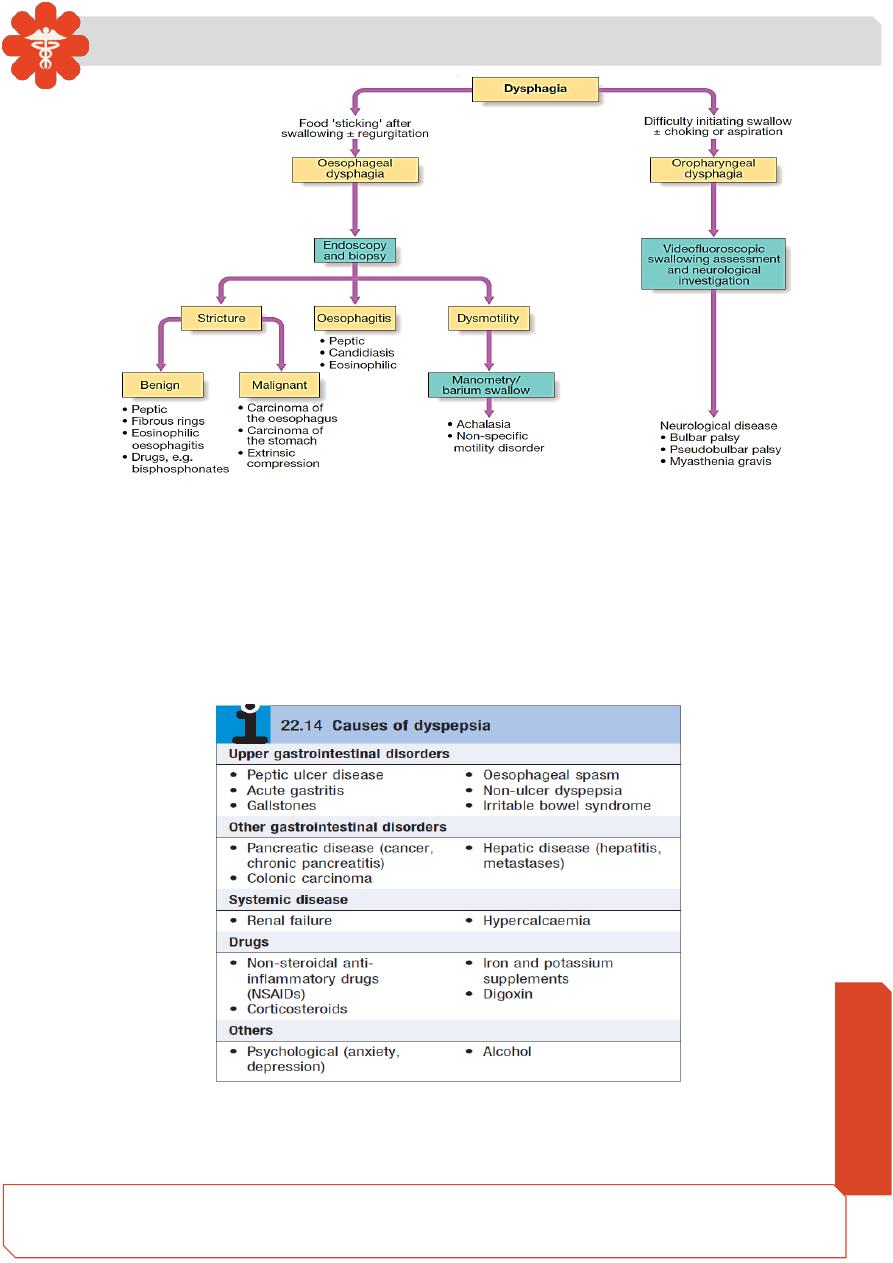
Dysphagia : Investigations
Need So
me
Help?
Medicine
Notes…
2
• Dysphagia should always be investigated urgently. Endoscopy is the investigation
of choice because it allows biopsy and dilatation of strictures.
• Even if the appearances are normal, biopsies should be taken .
• If no abnormality is found, then barium swallow with video -fluoroscopic swallowing
assessment is indicated to detect major motility disorders.
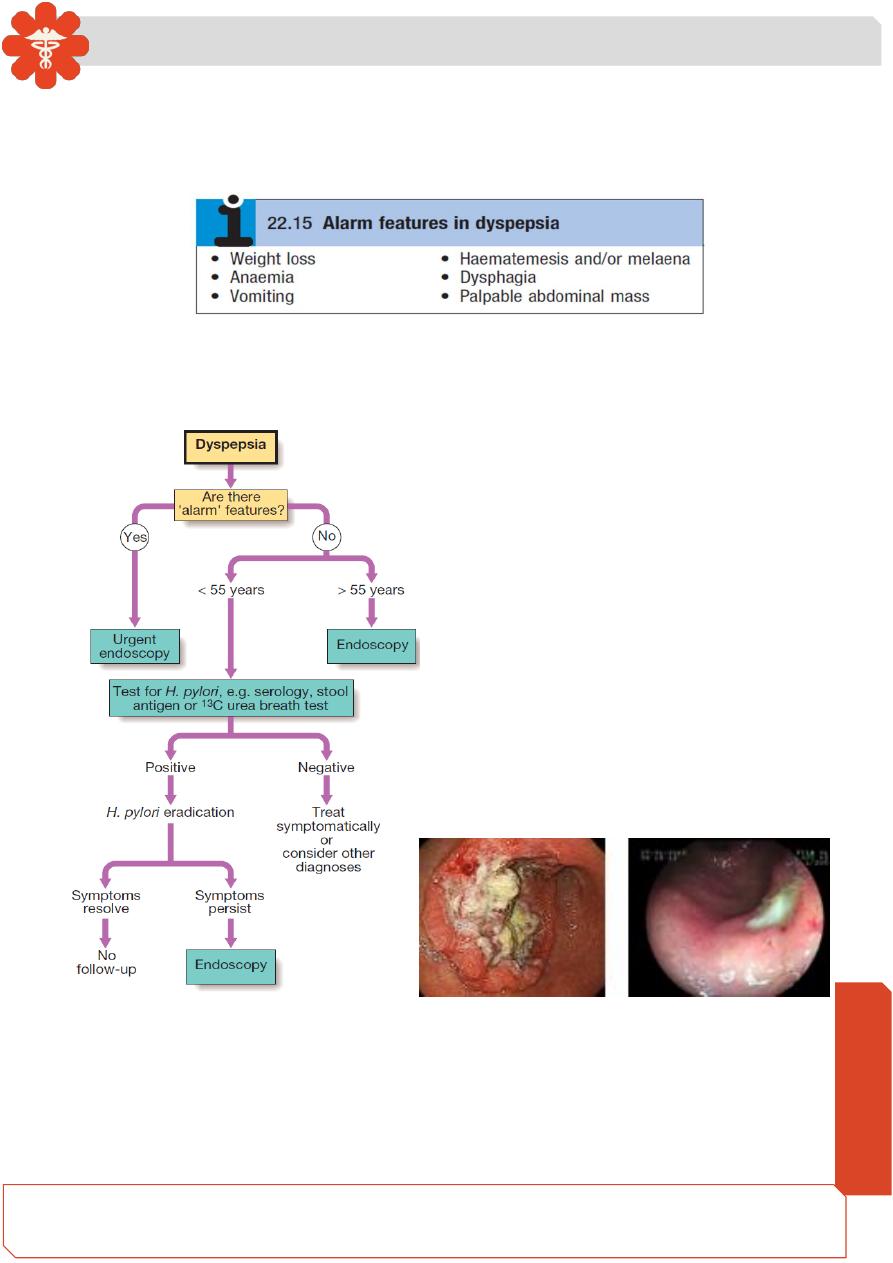
• Dyspepsia describes symptoms such as discomfort, bloating and nausea, which
are thought to originate from the upper gastrointestinal tract.
• People who present with new dyspepsia at an age of more than 55 years and
younger patients unresponsive to empirical treatment require investigation to
exclude serious disease.
Medicine
Notes…
3
• Although symptoms often correlate poorly with the underlying diagnosis, a careful
history is important to detect ‘alarm’ features requiring urgent investigation and to
detect atypical symptoms which might be due to problems outside the
gastrointestinal tract.
• Patients who present with new dyspepsia at an age of more than 55 years and
younger patients unresponsive to empirical treatment require investigation to
exclude serious disease.
Heartburn and regurgitation
• Heartburn describes retrosternal, burning discomfort, often rising up into the chest
and sometimes accompanied by regurgitation of acidic or bitter fluid into the throat.
These symptoms often occur after meals, on lying down or with bending, straining
or heavy lifting. They are classical symptoms of gastro-oesophageal reflux but up
Medicine
Notes…
4
to 50% of patients present with other symptoms, such as chest pain, belching,
halitosis, chronic cough or sore throats.
• In young patients with typical symptoms and a good response to dietary changes,
antacids or acid suppression investigation is not required, but in patients over 55
years of age and those with alarm symptoms or atypical features urgent endoscopy
is necessary.
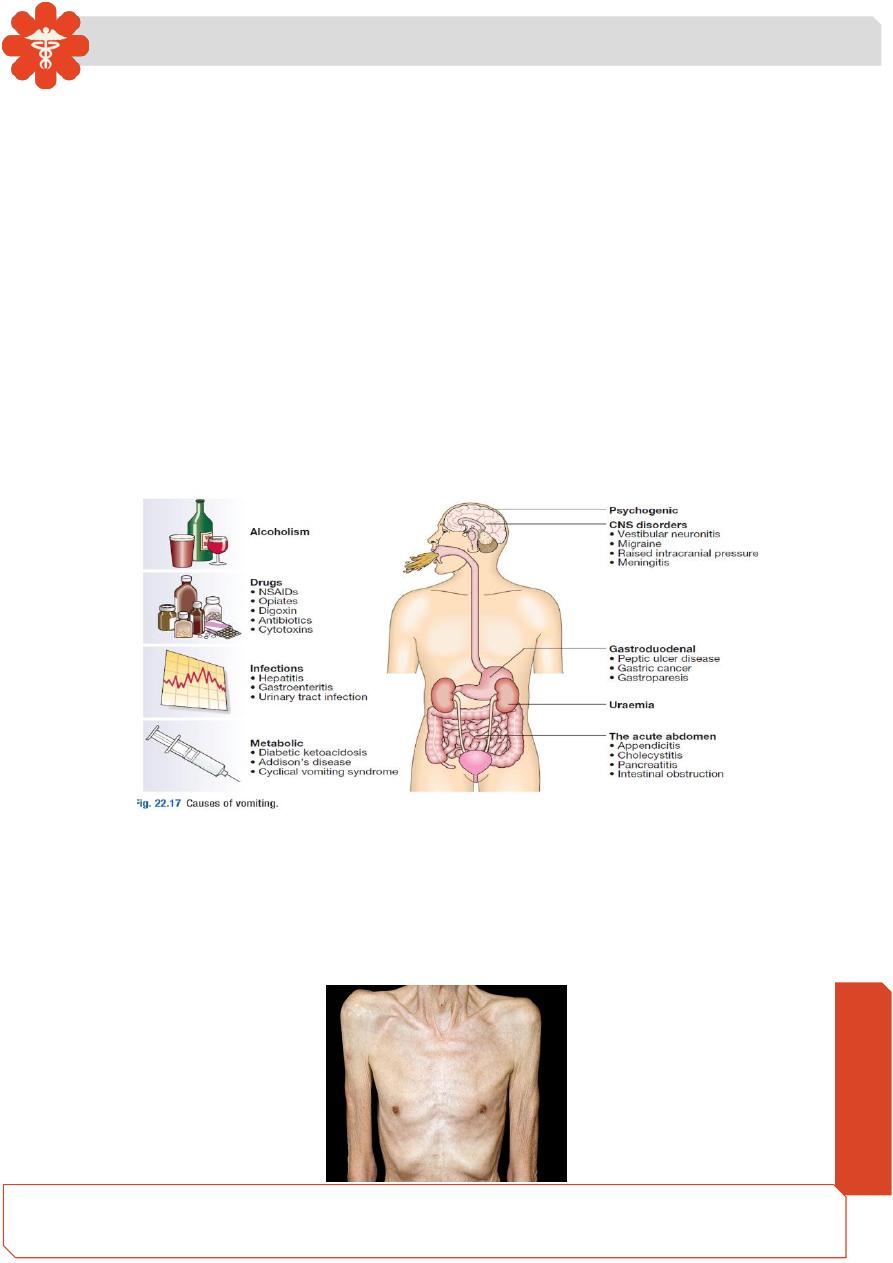
Vomiting
• Vomiting is a complex reflex involving both autonomic and somatic neural
pathways. Synchronous contraction of the diaphragm, intercostal muscles and
abdominal muscles raises intra-abdominal pressure and, combined with relaxation
of the lower esophageal sphincter, results in forcible ejection of gastric contents.
• It is important to distinguish true vomiting from regurgitation and to elicit whether
the vomiting is acute or chronic (recurrent), as the underlying causes may differ.
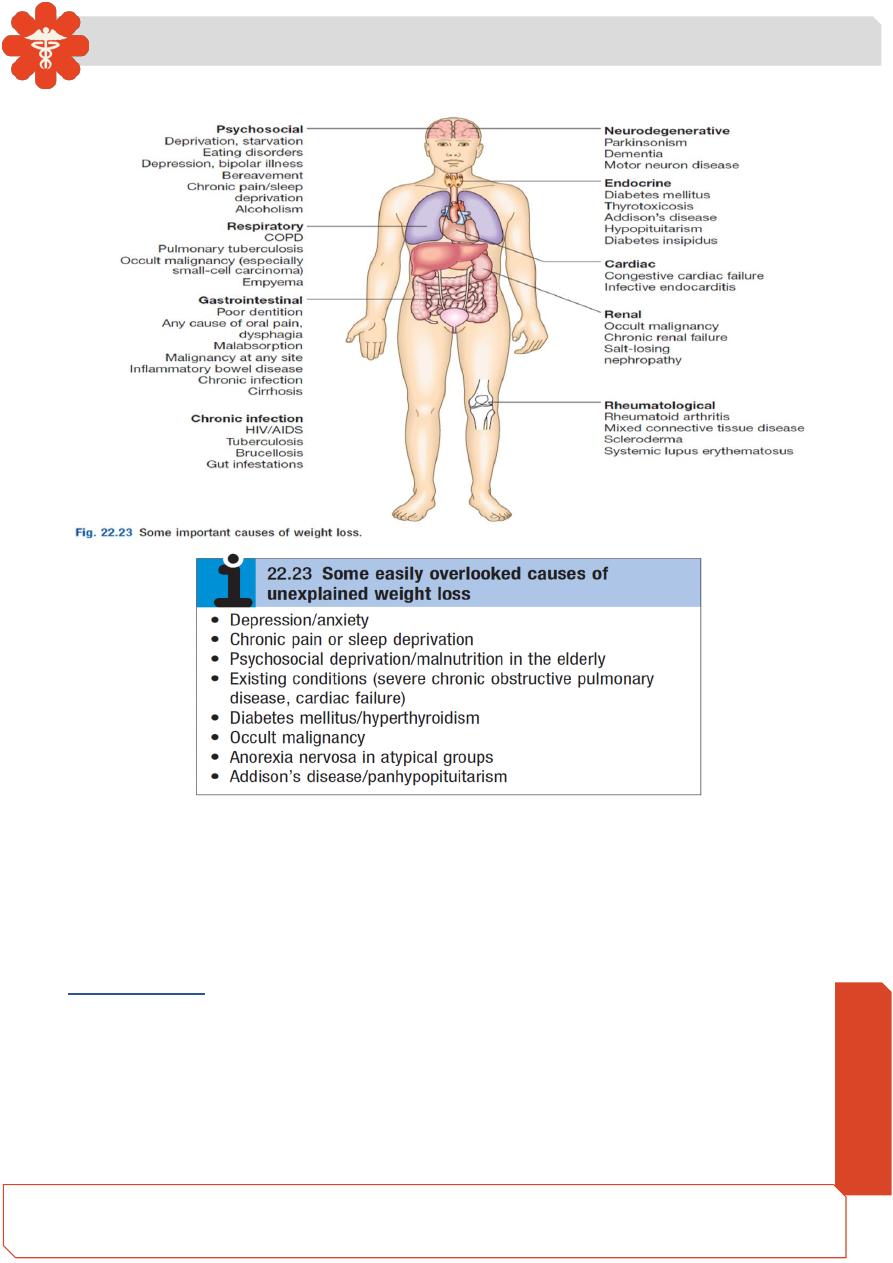
Weight loss
➢ Weight loss may be physiological, due to dieting, exercise, starvation, or the
decreased nutritional intake which accompanies old age.
➢ Weight loss of more than 3 kg over 6 months is significant and often indicates the
presence of an underlying disease.
Medicine
Notes…
5
Diarrhea
➢ Diarrhea is defined as the passage of more than 200 g of stool daily, and
measurement of stool volume is helpful in confirming this. The most severe
symptom in many patients is urgency of defecation, and fecal incontinence is a
common event in acute and chronic diarrheal illnesses.
Acute diarrhea
➢ This is extremely common and is usually due to feco oral transmission of bacteria
or their toxins, viruses or parasites .
➢ Infective diarrhea is usually short lived and patients who present with a history of
diarrhea lasting more than 10 days rarely have an infective cause.
Medicine
Notes…
6
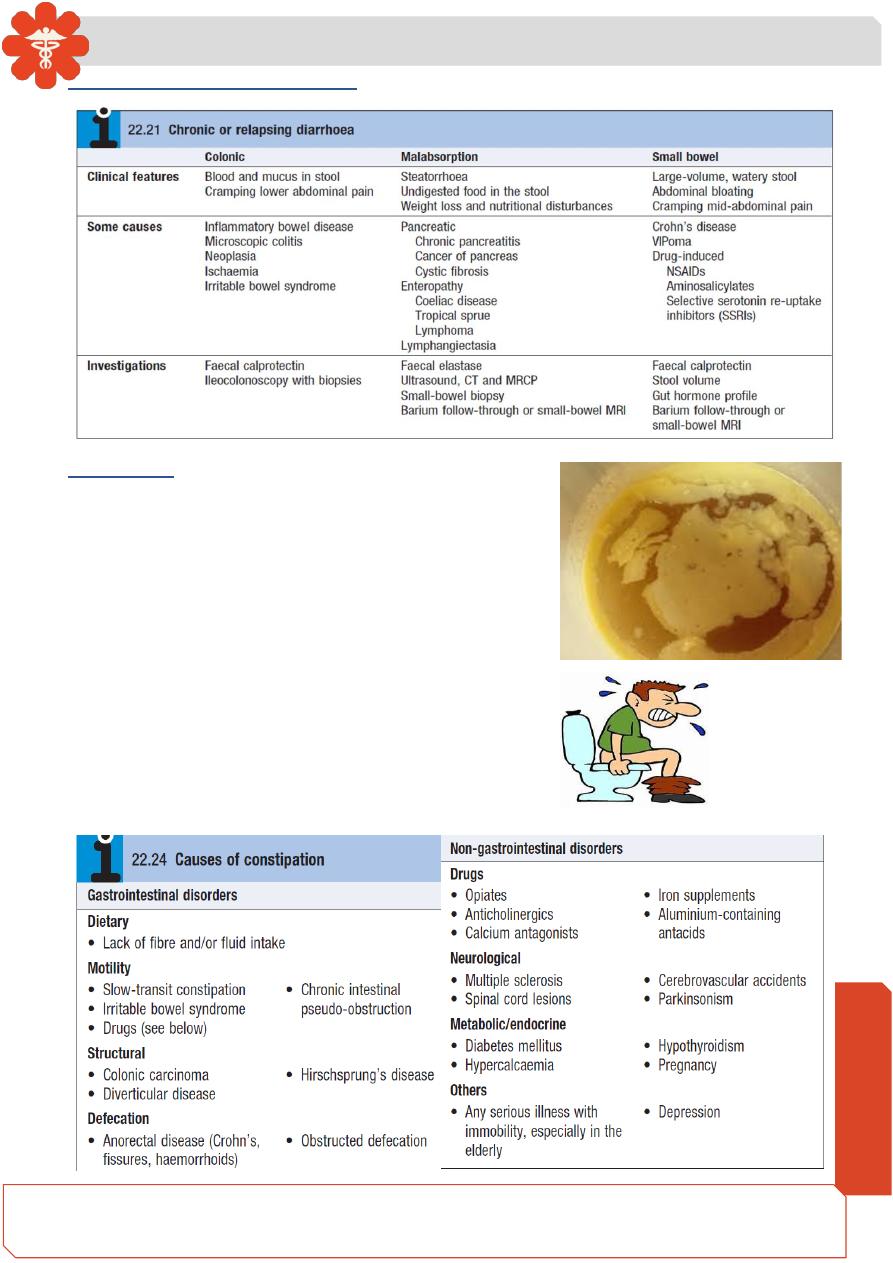
Chronic or relapsing diarrhea
steatorrhea
Bulky, pale and offensive stools which float in the toilet
. it signify fat malabsorption. Abdominal distension,
borborygmi, cramps, weight loss and undigested food
in the stool may be present. Some patients complain
only of malaise and lethargy.
Constipation
Constipation is defined as infrequent passage of hard
stools. Patients may also complain of straining, a
sensation of incomplete evacuation and either perianal
or abdominal discomfort. Constipation may occur in
many gastrointestinal and other medical disorders.

Medicine
Notes…
7
Acute upper gastrointestinal hemorrhage
➢ Hematemesis is red with clots when bleeding is r
apid and profuse, or black (‘coffee
grounds’) when less severe.
➢ Syncope may occur and is due to hypotension from intravascular volume depletion.
➢ Symptoms of anaemia suggest chronic bleeding.
Melena is the passage of black, tarry stools containing altered blood; it is usually caused
by bleeding from the upper gastrointestinal tract, although hemorrhage from the right side
of the colon is occasionally responsible. The characteristic color and smell are the result
of the action of digestive enzymes and of bacteria upon hemoglobin.
➢ Severe acute upper gastrointestinal bleeding can sometimes cause maroon or
bright red stool.
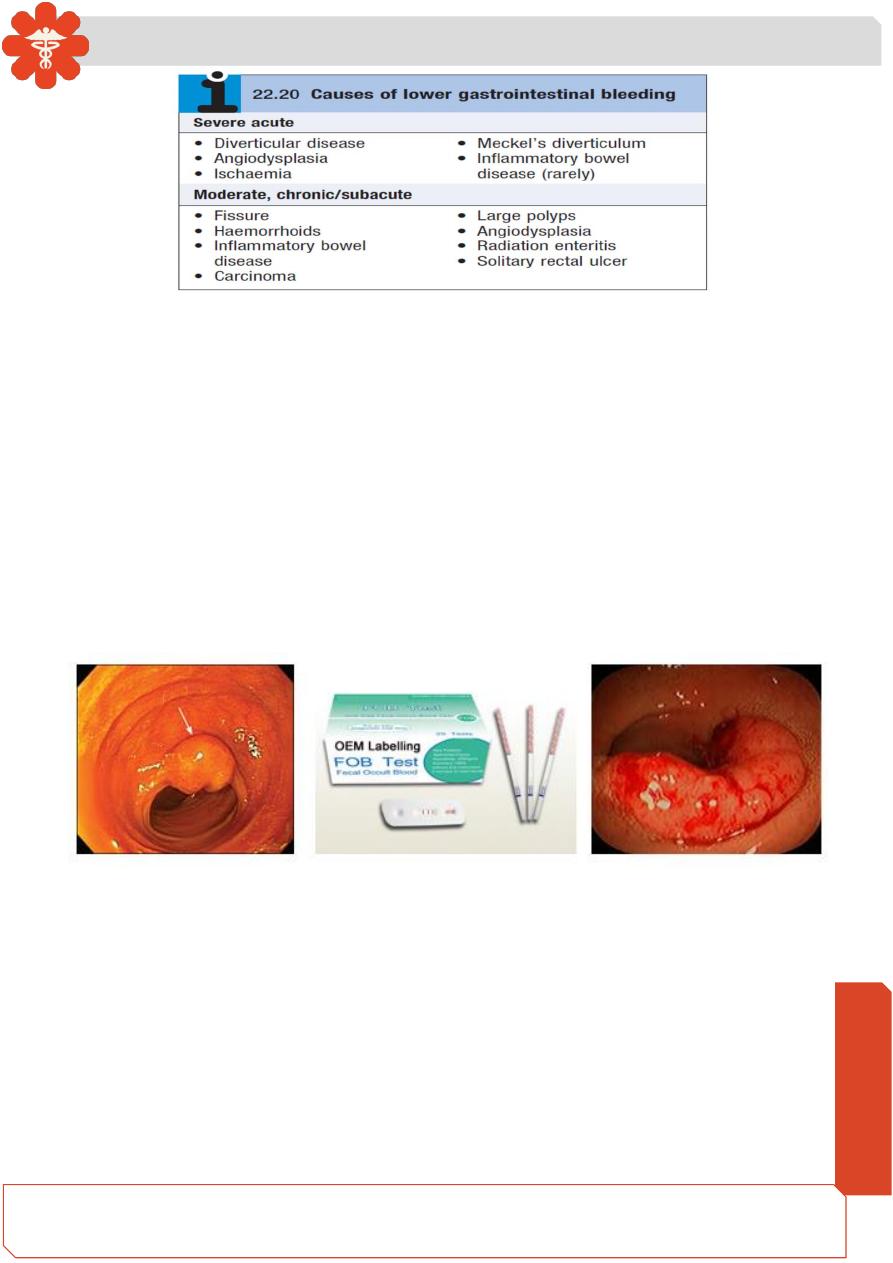
Lower gastrointestinal bleeding
• This may be due to hemorrhage from the colon, anal canal or small bowel. It is
useful to distinguish those patients who present with profuse, acute bleeding from
those who present with chronic or sub acute bleeding of lesser severity.
Medicine
Notes…
8
Chronic occult gastrointestinal bleeding
➢ occult means that blood or its breakdown products are present in the stool but
cannot be seen by the naked eye.
➢ Occult bleeding may reach 200 mL per day and cause iron deficiency anaemia.
➢ Any cause of gastrointestinal bleeding may be responsible but the most important
is colorectal cancer, particularly carcinoma of the caecum, which may produce no
gastrointestinal symptoms.
• Testing the stool for the presence of blood is unnecessary and should not influence
whether or not the gastrointestinal tract is imaged because bleeding from tumors is
often intermittent and a negative fecal occult blood (FOB) test does not exclude the
diagnosis.
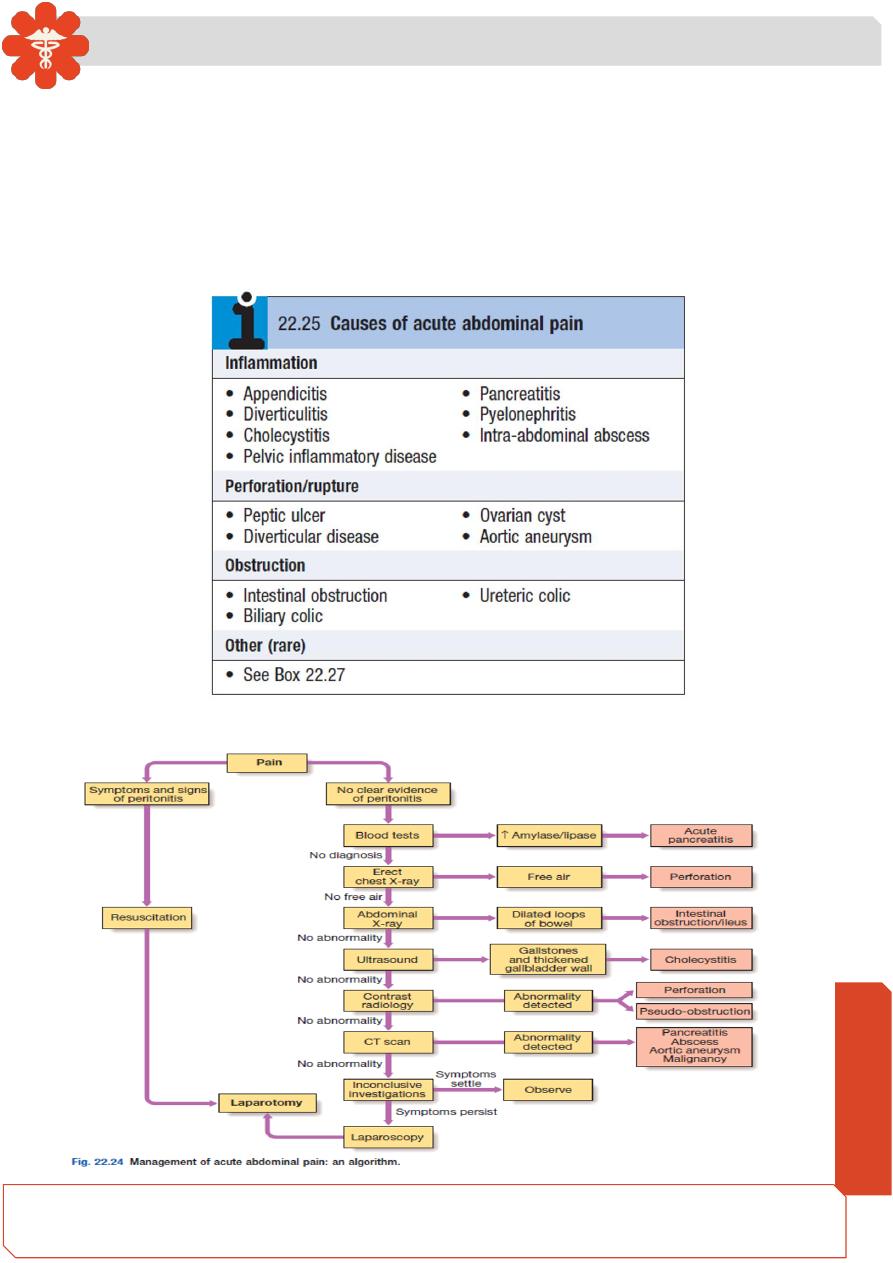
Abdominal pain
• There are four types of abdominal pain:
1.
• Visceral. Gut organs are insensitive to stimuli such as burning and cutting but are
sensitive to distension, contraction, twisting and stretching. Pain from unpaired
structures is usually but not always felt in the midline.
2.
• Parietal. The parietal peritoneum is innervated by somatic nerves, and its
involvement by inflammation, infection or neoplasia causes sharp, well-localised
and lateralized pain.
3. Referred pain. (For example, gallbladder pain is referred to the back or shoulder
tip.)
Medicine
Notes…
9
4. Psychogenic
. Cultural, emotional and psychosocial factors influence everyone’s
experience of pain. In some patients, no organic cause can be found despite
investigation, and psychogenic causes (depression or somatization disorder) may
be responsible
The acute abdomen
• This accounts for approximately 50% of all urgent admissions to general surgical
units. The acute abdomen is a consequence of one or more pathological processes.
The acute abdomen:Management
Medicine
Notes…
10
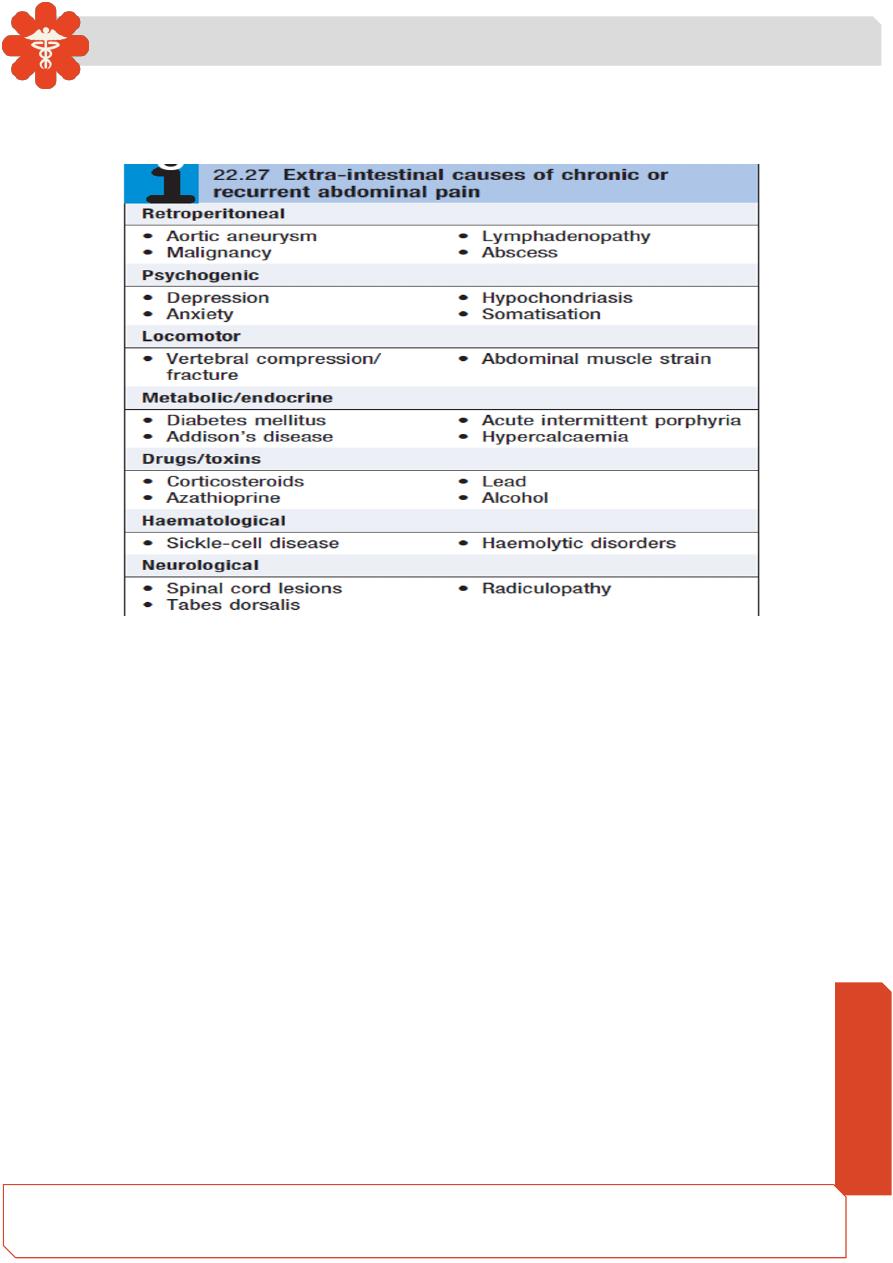
Chronic or recurrent abdominal pain
• It is essential to take a detailed history, paying particular attention to features of the
pain and any associated symptoms.
References of Lec 1 an
d 2: Davidson’s principles and Practice of medicine , 23
rd
edition ,
2018.
