Internal Medicine
Jaundice (Icterus)
Objectives:
1. Understand how bilirubin is formed.
2. Sumarrize the causes and different features of each type of jaundice.
3. How to approach a patient with jaundice
Jaundice: is yellowish discoloration of the skin, sclera and mucous
membrane, resulting from an increased bilirubin concentration in the
body fluid (N: < 1mg/dl). It is usually detectable clinically when the plasma
bilirubin exceeds 40µmol/l (~2.5mg/dl). Jaundice is a symptom or physical
sign of a disease.
Bilirubin Metabolism لالطالع فقط
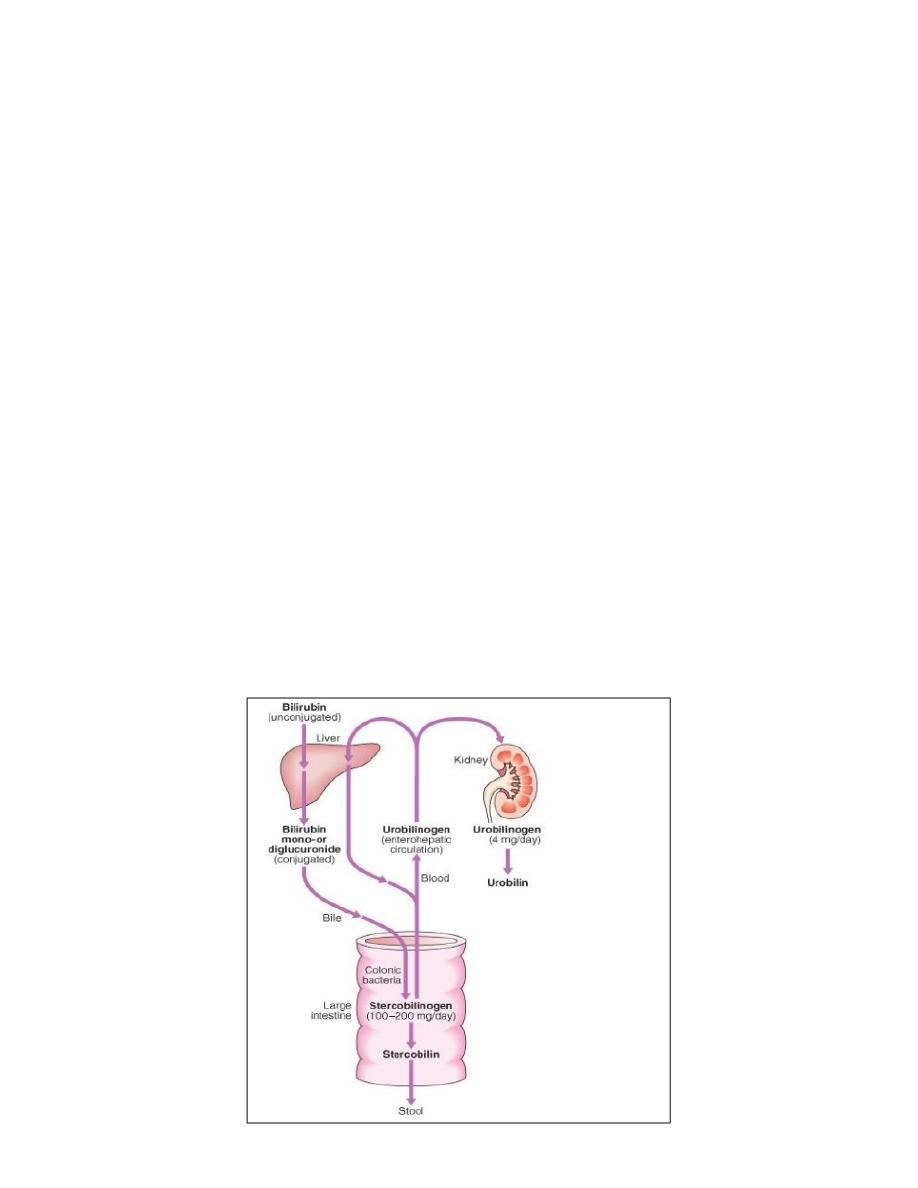
About 250mg of unconjugated bilirubin is produced from the catabolism
of Haem every day. Bilirubin in the blood is almost all unconjugated and,
because it is not water – soluble, it is bound to albumin and does not pass
into the urine. Unconjugated bilirubin is conjugated by the glucuronyl
transferase into mono and diglucuronide bilirubin. These are water
soluble and by specific carriers enter the bile and reach intestine.

Conjugated bilirubin is metabolized by colonic bacteria to form
stercobilinogen which may be oxidized to stercobilin and both are
excreted in the stool. A small amount of stercobilinogen (4mg/day) is
absorbed from the bowel and go to the blood and excreted through the
kidney (colorless urobilinogen).
Clinical types of Jaundice: for description purpose the jaundice is divided
into: pre-hepatic (hemolytic anaemia and congenital non-hemolytic
jaundice like Gilbert disease, hepatic or hepatocellular due to many
causes and lastly obstructive (cholestatic) either intrahepatic (medical)
which may be a consequences of hepatocellular damage or the causes may
be due to extra-hepatic biliary obstruction like stone, strictures, pancreatic
cancer, cancer of papilla of Vator, etc.
1. Haemolytic anaemia (Pre-hepatic): This is is characterised by an
isolated raised bilirubin level (usually unconjugated).
(unconjugated hyperbilirubinaemia) Increased destruction of RBCs or
their precursors in the marrow, causing increasing production of
bilirubin.

Features
A. Jaundice is usually mild (<100µmol/l) as healthy liver can excrete
bilirubin six times greater than normal before unconjugated bilirubin
accumulates in the plasma. This is not applied to new born
(Kernicterus may occur).
B. There are no features of liver disease other than jaundice. Also liver
function tests (LFTs) are normal.
C. There are no stigmata of chronic liver disease other than jaundice.
D. Normal or dark colored stool (stercobilinogen). Also urine may turn
dark on standing as urobilin is formed through the oxidation of
urobilinogen but a newly voided urine is colorless because no
bilirubinuria.
E. Pallor due to anaemia and splenomegaly are maybe (usually) present.
F. No bilirubinuria.
G. Blood count and film may show evidence of haemolytic anaemia
2. Congenital non-haemolytic hyperbilirubinaemia:
Are inherited either as autosomal dominant like Gilbert (unconjugated) or
autosomal recessive like Crigler-Najar (type1 & 2) also unconjugated and
type 1 is more serious and cause death in neonate. There are other types
of congenital non-hemolytic (Rotors & Dubin Jonson) which are causing
conjugated hyperbilirubinaemia.
Gilbert Disease: This is the comments type and benign condition causes
mild unconjugated hyperbilirubinaemia due to decrease in the level of
glucuronyl transferase or decrease bilirubin uptake inherited as (AD).
Usually follows viral infection or fasting well respond to phenobarbital.
Clinical examination is normal, except for mild jaundice.
Note: In Dubin Jonson syndrome , and Rotor disease, the bilirubin is
conjugated, whilist is unconjugated in Gilbert’s disease (syndrome).

Hepatic (Hepatocellular jaundice):
Results from inability of liver to transport bilirubin into the bile as a result
of parenchymal liver disease.
Swelling and oedema of cells may cause obstruction to the biliary
canaliculi. Both conjugated and unconjugated bilirubin is increased.
Examples of Causes:
A large number of conditions (acute & chronic parenchymal liver diseases)
can cause this type of jaundice:
- Viral hepatitis (A, B, C, D E).
- EBV, CMV.
- Drugs that cause hepatocellular damage like tetracycline, erythromycin,
anti-tuberculosis, etc.
- Alcohol consumption,
- Autoimmune liver disease (autoimmune hepatitis)
- Hereditary liver diseases.
- Ischaemia.
The severity of jaundice, the other clinical features, investigation,
treatment, and prognosis vary with underlying causes.
Characteristically, jaundice due to parenchymal liver disease is
associated with increases in transaminases (AST, ALT), but increases in
other LFTs, including cholestatic enzymes (GGT, ALP), may occur and
suggest specific aetiologies.
Acute jaundice in the presence of an ALT of > 1000 U/L is highly suggestive
of an infectious cause (e.g. hepatitis A or B), drugs (e.g. paracetamol) or
hepatic ischaemia.
Imaging is essential, in particular to identify features suggestive of
cirrhosis, define the patency of the hepatic vasculature and obtain
evidence of portal hypertension. Liver biopsy has an important
role in defining the aetiology of hepatocellular jaundice and the extent of
liver injury.
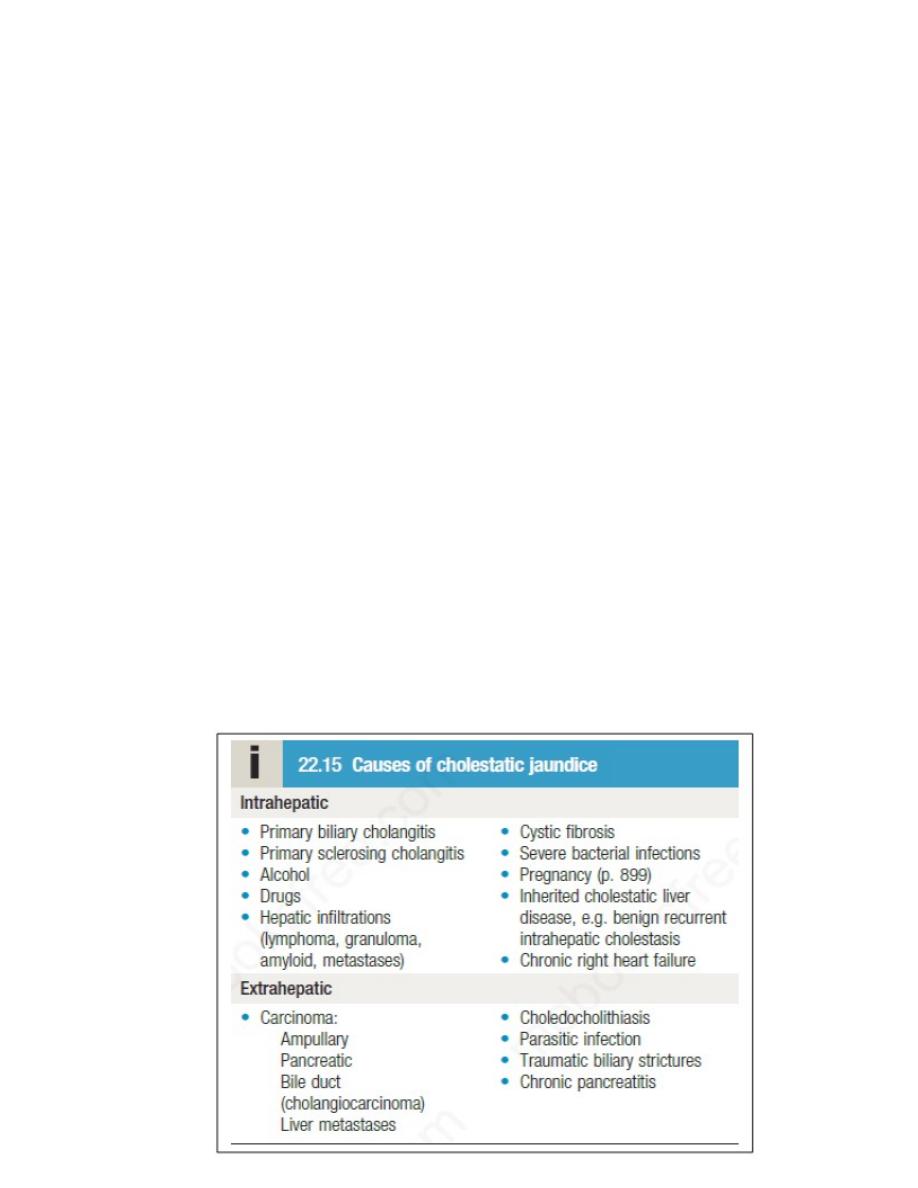
Obstructive (Cholestatic) jaundice: It is due biliary passage obstruction
(intra & extrahepatic). Tend to become progressive and severe because
conjugated bilirubin is unable to enter the bile canaliculi and passes back
into the blood and because failure of clearence of unconjugated bilirubin
arriving at the liver cells.
Causes of Obstructive Jaundice:
A. Intrahepatic cholestasis: examples of causes:
1. Primary biliary cholangitis (PBC),
2. Primary sclerosing cholangitis (PSC), it also cause extrahepatic biliary
passage obstruction.
3. Intrahepatic cholestasis of pregnancy.
4. Benign recurrent intrahepatic cholestasis (BRIC).
5. Drugs like contraceptive pills, chlorpromazine.
6. Hodgkin’s lymphoma.
7. Other parenchymal liver disease like viral hepatitis.
B. Extrahepatic:
1. Choledocholithiasis.
2. Carcinoma (ampullary, pancreatic,bile duct).
3. Parasitic infection.
4. Traumatic biliary stricture.

Clinical Features in Cholestatic Jaundice
A. Early features:
1. Jaundice.
2. Dark urine.
3. Pale stool.
4. Pruritis.
B. Late features:
1. Xanthelasma and xanthomas.
2. Malabsorption (weight loss, steatorrhea, osteomalacia, bleeding
tendency).
Features of choleangitis:
1. Fever 2. Rigor 3. Pain.
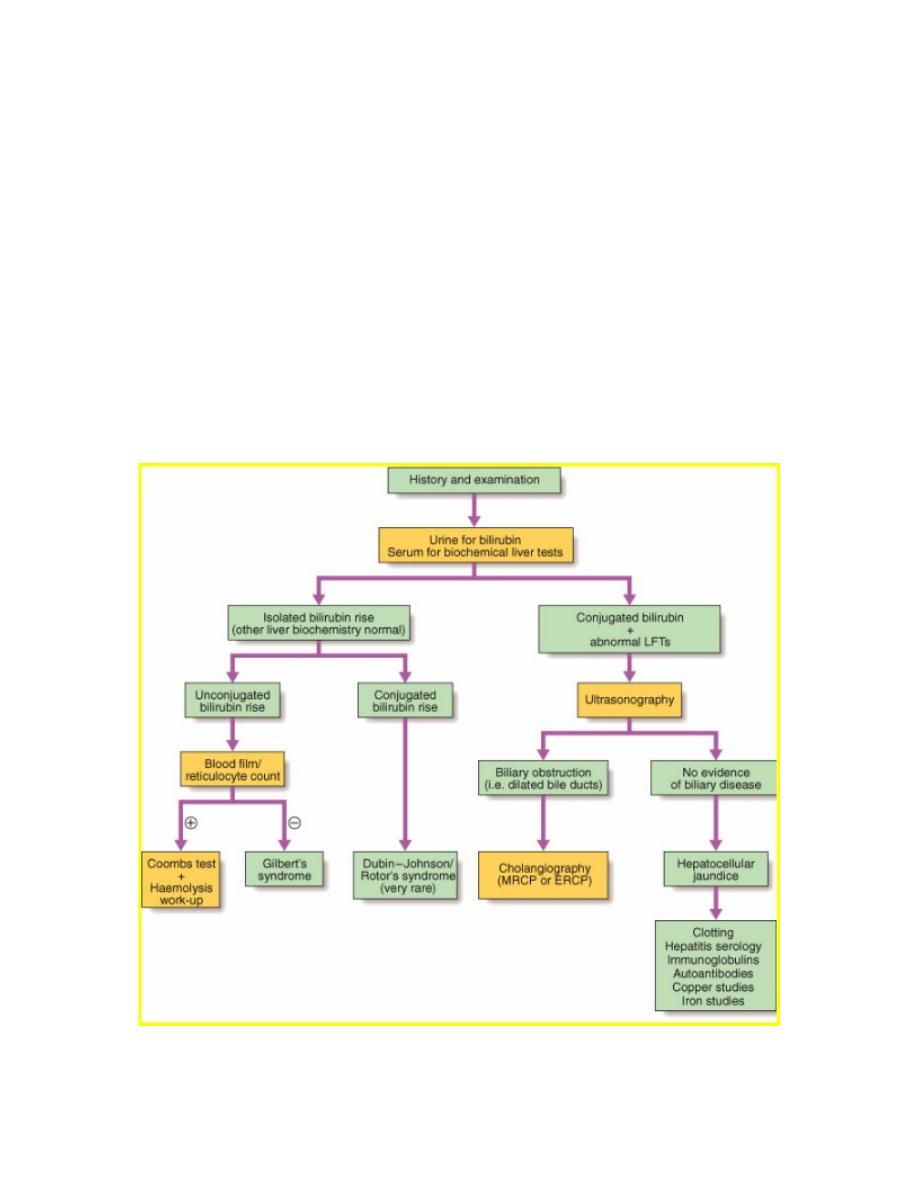
Early Investigations of Obstructive Jaundice
The history and clinical examination determine the investigation in
individual patients.
- Usually biochemistry tests show greater elevation of the alkaline
phosphatase and GGt compared with aminotransferases (ALT, AST).
- Ultrasound is performed to identify any biliary dilatation.
- Subsequent investigation is shown in next Schema.
Clinical Features suggesting an underlying cause of obstructive
jaundice:
1. Progressive, static or flacuating jaundic (carcinoma, stone, stricture,
pancreatitis).
2. Abdominal pain: (stone, pancreatitis, choedochal cyst).
3. Irregular hepatomegaly: (hepatic ca.)
4. Palpable gallbladder: (cancer below custic duct (usually pancreas))
5. Abdominal mass: (Ca, Pancreatic cyst, choledochal cyst)
6. Occult blood: Papillary tumour.
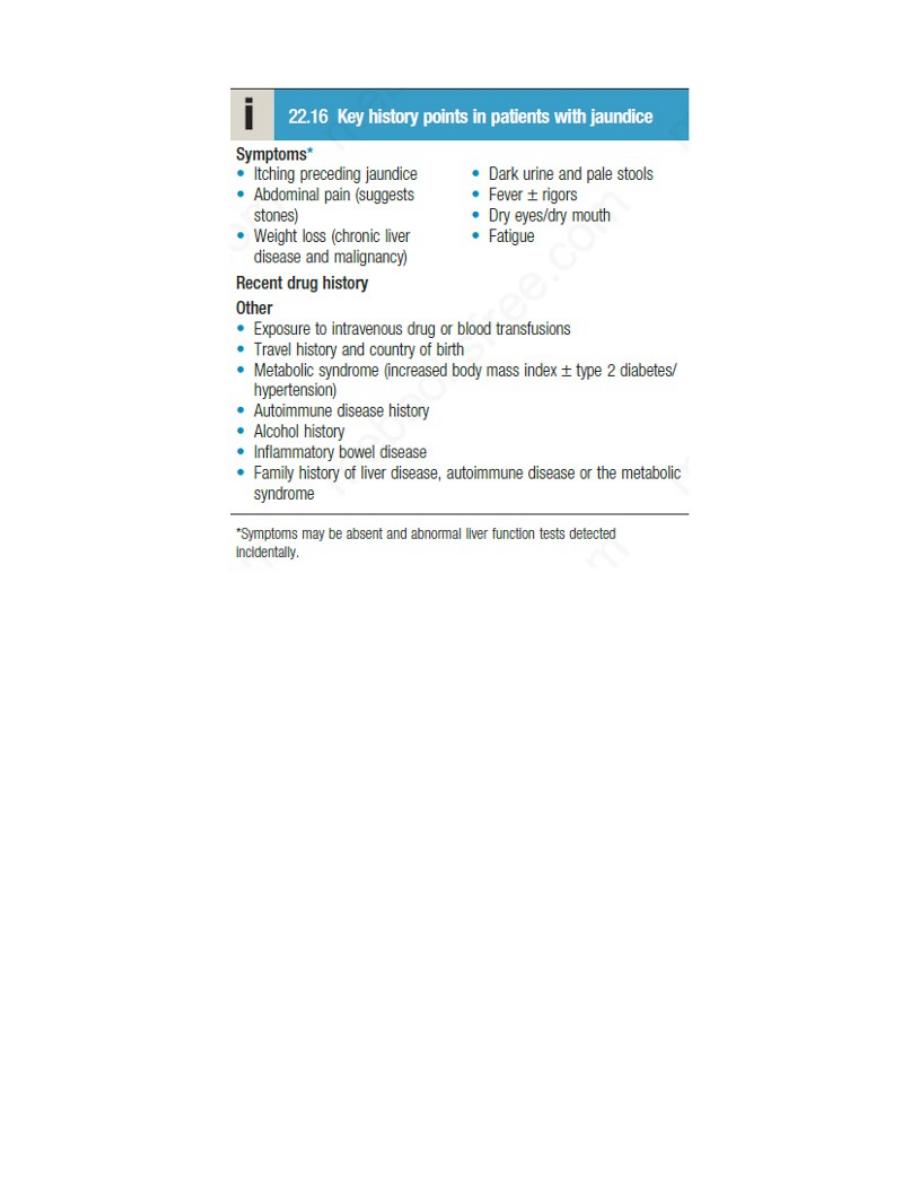
Take-home message
1. The history and clinical exam determine the investigations in individual
patients.
2. Obstructive jaundice shows greater elevation of the alkaline
phosphatase (ALP) and gama-glutamyltransferase (GGT) compared with
aminotransferases (ALT, AST) which are elevated in hepatocellular
jaundice.
3. Ultrasound is performed to identify any biliary dilatation in patients
with jaundice and an abnormal liver function test.
4. In isolated hyperbilirubinaemia, you must exclude hemolytic and
congenital non-hemolytic hyperbilirubinemia like Gilbert disease.
How to approach to a patient with jaundice?