Medicine
Notes…
1
Lecture.8 Presenting problems in renal and urinary tract disease
N
eed S
om
e H
el
p?
Medicine
Notes…
2
Loin pain
Loin pain is often caused by musculoskeletal disease but can be a manifestation of renal
tract disease; in the latter case, it may arise from renal stones, ureteric stones, renal
tumours, acute pyelonephritis and urinary tract obstruction. Acute loin pain radiating
anteriorly and often to the groin is termed renal colic. When combined with haematuria,
this is typical of ureteric obstruction due to calculi .
Dysuria
Dysuria refers to painful urination, often described as burning, scalding or stinging, and
commonly accompanied by suprapubic pain. It is often associated with frequency of
micturition and a feeling of incomplete emptying of the bladder. By far the most common
cause is urinary tract infection. Other diagnoses that need to be considered in patients
with dysuria include sexually transmitted infections and bladder stones .
Frequency
Frequency describes daytime micturition more often than a patient would expect. It
may be a consequence of polyuria, when urine volume is normal or high, but is also
found in patients with dysuria and prostatic diseases, when the urine volume is
normal.
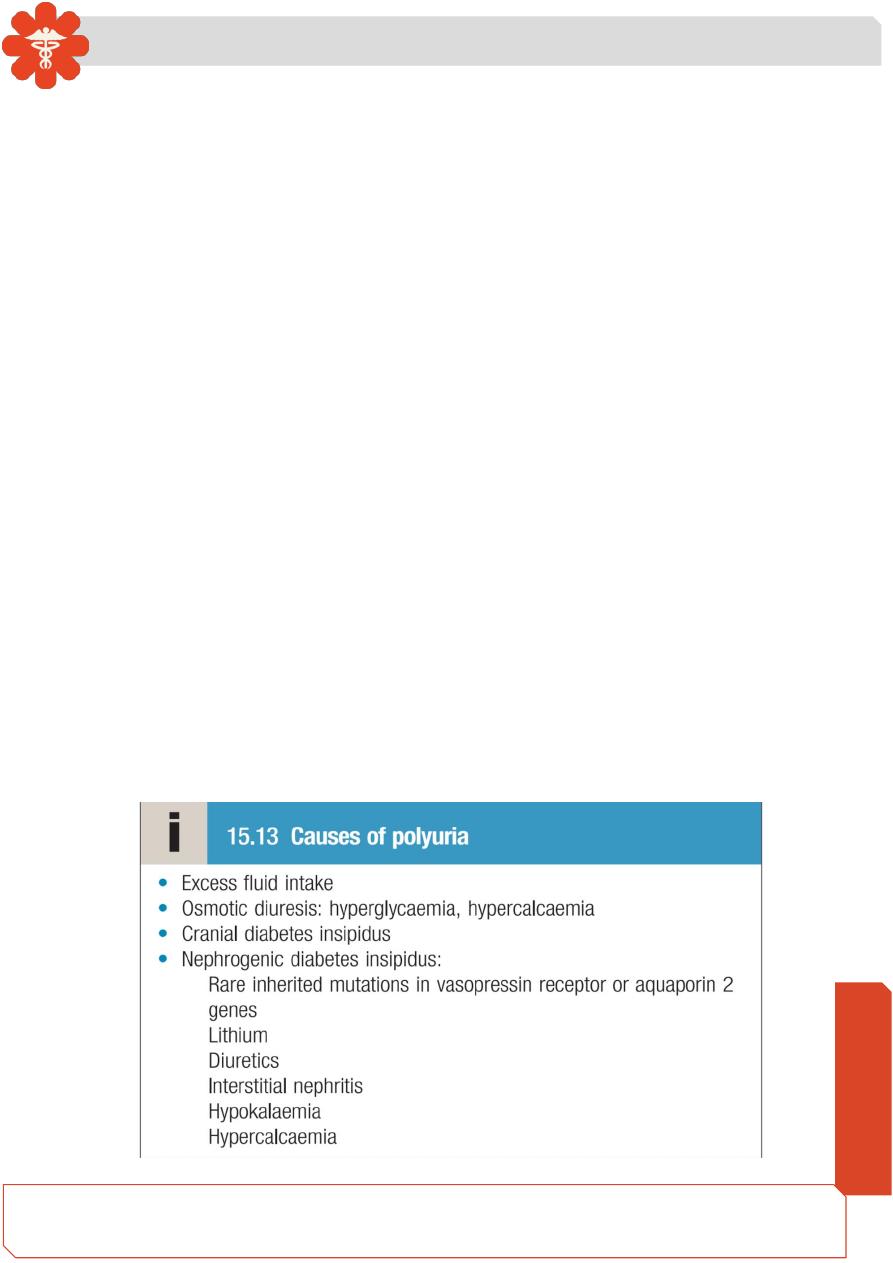
Polyuria
Polyuria is defined as a urine volume in excess of 3 L/24 hrs. Various underlying
conditions, both renal and extrarenal, may be responsible. Investigation of polyuria
includes measurement of urea, creatinine and electrolytes, glucose, calcium and
albumin. A 24-hour urine collection may be helpful to confirm the severity of
polyuria. The presence of nocturnal polyuria suggests a pathological cause.

Medicine
Notes…
3
Nocturia
Nocturia is defined as waking up at night to void urine. It may be a consequence of
polyuria but may also result from increased fluid intake or diuretic use in the late
evening (including caffeine). Nocturia also occurs in CKD, and in prostatic
enlargement when it is associated with poor stream, hesitancy, incomplete bladder
emptying, terminal dribbling and urinary frequency due to partial urethral
obstruction . Nocturia may also occur due to sleep disturbance without any
functional abnormalities of the urinary tract.
Urinary incontinence
Urinary incontinence is defined as any involuntary leakage of urine. It may occur in
patients with a normal urinary tract, as the result of dementia or poor mobility, or
transiently during an acute illness or hospitalisation, especially in older people.
types:
1- Stress : [bladder pressure exceeds the urethral pressure] , either due to weak pelvic
floor muscles or weak urethral sphincter.
incont. During coughing , sneezing , straining . more in women.
2- Urge : detrusor overactivity [ bladder pressure > urethral sphincter ]
Occur more in elderly ( > 65 y) , with some neurological conditions .
3- Continual: suggestive of fistula ( after surgery or radiotherapy) may occur with
advanced stress incontinence.
4
–Overflow : with chronically over distended bladder .
Either by bladder outflow obstruction or detrusor muscle failure ( atonic bladder )
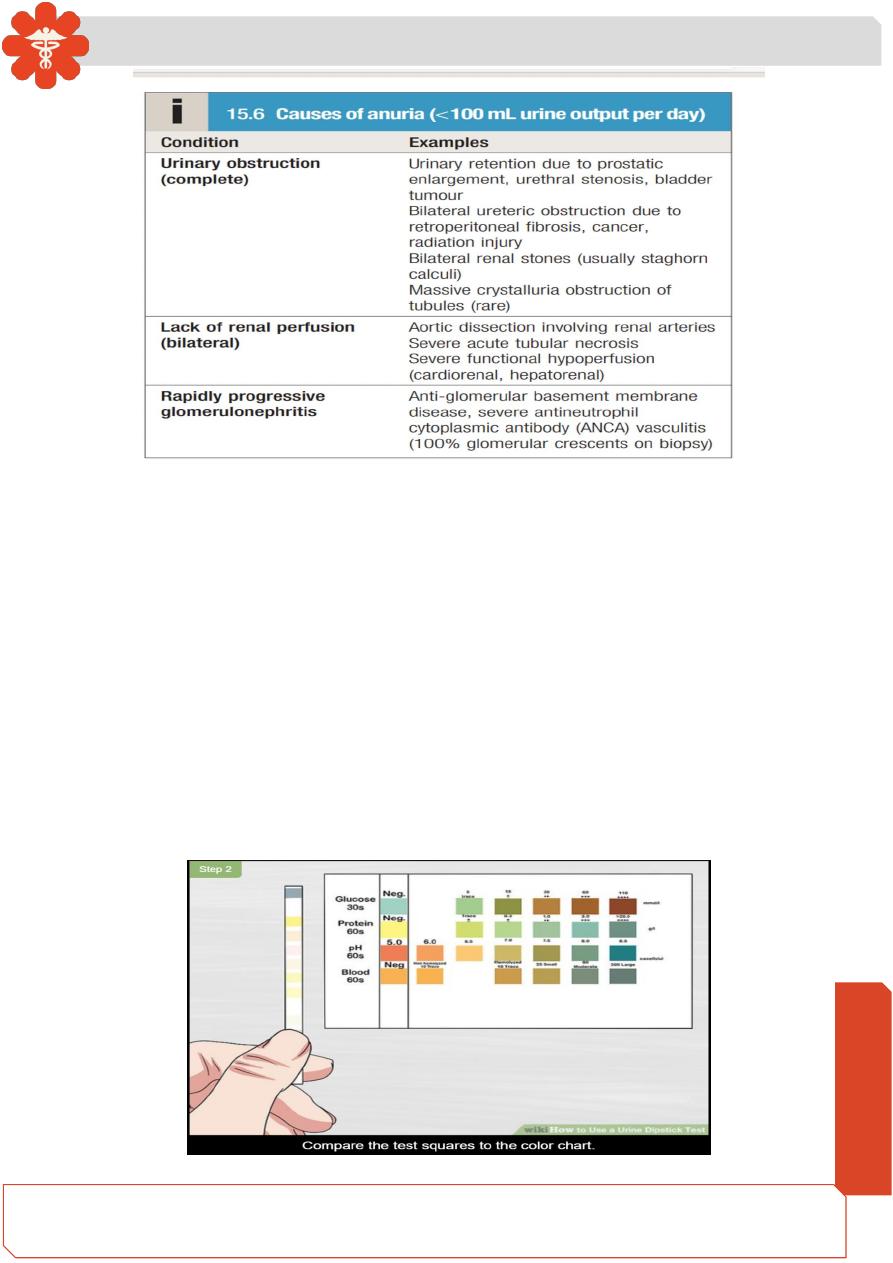
Oliguria/anuria
Oliguria: less than 400 mL of urine is passed per day, anuria: less than 100 mL of urine
is passed per day. Urine volume alone is a poor indicator of the severity of kidney disease.
Oliguria and anuria may be caused by a reduction in urine production, as in pre-renal AKI,
when GFR is reduced and tubular homeostatic mechanisms increase reabsorption to
conserve salt and water.
Obstruction of the renal tract can produce oliguria and anuria, but to do so, obstruction
must be complete and occur distal to the bladder neck, be bilateral, or be unilateral on the
side of a single functioning kidney.
Partial obstruction can be associated with a normal or even high urine volume due to
chronic tubular injury, which causes loss of tubular concentrating ability.
Medicine
Notes…
4
Hypertension
Hypertension is a very common feature of renal disease. Additionally, the presence
of hypertension identifies a population at risk of developing CKD and current
recommendations are that hypertensive patients should have renal function
checked annually. Control of hypertension is very important in patients with renal
impairment because of its close relationship with further decline of renal function
and because of the exaggerated cardiovascular risk associated with CKD.
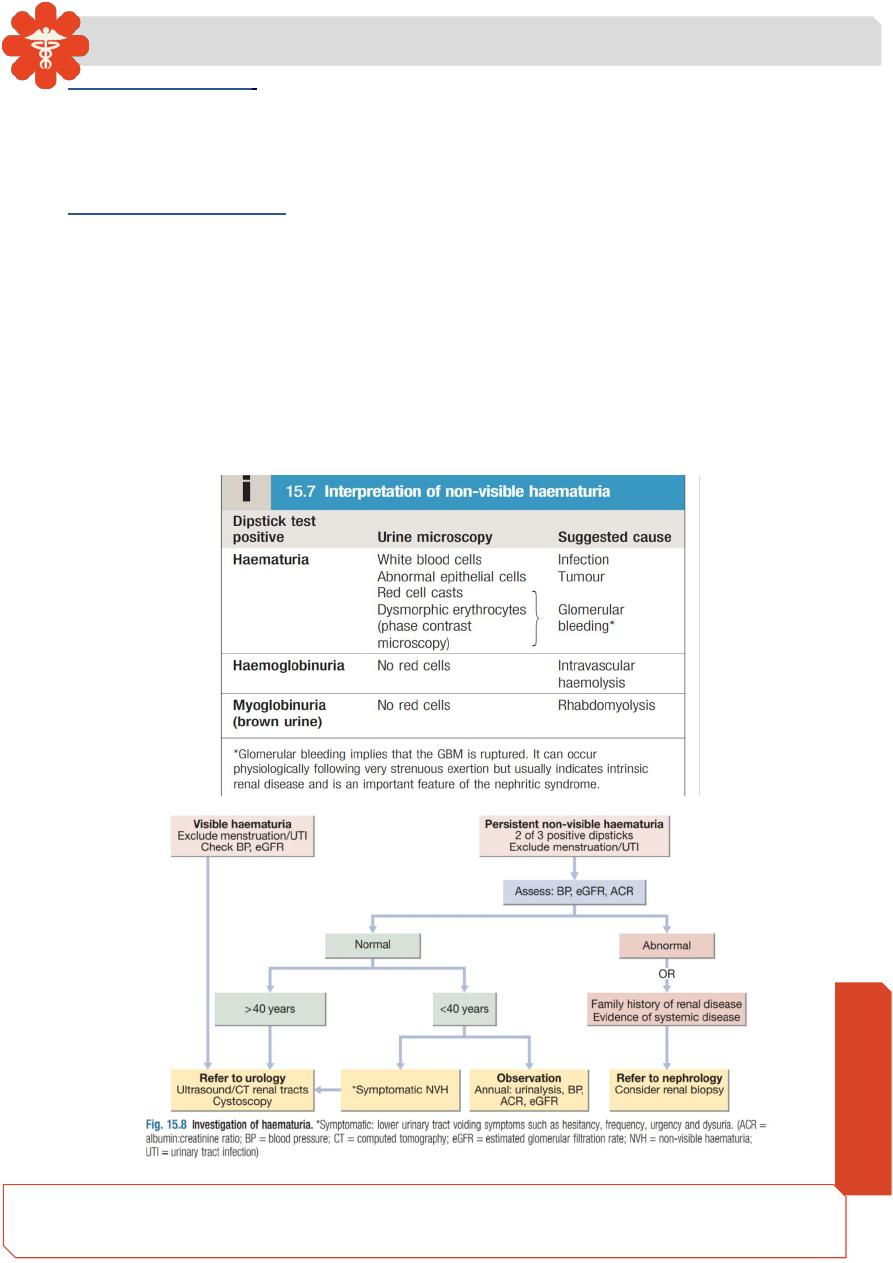
Haematuria
Healthy individuals may have occasional red blood cells in the urine (up to 12 500
cells/mL), but the presence of visible (macroscopic) haematuria or non-visible
haematuria (microscopic, only detectable on dipstick testing) is indicative of
significant bleeding from somewhere in the urinary tract .
Medicine
Notes…
5
Visible haematuria
is most likely to be caused by tumour, which can affect any part of
the urogenital tract. Other common causes of visible haematuria are urine infection and
stones. Visible haematuria may also be encountered in patients with IgA nephropathy,
typically following an upper respiratory tract infection.
Non-visible haematuria
may also indicate an underlying tumour, and all patients over 40
years old with persistent (detected on at least 2 of 3 consecutive dipstick tests) non-visible
haematuria should therefore undergo imaging and cystoscopy. In younger patients, an
underlying tumour is much less likely, and if aglomerular cause is not suspected (see
below), it may be appropriate to manage them by periodic observation in primary care.
Glomerular bleeding occurs when inflammatory, destructive or degenerative processes
disrupt the GBM, permitting passage of red blood cells into the urine. A characteristic
feature of glomerular bleeding is an ‘active urinary sediment’ (the presence of dysmorphic
red blood cells or red cell casts on microscopy); this is not always present, however.
Medicine
Notes…
6
Proteinuria
While very small amounts of high-molecular-weight proteins and moderate
amounts of low-molecular-weight proteins pass through the healthy GBM, these
proteins normally are completely reabsorbed by receptors on tubular cells. Hence,
in healthy individuals, less than 150 mg of protein is excreted in the urine each day,
much of which is derived from tubular cells.
The presence of larger amounts of protein is usually indicative of significant renal
disease.
Proteinuria is usually asymptomatic and is often picked up by urinalysis, although large
amounts of protein may make the urine frothy. Transient proteinuria can occur after
vigorous exercise, during fever, in heart failure and in people with urinary tract infection.
Testing for proteinuria is best done on an early morning sample, as some individuals
exhibit orthostatic proteinuria. In these patients, typically less than 1 g/24 hrs of protein is
excreted only in association with an upright posture, the first morning sample being
negative. Orthostatic proteinuria is regarded as a benign disorder that does not require
treatment.
Moderately elevated albuminuria(microalbuminuria)
May indicate early glomerular pathology, at a time when the standard dipstick test remains
negative . Screening for moderately elevated albuminuria should be performed regularly
in patients with diabetes, as persistently elevated levels warrant therapy with inhibitors of
the renin
–angiotensin–aldosterone system, even in normotensive individuals, to reduce
the rate of loss of renal function. Persistent moderately increased albuminuria has also
been associated with cardiovascular mortality in patients with and without diabetes.
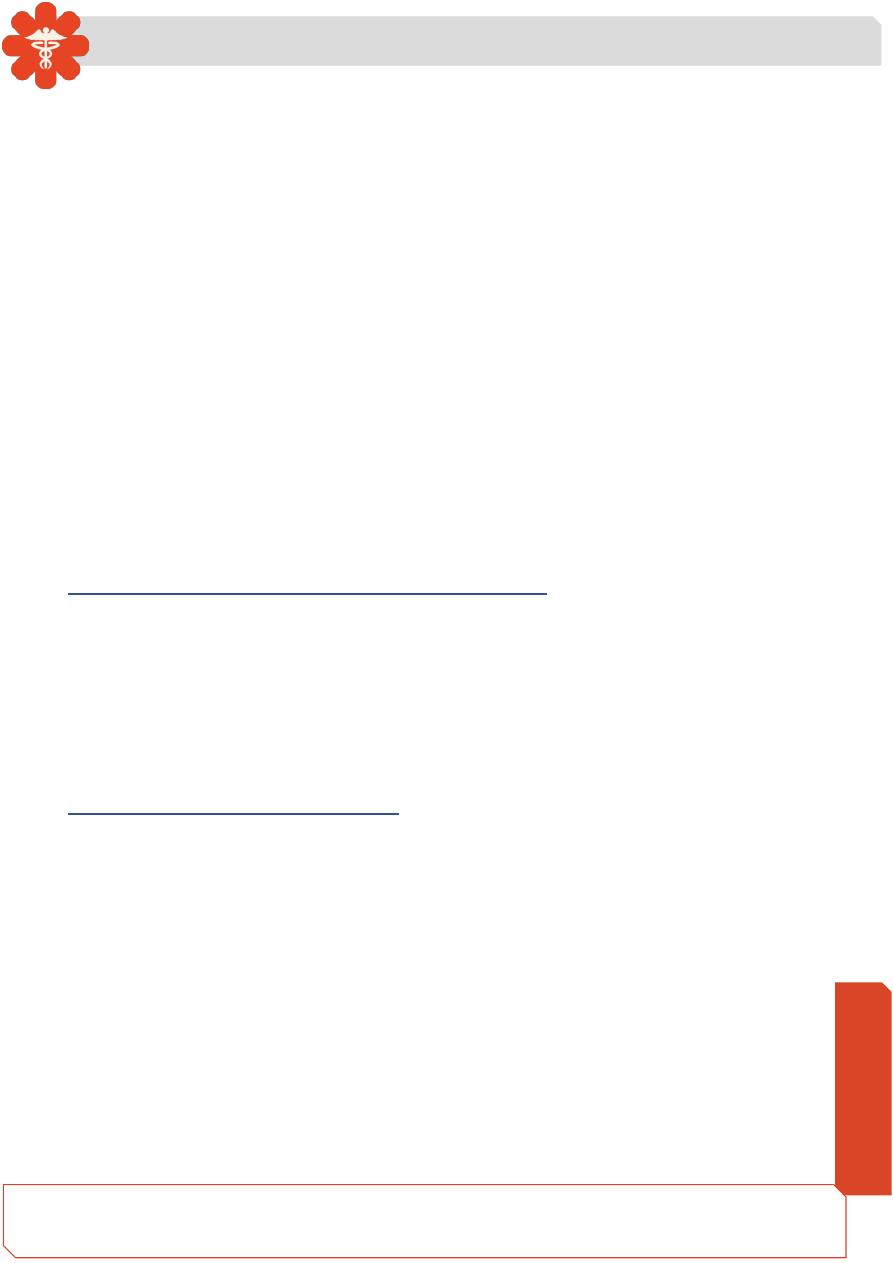
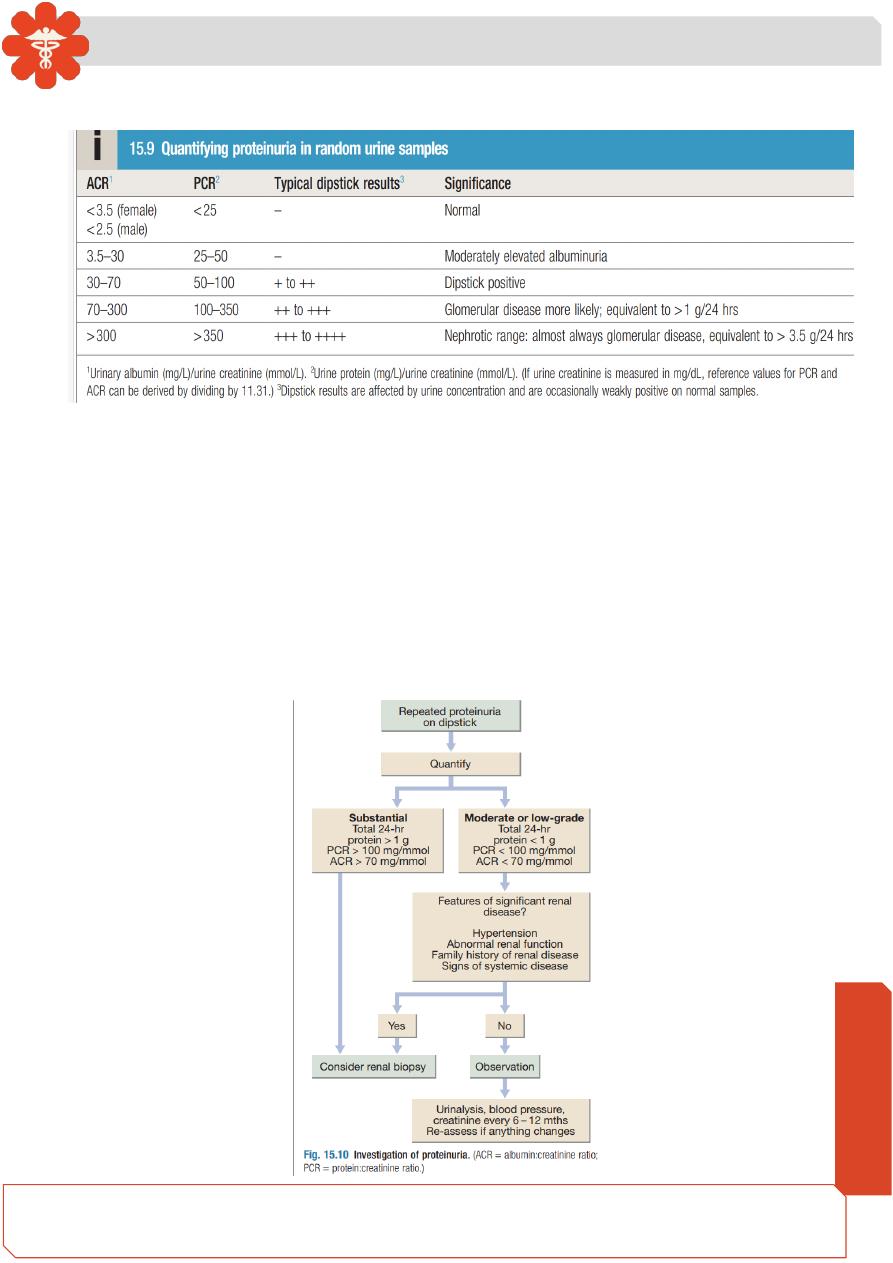
Overt (dipstick-positive) proteinuria
Typically, standard dipsticks test positive for protein once the urinary protein
exceeds approximately 0.5 g/24 hrs; however, trace to 1+ on dipstick may be
observed in very concentrated urine from individuals with no evidence of renal
pathology. Hence all patients with persistent proteinuria on dipstick should have the
amount of protein quantified to guide further investigations . When more than 1 g
of protein per day is being excreted, glomerular disease is likely and this is an
indication for renal biopsy.
Since quantification by 24-hour urine collection is often inaccurate, the protein:creatinine
ratio (PCR) in a spot sample of urine is preferred. It is possible to measure
albumin:creatinine ratio (ACR), but this requires a more expensive immunoassay and is
Medicine
Notes…
7
usually reserved for situations when high sensitivity is required, such as detection of the
early stages of diabetic nephropathy.
It is sometimes helpful to identify the type of protein in the urine. Large amounts of low-
molecular-
weight proteins, such as β2-microglobulin (molecular weight 12 kDa), in the
urine suggest renal tubular damage and are referred to as tubular proteinuria. This rarely
exceeds 1.5
–2 g/24 hrs (maximum PCR 150–200 mg/ mmol.
Free immunoglobulin light chains (molecular weight 25 kDa) are filtered freely at the
glomerulus but are poorly identified by dipstick tests. Hence, electrophoresis of the urine
and specific immunodetection methods are required to detect immunoglobulin light
chains, known as ‘Bence Jones protein’. This may occur in AL amyloidosis and in B-cell
dyscrasias but is particularly important as a marker for myeloma .
