Introduction to neurology
1 & 2
Manifestations of neurological diseases
د . بشار شاكر
The aim of the history is to address two key issues:
Where is the lesion and What is the lesion.
The key diagnostic questions
Is it neurological ? // If so, to which part of the nervous system does it
localise
Central versus peripheral // Sensory versus motor versus both
What is the lesion ?
Hereditary or congenital
Acquired
Traumatic / Infective / Neoplastic / Degenerative / Inflammatory or
immune-mediated / Vascular / Drug- induced / Nutritional / Toxins
/ Functional
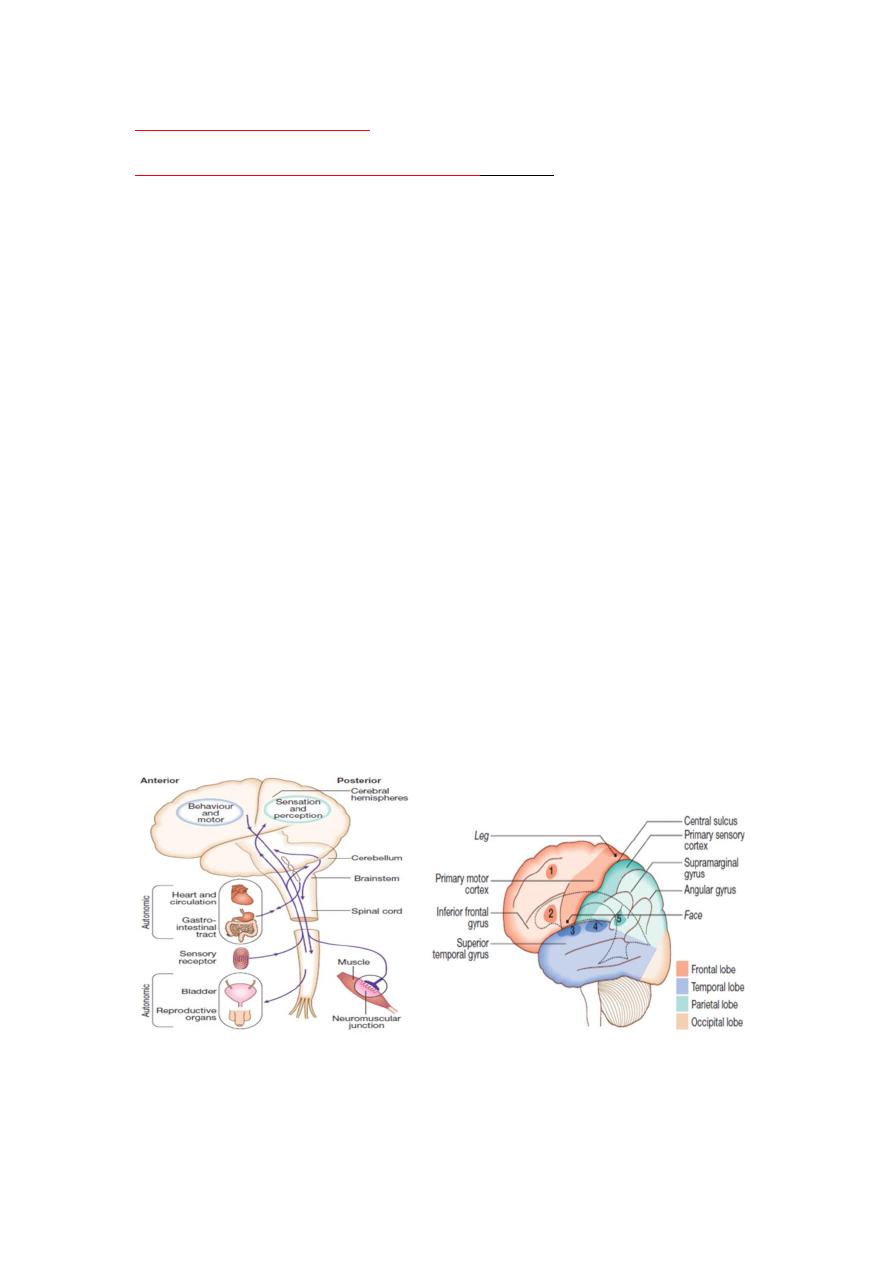
The major anatomical components of the nervous system
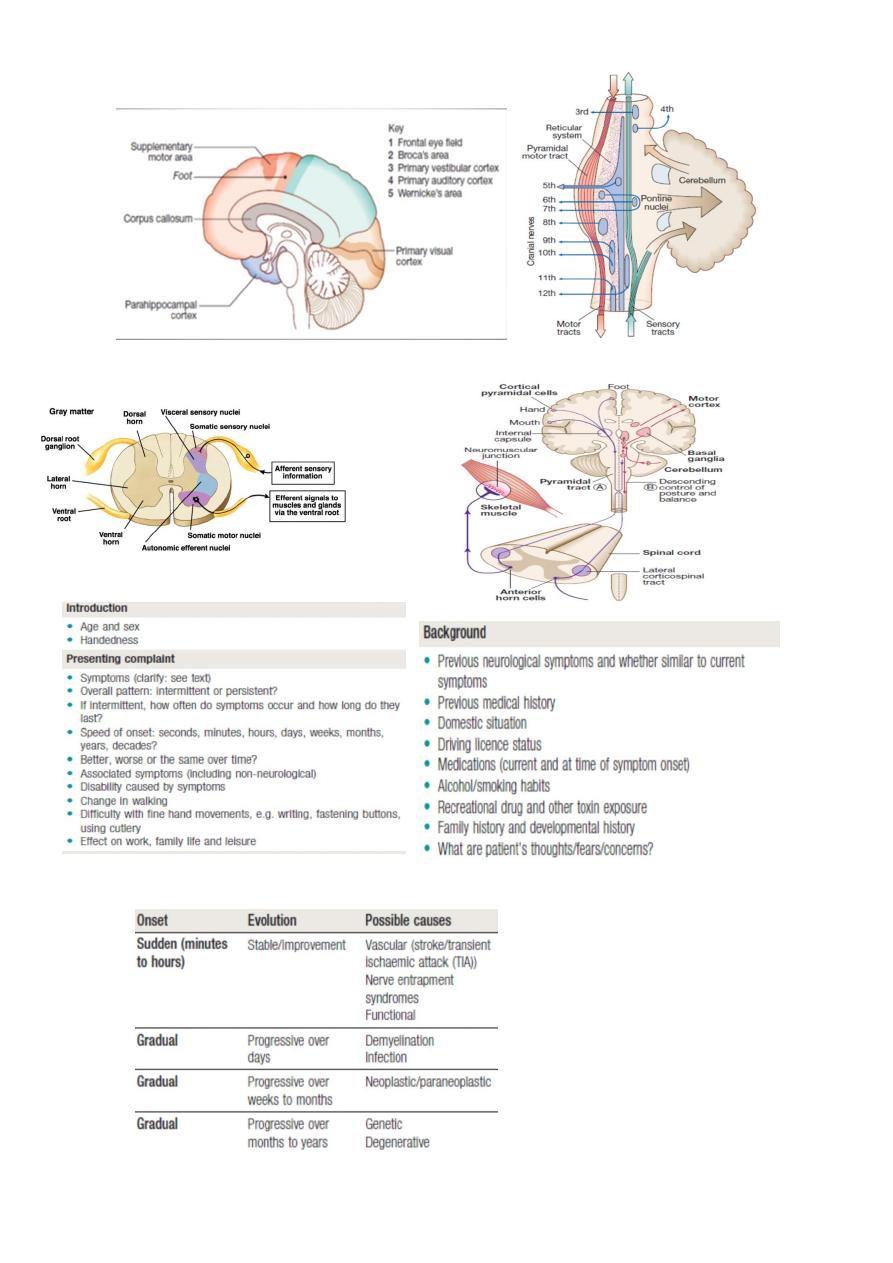
Determining the evolution, speed of onset and progression of a disease is important
The impact on day-to-day activities, such as walking, climbing stairs and
carrying out fine hand movements, should also be established in order
to gauge the level of associated disability.
Estimates of the frequency and duration of specific events are essential
when taking details of a paroxysmal disorder such as migraine and
epilepsy. Vague terms such as ‘a lot’ or ‘sometimes’ are unhelpful, and it
can assist the patient if choices are given to estimate numbers, such as
once a day, week or month
.
Cardinal symptoms
Headache and facial pain
Most headaches are chronic disorders but acute presentation of
headaches is an important aspect of emergency medical care. Headache
may be divided into primary (benign) or secondary. Site / Character /
Severity / Duration / Triggers ……… etc.
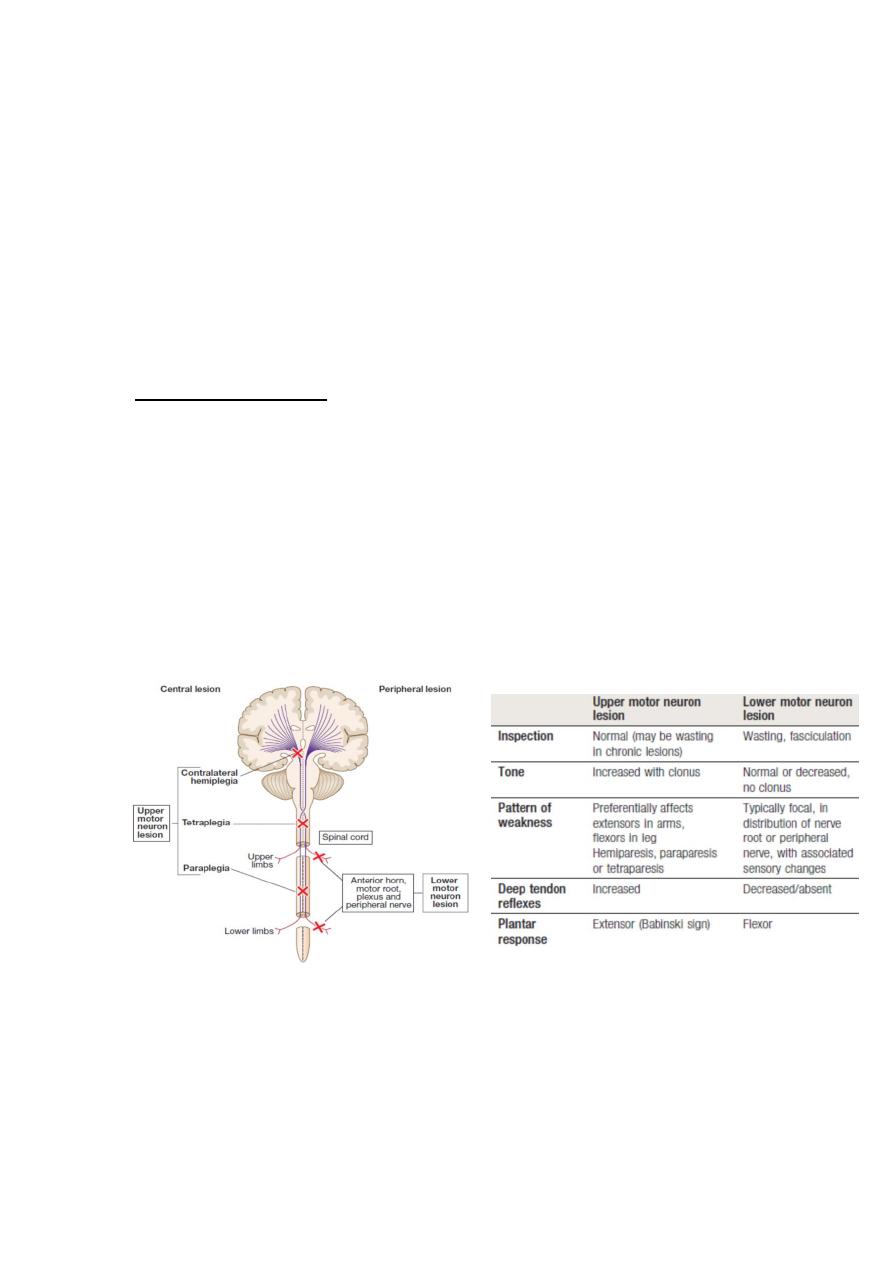
Weakness ( Paresis ) // Paralysis ( Plegia) Hemi – Mono – Para - Tetra
Patterns of motor loss according to the anatomical site of the lesion
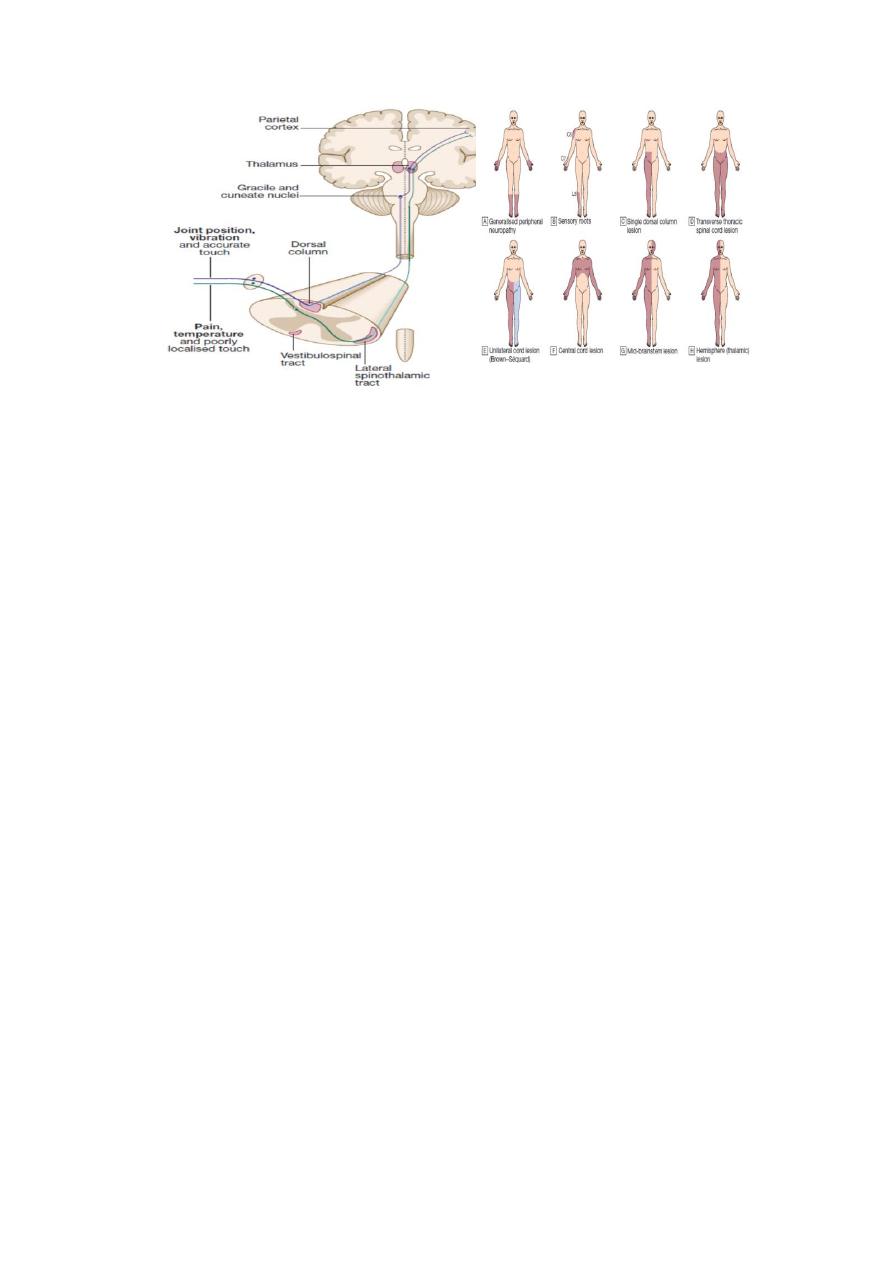
Sensory disturbance : Numbness and paraesthesia
Altered balance and vertigo
Balance is a complicated dynamic process that requires ongoing
modification of both axial and limb muscles to compensate for the
effects of gravity and alterations in body position and load (and hence
(centre of gravity) in order to prevent a person from falling.
This requires input from a variety of sensory modalities (visual,
vestibular and proprioceptive), processing by the cerebellum and
brainstem.
The patient may complain of different symptoms, depending on the
location of the lesion.
For example, loss of joint position sense or cerebellar function may
result in a sensation of unsteadiness
while damage to the vestibular
nuclei or labyrinth may result in an illusion of movement, such as
vertigo.
A careful history is vital
Since vision can often compensate for lack of joint position sense,
patients with peripheral neuropathies of dorsal column loss will often
find their problem more noticeable in the dark.
Vertigo is defined as an abnormal perception of movement of the
environment or self, and occurs because of conflicting visual,
proprioceptive and vestibular information about a person’s position in
space.
Abnormal speech
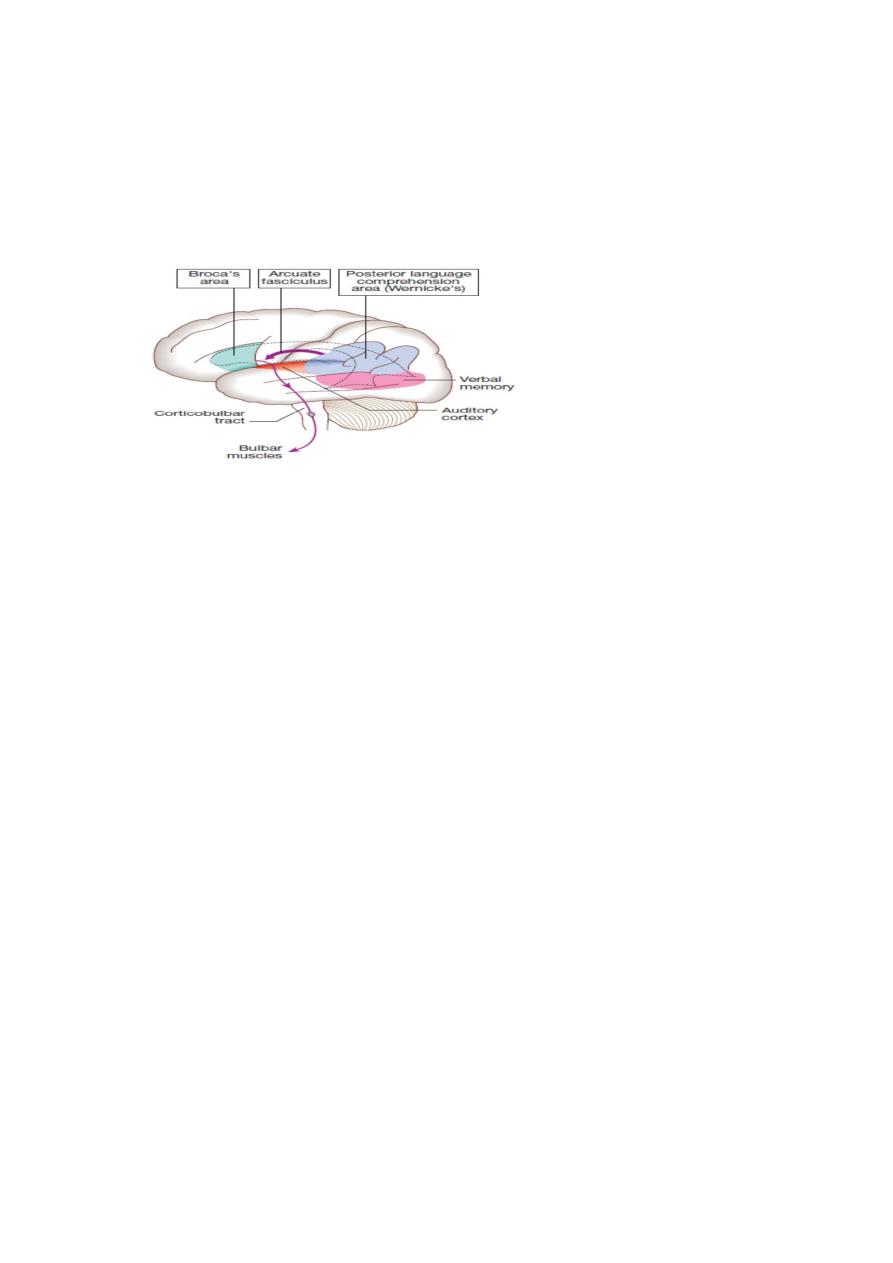
Areas of the cerebral cortex involved in the generation of spoken language
Dysarthria
Dysarthria is slurred speech caused by articulation problems due to a
motor deficit.
Disturbed articulation may result from lesions of the tongue, lips or
mouth, ill-fitting dentures or disruption of the neuromuscular pathways.
Cerebellar dysarthria may be slow and slurred, similar to alcohol
intoxication.
Myasthenia gravis is the most common cause of fatiguing speech.
Parkinsonism may cause dysarthria and dysphonia with a low-volume,
monotonous voice in which the words run into each other.
Dysphonia
Dysphonia is loss of volume caused by laryngeal disorders.
This usually results from either vocal cord pathology, as in laryngitis, or
damage to the vagal (X) nerve supply to the vocal cords (recurrent
laryngeal nerve). Inability to abduct one of the vocal cords leads to a
‘bovine’ (and ineffective) cough.
Dysphasia

Expressive (motor) dysphasia results from damage to Broca’s area. It is
characterised by reduced verbal output with non-fluent speech and
errors of grammar and syntax. Comprehension is intact.
Receptive (sensory) dysphasia occurs with dysfunction in Wernicke’s
area. There is poor comprehension, and although speech is fluent, it may
be meaningless and contain paraphasias (incorrect words) and
neologisms (nonsense or meaningless new words).
Global dysphasia is a combination of expressive and receptive difficulties
due to involvement of both areas.
Dysphasia (a focal sign) is frequently misdiagnosed as confusion (non-
focal sign). Always consider dysphasia before assuming confusion, as this
fundamentally alters the differential diagnosis and investigation plan.
Dominant parietal lobe lesions affecting the supramarginal gyrus may
cause dyslexia (difficulty comprehending written language), dyscalculia
(problems with simple addition and subtraction) and dysgraphia
(impairment of writing).
Disturbance of consciousness
Neurological or not // Continuous or episodic ( attacks)
Transient loss of consciousness
If patients are unaware of their symptoms, obtain a witness account.
This is more valuable than an unfocused neurological examination. Ask
the witness about symptoms before, during and after the TLOC – were
there any warning symptoms, any colour changes, did the patient lie still
or move, what was the patient like immediately afterwards ?
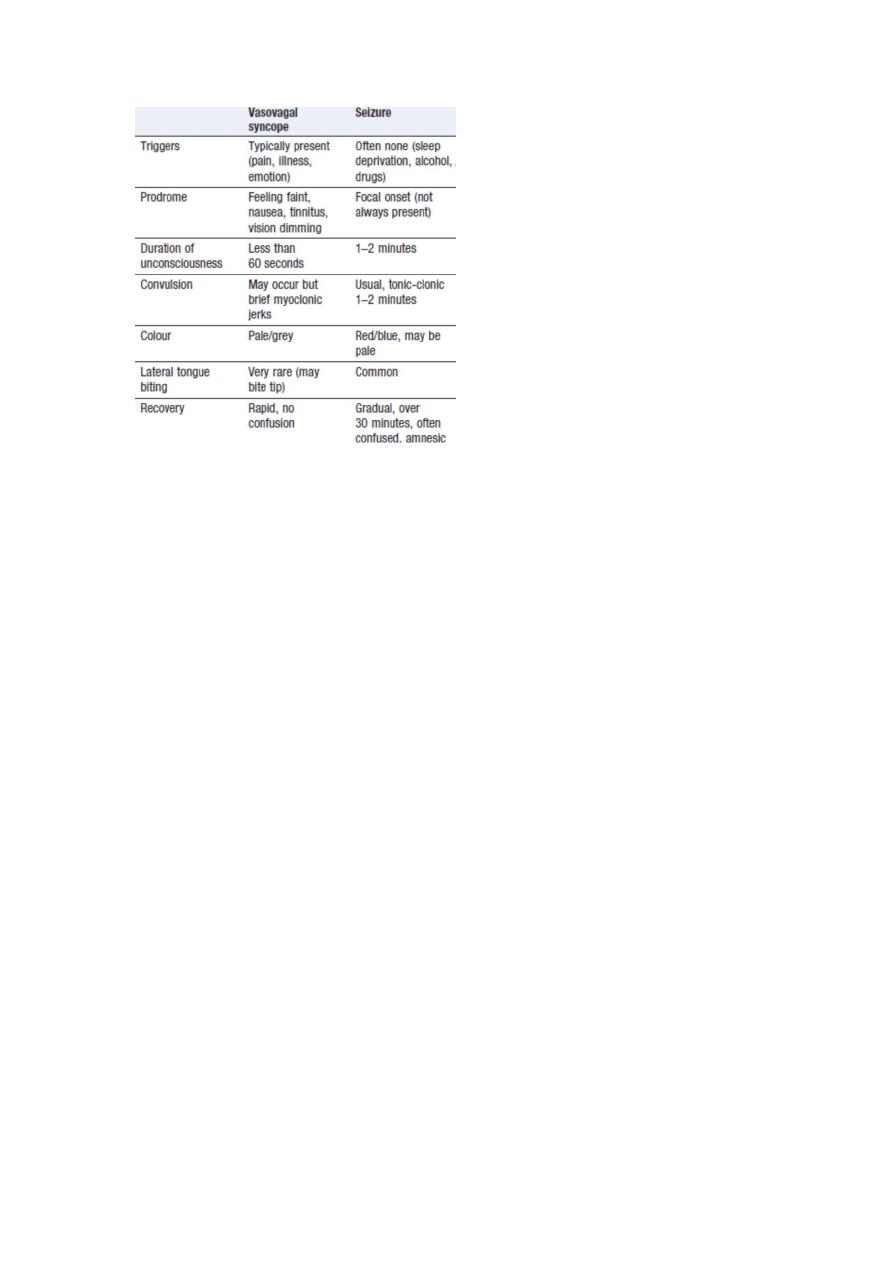
Fits ( Epilepsy ) vs Syncope
Grading of level of consciousness
GCS //Drowsy // Stuporous // Confused // Delerious // Unconscious
Memory disturbance (Amnesia )
Transient global amnesia // Persistent amnesia
Other symptoms
Visual symptoms // Visual acuity // Double vision // Hearing //
Swallowing // Bladder dysfunction // Sexual dysfunction
