
CONNECTIVE TISSUE DISEASES (CTD)s
Lecture TWO
Prof Sami Salman, FRCP, MRCP, DMR, CES, MB ChB
College of Medicine
University of Baghdad

systemic sclerosis
13-Oct-15
Connective Tissue Diseases SSalman
2

Generalised disorder of connective tissue affecting
the skin, internal organs and vasculature
Sclerodactyly with Raynaud’s or digital ischaemia
The peak age 4th and 5th decades
Prevalence 10–20 per 100 000
4:1 female
Diffuse cutaneous systemic sclerosis (DCSS; 30% of cases)
limited cutaneous systemic sclerosis (LCSS; 70% of cases).
Systemic sclerosis
13-Oct-15
Connective Tissue Diseases SSalman
3

‘CREST’ syndrome (Calcinosis, Raynaud’s,
oEsophageal involvement, Sclerodactyly and
Telangiectasia).
LCSS
13-Oct-15
Connective Tissue Diseases SSalman
4

The prognosis in DCSS is poor, with a 5-year
survival of approximately 70%.
Features that associate with a poor prognosis:
Older age
Diffuse skin disease
Proteinuria
High ESR
Low TLCO (gas transfer factor for carbon monoxide)
Pulmonary hypertension.
13-Oct-15
Connective Tissue Diseases SSalman
5

13-Oct-15
Connective Tissue Diseases SSalman
6

Cause is poorly understood.
Genetic component and associations with alleles at the HLA locus.
The disease occurs in all ethnic groups, and race may influence severity
since DCCS is significantly more common in black women.
Systemic sclerosis-like disease that has been triggered by exposure to
silica dust, vinyl chloride, hypoxyresins and trichloroethylene.
Immunological dysfunction; T lymphocytes infiltrate the skin
Abnormal fibroblast activation leading to increased production of
extracellular matrix in the dermis, primarily type I collagen.
This results in symmetrical thickening, tightening and induration of the
skin (sclerodactyly).
Arterial and arteriolar narrowing occurs due to intimal proliferation and
vessel wall inflammation.
Endothelial injury causes release of vasoconstrictors and platelet
activation, resulting in further ischaemia, which is thought to exacerbate
the fibrotic process.
Pathophysiology
13-Oct-15
Connective Tissue Diseases SSalman
7

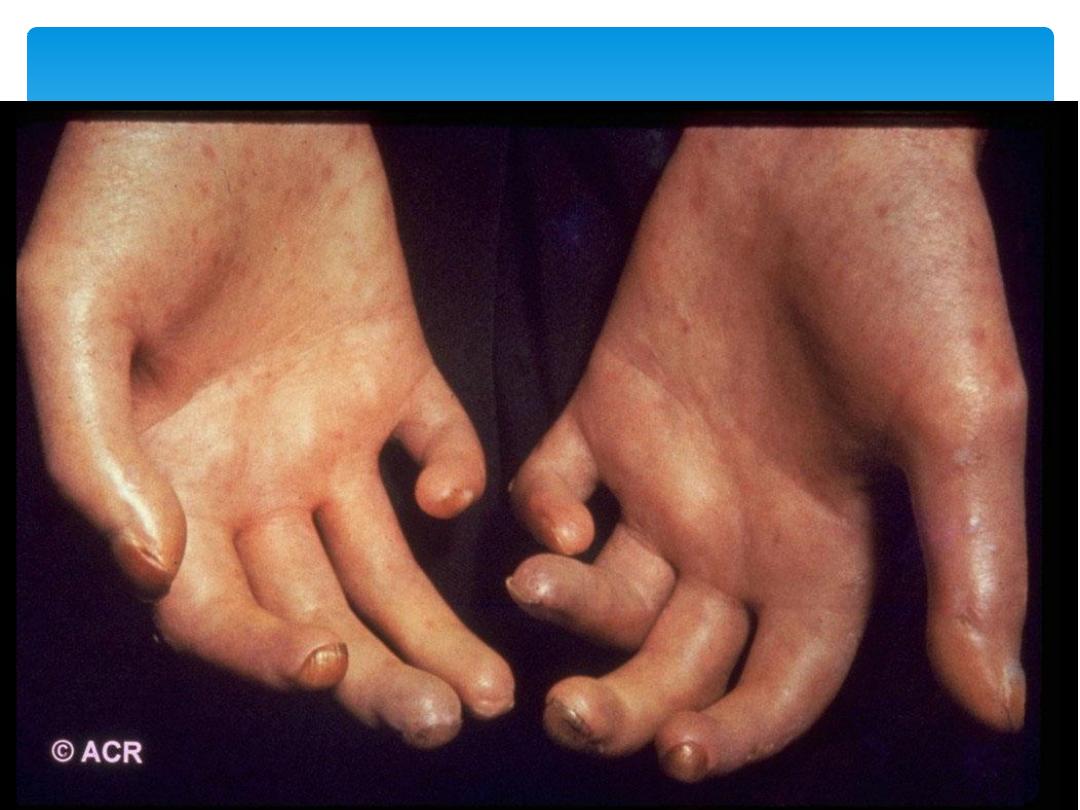
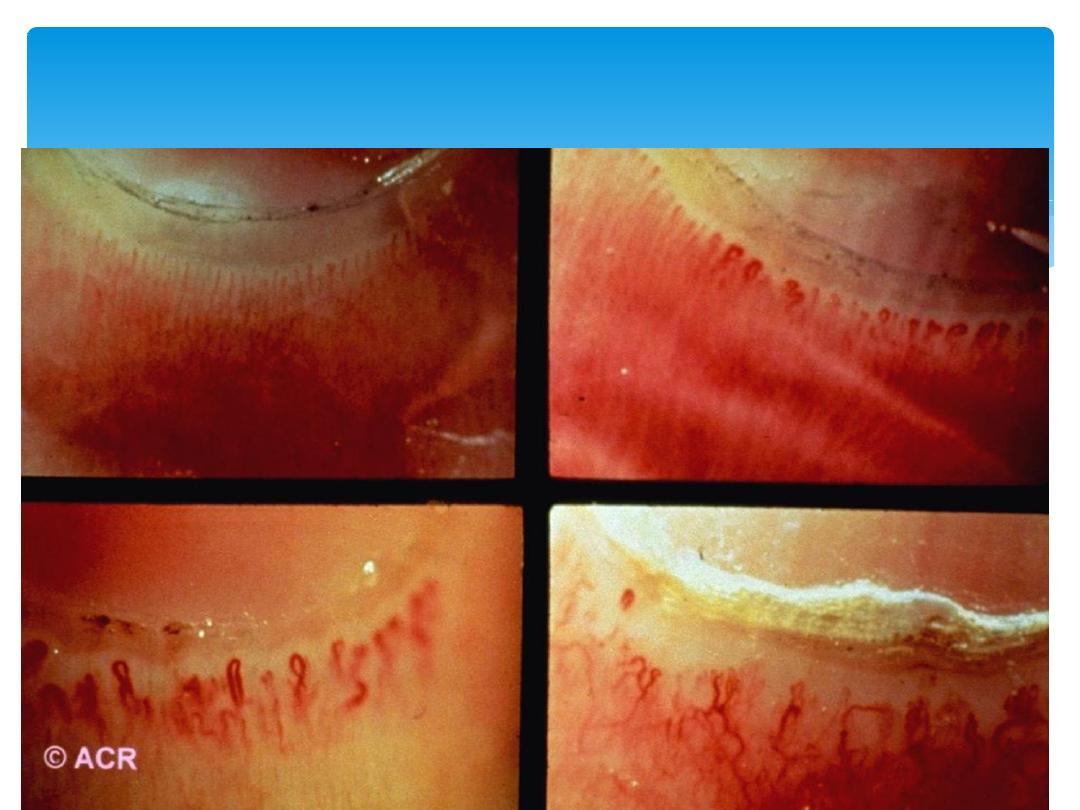
Skin
Initially there is non-pitting oedema of fingers and flexor
tendon sheaths. Subsequently, the skin becomes shiny
and taut, and distal skin creases disappear.
Erythema and tortuous dilatation of capillary loops in
the nail-fold bed, readily visible with an ophthalmoscope
or dissecting microscope (and oil placed on the skin).
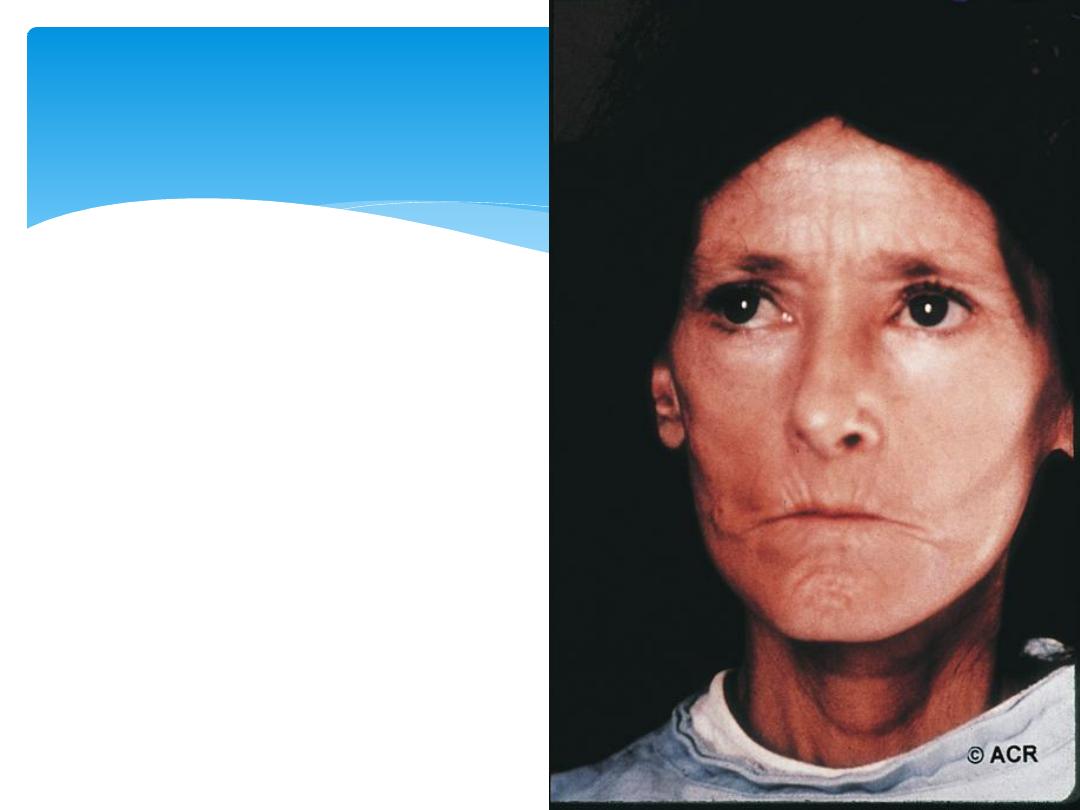
The face and neck are usually involved next, with
thinning of the lips and radial furrowing.
Skin involvement restricted to sites distal to the elbow
or knee (apart from the face) is classified as ‘limited
disease’ or CREST syndrome.
Involvement proximal to the knee and elbow and on the
trunk is classified as ‘diffuse disease’.
Clinical features
13-Oct-15
Connective Tissue Diseases SSalman
8

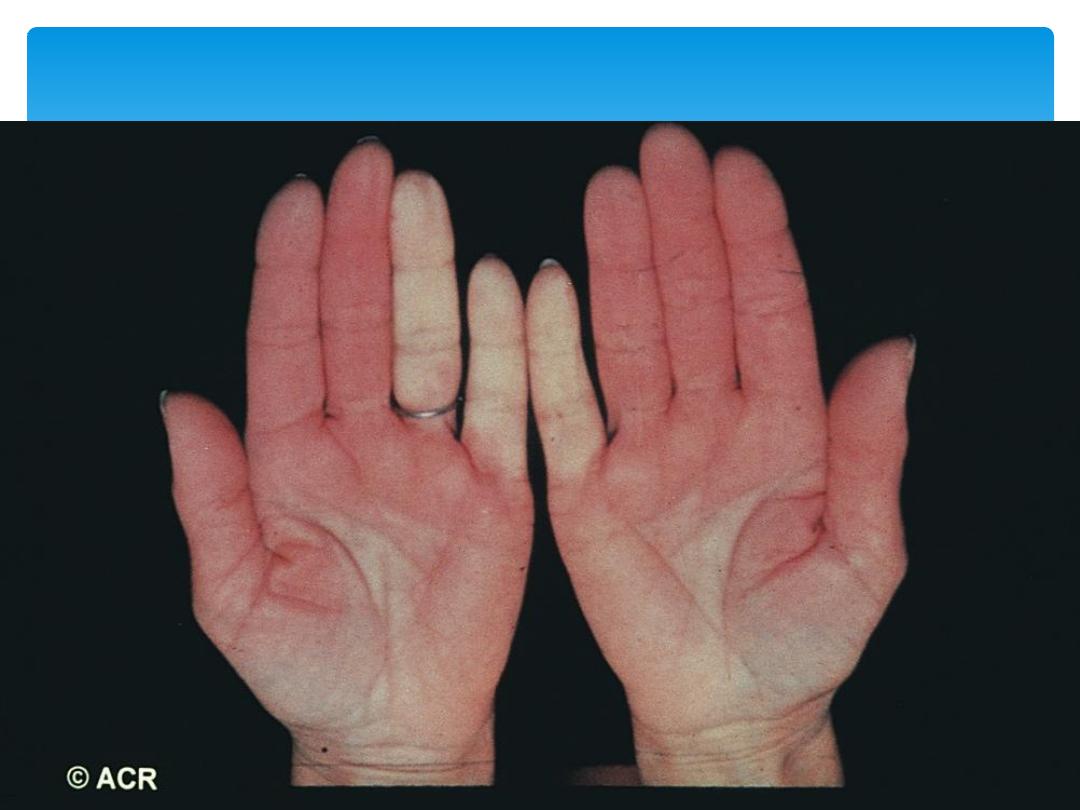
Raynaud’s phenomenon
This is a universal feature and can precede other
features by many years. Involvement of small blood
vessels in the extremities may cause critical tissue
ischaemia, leading To skin ulceration over pressure
areas, localised areas of infarction and pulp atrophy
at the fingertips.
Musculoskeletal features
Arthralgia, morning stiffness and flexor tenosynovitis
are common.
Restricted hand function is due to skin rather than
joint disease and erosive arthropathy is uncommon.
Muscle weakness and wasting can occur due to
myositis.
13-Oct-15
Connective Tissue Diseases SSalman
9

Gastrointestinal involvement
Smooth muscle atrophy and fibrosis in the lower two thirds of
the oesophagus lead to reflux with erosive oesophagitis.
Dysphagia and odynophagia may also occur.
Involvement of the stomach causes early satiety and
occasionally outlet obstruction.
Recurrent occult upper gastrointestinal bleeding may indicate a
‘watermelon’ stomach (antral vascular ectasia), which occurs in
up to 20% of patients.
Small intestine involvement may lead to malabsorption due
to bacterial overgrowth and intermittent bloating, pain or
constipation.
Dilatation of large or small bowel due to autonomic
neuropathy may cause pseudo-obstruction with nausea,
vomiting, abdominal discomfort and distension, often worse
after food.
13-Oct-15
Connective Tissue Diseases SSalman
10

Pulmonary involvement
This is a major cause of morbidity and mortality.
Pulmonary hypertension complicates long-standing disease and
is six times more prevalent in LCSS than in DCSS. It presents
with rapidly progressive dyspnoea (more rapid than interstitial
lung disease), right heart failure and angina, often in
association with severe digital ischaemia.
Fibrosing alveolitis mainly affects patients with DCSS who have
topoisomerase 1 antibodies.
Renal involvement
Hypertensive renal crisis characterised by rapidly developing
malignant hypertension and renal failure.
Hypertensive renal crisis is much more likely to occur in DCSS
than in LCSS, and in patients with topoisomerase 1 antibodies.
13-Oct-15
Connective Tissue Diseases SSalman
11
13-Oct-15
Connective Tissue Diseases SSalman
12

A clinical diagnosis but various laboratory
abnormalities:
ESR High
IgG High
CRP normal unless severe organ involvement or
coexisting infection.
ANA is positive in about 70%
Topoisomerase 1 (Scl-70) in 30% of DCSS.
Anticentromere antibodies in 60% of CREST.
Investigations
13-Oct-15
Connective Tissue Diseases SSalman
13
13-Oct-15
Connective Tissue Diseases SSalman
14
Raynaud’s Phenomenon
13-Oct-15
Connective Tissue Diseases SSalman
15
Sclerodactyly
13-Oct-15
Connective Tissue Diseases SSalman
16
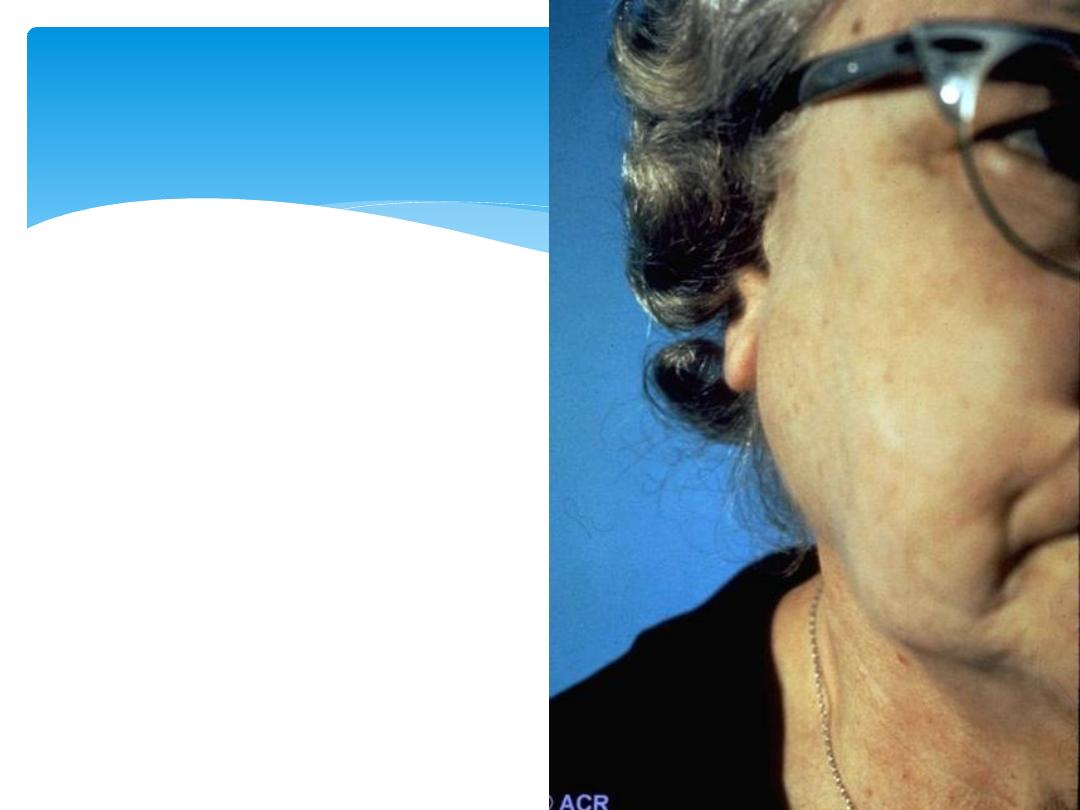
Systemic Sclerosis- face

13-Oct-15
Connective Tissue Diseases SSalman
17
Calcinosis (CREST)

13-Oct-15
Connective Tissue Diseases SSalman
18
Chronic Ulcer
13-Oct-15
Connective Tissue Diseases SSalman
19
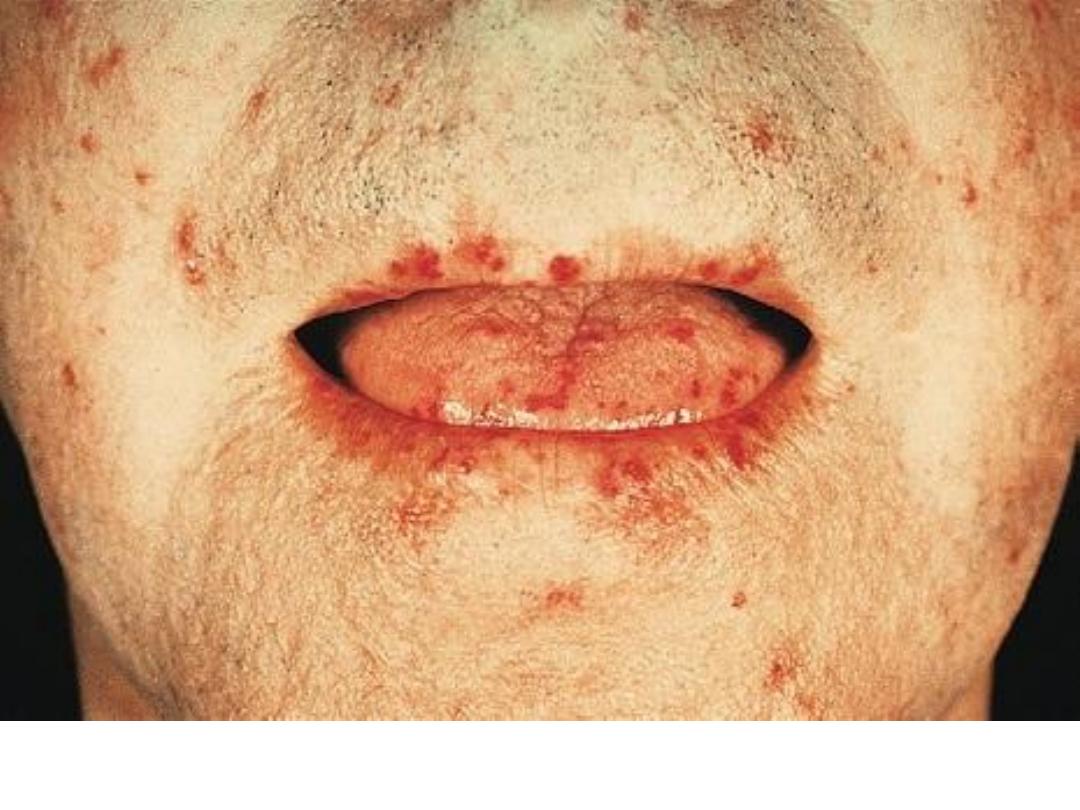
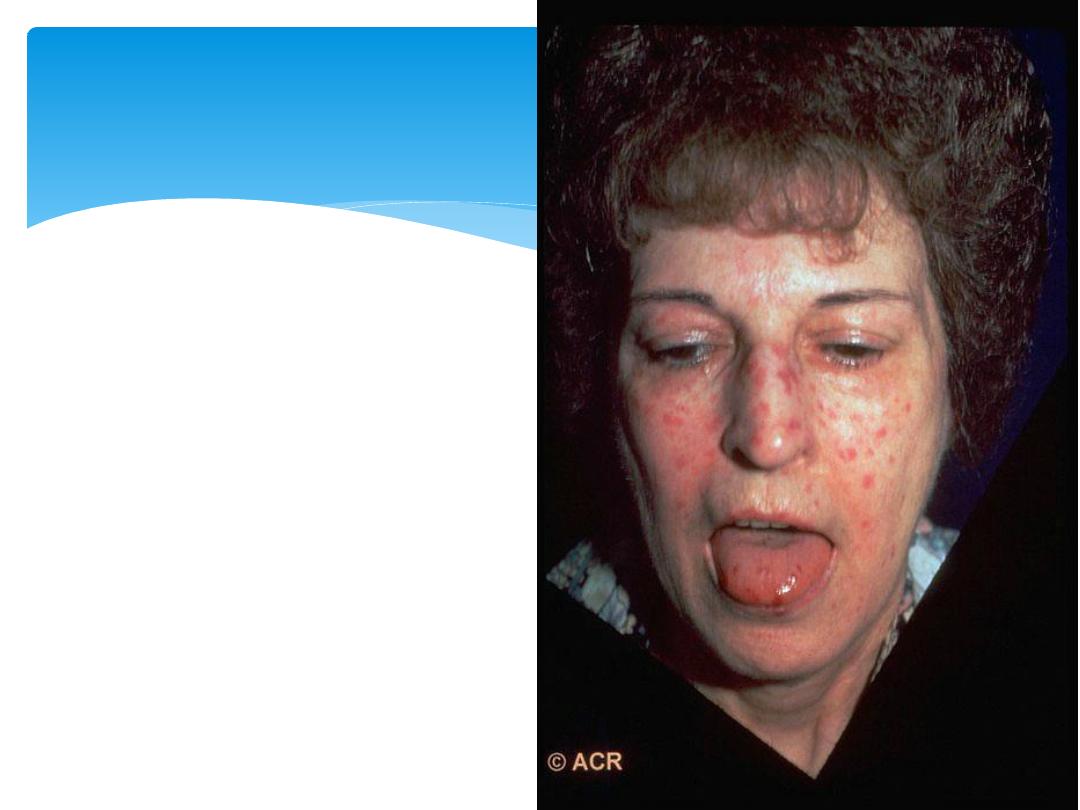
CREST- Face

13-Oct-15
Connective Tissue Diseases SSalman
20
Osteolysis
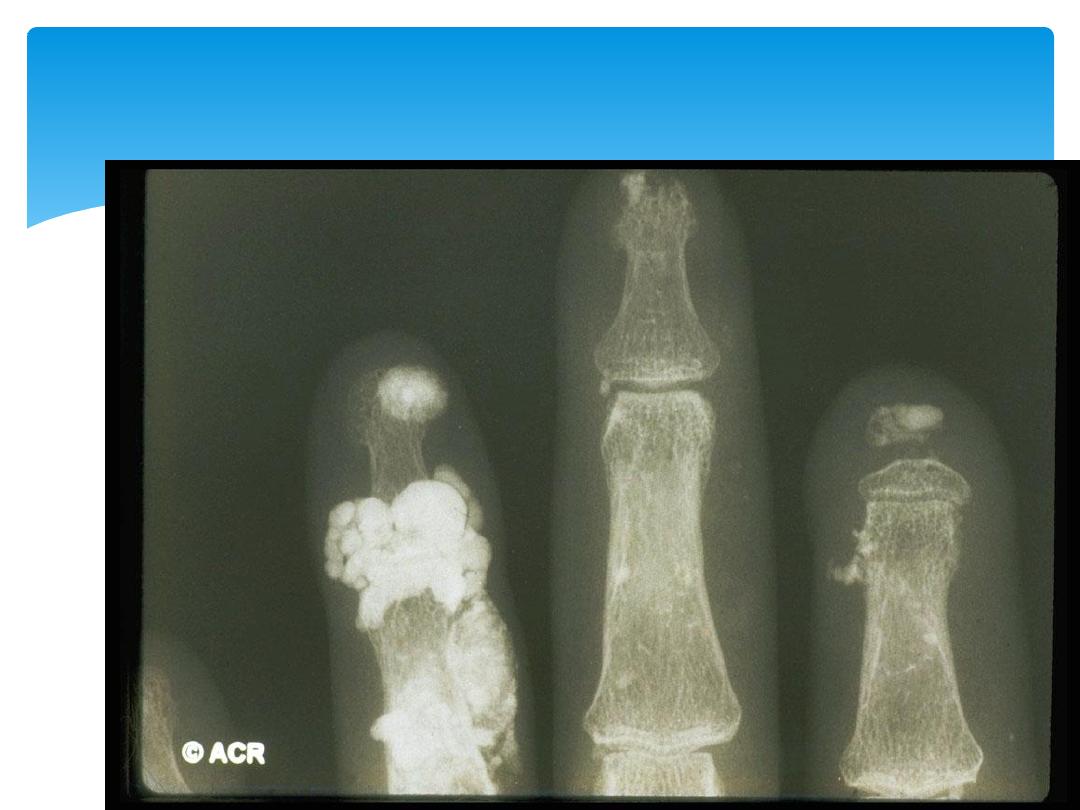
13-Oct-15
Connective Tissue Diseases SSalman
21
Calcinosis
13-Oct-15
Connective Tissue Diseases SSalman
22
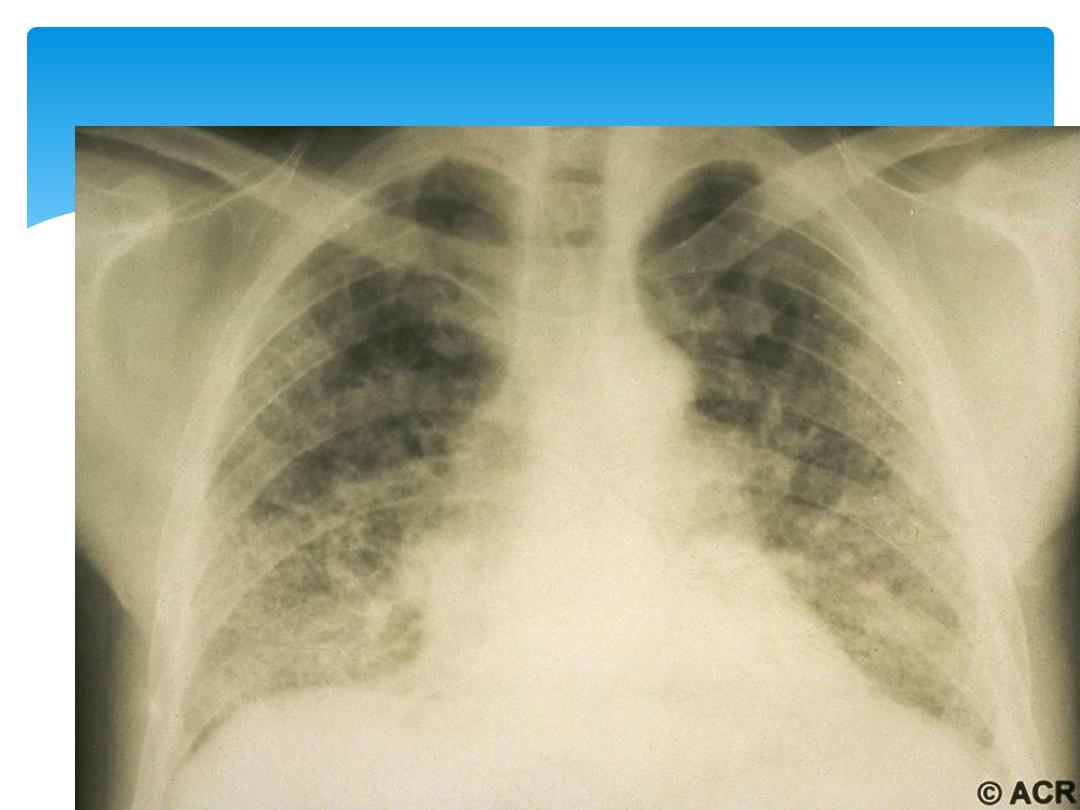
Pulmonary fibrosis
13-Oct-15
Connective Tissue Diseases SSalman
23
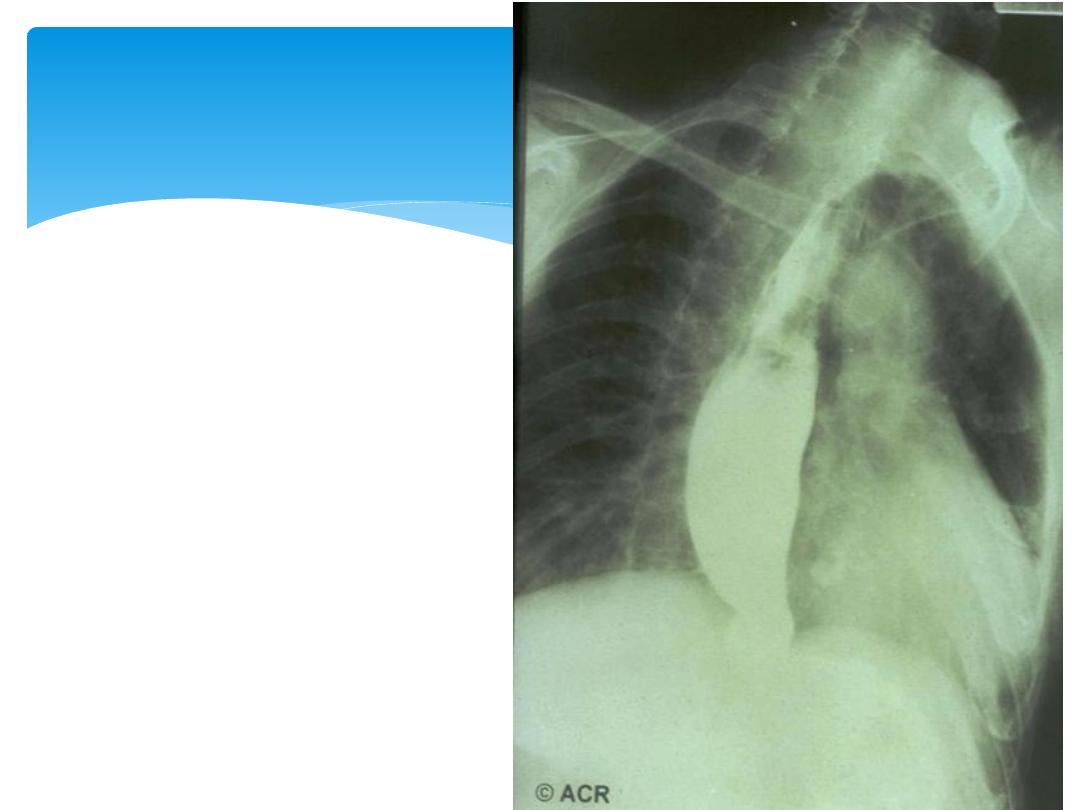
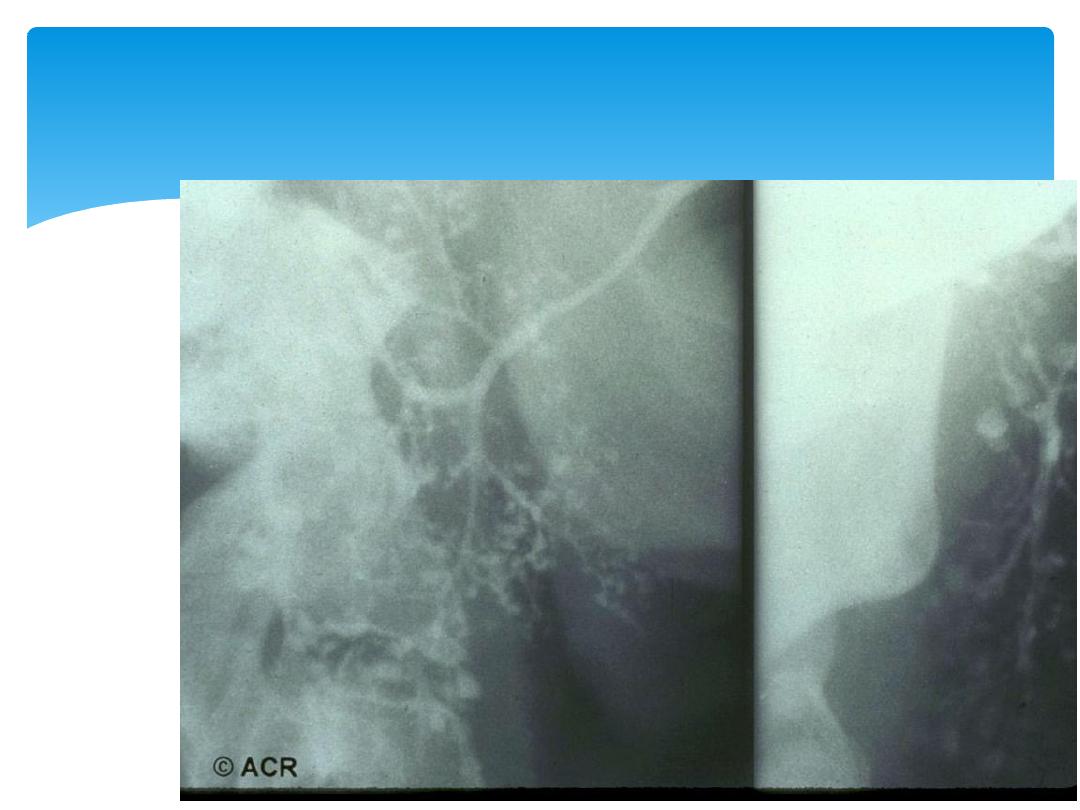
Oesophageal
obstruction and
dilatation

13-Oct-15
Connective Tissue Diseases SSalman
24
Diverticular dilatation

No treatments are available that halt or reverse the
fibrotic changes which underlie the disease.
Raynaud’s syndrome and digital ulcers
Avoidance of cold exposure and use of mittens
Calcium antagonists
Angiotensin II receptor blockers
Intermittent infusions of epoprostenol
Ulcerated skin require treatment with antibiotics, but
as these penetrate tissues poorly in scleroderma they
need to be given at higher doses for longer courses
than usual.
Management
13-Oct-15
Connective Tissue Diseases SSalman
25

GIT
Oesophageal reflux : PPIs and anti-reflux agents.
Antibiotics for bacterial overgrowth syndromes
Metoclopramide or Domperidone for pseudo-obstruction.
Hypertension
Angiotensin-converting enzyme (ACE) inhibitors, even if renal
impairment is present.
Joint involvement may be treated with analgesics.
Pulmonary hypertension
Endothelin 1 antagonist, bosentan
Corticosteroids and cytotoxic drugs are indicated in patients
who have coexisting myositis or fibrosing alveolitis.
Heart-lung transplantation
Management
13-Oct-15
Connective Tissue Diseases SSalman
26

mixed connective tissue disease
13-Oct-15
Connective Tissue Diseases SSalman
27

Overlap of clinical features of SLE, systemic
sclerosis and myositis.
Synovitis and oedema of the hands with
Raynaud’s phenomenon and muscle
pain/weakness.
Most patients have anti ribonucleoprotein (RNP)
antibodies
Management: treating the individual
components of the syndrome.
mixed connective tissue disease
13-Oct-15
Connective Tissue Diseases SSalman
28

Sjögren’s syndrome
13-Oct-15
Connective Tissue Diseases SSalman
29

This is an autoimmune disorder of unknown cause
characterised by lymphocytic infiltration of
salivary and lachrymal glands, leading to glandular
fibrosis and exocrine failure.
Age of onset is between 40 and 50
9:1 female.
Primary or secondary to other autoimmune
diseases.
Sjögren’s syndrome
13-Oct-15
Connective Tissue Diseases SSalman
30

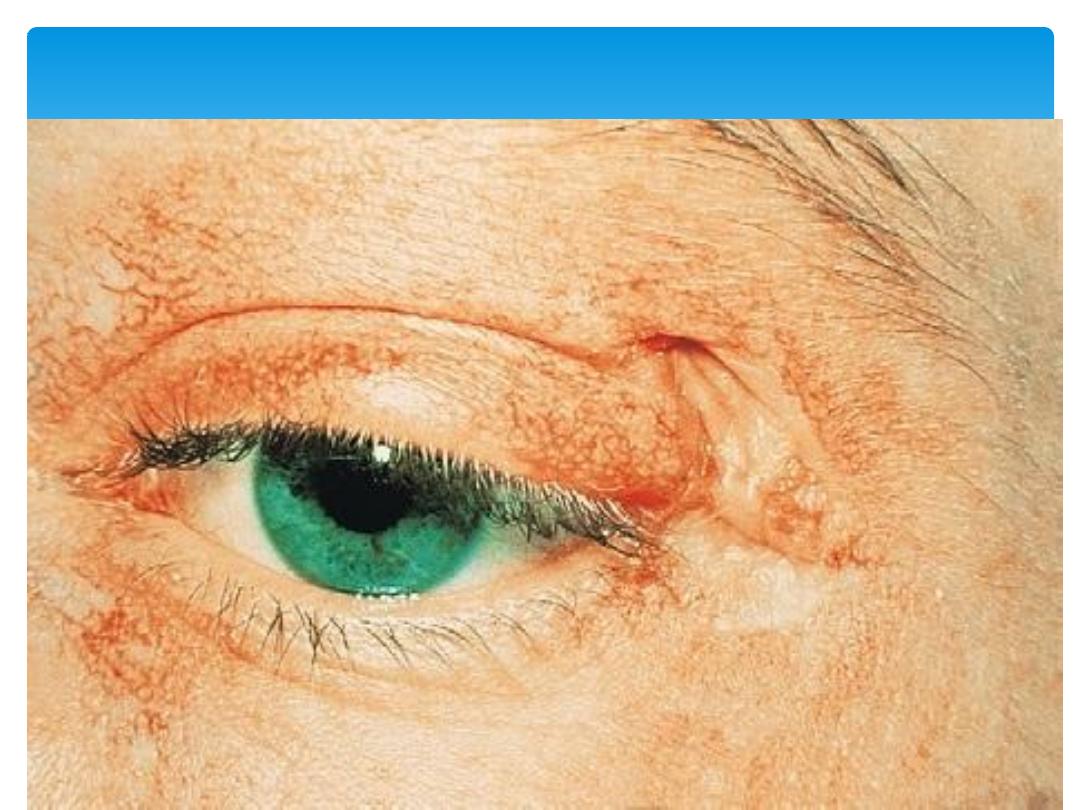
The eye symptoms
Keratoconjunctivitis sicca, are due to lack of
lubricating tears.
Conjunctivitis and blepharitis may lead to Filamentary
keratitis due to tenacious mucous filaments binding
to the cornea and conjunctiva.
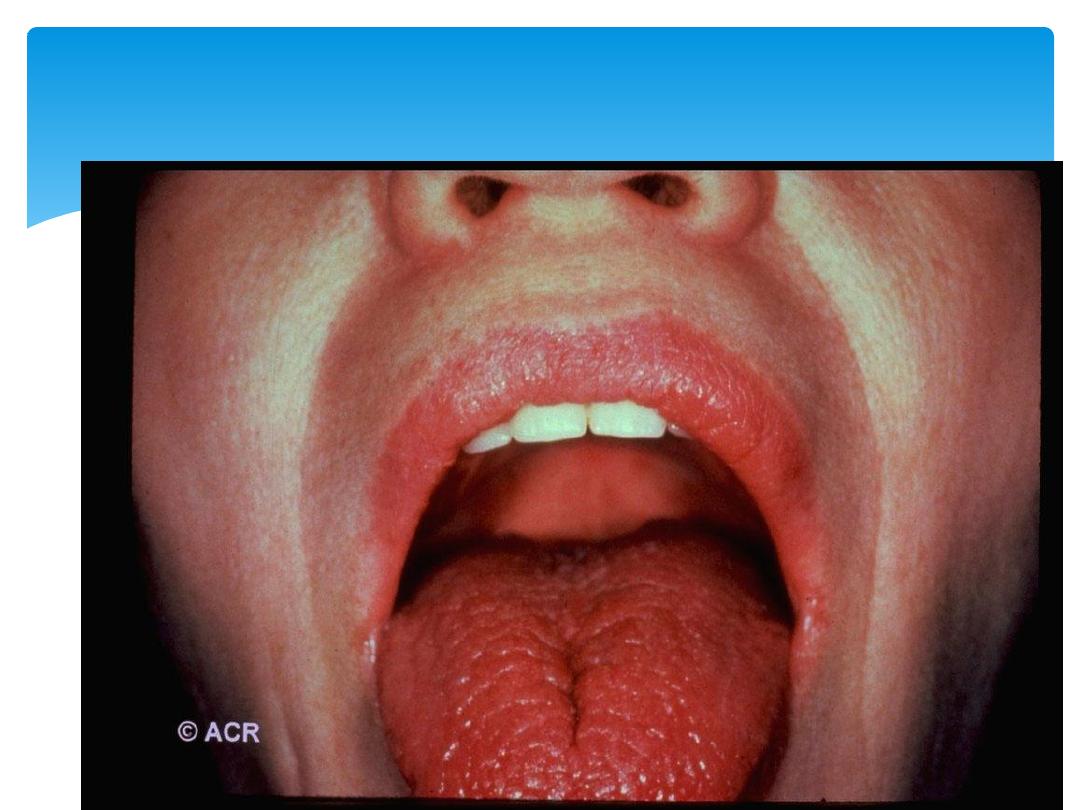
Oral
Dry mouth and typically the patient needs water to
swallow food.
Dental caries.
The disease is associated with a 40-fold increased
lifetime risk of lymphoma.
Clinical features
13-Oct-15
Connective Tissue Diseases SSalman
31
13-Oct-15
Connective Tissue Diseases SSalman
32
Parotid swelling
13-Oct-15
Connective Tissue Diseases SSalman
33
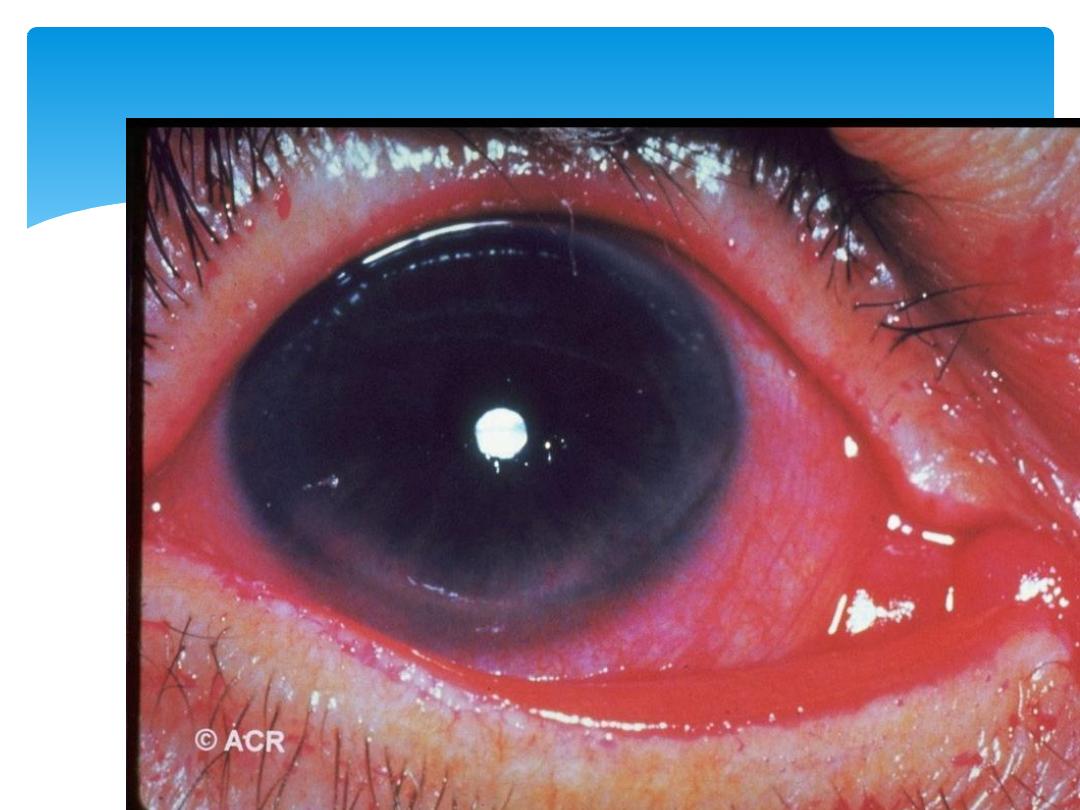
Keratitis
13-Oct-15
Connective Tissue Diseases SSalman
34
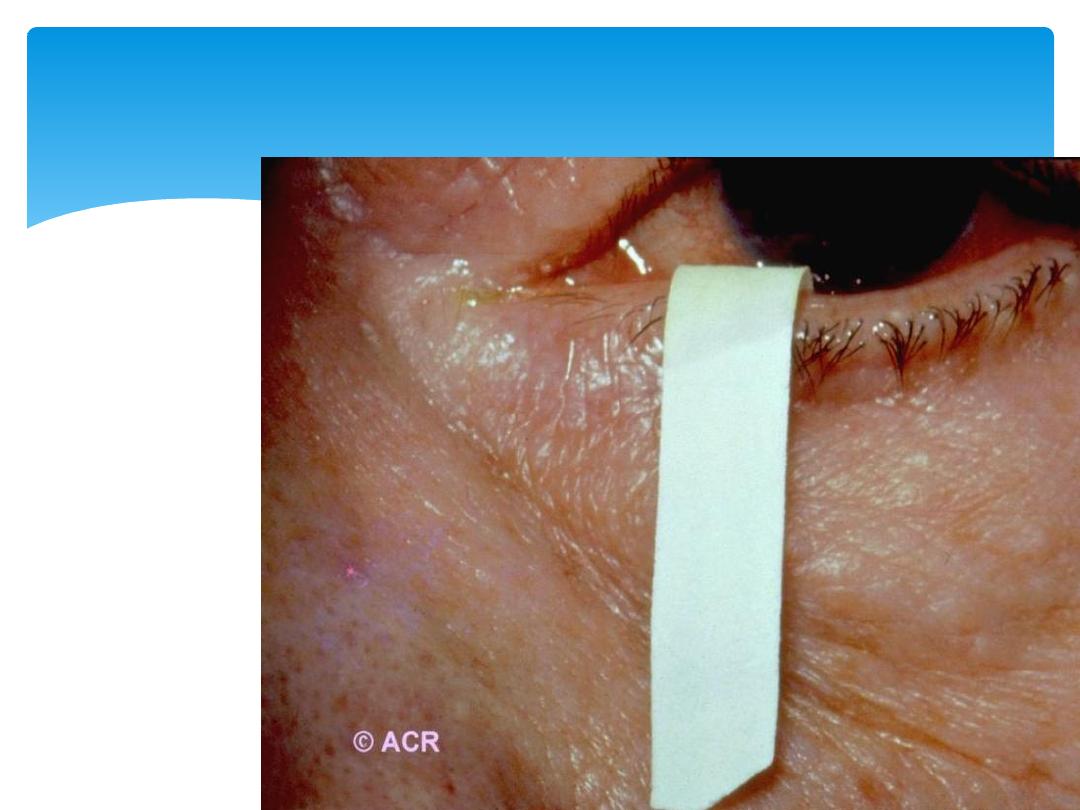
Schirmer Tear Test
13-Oct-15
Connective Tissue Diseases SSalman
35
xerostomia
13-Oct-15
Connective Tissue Diseases SSalman
36
Sjogren’s Minor Lip salivary biopsy
13-Oct-15
Connective Tissue Diseases SSalman
37
Sjogren’s Sialography

Schirmer tear test, which measures tear flow over 5
minutes using absorbent paper strips placed on the lower
eyelid; a normal result is more than 6 mm of wetting.
Staining with rose Bengal may show punctate epithelial
abnormalities over the area not covered by the open
eyelid.
Lip biopsy which shows focal lymphocytic infiltrate of the
minor salivary glands.
elevated ESR
Hypergammaglobulinaemia
ANA and RF
Anti-Ro and anti-La antibodies
Investigations
13-Oct-15
Connective Tissue Diseases SSalman
38

Treatment is symptomatic.
Lachrymal substitutes eg hypromellose eye drops
Viscous lubricating ointment at night.
Soft contact lenses for corneal protection in filamentary keratitis
Occlusion of the lachrymal ducts
Artificial saliva and oral gels
Stimulation of saliva flow by sugar-free chewing gum or lozengesl
Oral hygiene and prompt treatment of oral candidiasis
Vaginal dryness is treated with lubricants such as K-Y jelly
Extraglandular and MSK manifestations may respond to steroids
Immunosuppressive drugs
If lymphadenopathy or salivary gland enlargement develops, biopsy
should be performed to exclude malignancy.
Management
13-Oct-15
Connective Tissue Diseases SSalman
39

Polymyositis and
dermatomyositis
13-Oct-15
Connective Tissue Diseases SSalman
40

Polymyositis is characterised by an inflammatory
process affecting skeletal muscle.
Dermatomyositis describes the same disease but with
skin involvement.
They are rare, 2–10 cases per million/year.
Polymyositis can occur in isolation or in association
with other autoimmune diseases such as SLE, systemic
sclerosis and Sjögren’s syndrome.
The cause is unknown, although there is evidence for a
genetic contribution.
Polymyositis and dermatomyositis
13-Oct-15
Connective Tissue Diseases SSalman
41

Lymphoreticular • lymphoma Glomerulonephritis•
Renal tubular acidosis• RF• SS-B (anti-La)• ANA•
Gastric parietal cell• SS-A (anti-Ro)• Thyroid•
associated autoimmune disorders SLE•Progressive
systemic sclerosis• Primary biliary cirrhosis•
Systemic connective tissue disease Chronic active
hepatitis• Myasthenia gravis•
Clinical features
13-Oct-15
Connective Tissue Diseases SSalman
42

symmetrical proximal muscle weakness, usually affecting
the lower limbs more than the upper limbs.
40 - 60 years of age
Difficulty rising from a chair, climbing stairs and lifting,
sometimes in combination with muscle pain.
Systemic features of fever, weight loss and fatigue are
common.
Respiratory or pharyngeal muscle involvement can lead
to ventilatory failure or aspiration that requires urgent
treatment.
Interstitial lung disease in up to 30% of patients and is
strongly associated with the presence of antisynthetase
(Jo-1) antibodies.
Clinical features
13-Oct-15
Connective Tissue Diseases SSalman
43

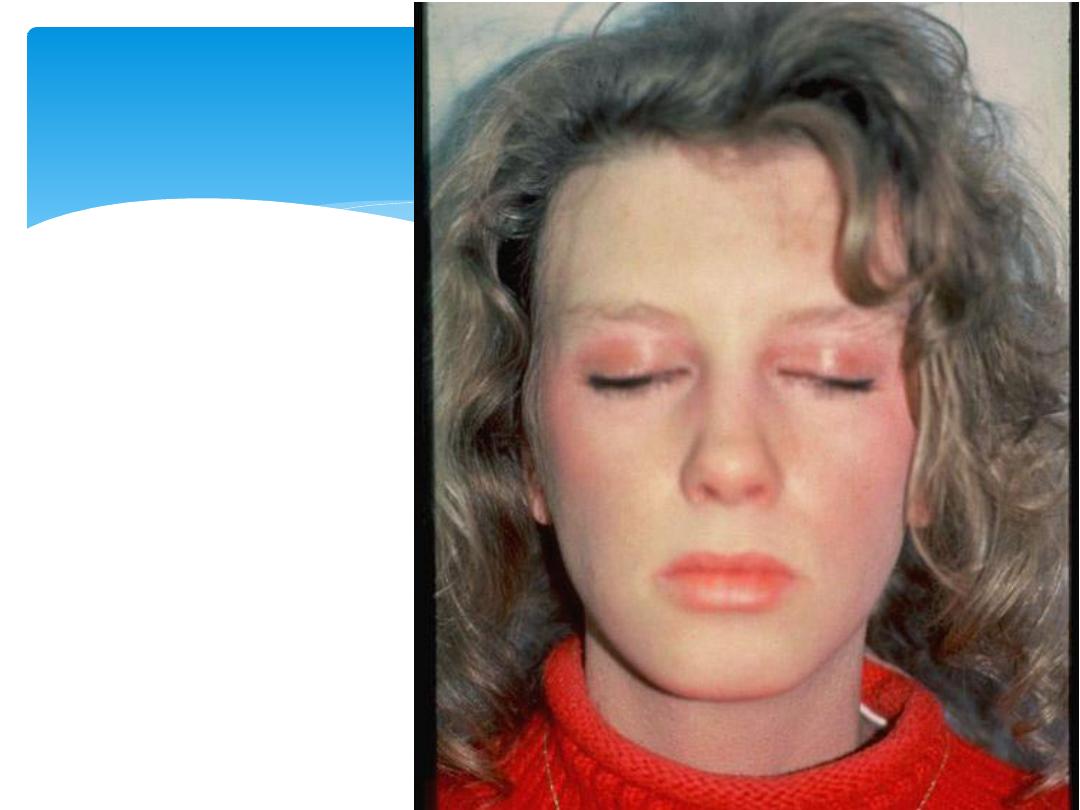
Dermatomyositis presents similarly but in combination with
characteristic skin lesions.
Gottron’s papules, which are scaly erythematous or
violaceous psoriaform plaques occurring over the extensor
surfaces of proximal and distal IPJs
Heliotrope rash which is a violaceous discoloration of the
eyelid in combination with periorbital oedema
Rashes occur on the upper back, chest and shoulders
(‘shawl’ distribution).
Periungual nail-fold capillaries are often enlarged and
tortuous.
Threefold increased risk of malignancy in patients with
dermatomyositis and polymyositis. This may be apparent
at the time of presentation, but the risk remains increased
for at least 5 years following diagnosis.
13-Oct-15
Connective Tissue Diseases SSalman
44
Dermatomyositis
13-Oct-15
Connective Tissue Diseases SSalman
45
13-Oct-15
Connective Tissue Diseases SSalman
46
Heliotrope
Rash

13-Oct-15
Connective Tissue Diseases SSalman
47
Photosensitive shawl Sign

13-Oct-15
Connective Tissue Diseases SSalman
48
Gottron’s sign

13-Oct-15
Connective Tissue Diseases SSalman
49
Periungual infarcts

13-Oct-15
Connective Tissue Diseases SSalman
50
Subcutaneous Calcifications

13-Oct-15
Connective Tissue Diseases SSalman
51
Skin rash, knees

13-Oct-15
Connective Tissue Diseases SSalman
52
Soft tissue
calcifications
13-Oct-15
Connective Tissue Diseases SSalman
53
Nail fold cappilaroscopy

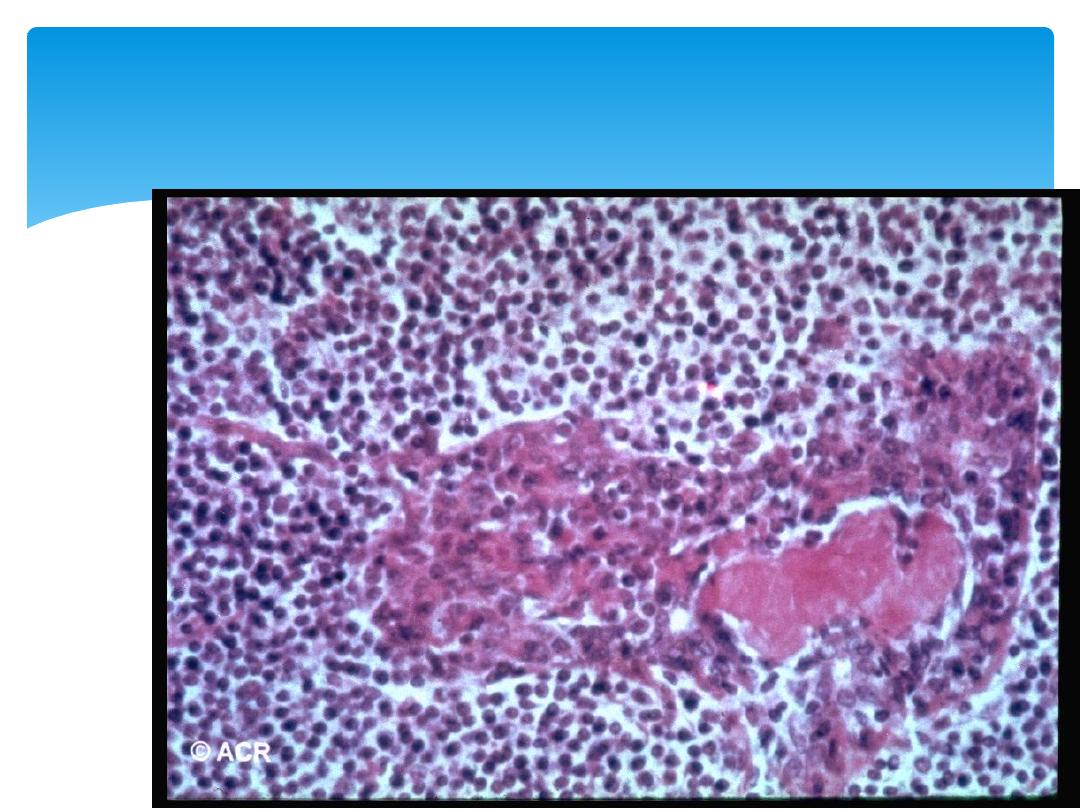
Muscle biopsy :typical features of fibre necrosis,
regeneration and inflammatory cell infiltrate.
EMG : myopathy and exclude neuropathy.
MRI :areas of abnormal muscle for biopsy.
Serum levels of CK are usually raised and are a
useful measure of disease activity,
Screening for underlying malignancy should be
undertaken routinely, and should include
chest/abdomen/pelvis CT, gastrointestinal tract
imaging and mammography (in women).
Investigations
13-Oct-15
Connective Tissue Diseases SSalman
54
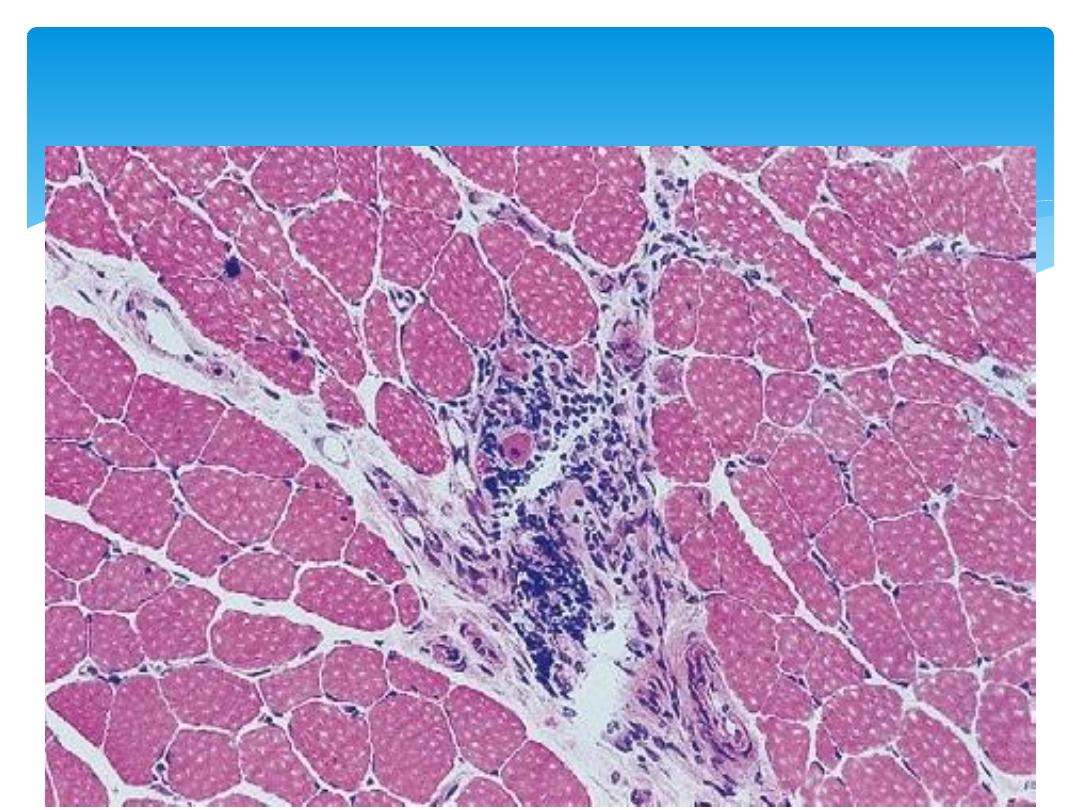
Muscle biopsy
13-Oct-15
Connective Tissue Diseases SSalman
55

Oral corticosteroids (e.g. prednisolone 40–60 mg daily)
High-dose intravenous methylprednisolone (1 g/day for 3
days) may be required in patients with respiratory or
pharyngeal weakness.
Reduce steroids monthly to a maintenance dose of 5–7.5
mg.
Most Patients need additional immunosuppressive
therapy:
Azathioprine and methotrexate
ciclosporin, cyclophosphamide, tacrolimus or MMF
Intravenous immunoglobulin in refractory cases.
Relapses may occur associated with a rising CK, and
indicate the need for additional therapy.
Management
13-Oct-15
Connective Tissue Diseases SSalman
56

Davidson’s Principles and Practice of
Medicine 21
st
Edition
Slide collection of American College of
Rheumatology (ACR)
References

13-Oct-15
Connective Tissue Diseases SSalman
58
THANK U 4 LISTENING !!
DR SAMI SALMAN, FRCP, MRCP, DMR, CES, MB,ChB
PROFESSOR OF MEDICINE & RHEUMATOLOGY
Baghdad Medical College
http://www.samisalman.comyr.com
Arab rheumatologists listing:



