1- Describe septal deviation & spurs.
2- Describe nasal foreign bodies.
3-Describe epistaxis.

Septal deflections and spurs

Aetiology:
Trauma commonest cause of septal deviation
requiring surgery.
Genetic factors (errors of development).
The position of the fetus in utero.
Compression of the nose during birth.
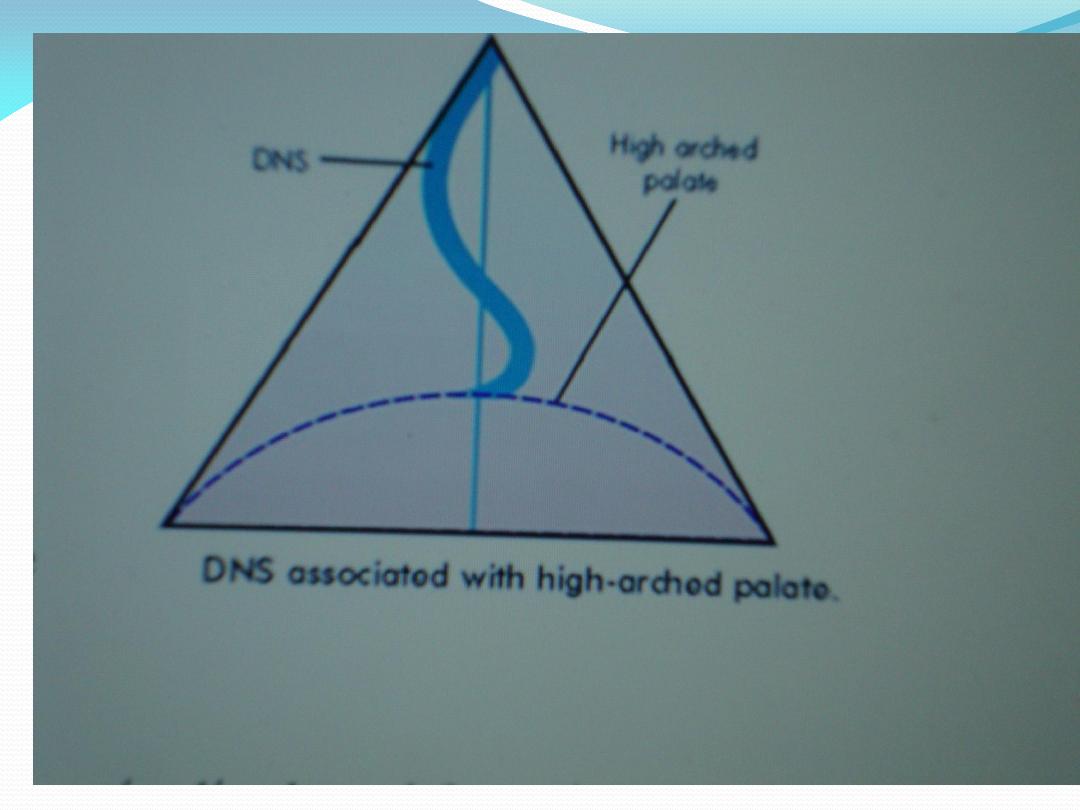
Associated with high-arched palate.

Pathology:
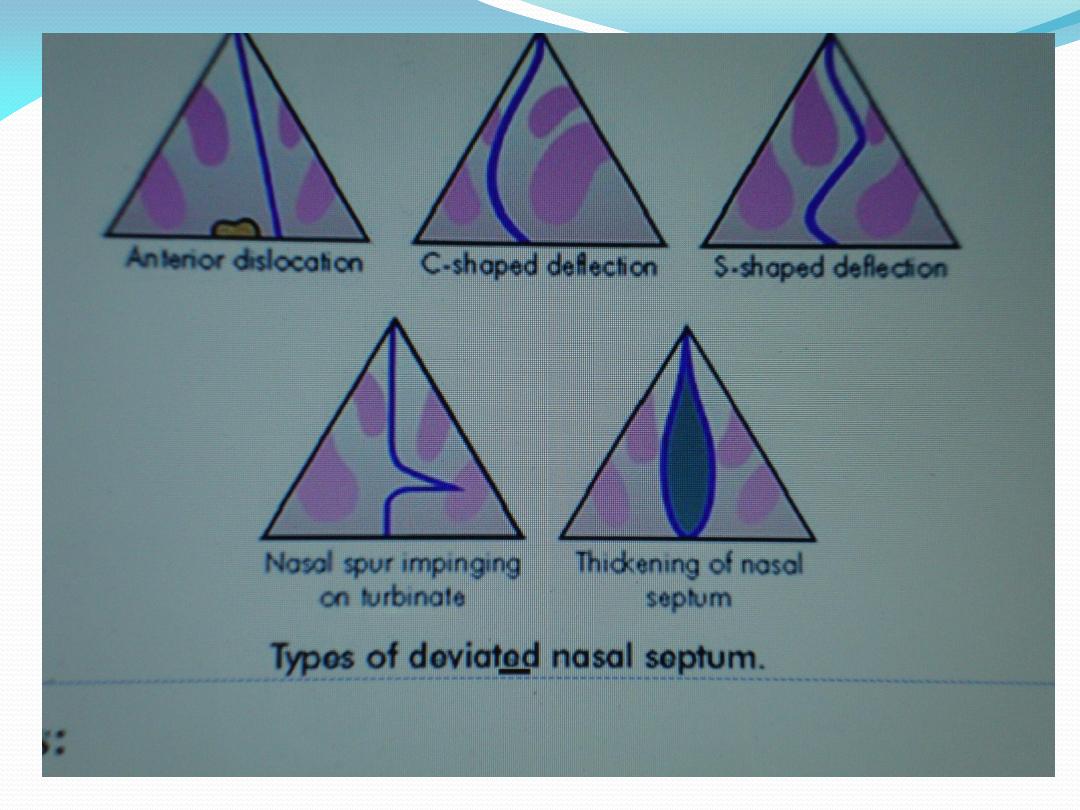
Septal deviation is classified into:
Spurs
which are sharp angulations of the septum as in
septal fracture.
Deviations:
C or S shaped.
Dislocation:
the lower border of the septum is
displaced from its medial position and projects into
one of the nostrils.

Clinical features:
Nasal obstruction:
is the presenting symptom.
Epistaxis:
due to change in the direction of air current
→
dry mucosa
→
crustation
→
epistaxis.
Pressure headache:
due to contact of the deviated
septum to lateral nasal wall called the anterior
ethmoidal nerve syndrome.
Anosmia
(loss of olfaction): due to obstruction, the
odorant molecules do not reach olfactory area
→
loss
of smell sensation.
Treatment:
No treatment:
when there is simple deviation without
obstruction.
Surgery
is used when the deviation is symptomatic or
there is complication. It includes:
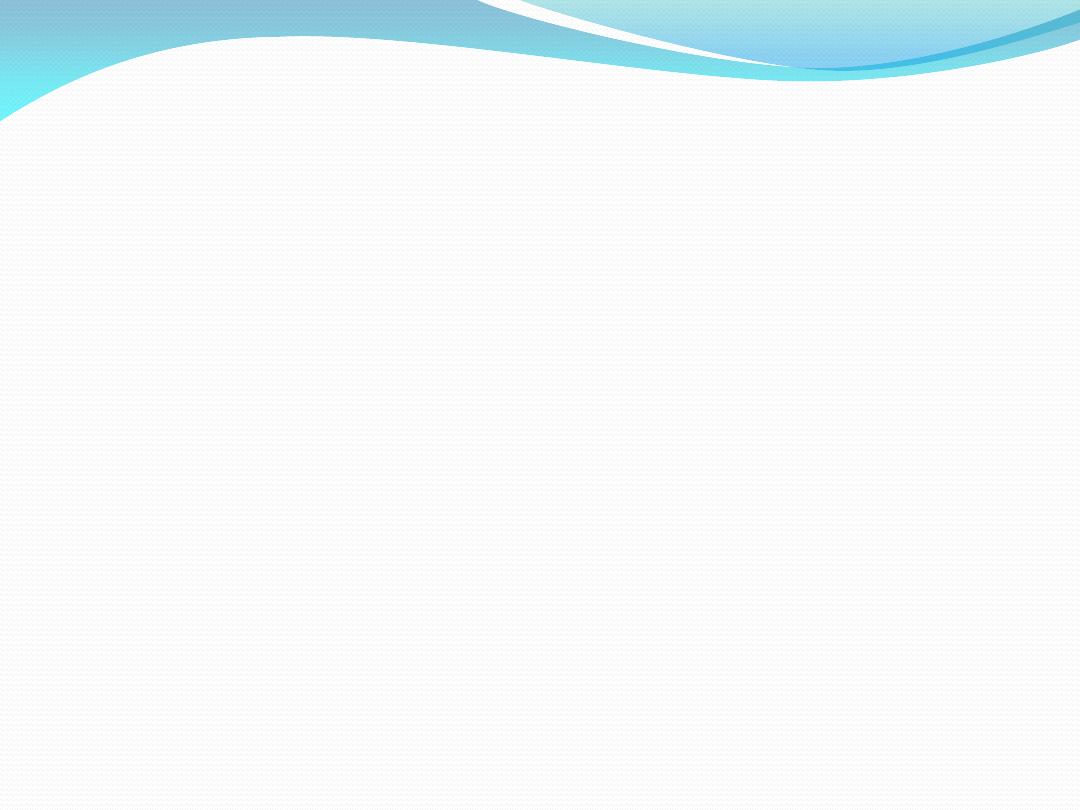
1- Submucous resection (SMR):
removal of deviated
septal cartilage and bone by using Killian incision.
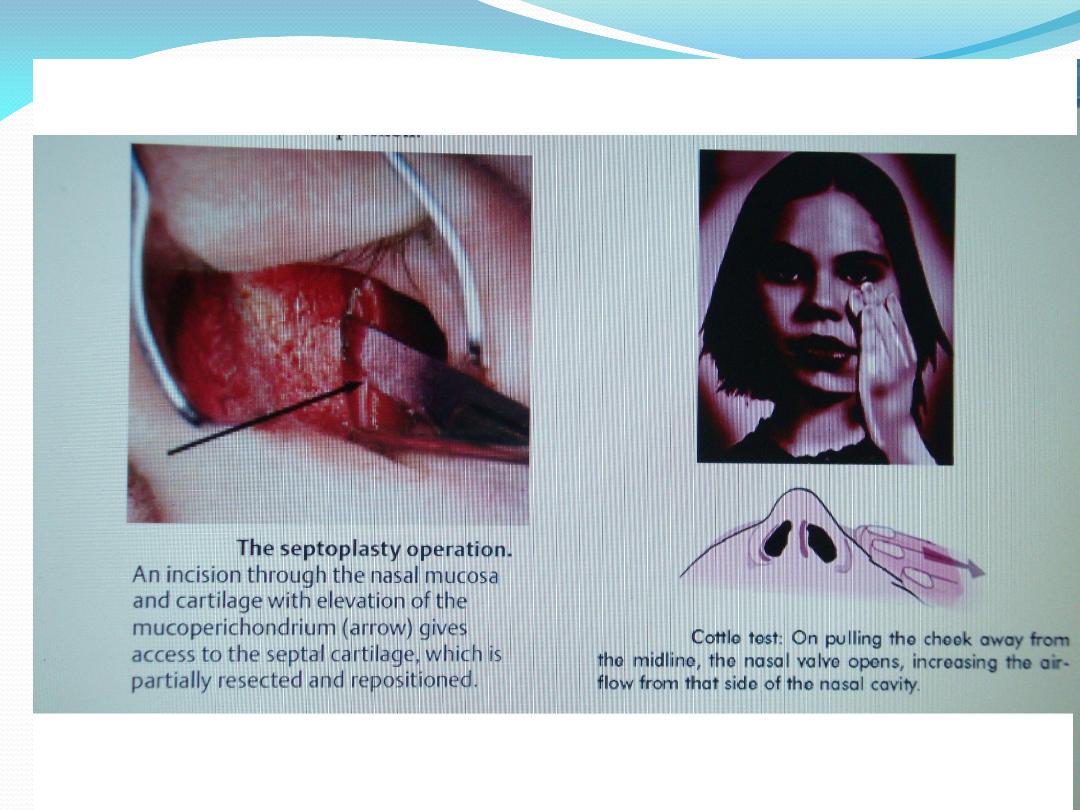
2- Septoplasty:
freeing of the septal cartilage and bone
and repositioned into midline without removal of
cartilage or bone by using freer's incision.

Note:
the septum is divided by imaginary line from
the spine of the maxilla to the spine of the frontal bone
into anterior and posterior parts, septoplasty is usually
used when there is deviation anterior to this lines,
SMR is usually used when the deviation is posterior to
this line.

Foreign bodies in the nose:

Aetiology:
foreign bodies may be introduced into the nose
by many routes:
Through anterior nares (most common).
Through posterior nares such as in coughing or vomiting.
Penetrating wounds and nasal surgery i.e.: swab left in the
nasal cavity.
Through palatal perforation (syphilis, malignant tumor of
hard palate).
Sequestration of bone in situ (syphilis).
Calcification in situ of inspissated mucopus or foreign
bodies → rhinolith.
Site:
usually beyond the constriction at the nasal vestibule.

Types
: 1- Inanimate 2-Animate
1-Inanimate:
Organic
e.g.: vegetable foreign bodies such as beans,
paper, cotton... etc.
Inorganic
e.g.: metallic or plastic foreign bodies.

Pathology:
Inorganic foreign bodies are usually inert and may
remain in the nose for years without causing
inflammation.
Organic foreign bodies cause inflammation and
infection of the mucous membrane → granulation
tissue formation, ulceration of the mucosa →
epistaxis.
Button batteries
leak alkaline material → severe
inflammation and necrosis of the bone and cartilages,
so should be removed urgently.

Clinical features:
History of putting foreign bodies into the nasal cavity.
More common in children under 4 years.
Unilateral foul smelling nasal discharge which is purulent
that is characteristic.
Bleeding may occur and nasal obstruction.
Pain may occur.
Sneezing may occur.
O/E we see foreign body inside the nasal cavity.
Diagnosis:
By x-ray when the foreign bodies are
radiopaque.

Treatment:
Removal is the only treatment; removal
may be:
Forcible nose blowing.
Removal through the anterior nares (under local or
general anesthesia) by hooks or probe passed beyond
the foreign body and then drawn forward (this
especially done in rounded foreign bodies) or by
sucker or by using forceps when the foreign body can
be caught by forceps.

2-Animate foreign body
e.g.: maggot, ascaris.
The symptoms are often bilateral.
Treatment of maggot is by instilling 25% chloroform
solution into the nose 3 times/week for 6 weeks to kill
the larvae.
Treatment of ascaris is by removal of the worm by
forceps and treatment of the disease by piperazine and
magnesium sulphate.

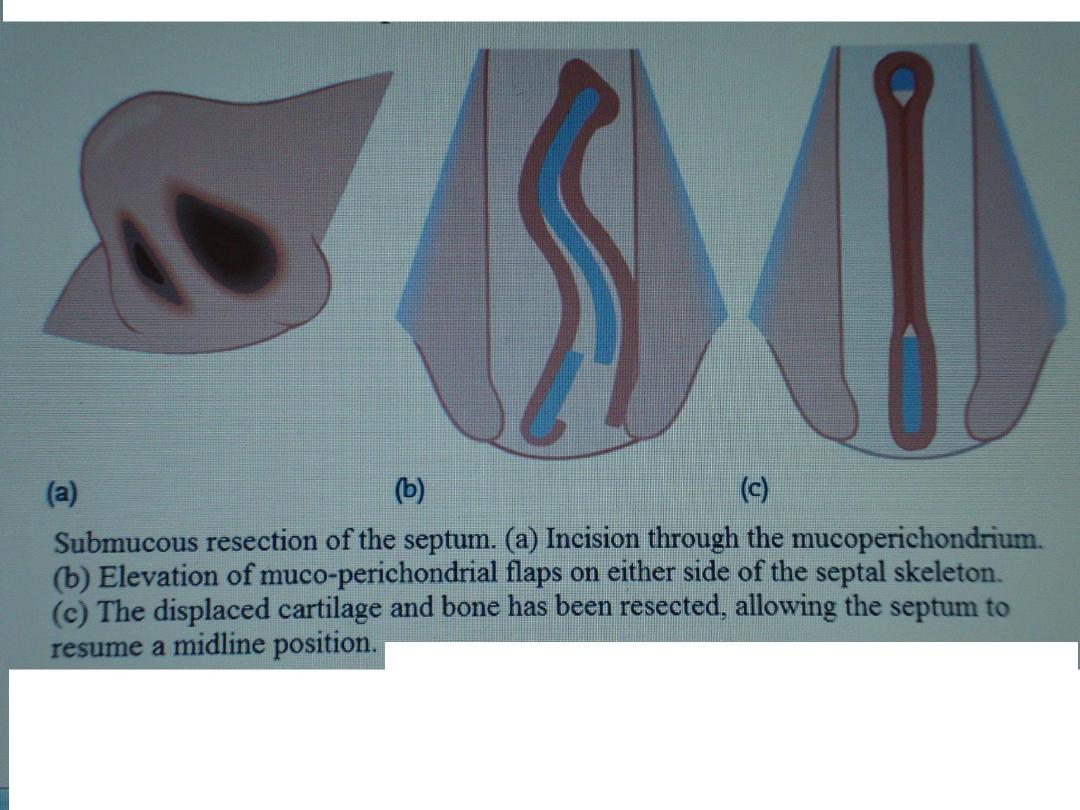
Rhinoliths:
It is nasal concretion of calcium, magnesium phosphate
and carbonate around foreign body, inspissated mucopus
or blood.
Clinical features:
Nasal obstruction
O/E there is brown or grayish large irregular mass near the
floor of the nose, which is stony hard on probing.
Diagnosis:
By radiology → radiopaque.
Treatment:
should be removed under GA & sometimes it
is very large; so should be broken by forceps in the nasal
cavity and then removed.

Epistaxis:
It is bleeding from the nasal cavity.

Aetiology:
1- Local cause:
Idiopathic 85%
Trauma.
Foreign body.
Inflammatory e.g.: rhinitis, sinusitis,
Neoplastic → benign or malignant tumors of the nose,
sinuses or nasopharynx.
Environmental e.g.: high altitude and air conditioning due
to drying effect.
Iatrogenic e.g.: nasal surgery, topical nasal steroid.

2- General causes:
Hypertension does not lead to epistaxis but epistaxis
tends to be more severe and prolonged in
hypertension.
Raised venous pressure e.g.: whooping cough,
pneumonia.
Disease of blood and blood vessels e.g.: leukemia,
hemophilia and familial haemorrhagic telangiectasia
(Osler-Rendu disease).
Anticoagulant e.g.: warfarin, aspirin.

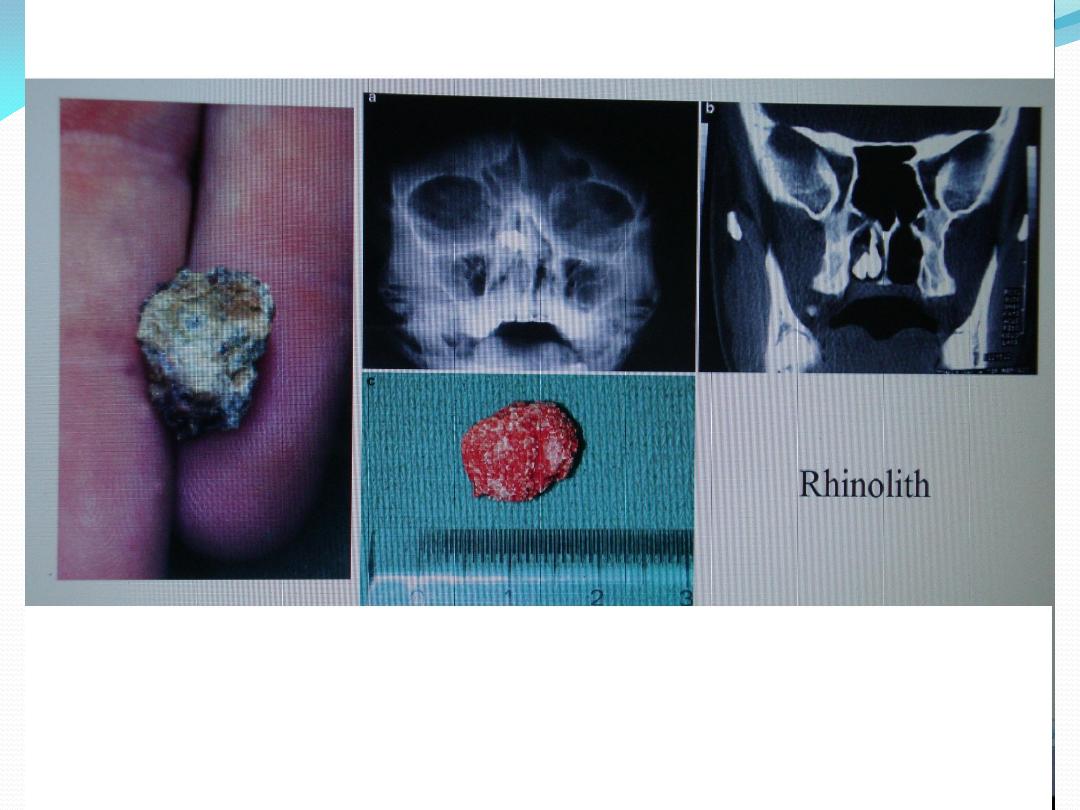
Site of epistaxis:
the commonest site is
little's area
(kiesselbach's plexus)
which is situated in the
anteroinferior part of the nasal septum, it is formed by
anastomosis of:
Anterior ethmoidal a.
Greater palatine a.
Sphenopalatine a.
Superior labial branch of facial a.
Epistaxis
→ Active epistaxis
(active bleeding in the time of
examination).
→ Recurrent epistaxis.

Management of active epistaxis:
1-Stop the bleeding:
A-Pressure on the nostrils:
the patients sit on a chair,
leaning forward and simple pressure on the nose by
fingers below the nasal bones for 10 min, ice packs may
be applied to the nasal bridge.

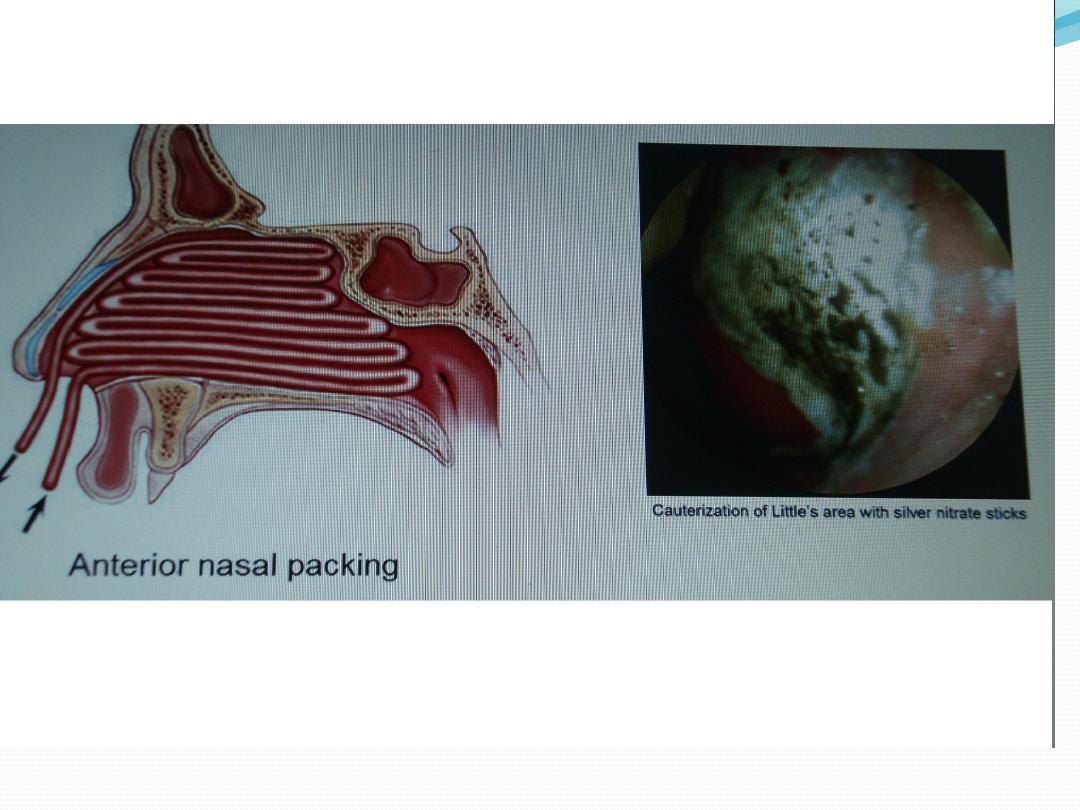
B-Cauterization
(if we can see the bleeding point).
Cauterization is divided into
1-
chemical cautery
by using
silver nitrate or trichloro-acetic acid which is more
effective. The chemical material is applied by using very
smooth cotton wood carrier around bleeding point.
2-Electrical cautery
is more effective than chemical cautery
but is painful and in young children it should be done
under general anesthesia, it is done by using small
instrument (Galvanic cautery) which cauterize the
bleeding point by electrical current lead to coagulation of
blood vessels and stop the bleeding. (
**
we avoid cautery on
the same point on the two sides to avoid perforation of the
septum).

C- Anterior nasal pack:
It is used when we cannot see the
bleeding point. It is done
by using ribbon gauze
soaked with Bismuth iodoform paraffin paste (BIPP);
(
Bismuth = detergent
;
iodoform = antiseptic
,
paraffin =
lubricant
). The pack is inserted by using Tilley forceps
and inserted layer by layer starting from the nasal
floor to roof to produce good pressure inside the nasal
cavity to stop bleeding. The pack removed after 48 hrs.
The pack should be on both nasal cavities.

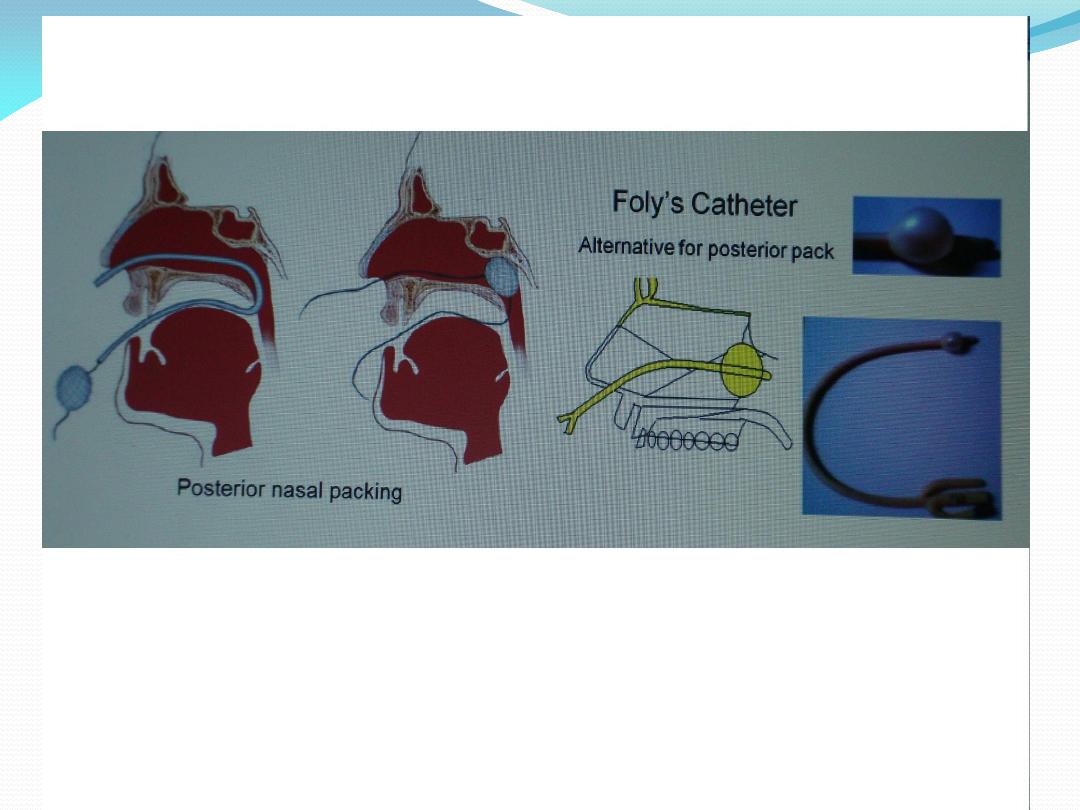
D- Posterior nasal pack:
when the bleeding point is
posterior and bleeding does not stop by anterior nasal
pack then use posterior nasal pack which are placed in
the nasopharynx under G.A. and always it is
accompanied by anterior nasal pack, Foley's catheter
may be used instead of posterior nasal pack, the
catheter is passed through the nostrils into the
nasopharynx and the balloon is expanded with 7 ml of
normal saline or air.

E- Surgery:
if bleeding is severe and does not stop we
have to do surgical operations which include:
Arterial ligation
(maxillary a. or external carotid a. or
anterior or posterior ethmoidal a.)
SMR
assisted by dissection of blood vessels which
cause the bleeding.
Embolization
by using polyvinyl alcohol sponge or
coiled spring.

2- Supportive measures:
Resuscitation
by I.V. fluid and blood transfusion to
replace the lost blood. So we have to do blood group,
blood cross match and repeated HB estimation).
Antibiotic:
when the pack is put for more than 48 hrs.
Analgesia:
pain → ↑ BP → more bleeding so use
analgesia.
Hospitalization
in severe cases.

3-Treatment of underlying causes
e.g.: sinusitis →
antibiotics, tumor or polyps → surgery...etc. and this is
done by taking full history, examination and
investigation.

Management of recurrent epistaxis:
In recurrent epistaxis the patient presented with history of
repeated attacks of bleeding from the nasal cavity, but
there is no active bleeding when the patient examined by
the doctor, only we see a bleeding point. The best
treatment is by cauterization on each side of bleeding point
(do not cauterize the bleeding point itself to avoid rupture
of the blood vessels → active bleeding).
Note:
we should avoid cauterization of both side of nasal
septum at the same time to avoid septal perforation.
so if we do cautery of one side of the nasal septum,
cauterization of the other side (if needed) should be done
after 4 weeks to avoid septal perforation.

General advice to avoid recurrent
epistaxis:
Avoid nose picking.
Avoid hotness
Antibiotic ointment applied to nasal vestibule and
little's area twice daily.
Only blow one nostril at a time.



