1
4th stage
Surgery
Lec-1,2,3
د
.
يحيى
13/10/2015
BREAST DISEASES
Embryology
The paired glands normally develops in the pectoral region,
one gland on each side.
The paired mammary gland embryologically
develops along the milk line that extends between the limb
buds from the axilla to the inguinal region.
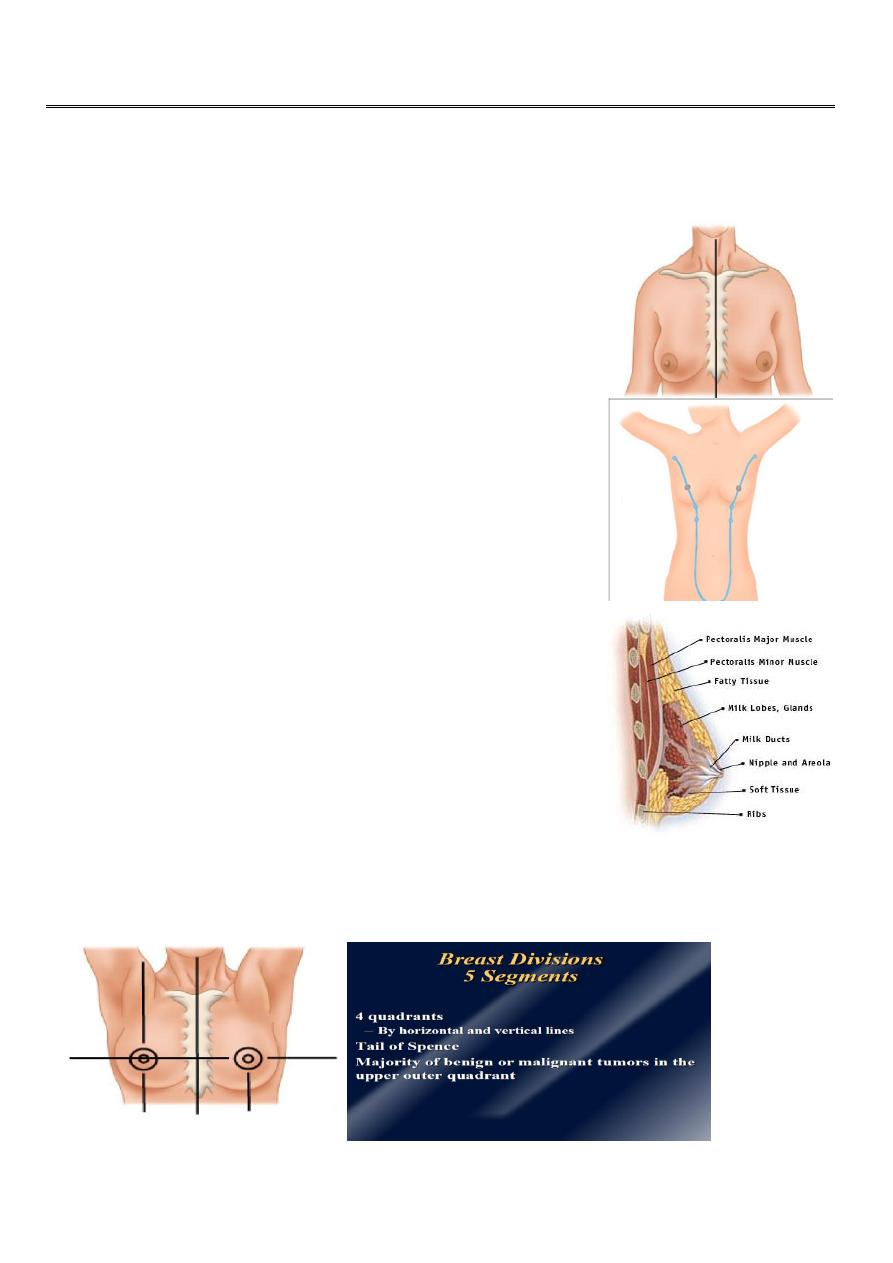
Surgical Anatomy Of Breast
Mammary tissues anatomically represent mature modified
sweat glands.
The Mammary gland Lies between the superficial and
deep layers of the pectoral fascia of the chest wall.
The breast is partitioned into 4 quadrants by vertical
and horizontal lines across the nipple:
Upper inner quadrant (UIQ)
Lower inner quadrant (LIQ)
Upper outer quadrant (UOQ)
Lower outer quadrant (LOQ)
2
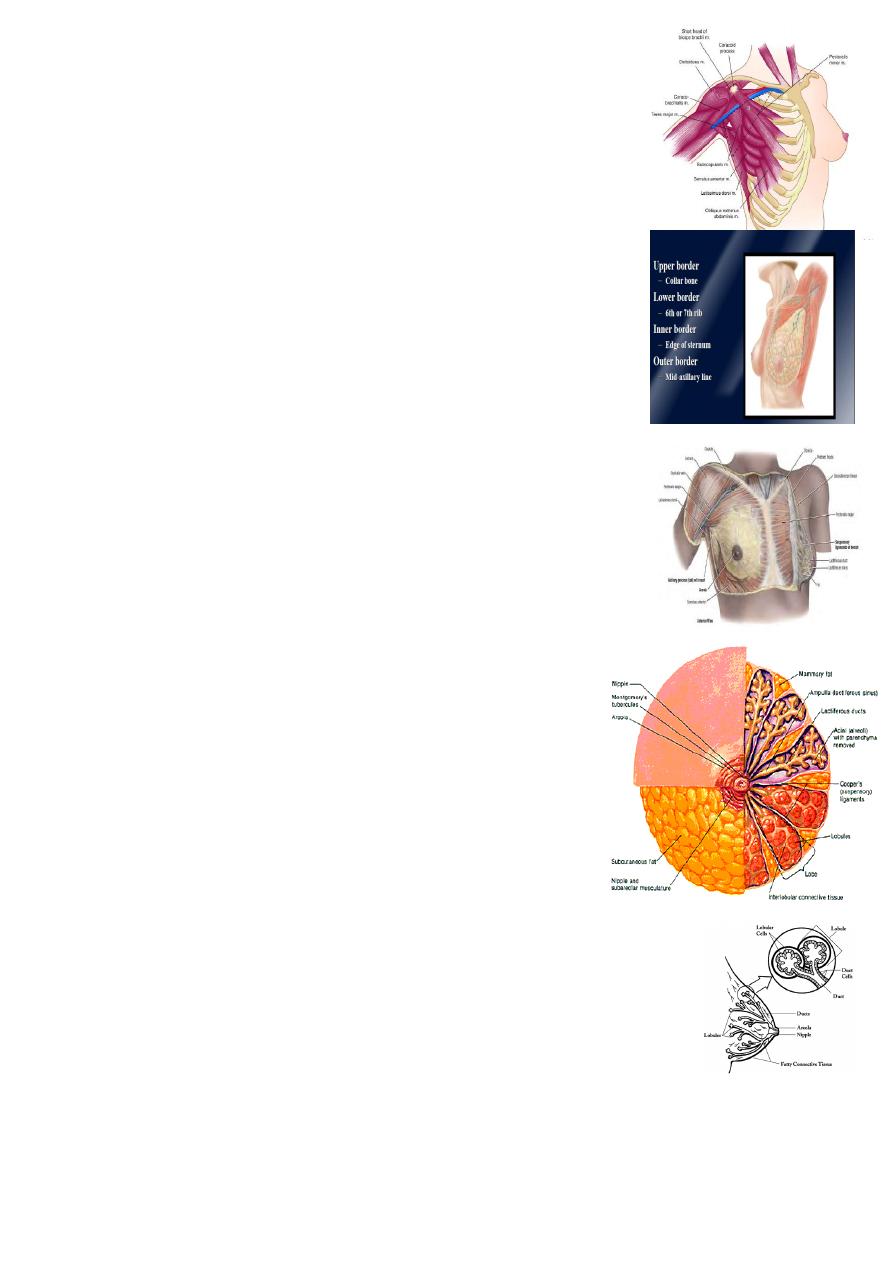
The mature female breast extends superiorly from the level of
the second or third rib to the inframammary fold inferiorly
that is located at the level of the sixth or seventh rib.
Medialy, the breast extends from the lateral border of the
sternum to the anterior or midaxillary line laterally .
The breast frequently extends into axilla as the axillary tail of
Spence.
The upper half of the breast, particularly the upper outer
quadrant, contains the greater volume of glandular tissue than
the remainder of the breast.
The Breast Are Composed Of
Three tissue types
Glandular epithelium.
Milk producing tissue.
Fibrous stroma and supporting structures.
Adipose tissue.
Glandular epithelium
The breast is composed of 15 to 20 lobes , which are each composed
of several lobules.
The lobule
Is the basic structural unit of the mammary gland.
The number and size of the lobules vary from 20 to over 40 lobules
empty via ductules into a lactiferous duct.
there are 15–20 lactiferous duct.
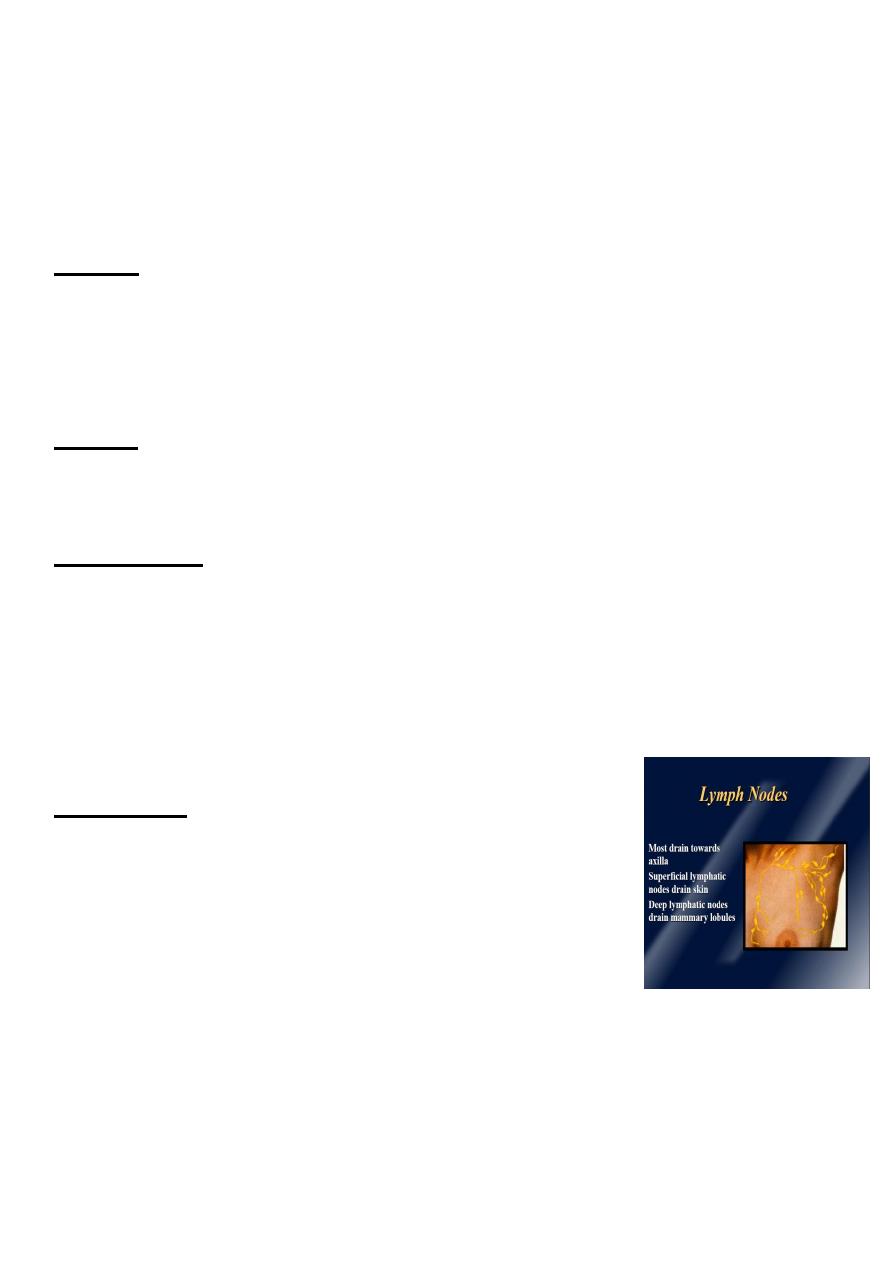
3
each lactiferous duct is lined with a spiral arrangement of contractile myoepithelial
cells and is provided with a terminal ampulla, a reservoir for milk or abnormal
discharges.
Blood Supply of the Breast
Arterial
It is supplied by the axillary artery via the lateral thoracic and thoracoacromial
branches.
The internal mammary artery via its perforating branches.
Adjacent intercostal arteries.
Venous
It tends to follow the arterial supply; axillary, internal mammary, and intercostal veins.
The axillary vein is responsible for the majority of venous drainage
Nerve Supply
The breast is supplied by 4 main nerves:
Long thoracic nerve
Thoracodorsal nerve
Medial and lateral pectoral nerves
Intercostobrachial nerve
Lymphatic's
The lymphatic's of the breast drain predominantly into the
axillary and internal mammary lymph nodes.
The axillary nodes receive approximately 85% of the drainage.
DIAGNOSIS OF BREAST DISEASE
Symptoms of breast disease
Mastalgia
Swelling or change in size or shape
Breast lumps
NIPLE (Discharge, Retraction)

4
HISTORY
A history and physical examination are essential for the diagnostic evaluation of a
breast abnormality.
the history include details about the :
presenting symptom.
history of previous breast disease.
risk factors for breast cancer
a menstrual history.
questions focused on the presenting symptom, whether it be
a mass,
nipple discharge,
palpable adenopathy,
pain,
abnormal imaging.
Examination
The physical examination should be performed with respect for patient privacy and
comfort without compromising the complete evaluation.
The examination begins with inspection.
The breasts are visually observed and compared , any obvious masses, asymmetries,
and skin changes.
The nipples are inspected for the presence of retraction, inversion, or excoriation.
Palpation the breast is examined
patient upright with arms relaxed and supine with the ipsilateral arm raised above the
head.
Finally the regional nodes should follow to include the axillary, infraclavicular,
supraclavicular, and cervical nodes.
If a mass is identified, it should be measured, and its location,mobility, and character
should be documented in the medical record.
True masses will persist throughout the menstrual cycle.
Diagnosis should not be delayed.

5
In patients who present with nipple discharge, the nipple discharge is often elicited
during palpation of the breast.
The character, color, and location of the discharging duct or ducts should be
documented.
If the discharge is not grossly bloody, a Hem occult test may be used to detect occult
blood.
Pathologic discharge:
unilateral,
uniduct,
spontaneous, and/or bloody discharge, should be evaluated with surgical duct
excision.
INVESTIGATION
Mammography
Ultrasound
Magnetic resonance imaging (MRI)
Computed tomography
Needle biopsy\cytology
Mammography
X-rays taken by placing the breast in direct contact with
ultrasensitive film.
The dose of radiation is approximately 0.1 cGy and, therefore,
mammography is a very safe investigation.
The sensitivity of this investigation increases with age as the
breast becomes less dense.
Mammography is the most sensitive and specific imaging test currently available.
In total, 5% of breast cancers are missed by mammographic screening programmes.
Thus, a normal mammogram does not exclude the presence of carcinoma.
Digital mammography is being introduced, which allows manipulation of the images
and computer-aided diagnosis.

6
Screening mammography
is used to detect cancer in asymptomatic women when cancer is not suspected.
Diagnostic mammography
is used to evaluate the breasts of patients with breast symptoms or complaints, such
as nipple discharge or a palpable mass or patients who have had breast cancer treated
with breast conservation therapy.
Ultrasound
Ultrasound initially used to differentiate solid masses from cystic masses, but it has
become an important adjunct to mammography and is an excellent method for guiding
some interventional procedures.
Ultrasound is not a breast screening tool and remains operator dependent.
MRI BREAST
(MRI) is being used with increasing frequency for the screening and diagnosis of breast
cancer.
While mammography remains the “gold standard,” MRI is
emerging as an important modality for evaluating breast diseases.
MRI has several advantages, There is no ionizing radiation to the patient with MRI.
MRI is not limited by breast density and is an excellent tool for the screening of young
women with increased risk for inherited breast cancer.
Disadvantages of MRI are cost, limited availability.
Patients with MRI-incompatible implantable devices, metallic clips, or prostheses
cannot undergo MRI.
Computed tomography
appears to be the best way to image internal mammary nodes and to evaluate the
chest and axilla after mastectomy.
Needle biopsy/cytology
Fine-Needle Aspiration Cytology
Core-Needle (Cutting-Needle) Biopsy
Image-Guided
Stereotactic
Ultrasound-Guided
7
• Fine-needle aspiration cytology (FNAC) is the least invasive technique of obtaining a
cell diagnosis and is rapid and very accurate if both operator and cytologist are
experienced.
• The diagnostic accuracy of FNA biopsy of breast masses approximates 80%,
False-negative results occur in approximately 15% of cases and the False-positive result
is rare.
When the specimen is properly prepared and reviewed by an experienced
cytopathologist, the false-negtive a lesion that is suspicious clinically or by imaging
must be further investigated with surgical excision.
Triple assessment
any patient who presents with a breast lump or other symptoms suspicious of
carcinoma,
the diagnosis should be made by a combination of clinical assessment, radiological
imaging and a tissue sample taken for either cytological or histological analysis, the
so called triple assessment.
The combinations should exceed 99.9%.
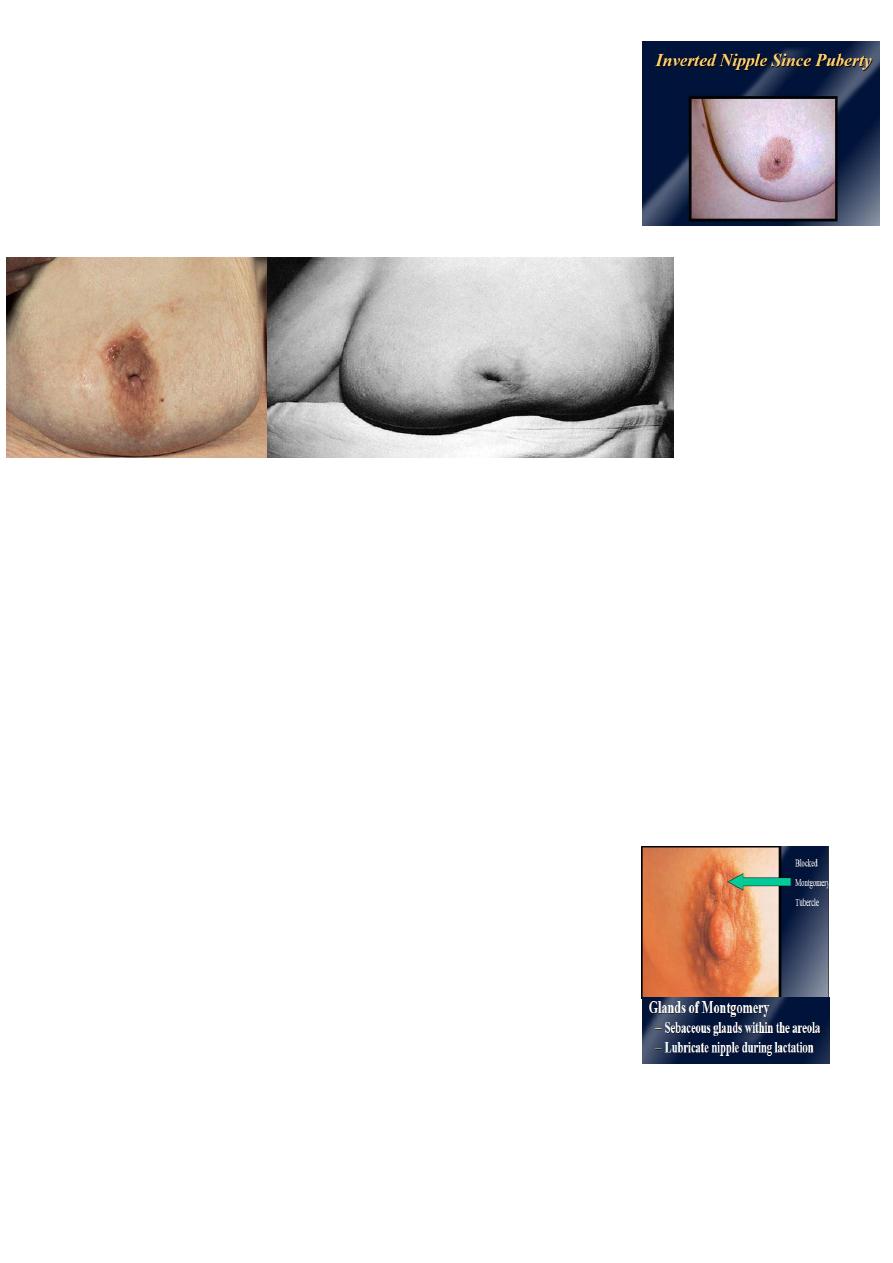
Diseases Of The Nipple
Nipple retraction.
Cracked nipple.
Papilloma of the nipple.
Retention cyst of a gland of Montgomery.
Eczema.
Paget’s disease.
Discharges from the nipple.
Nipple retraction
occur at puberty or later in life.
pubertal retraction, known as simple nipple inversion, is of unknown aetiology.
In 25% of cases it is bilateral.
It may cause problems with breast-feeding and infection can occur, especially
during lactation, because of retention of secretions.
8
Recent retraction of the nipple may be of considerable
pathological significance.
A slit-like retraction of the nipple may be caused by
ductectasia and chronic periductal mastitis , but
circumferential retraction, with or without an underlying
lump, may well indicate an underlying carcinoma
Cracked nipple
This occur during lactation and it’s the cause of acute mastitis.
If the nipple becomes cracked during lactation, it should be rested for 24–48 hours
and the breast should be emptied with a breast pump.
Feeding should be resumed as soon as possible.
Papilloma of the nipple
Papilloma of the nipple has the same features as any cutaneous papilloma and
should be excised with a tiny disc of skin.
Alternatively, the base may be tied with a ligature and the papilloma will
spontaneously fall off.
Retention cyst of a gland of Montgomery
These glands, situated in the areola, secrete sebum and if
they become blocked a sebaceous cyst forms.
Eczema
Eczema of the nipples is a rare condition and is often bilateral; it is usually
associated with eczema elsewhere on the body.
It is treated with 0.5% hydrocortisone (not a stronger steroid preparation).
9
Paget’s disease
Paget’s disease of the nipple must be distinguished from eczema.
Paget’s disease is caused by malignant cells in the subdermal layer.
Eczema tends to occur in younger people who have signs of eczema elsewhere.
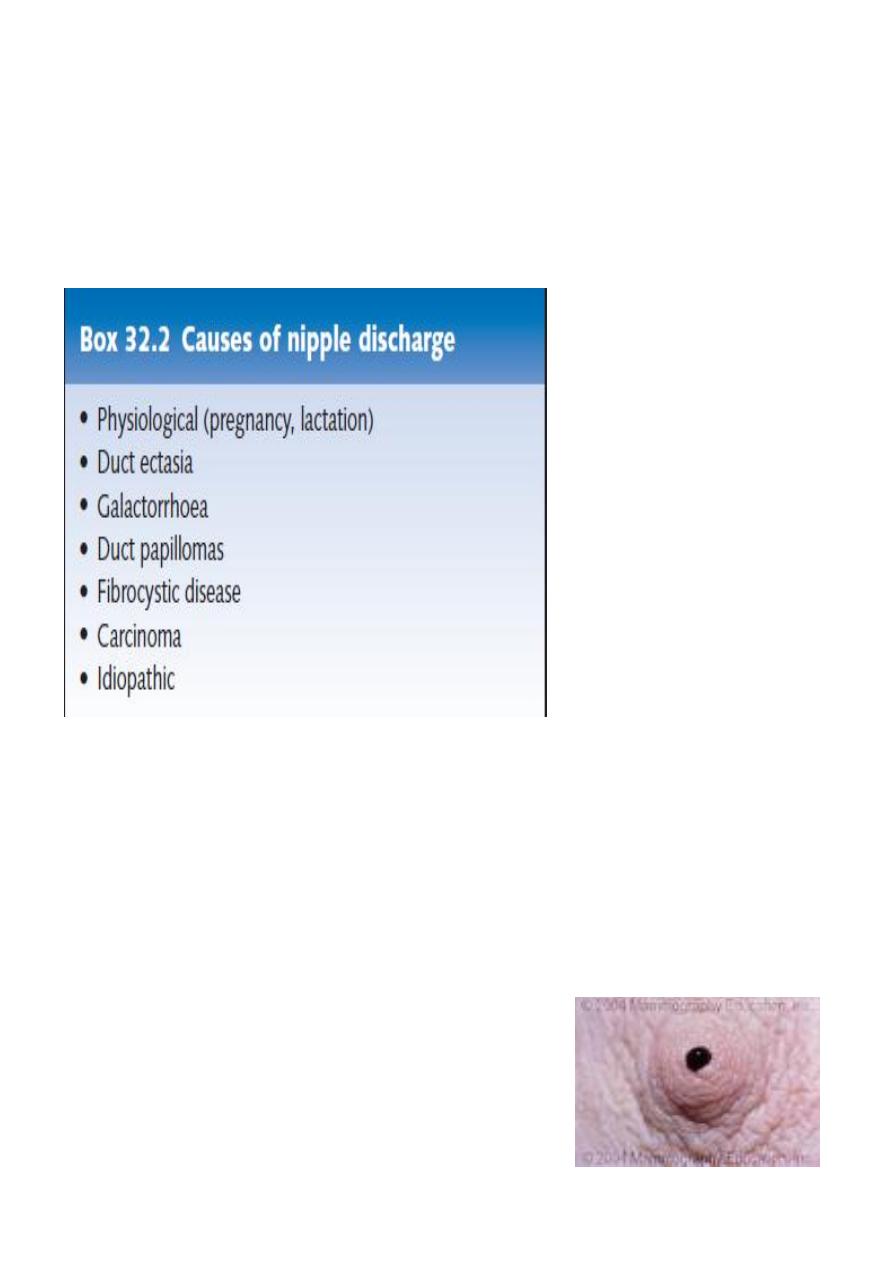
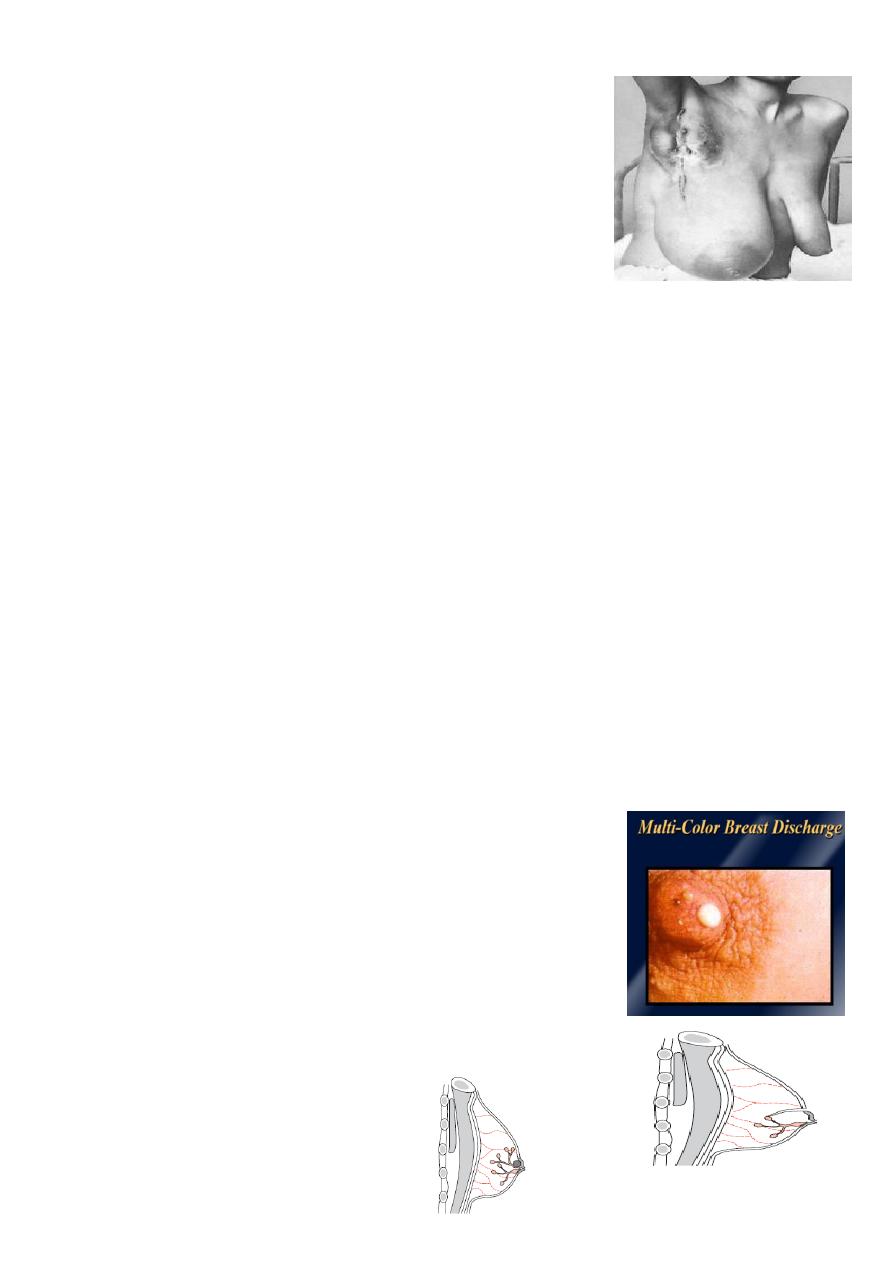
Discharges from the nipple
Discharge can occur from one lactiferous ducts or more.
Physiologic
Bilateral
Involves multiple ducts
Heme (-)
Non-spontaneous
Pathologic
Unilateral
persistent and spontaneous
Heme (+)
not associated with nursing& Requires further
evaluation.
Most common cause intraductal papilloma
11
Workup
Exam
Labs- Prolactin, Heme
Mammogram
Cytologic evaluation of discharge
Ductography
Galactorrhea
Bilateral, milky discharge.
Obtain prolactin levels, if highly elevated, suspect pituitary
adenoma as one of causes.
Bloody nipple discharge
Most common cause is intraductal papilloma
Cancer present 10% of cases .
Management depends on:
the presence of a lump (which should always be given priority in diagnosis and
treatment).
the presence of blood in the discharge from multiple duct or discharge from a single
duct.
Mammography is useful to exclude an underlying impalpable mass.
Cytology may reveal malignant cells.
Treatment
Treatment must firstly be to exclude a carcinoma by cytology.
Simple reassurance of the patient,
if the discharge is proving intolerable, an operation to remove the affected duct or
ducts can be performed.
Intraductal papilloma
Benign epithelial tumors arising in ducts of breast.
Main cause of bloody nipple discharge.
Usually women age (40-45).
Size (2-5 ) mm, usually not palpable, nearly always situated within 4–5 cm of the
nipple orifice.
Present with spontaneous, bloody, serous or cloudy nipple discharge.
11
Management
excisional biopsy
When the duct of origin of nipple bleeding is uncertain or when there is
bleeding or discharge from multiple ducts, the entire major duct system can be
excised for histological examination without sacrifice of the breast form.
BENIGN BREAST DISEASE
The most common cause of breast problems.
30% of women will suffer from a benign breast disorder requiring treatment .
The most common symptoms are pain, lumpiness or a lump.
The aim of treatment is to exclude cancer and, once this has been done, to treat any
remaining symptoms.
BENIGN BREAST DISEASE cont,
Congenital disorders.
Infectious and inflammatory.
Fibrocystic Disease
Mastalgia.
Benign mass.
Injury.
Congenital abnormalities
Amazia
Congenital absence of the breast may occur on one or both
sides.
It is sometimes associated with absence of the sternal
portion of the pectoralis major (Poland’s syndrome).
It is more common in males.
Polymazia
Accessory breasts recorded in the axilla (the most frequent
site), groin, buttock and thigh.
They have been know to function during lactation.
In approximately 1% of the female population,
supernumerary breasts (polymastia) or nipples (polythelia)
may develop.
12
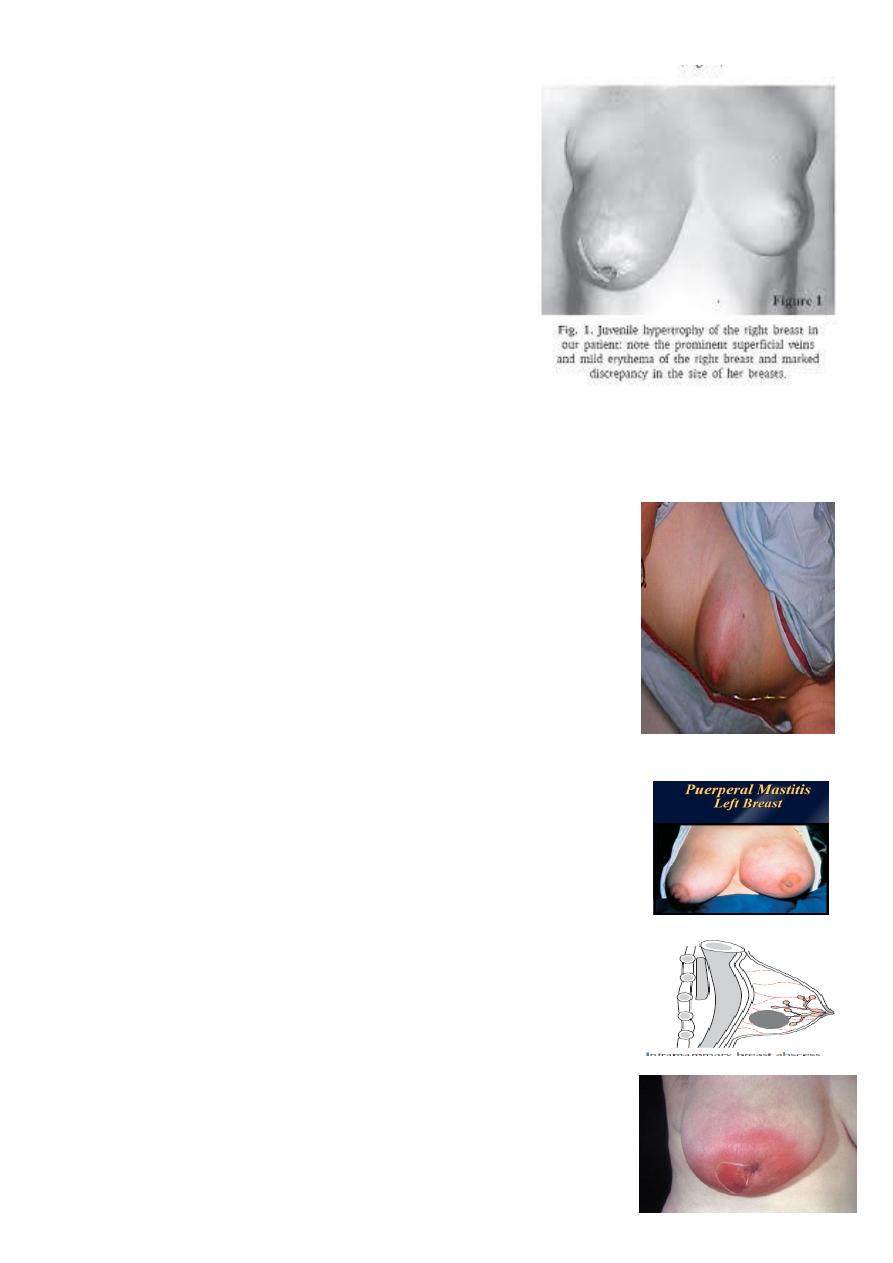
Diffuse hypertrophy
occurs in girls at puberty (benign virginal
hypertrophy) and less often, during the first
pregnancy.
The breasts enlarges and may reach the
knees when the patient is sitting, The
condition is rarely unilateral.
This caused by an alteration in the normal
sensitivity of the breast to oestrogenic
hormones and some success in treating it
with anti-oestrogens has been reported.
Treatment by reduction mammoplasty.
Infectious
Mastitis
Generalized cellulitis of the breast.
Ascending infection subareolar ducts
commonly occurs during lactation
Aetiology
Lactational mastitis in most cases are caused by
Staphylococcus aureus or Streptococcus spp .
The intermediary is usually the infant; after the second day
of life, 50% of infants harbour staphylococci in the
nasopharynx.
Although ascending infection from a cracked nipple
may initiate the mastitis.
Clinical features
The affected breast, or more usually a segment of it,
presents the classical signs of acute inflammation.
focal tenderness with erythema and warmth of
overlapping skin.
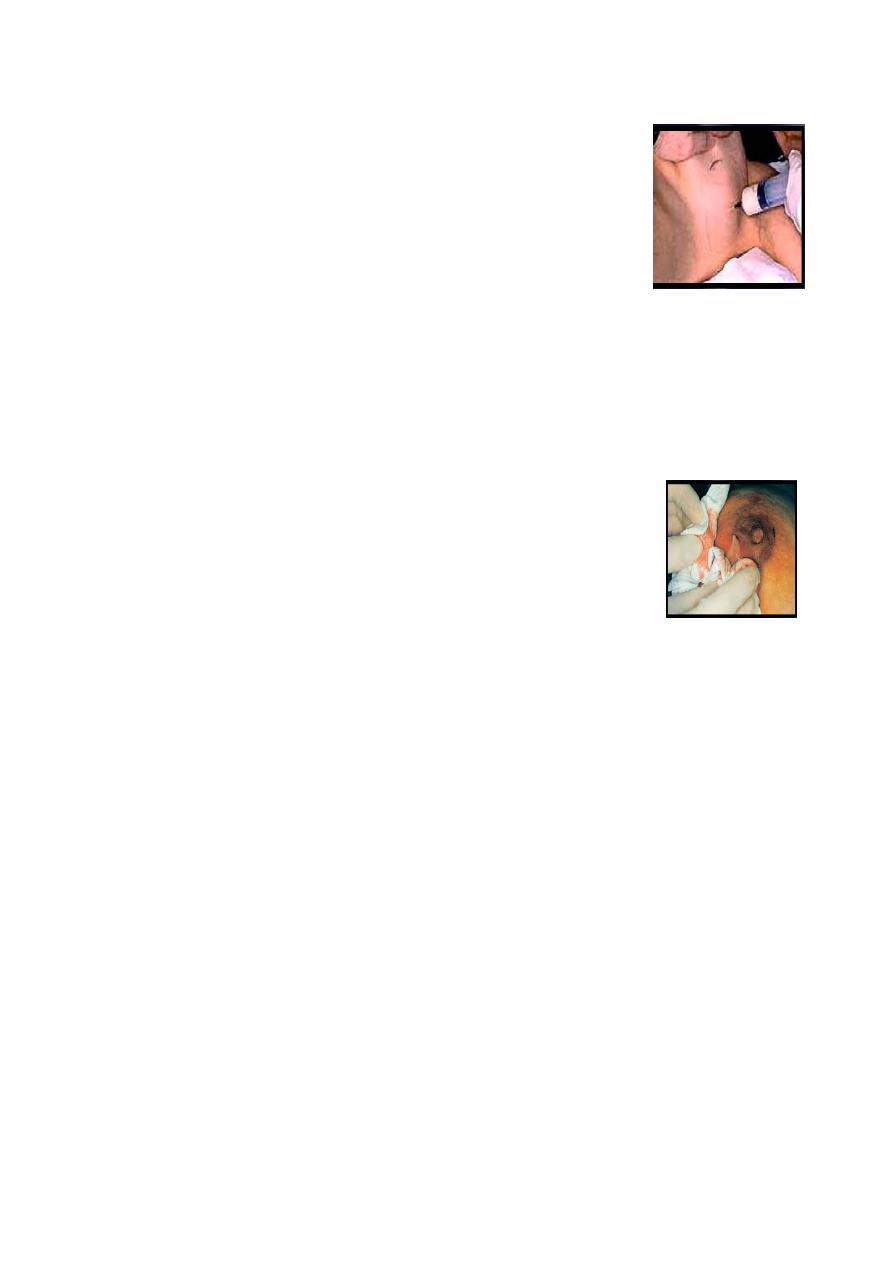
13
Early on this is a generalized cellulites but later an abscess will form.
• The presence of pus confirmed with needle aspiration.
• the pus sent for bacteriological culture.
• When in doubt an ultrasound scan may clearly define an area
suitable for drainage.
Treatment
• During the cellulitic stage the patient should be treated with an appropriate
antibiotic, for example flucloxacillin or co-amoxiclav.
• Feeding from the affected side may continue if the patient can manage and
recommend breast pump as an alternative..
• Support of the breast, and analgesia will help to relieve pain.
Breast Abscess
• Treated by surgical drainage
Chronic intramammary abscess
• A chronic intramammary abscess, which may follow inadequate drainage or
inprpoer antibiotic treatment, is often a very difficult condition to diagnose.
• When encapsulated amass will form within a thick wall of fibrous tissue the
condition cannot be distinguished from a carcinoma without the histological
evidence from a biopsy.
Antibioma:
• This is a large, sterile, brawny oedematous swelling that
takes many
weeks to resolve, may form If antibiotic is used in the presence of undrained
pus.
Mondor’s disease
• Phlebitis of the thoracoepigastric vein
• Palpable, visible, tender cord
• Ultrasound may be helpful in confirming this diagnosis.
• Treatment self-limited, can use anti-inflammatories if necessary
14
Tuberculosis Of The Breast
Rare, usually associated with active pulmonary
tuberculosis or tuberculous cervical adenitis.
Tuberculosis of the breast, presents with
multiple chronic abscesses and sinuses and a
typical bluish, appearance of the surrounding
skin.
Diagnosis
rests on bacteriological and histological examination.
Treatment :
anti-tuberculous chemotherapy.
Healing is usual, but delayed, and mastectomy restricted to patients with
persistent residual infection.
Inflammatory
Ductectasia / periductal mastitis
This is a dilatation of the breast ducts, which is often associated with
periductal inflammation.
The underlying cause is unknown, although the disease is common in
smokers.
Generally found in older women 5th and 6th decades .
The dilated lacteferouse ducts, filled with a stagnating brown or green
secretion.
Clinical features
This secretion may discharge, Nipple discharge
(of any colour) , thick, cheesy nipple discharge.
These fluids then set up an irritant reaction in
surrounding tissue leading to periductal mastitis
or even abscess and fistula formation.
In some cases, a chronic indurated mass forms
beneath the areola,
which mimics a
carcinoma.
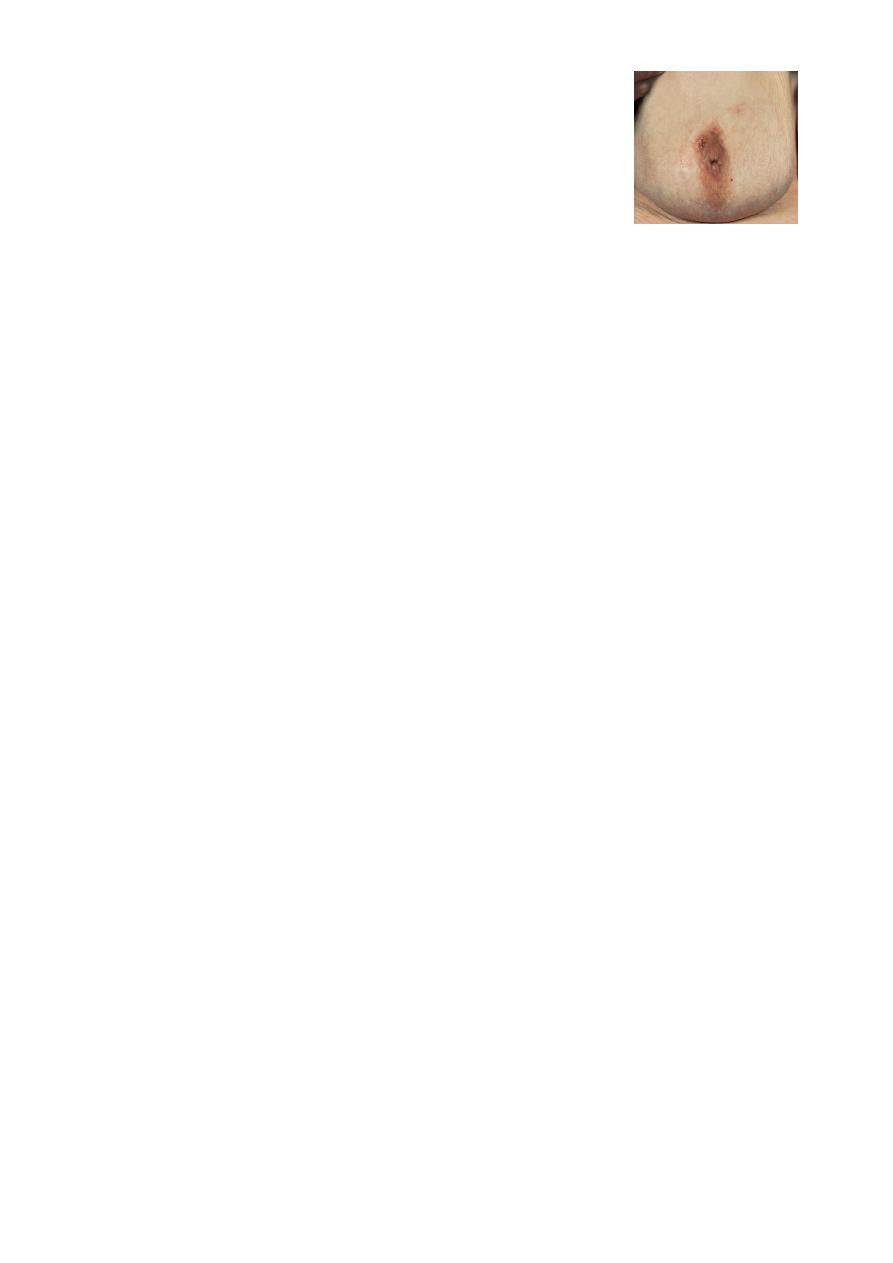
15
Fibrosis eventually develops, which may cause slit-
like nipple retraction.
Treatment
In the case of a mass or nipple retraction, a carcinoma must be excluded by
obtaining a mammogram and negative cytology or histology, If any
suspicion remains the mass should be excised.
Antibiotic therapy may be tried, the most appropriate agents being co-
amoxiclav or flucloxacillin and metronidazole.
surgery is often the only option likely to bring about cure of this difficult
condition; this consists of excision of all of the major ducts (Hadfield’s
operation).
Fibrocystic Disease
Fibrocystic changes affect 50-80% of all menstruating women.
Age 30-50, 10% < 21Y.
Exaggerated response from hormones and growth factors usually prior to
menstrual cycle.
Pathology
The disease consists essentially of four features that may vary in extent and
degree in any one breast.
Cyst formation:
Cysts are almost inevitable and very variable in size.
Fibrosis:
Fat and elastic tissues disappear and are replaced with dense white
fibrous trabeculae.
Hyperplasia:
of epithelium in the lining of the ducts and acini may occur, with or
without atypia.

16
Papillomatosis:
The epithelial hyperplasia may be so extensive that it results in
papillomatous overgrowth within the ducts.
Usually diagnosed 20 to 40 years
Present as pain and tenderness, palpable lumps, nipple discharge.
Often multifocal and bilateral , general “lumpiness”
• A solitary cyst or small collection of cysts can be aspirated. If they resolve completely
no further treatment is required.
• However, 30% will recur and require reaspiration.
• If there is a residual lump or if the fluid is blood-stained, a core biopsy or local
excision for histological diagnosis is advisable, which is also the case if the cyst
reforms repeatedly.
• This will exclude cystadenocarcinoma, which is more common in elderly women.
Mastalgia
Breast pain is the most common breast symptoms .
Classified as:
• Cyclical mastalgia.
• Non-cyclical mastalgia.
• Extra mammary (non breast) pain.
• It can be severe enough to interfere with usual daily activities.
• Cyclical mastalgia has a clear relationship to the menstrual cycle, due to hormonal
changes during luteal phase.
• Dull, diffuse and bilateral
• Non-cyclical mastalgia may be constant or intermittent but is not associated with the
menstrual cycle and often occurs after menopause.
• Extramammary pain arises from the chest wall or other

17
•
sources and its interpreted as a cause within the breast.
• The risk of cancer with breast pain as her only symptom is extremely low.
• Cancer must be excluded through examination, mammogram, and ultrasound if the
pain is localized.
• After clinical evaluation, most patients with breast pain respond by reassurance and
simple pharmacological measures.
Treatment of mastalgia
Cyclical mastalgia
• Firm reassurance that the symptoms are not associated with cancer will help the
majority of women.
• appropriate fitting supportive bra should be worn throughout the day and a soft bra
worn at night.
• Avoiding caffeine drinks is said to help.
• The medications danazol, tamoxifen, and bromocriptine are effective; however, the
serious adverse effects of these medications limit their use to selected patients with
severe, sustained breast pain.
Non-cyclical mastalgia
• It is important to exclude extramammary causes such as chest wall pain.
• This is common in postmenopausal women who are not on HRT and the neck and
shoulders are common sites of referred pain.
• Treatment may be with non-steroidal analgesics or by injection with local anaesthetic
on a ‘trigger spot’.

18
Benign masses
Galactocele
• rare, presents as a solitary, subareolar cyst and usually follows lactation.
• Milk-filled cyst & in longstanding cases its walls tend to calcify.
• Firm, tender mass.
• Diagnostic aspiration often curative.
Fibroadenoma
• These tumor are benign, mobile (breast mouse) , most common tumor in women
younger than age 30 years.
• They arise from hyperplasia of a single lobule Composed of both stromal and
epithelial elements and usually grow up to 2–3 cm in size, They are surrounded by a
well marked capsule.
• Can be diagnosed by FNA ,Otherwise Dx by excision.
•
Giant fibroadenomas occasionally occur during puberty.
They are over 5 cm in diameter and are often rapidly growing but,
in other respects, are similar to smaller fibroadenomas and can be
enucleated through a submammary incision.
19
Phyllodes tumour
• These are benign tumours.
• previously known as serocystic disease of Brodie or cystosarcoma phyllodes,
• occur in women over the age of 40 years but can appear in younger women.
• They are large, sometimes massive, tumour .
• Malignant potential.
• These may metastasise via the blood stream
• Occasionally, ulceration of overlying skin occurs because of pressure necrosis.
• Despite their size they remain mobile on the chest wall.
• They tend to recur locally .
Lipoma
• Nontender
• No associated skin or nipple changes
• Usually postmenopausal women
• Management- biopsy or excision
Injuries of the breast
Haematoma
• Haematoma, particularly a resolving
haematoma, gives rise to a lump, which, in the
absence of overlying bruising, is difficult to
diagnose correctly unless it is biopsied.
21
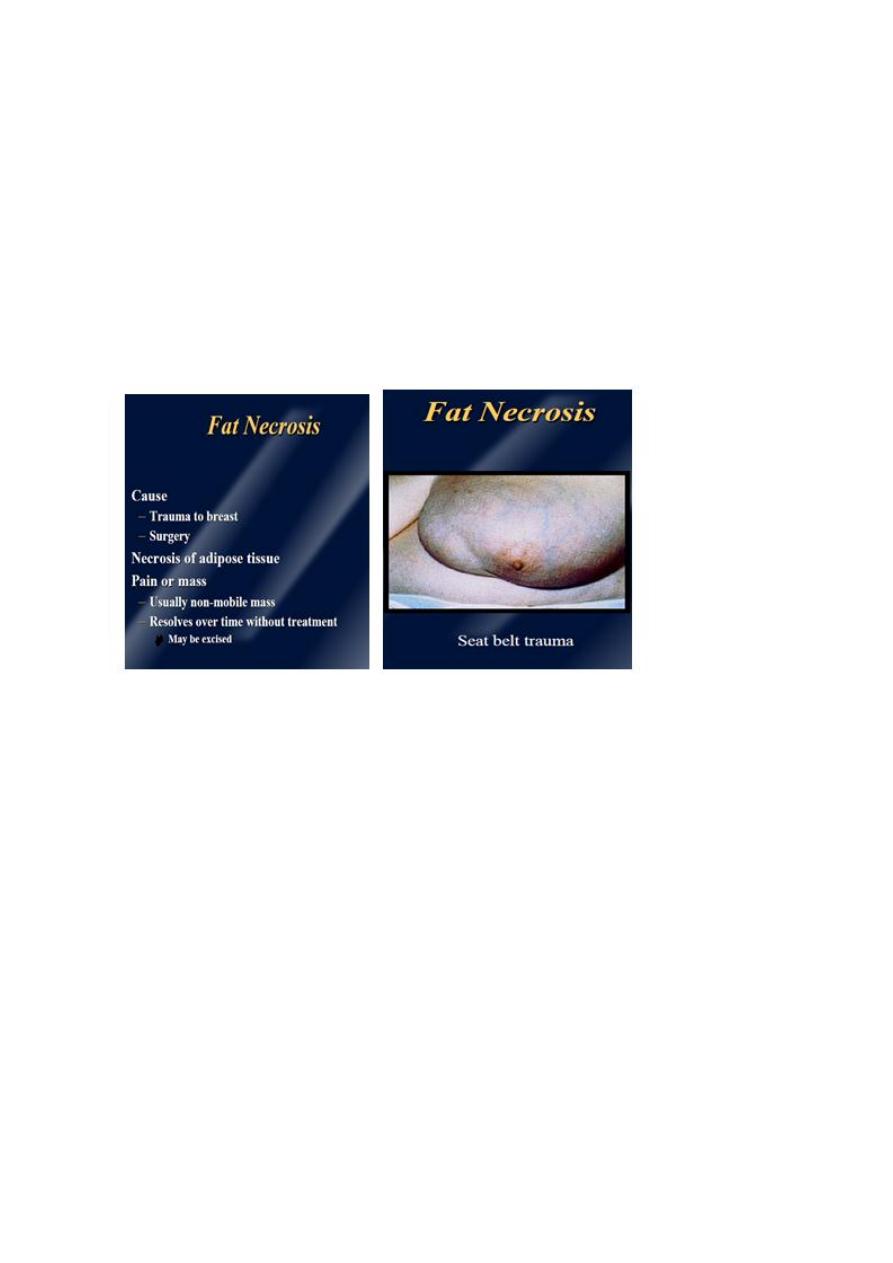
Fat Necrosis
• Traumatic fat necrosis may be acute or chronic and usually occurs in middle-aged
women.
• Following a blow a lump, often painless, appears.
• This may mimic a carcinoma, displaying skin tethering and nipple retraction, and
biopsy is required for diagnosis.
• A history of trauma is not diagnostic as this may merely have drawn the patient’s
attention to a pre-existing lump.

21
CARCINOMA OF THE BREAST
• Breast cancer is the most common cause of death in middle-aged women in western
countries.
• Breast cancer is second only to lung cancer as a cause of cancer deaths in women.
• One out of 8 women will be diagnosed with breast cancer.
Breast Cancer Facts
• 2nd leading cause of death
• 2nd most common cancer
• Incidence increases with age
• All women are at risk
Risk factors
• Age
• Gender
• Genetic
• Diet
• Endocrine
• Previous radiation
• Age Carcinoma of the breast is extremely rare below the age of 20 years but,
thereafter, the incidence steadily rises so that by the age of 90 years nearly 20% of
women are affected.
• Gender Less than 0.5% of patients with breast cancer are male.
• Genetic It occurs more commonly in women with a family history of breast cancer
than in the general population
• Diet breast cancer commonly affects women in the ‘developed’ world, dietary
factors may play a part in its causation, A high intake of alcohol is associated with an
increased risk of developing breast cancer.
22
Endocrine
• common in nulliparous women.
• breast feeding appears to be protective.
• Also protective is having a first child at an early age, especially if associated with late
menarche and early menopause.
• It is known that in postmenopausal women, breast cancer is more common in the
obese,This is thought to be because of an increased conversion of steroid hormones
to oestradiol in the body fat.
• Recent studies clarified the role of exogenous hormones, in particular the oral
contraceptive pill and HRT, in the development of breast cancer.
Previous radiation
• women who have been treated with radiotherapy as part of the management of
Hodgkin’s disease, in which significant doses of radiation to the breast are received.
• The risk appears about a 10 years after treatment and is higher if radiotherapy
occurred during breast development.
23
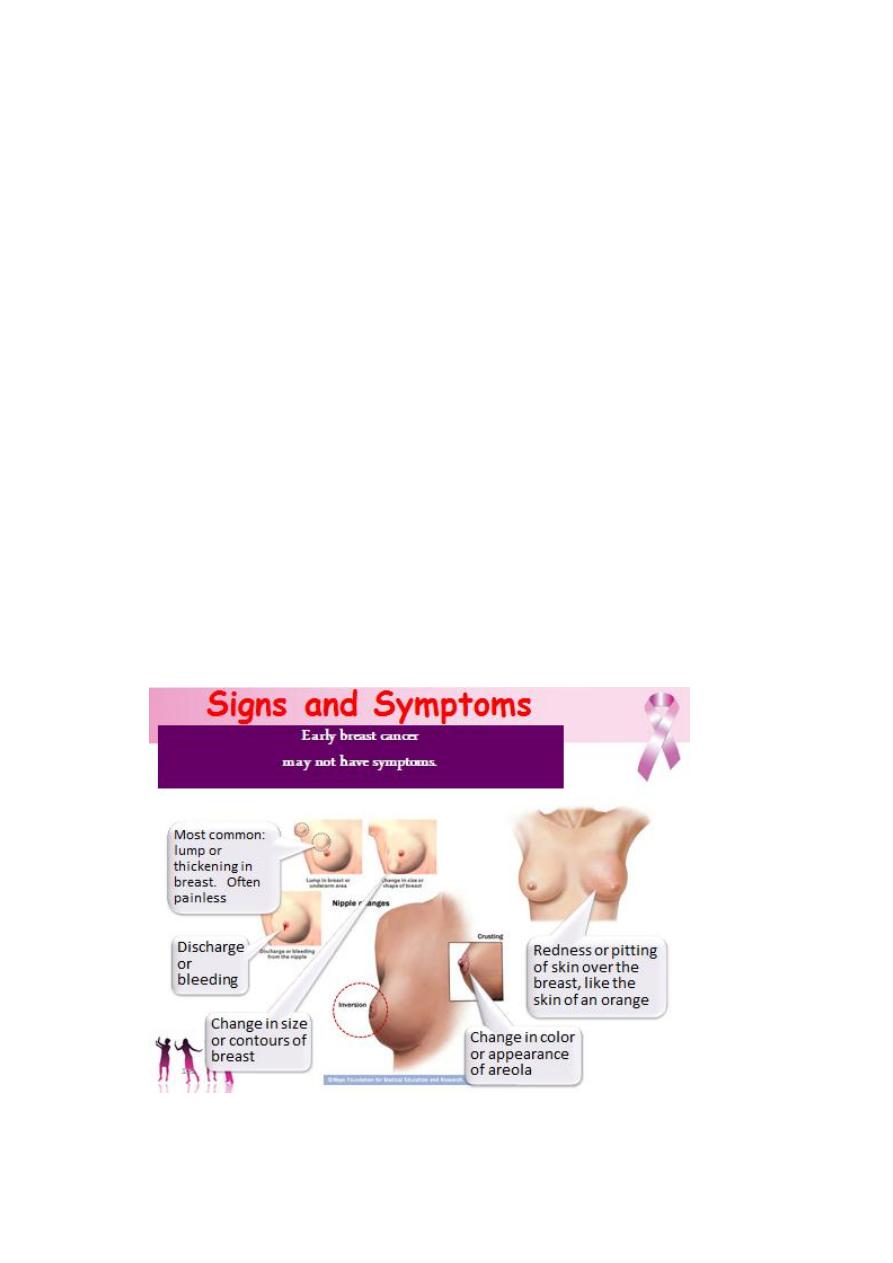
Symptoms of breast cancer
• Asymptomatic
• Why we advise yearly mammogram after age 40
• Lumps
• Presenting symptom in 85% of patients with carcinoma
• Pain
• Must completely evaluate to rule out carcinoma
• Metastatic disease
• Axillary nodes
• Distant organ symptoms, such as neurological
Signs of breast cancer
• Most breast cancers will present as a hard lump, which may be associated with
indrawing of the nipple.
• As the disease advances locally there may be skin involvement
with peau d’orange.
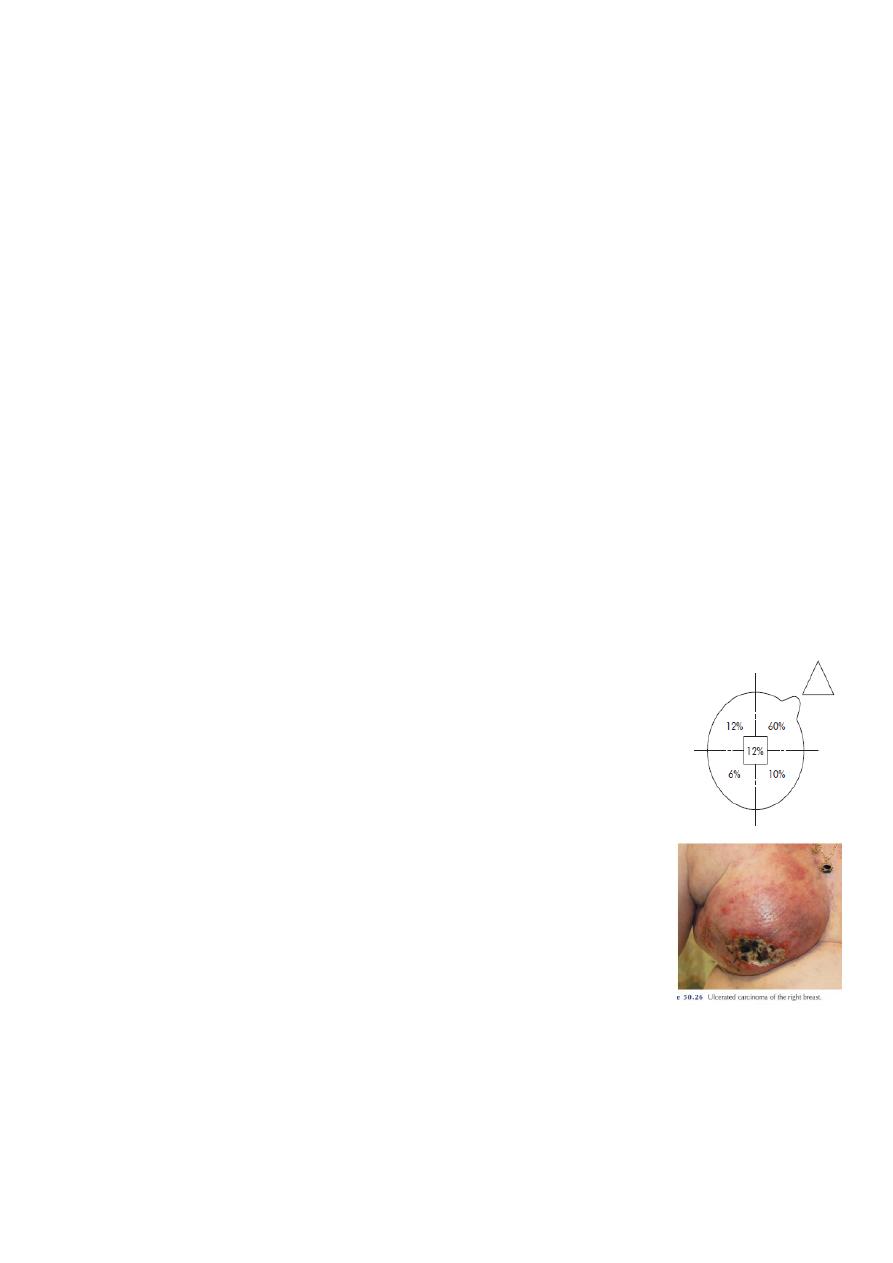
• Although any portion of the breast, including the axillary tail,
may be involved, breast cancer is found most frequently in the
upper outer quadrant .
• As the disease advances locally there may be ulceration and
fixation to the chest wall , described as cancer-en-cuirasse.
• 5% of breast cancers in the UK will present with either locally
advanced disease or symptoms of metastatic disease.
• This figure is much higher in the developing world.
• These patients must then undergo a staging evaluation(metastatic workup) , which
include:
– a careful clinical examination, chest radiograph, computerised tomography
(CT) of the chest and abdomen and pelvis and an isotope bone scan .

24
• Why we do this metastatic work up
•
This important for both prognosis and treatment; a patient with widespread
visceral metastases may obtain an increased length and quality of survival from
systemic hormone therapy or chemotherapy but is unlikely to benefit from surgery as
she will die from her metastases before local disease becomes a problem.
•
patients with relatively small tumours (< 5 cm in diameter) confined to the
breast and ipsilateral lymph nodes rarely need staging beyond a good clinical
examination as the pick-up rate for distant metastases is so low.
•
A chest radiograph, full blood count and liver function tests are all that are
recommended for screening of patients with early-stage breast cancer.
The spread of breast cancer
Local spread
• The tumour increases in size and invades other portions of the breast.
• It involve the skin and penetrate the pectoral muscles and chest wall if diagnosed
late.
Lymphatic metastasis
• occurs primarily to the axillary and the internal mammary lymph nodes.
• Involvement of supraclavicular nodes and contralateral lymph nodes represents
advanced disease.
Spread by the blood stream
• By this route bone metastases occur, In order of frequency the lumbar vertebrae,
femur, thoracic vertebrae, ribs and skull and these deposits are generally osteolytic.
• Metastases occur in the liver, lungs and brain and, the adrenal glands and ovaries.

25
Pathology
• Breast cancer may arise from the epithelium of the duct system anywhere from the
nipple end of the major lactiferous ducts to the terminal duct unit, which is in the
breast lobule.
• Cancer cells are in situ or invasive depending on whether or not they invade through
the basement membrane.
• The disease may be in situ, an increasingly common finding with the progress of
breast cancer screening, or invasive cancer.
• The degree of differentiation of the tumour is usually described using three grades:
• well differentiated,
• moderately differentiated
• poorly differentiated.
•
Grading system based on the scoring of three individual factors (nuclear
pleomorphism, tubule formation and mitotic rate) is used, with grade III cancers
roughly equating to the poorly differentiated group
.
Classifications
• I. Non-invasive breast cancers
• II. Invasive breast cancers
I. Non-invasive breast cancers
– 10% of all types of breast cancer
– Good prognosis
– Ductal carcinoma in situ, lubular carcinoma in situ, and paget’s disease
Ductal Carcinoma in Situ
• Seen as microcalcifications on mammogram
• Confined to ductal cells.
• No invasion of the underlying basement membrane.
• Chance of recurrence 25-50% in 5 years.

26
Rx
– Wide excision alone suitable and the margins are clear.
– Wide local excision and radiation reduce local recurrence to 2%
– Node dissection not necessary (nodal disease < 1%)
– Mastectomy an option if there is a substantial risk of local/regional recurrence
Lobular Carcinoma in Situ
• Not detectable on mammography
• Most commonly found incidentally
• Risk of invasive breast cancer in 20 years is 15-20% bilaterally
Rx
• Careful follow-up
• Bilateral masectomy may be considered if other risk factors are present such as
family history or prior breast cancer, and also dependent on patient preference.
Paget’s disease of the nipple
• Uncommon, Usually involves the nipple.
• It is a superficial manifestation of an underlying breast carcinoma.
• Eczematous dermatitis of the nipple, which persists despite local treatment.
• The nipple is eroded slowly and eventuall disappears.
• If left, the underlying carcinoma will sooner or later become clinically evident.
• Nipple eczema should be biopsied if there is any doubt about its cause.
• It is associated with an underlying intraductal carcinoma.
– Mammography should be performed
– About 30% of patients have axillary node metastasis at diagnosis.
• Mastectomy is the standard care of treatment
– 80% have a 10 year survival rate if there is no mass present and no axillary
nodes are involved.

27
II. Invasive breast cancers
– Favorable histologic types
– Less favorable types
– Least favorable type
Favorable histologic types
• Tubular carcinoma
• Mucinous (colloid) carcinoma
• Papillary carcinoma
2-3% of all invasive breast cancers .
5 and 10 year survival rates are 73 and 59 %.
Less Favorable Histologic Types
• Invasive ductal carcinoma
– Most common and occurs in 78% of all invasive breast cancers.
– Metastases to axillary nodes in 60%
– 5 and 10 year survival rates are 54 and 38 %
• Invasive lobular carcinoma
– 9% of all invasive breast cancers
– Metastases to axillary nodes in 60%
– 5 and 10 year survival rates are 50 and 32 %
– Higher incidence of bilaterality
Least favorable type
Inflammatory carcinoma
• 1.5 - 3% of breast cancers
• Characteristic clinical features of erythema, peaud’orange, and skin ridging with or
without a palpable mass.
28
• Commonly mistaken for cellulitis.
– Will generally fail antibiotics before being diagnosed
• Disease progresses rapidly, and more than 75% of patients present with palpable
axillary nodes.
• Distant metastatic disease also at much higher frequency than the more common
breast cancers.
• 30% 5 year survival rate
• Requires chemotherapy treatment immediately
Diagnosis of breast cancer
1. Fine-needle aspiration
Sensitivity is 80-98%, specificity 100%
False negatives are 2-10%.
2. Core-needle biopsy
More tissue, however still possibility of false “negative” and could represent sampling error.
3. Excisional biopsy
Removal of entire lesion and a margin of normal breast parenchyma.
Staging, Prognosis, And Treatment
Staging of breast cancer
• The clinical stage of breast cancer is determined primarily through physical
examination of the skin, breast tissue, and regional lymph nodes (axillary,
supraclavicular, and cervical).
• Mammography, chest radiography, an intraoperative findings (primary tumor size,
chest wall invasion) also provide necessary staging information.
• Pathologic stage combines the findings from pathologic examination of the resected
primary breast cancer and axillary or other regional lymph nodes.
Classical staging of breast cancer by means of the TNM (tumour– node–metastasis) .
29
Staging and Prognosis
• Primary Tumor
– T1 = Tumor < 2 cm. in greatest dimension
– T2 = Tumor > 2 cm. but < 5 cm.
– T3 = Tumor > 5 cm. in greatest dimension
– T4 = Tumor of any size with direct extension to chest wall or skin
Regional Lymph Nodes
– N0 = No palpable axillary nodes
– N1 = Metastases to movable axillary nodes
– N2 = Metastases to fixed, matted axillary nodes
Distant Metastases
– M0 = No distant metastases
– M1 = Distant metastases including ipsilateral supraclavicular nodes
31
Clinical Staging and prognosis
– Clinical Stage I
T1 N0 M0)
– Clinical Stage IIA
T1 N1 M0
T2 N0 M0
– Clinical Stage IIB
T2 N1 M0
T3 N0 M0
– Clinical Stage IIIA
T1 N2 M0
T2 N2 M0
T3 N1 M0
T3 N2 M0
– Clinical Stage IIIB
T4 any N M0
– Clinical Stage IV
any T any N M1
Stage Prognosis (5 year surv. Rate)
– I 93%
– II 72%
– III 41%
– IV 18%
Breast Cancer Treatments Modalities
– Surgery
• Local treatment
– Radiation
• Local treatment
– Chemotherapy and hormonal therapy
• Systemic treatment

31
Surgery
– Breast conservation surgery (BCS)
• Stage I, stage II, and sometime stage III carcinomas
• Lumpectomy, axillary lymphadenectomy, and postoperative radiation
therapy
• Contraindications:
tumors > 5 cm , gross multifocal disease, and diffuse malignant microcalcifications by
mamography.
• Local recurrence more than mastectomy so follow up important
– Modified radical mastectomy
(most common mastectomy procedure for invasive breast cancer)
• Entire breast and axillary contents are removed
• Pectoralis muscles remains
– Halsted radical mastectomy
• Removes breast, axillary contents, and pectoralis major muscle
• Cosmetically deforming
• Only indicated when pectoralis muscle involved
– Simple mastectomy
• All breast tissue is removed, axillary contents not removed
• Treatment for non-invasive breast cancer
Sentinel node biopsy
• The sentinel node is defined as the first lymph node draining the tumour-bearing
area of the breast.
• This technique is currently becoming the standard of care in the management of the
axilla in patients with clinically node-negative disease.
32
• The sentinel node is localised peroperatively by the injection of patient blue dye and
radioisotope-labelled albumin in the breast.
• The recommended site of injection is in the subdermal plexus around the nipple
although some still inject on the axillary side of the cancer.
• The marker passes to the primary node draining the area and is detected visually and
with a hand-held gamma camera.
• The excised node can be sent for frozen-section histological analysis
• In patients in whom there is no tumour involvement of the sentinel
node, further axillary dissection can be avoided.
Radiation
• Utilized for primary and metastatic disease
• Useful in breast conservation therapy to reduce rate of recurrence.
• Radiate entire breast
Chemotherapy
– Eradicates risk of occult distant disease in stage I and stage II patients.
– All patients with axillary node involvement are candidates along with patients
with negative axillary node involvement who are high risk by other prognostic
indicators.
– Example treatment is 6 months of cyclophosphamide, methotrexate or
adriamycin, and flourouracil along with paclitaxel.
• Improvement in disease free interval and overall survival
Hormonal therapy
– Tamoxifen
• Generally taken for five years in patients with estrogen
receptor positive tumors.
33
• As effective as chemotherapy in post-menopausal
patients with estrogen receptor positive tumors
Treatment of advanced breast cancer
• Breast cancer may present as metastatic disease without evidence of a primary
tumour (occult primary).
• The diagnosis is made by exclusion of another site
for the primary tumour and confirmed by histology with special
immunohistological stains of the metastatic lesions.
• Management by palliation of symptoms and treatment of breast cancer by
endocrine manipulation with or without radiotherapy.
Locally advanced inoperable breast cancer
• Locally advanced inoperable breast cancer, including inflammatory breast cancer, is
usually treated with systemic therapy, either chemotherapy or hormone therapy.
• Occasionally, ‘toilet mastectomy’ or radiotherapy is required to control a fungating
tumour.
Metastatic carcinoma of the breast
• Metastatic carcinoma require palliative systemic therapy to alleviate symptoms.
1) Hormonal manipulation: is the first-line treatment because of its minimal side
effects, hormonal therapy like Tamoxifen, It is particularly useful for bony
metastases.
2) Surgery: for ovarian suppression (premenopausal women).
3) Radiotherapy : for bone mets.
4) Cytotoxic therapy : used in younger women, visceral metastases, rapidly growing
tumours.
5)Local treatment : may also prove useful for some metastatic disease such as
radiotherapy for painful bony deposits and internal fixation of pathological fractures.

34
Follow-up of breast cancer
• Patients with breast cancer used to be followed for life to detect recurrence and
dissemination.
• It is current practice to arrange yearly or 2-yearly mammography of the treated and
contralateral breast.
• There is currently no routine role for repeated measurements of tumour markers or
imaging other than mammography if no new symptoms or signs appear .
Screening for breast cancer
• a population screening programme that could detect tumours before they come to
the patient’s notice might reduce mortality from breast cancer, a number of studies
have shown that breast screening by mammography in women over the age of 50
years will reduce mortality .
• self examination programmes that have benefit for the population in terms of earlier
detection or decreased
mortality from breast cancer .
Familial breast cancer
• Recent developments in molecular genetics and the identification of a number of
breast cancer predisposition genes (BRCA1, BRCA2 and p53).
• Those who prove to be ‘gene positive’ have a 50–80% risk of developing breast
cancer, predominantly while premenopausal.
• Many will have option for prophylactic mastectomy.
• This work should be carried out in special centres.
35
Pregnancy
Breast cancer presenting during pregnancy or lactation tends to be at a later stage,
because the symptoms are masked by the pregnancy;
Treatment : is similar with some precautions:
• Mastectomy is agood option than breast conservening surgery.
• Chemotherapy avoided during the 1st trimester but safe subsequently.
• Radiotherapy should be avoided during pregnancy.
• Hormonal therapy, which is potentially teratogenic, is not required.
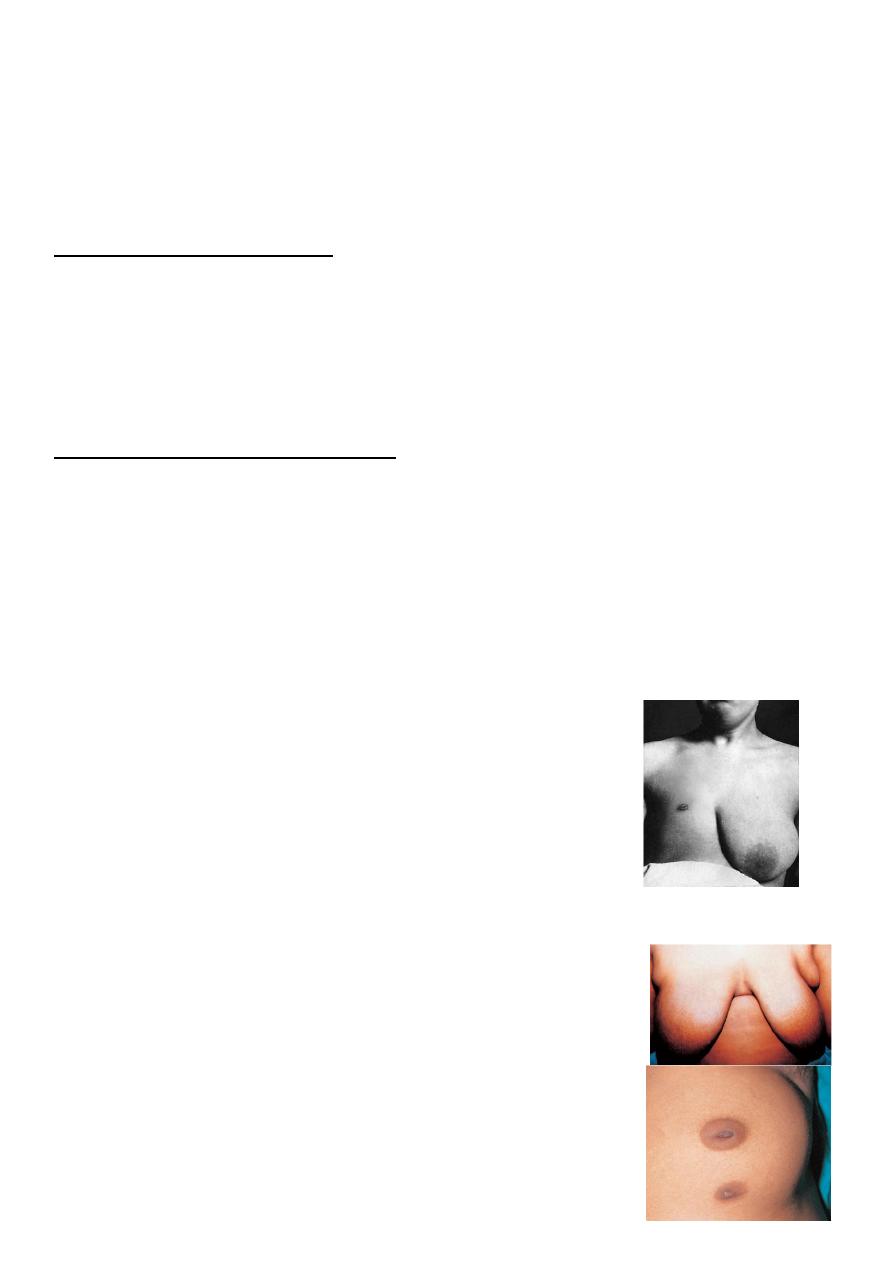
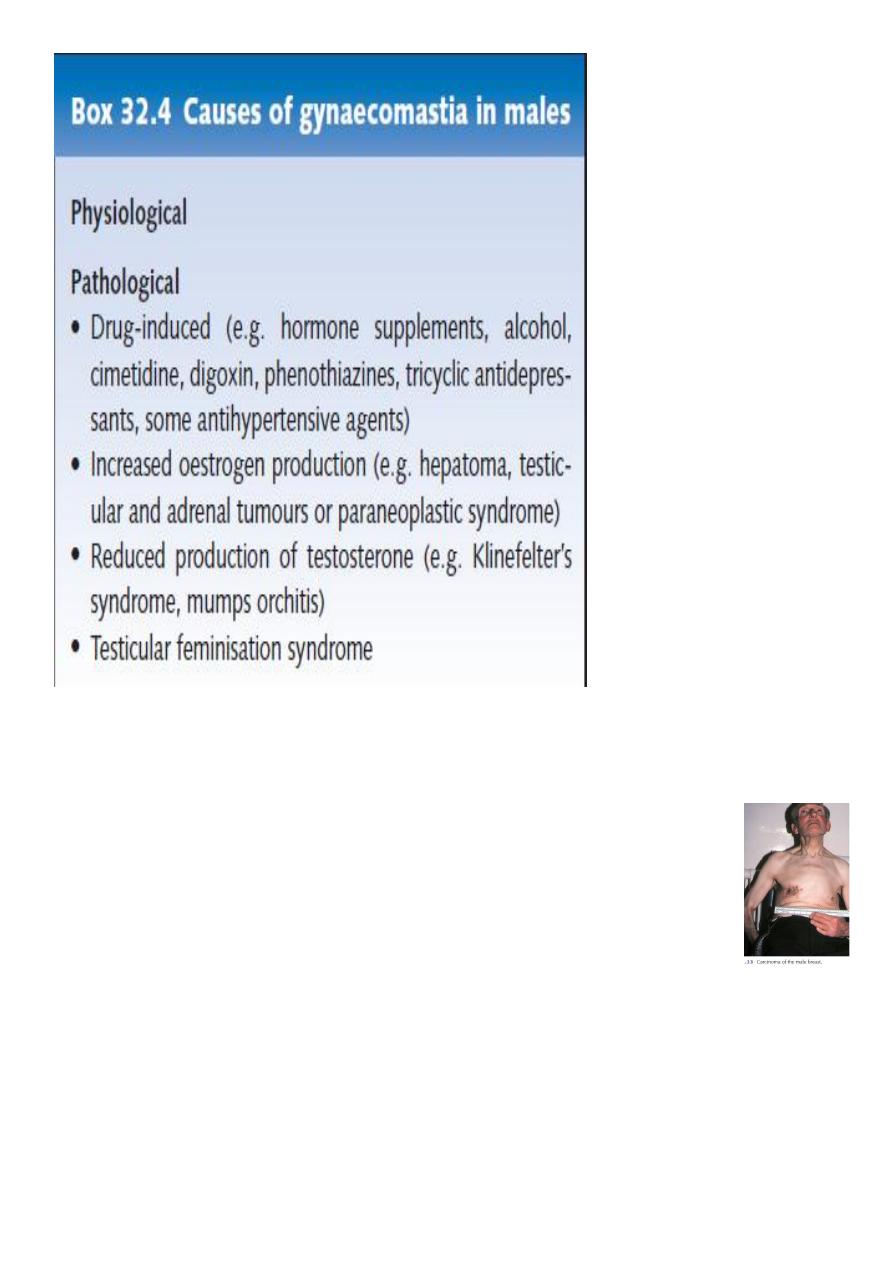
The Male Breast
Gynecomastia
• The most common breast problem in men is gynecomastia.
• Gynecomastia is a benign hypertrophy of breast tissue.
• The unilateral gynecomastia patient usually presents with a discoid mass
symmetrically placed beneath the areola, which may be tender to palpation.
Prepubertal gynecomastia
• Rare, adrenal carcinoma and testicular tumor can cause this.
• Pubertal gynecomastia
• Occurs in 60-70% of pubertal boys.
• Senescent gynecomastia
• 40% of aging men have this to some degree.
• Drugs, such as steroids, digitalis, hormones,
spironolactone, and antidepressants can cause
this.
36
Male breast carcinoma
– 0.7% of all breast cancers
– <1% of male cancers
– Average age of diagnosis is 63.6 years old
– Painless unilateral mass that is usually subareolar with skin
fixation, chest wall fixation,, and ulceration.
– Mostly ductal carcinoma
– Males generally present at later stage than woman
• Overall survival worse in men, however when compared stage for stage
the survival rates are similar.
37
