Prof. Dr. Faeza Aftan
Dept of PathologyCol of Med
Aliraqia University
Oct. 21st 2015
Small & Large Intestine IBD
SMALL/LARGE INTESTINE
NORMAL: Anat., Vasc., Mucosa, Endocr., Immune, Neuromuscular.PATHOLOGY:
CONGENITAL
ENTEROCOLITIS: DIARRHEA, INFECTIOUS, OTHER
MALABSORPTION: INTRALUMINAL, CELL SURFACE, INTRACELL.
(I)IBD: CROHN DISEASE and ULCERATIVE COLITIS
VASCULAR: ISCHEMIC, ANGIODYSPLASIA, HEMORRHAGIC
DIVERTICULOSIS/-IT IS
OBSTRUCTION: MECHANICAL, PARALYTIC (ILEUS) (PSEUDO)
TUMORS: BENIGN, MALIGNANT, EPITHELIAL, STROMAL
Clinical Features
Adults, celiac disease 30 and 60 Year
silent celiac disease,
anemia (due to iron deficiency, less, B12 and folate deficiency), diarrhea, bloating, and fatigue.
Pediatric celiac disease, 6 and 24 months
dermatitis herpetiformis
Dermatitis Herpitiformis (DH)
T cell lymphoma,S Int Ca.
Sq cell ca. esophagus
Causes of subtotal villous atrophy
Coeliac Dis
Giardiasis
Lymphoma
DH
Tropical sprue (Enviromental enteropathy)
AIDS
Others
Cystic Fibrosis
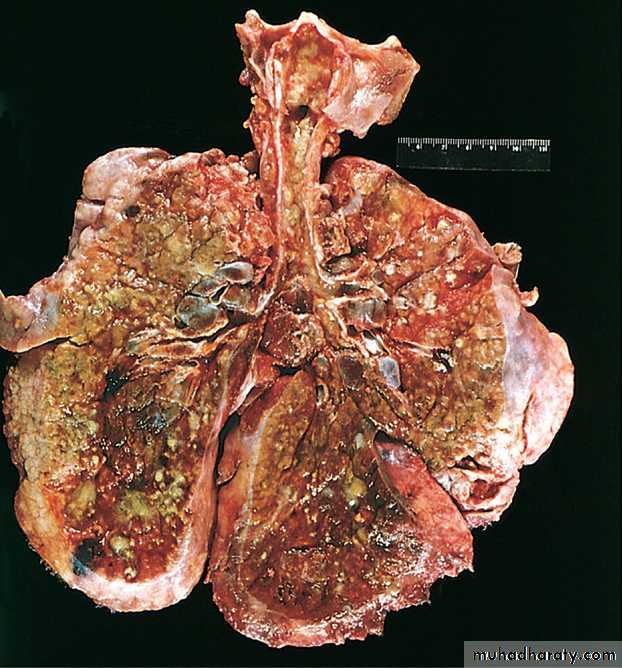
Lungs of a cystic fibrosis. Extensive mucous plugging the tracheobronchial tree.The parenchyma is consolidated by both secretions &pneumonia; the greenish discoloration is the Pseudomonas infections.
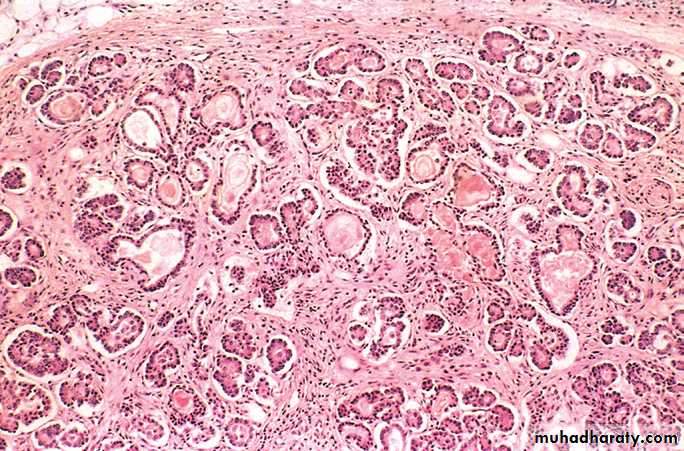
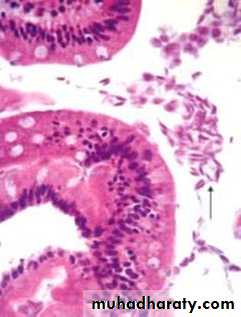
Cystic fibrosis in the pancreas.
The ducts are dilated and plugged with eosinophilic mucin, and the parenchymal
glands are atrophic and replaced by fibrosis __ Pancreatic insufficiency, ___ Malabsorption
Malabsorptive Diarrhea
Irritable bowel syndrome (IBS); chronic, relapsing abdominal pain, bloating, and changes in bowel habits.
- Stress, Diet, GIT motility
- No gross or Mic abnormalities.
- Colitis, celiac disease, giardiasis, cancer, & IBD should be excluded.
The Microscopic colitis,
collagenous colitis &
lymphocytic colitis,
both cause chronic watery diarrhea.
The intestines are grossly normal, and the diseases
are identified by their histologic features.
- Ass with Celiac & Autoimmune dis.
Infectious Enterocolitis
Vibrio cholerae secretes toxin that causes massive chloride secretion, H2O follows & diarrhea.Campylobacter jejuni .
Salmonella and Shigella spp. are invasive , dysentery.
Nontyphoid Salmonella cause ood poisoning.
S. typhi cause systemic disease (typhoid fever).
Pseudomembranous colitis ; AB allows C. difficile to grow & releases toxins, The inflammatory response volcanolike eruptions of PMN from colonic crypts that form mucopurulent pseudomembranes.
Rotavirus is the most common cause of childhood diarrhea
Parasitic and protozoal infections affect over half of the world’s population on a chronic or recurrent basis
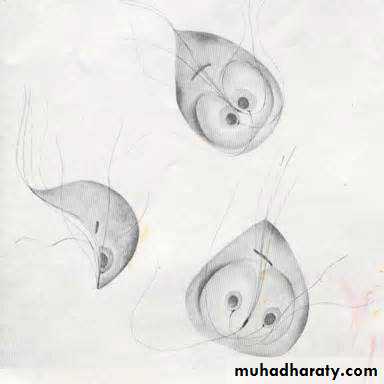
ENTAMOEBA HISTOLYTICA
“please do not drink the water”.
GIARDIA LAMBLIA“please do not drink the water”.
“Environmental (Tropical) EnteropathyTropical enteropathy or tropical sprue
Repeated bouts of diarrhea within the first 2 or 3 years of life
Epidemic forms in developing countries
NOT related to gluten
No single infectious agent.
RECOVERY with antibiotics
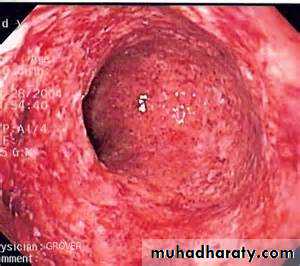
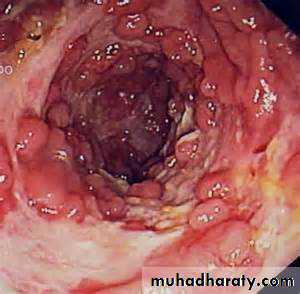
CLOSTRIDIUM DIFFICILE (ANTIBIOTIC ASSOCIATED) COLITIS
NOSOCOMIAL
CYTOTOXIN (lab test readily available)
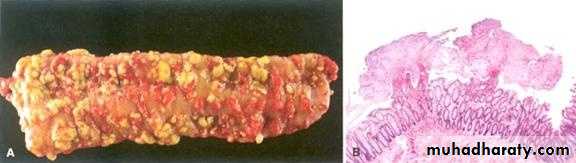
PSEUDOMEMBRANOUS (ANTIBIOTIC ASSOCIATED) COLITIS
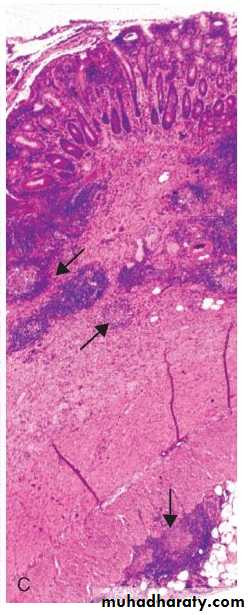
Clostridium difficile colitis. A, The colon is coated by tan pseudomembranes composed of neutrophils, dead epithelial cells, and inflammatory debris (endoscopic view). B, Pseudomembranes . C, Typical pattern of neutrophils emanating from a crypt is reminiscent of a volcanic eruption
BACTERIAL OVERGROWTH SYNDROME
One of the main reasons why “normal” gut flora is NOT usually pathogenic, they are constantly cleared by a NORMAL transit timeBLIND LOOPS
DIVERTICULA
OBSTRUCTION
Bowel PARALYSIS
(I) IBD
Idiopathicfemales , young adults.
Western industrialized nations
- Genetic factors .
- The hygiene hypothesis;
Early in life Limit mucosal IR & loss of intestinal
epithelial barrier function
- later in life, exposure of susceptible individuals to
harmless microbes triggers inappropriate IR
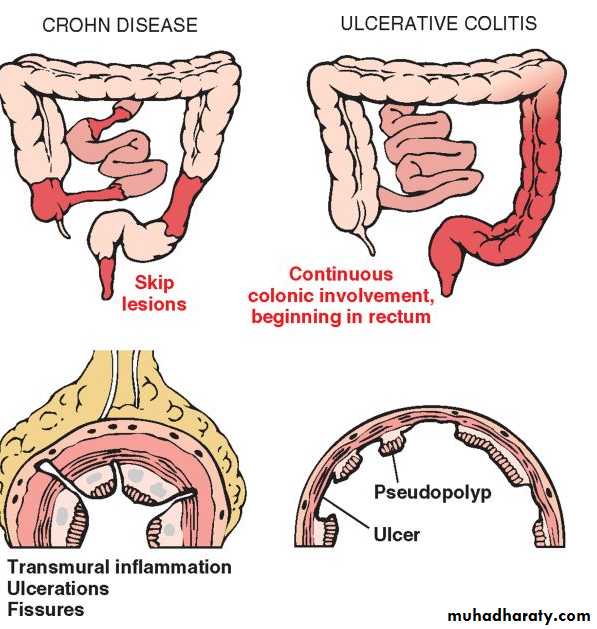
The distinction between UC & CD is based, on
Distribution of the lesionMorphology of disease
(I) IBD
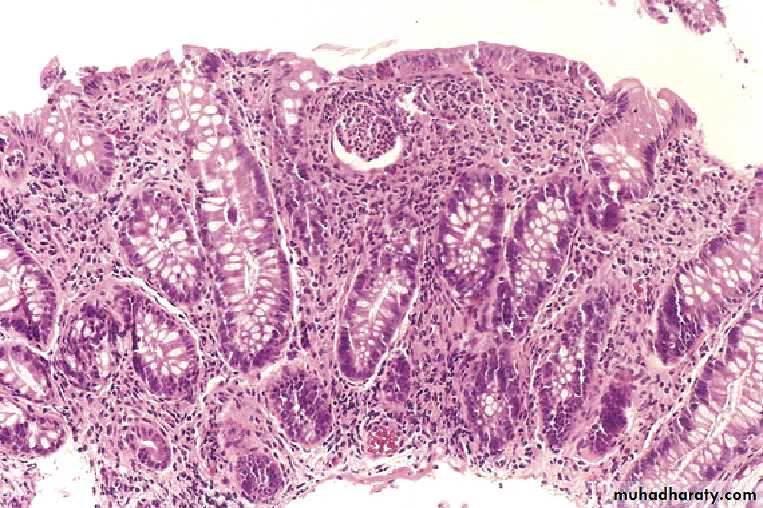
Ulcerative Colitisdisease begins in rectum & extends proximally (no skip lesions)
does not involve small intestines
superficial mucosal involvement (not transmural)
crypt abscesses (microabscesses) and crypt distortion
Pseudopolyp
increased risk of colon cancer and toxic megacolon
Crohn Disease
transmural involvement → fissures, fistulas, and obstruction
segmental involvement (skip lesions)
may involve small intestines (regional enteritis or ileitis)
Granulomas
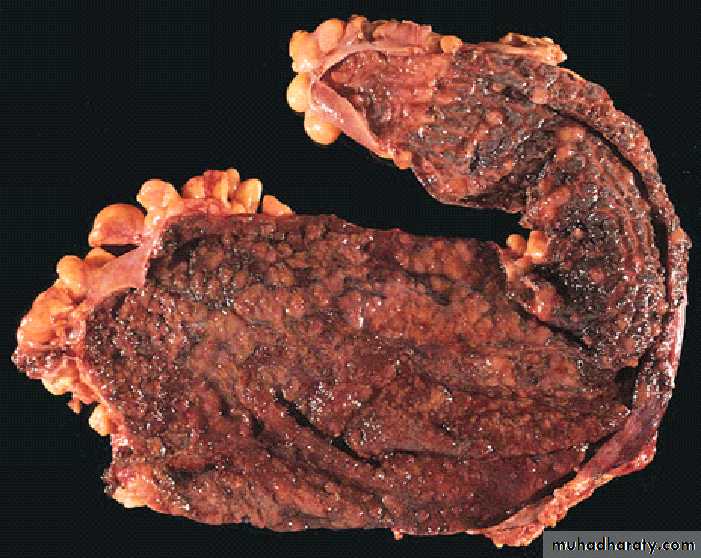
Ulcerative Colitis
Ulcerative proctitis or ulcerative proctosigmoiditis
Pancolitis.
Backwash ileitis.
Pseudopolyps
Toxic megacolon
Increased cancer risk
Active disease superf. Ulcer & hemorrhage
Pseudopolyps
UCinfectious enteritis
psychologic stress,
smoking cessation in some patients, and smoking may partially relieve symptoms.
Ulcerative Colitis
PSEUDOPOLYPSCrypt Abscess
Ulcerative Colitis
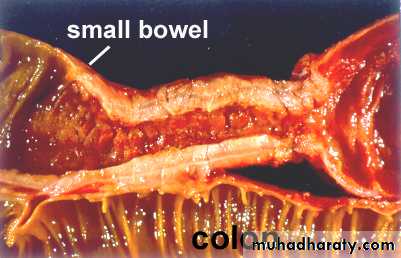
Crohn diseaseTerminal ileum, ileocecal valve, and cecum.
S. Int alone in 40% of cases;
S Int & colon are both involved in 30%
skip lesions
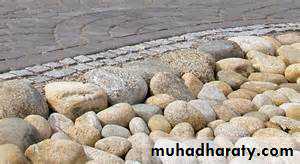
Cobblestone
Fissures
Fistula tracts
Strictures are common
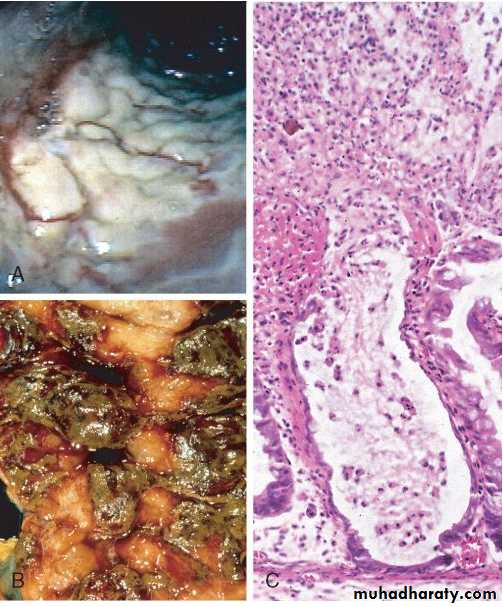
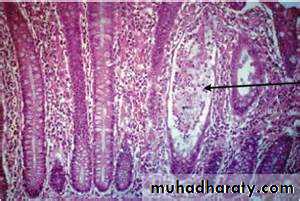
Crohn’s Disease
Transmural inflammation
• Cobblestones
• Skip areas
Scarring and stricture formation
Fistulae
• Crohn’s Dis.
• Cobble stones
• Skip areas
Crohn’s Dis.Scarring and stricture formation
Transmural Crohn disease with submucosal and serosal granulomas (arrows).
Crohn’s Dis.
Cobblestones
Extraintestinal manifestations ;erythema nodosum , arthritis, uveitis, pericholangitis and ankylosing spondylitis.
Indeterminate Colitis
Pathologic and clinical overlap between UC & CD.10% of IBD patients
Colonic disease in a continuous pattern (typical UC).
However, patchy pattern, fissures, a family history of Crohn disease, perianal lesions, onset after cigarettes, or other features that are not typical of UC.
Perinuclear anti-neutrophil cytoplasmic Abs are positive in 75% of UC, but only 11% with CD.
Colitis-Associated Neoplasia
The risk of dysplasia is related to :The frequency & severity of active disease
Duration, risk increases 8 - 10 years after disease initiation.
Pancolitis are at greater risk than those with only left-sided disease
Primary sclerosing cholangitis,
anti-TNF Ab Rx can suppress the development of colitis-associated cancers in experimental animals.