
Fifth stage
عيون
Lec-1
د.نزار
20/10/2015
GROSS ANATOMY
GROSS ANATOMY
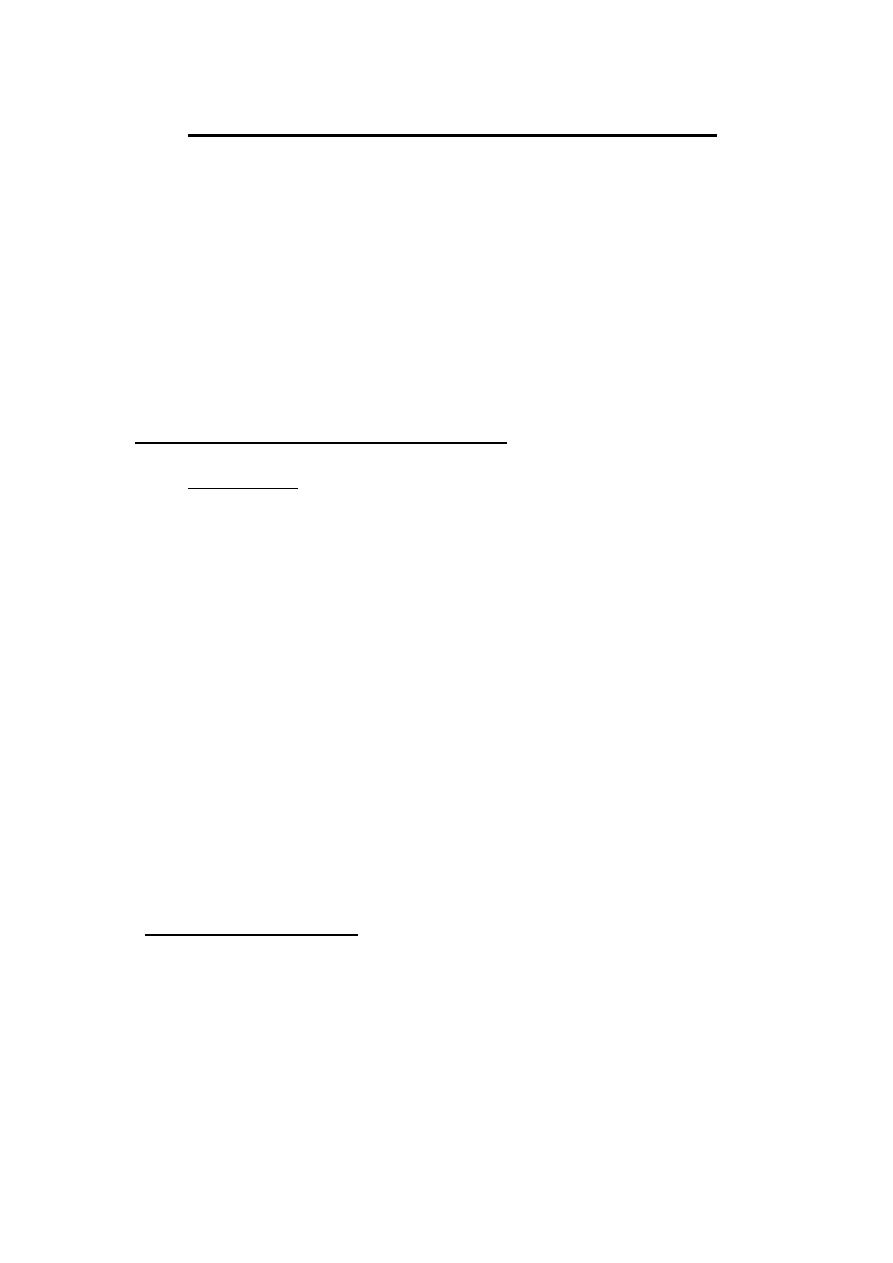
The eye comprises:
A tough outer coat which is transparent anteriorly (the cornea) and
opaque posteriorly (the sclera). The junction between the two is
called the limbus. The extraocular muscles attach to the sclera
while the optic nerve leaves the sclera posteriorly through the
cribriform plate.
A rich vascular coat (the choroid) lines the posterior segment of the
eye and nourishes the retina at its inner surface.
The ciliary body lies anteriorly. It contains the smooth ciliary
muscle whose contraction alters lens shape and enables the focus of
the eye to be changed. The ciliary epithelium secretes aqueous
humour and maintains the ocular pressure. The ciliary body
provides attachment for the iris.
The lens lies behind the iris and is supported by fine fibrils (the
zonule) running between the lens and the ciliary body.
The angle formed by the iris and cornea (the iridocorneal angle) is
lined by a meshwork of cells and collagen beams (the trabecular
meshwork). In the sclera outside this, Schlemm’s canal conducts
the aqueous humour from the anterior chamber into the venous
system, permitting aqueous drainage. This region is termed the
drainage angle.
Between the cornea anteriorly and the lens and iris posteriorly lies the
anterior chamber. Between the iris, the lens and the ciliary body lies
the posterior chamber). Both these chambers are filled with aqueous
humour. Between the lens and the retina lies the vitreous body.
Anteriorly, the conjunctiva is reflected from the sclera onto the
underside of the upper and lower eyelids. A connective tissue layer
(Tenon’s capsule) separates the conjunctiva from the sclera and is
prolonged backwards as a sheath around the rectus muscles
Cornea
Tendon
of
extraocular
muscle
Lens
Iris
Schlemm's
canal
Iridocorneal angle
Conjunctiva
Posterior
chamber
Sclera
Choroid
Retina
Anterior
chamber
Limbus
Zonule
Ciliary
body
Ora serrata
Vitreous
Fossa
for
lacrimal
gland
Superior orbital fissure
Inferior
Lesser wing of sphenoid
Orbital
plate of great
wing of sphenoid
Frontal
bone
Nasal bone
Lacrimal bone
and
fossa
Orbital plate
of
Supraorbital notch
Optic
foramen
Maxillary process
Ethmoid

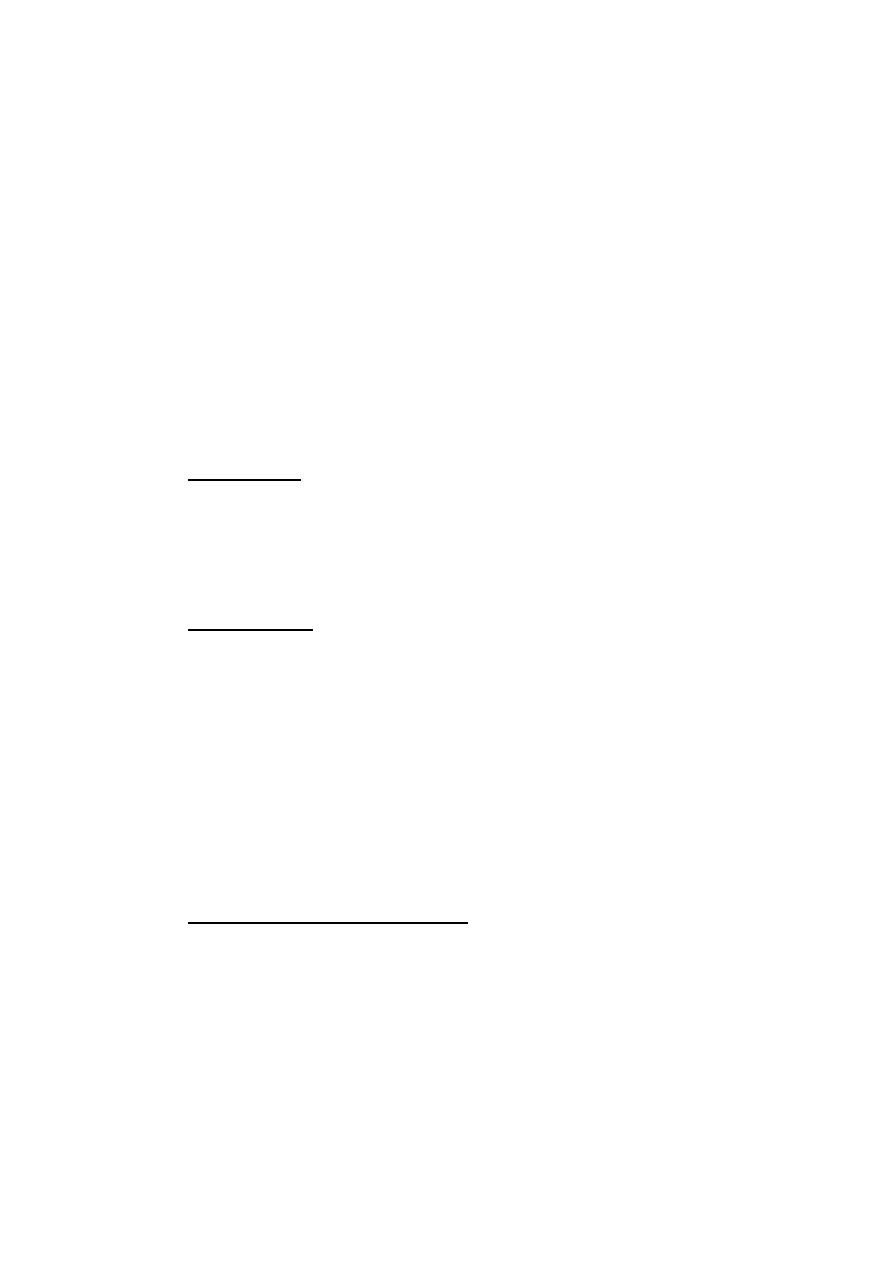
ORBIT (Fig. 1.2)
The eye lies within the bony orbit whose structure is shown in Fig.
1.2.The orbit has the shape of a four-sided pyramid. At its posterior
apex is the optic canal which transmits the optic nerve to the brain.
The superior and inferior orbital fissures allow the passage of
blood vessels and cranial
nerves which supply orbital structures. On the anterior medial wall
lies a fossa for the lacrimal
sac .The lacrimal gland
lies
anteriorly in the superolateral aspect of the orbit.
THE EYELIDS
The eyelids:
provide mechanical protection to the anterior globe;
secrete the oily part of the tear film;
spread the tear film over the conjunctiva and cornea;
prevent drying of the eyes;
contain the puncta through which the tears drain into the lacrimal
drainage system.
They comprise:
A surface layer of skin.
The orbicularis muscle.
A tough collagenous layer (the tarsal plate).
An epithelial lining, the conjunctiva, reflected onto the globe.
The levator muscle passes forwards to the upper lid and inserts into
the tarsal plate. It is innervated by the third nerve. Damage to the
nerve or changes in old age result in drooping of the eyelid (ptosis).
A flat smooth muscle arising from the deep surface of the levator
inserts into the tarsal plate. It is innervated by the sympathetic
nervous system. If the deep surface of the levator inserts into the
tarsal plate .It is innervated by the sympathetic nervous system
sympathetic supply is damaged (as in Horner’s syndrome) a slight
ptosis results.

The margin of the eyelid is the site of the mucocutaneous
junction .It contains the openings of the meibomian oil glands
which are located in the tarsal plate. These secrete the lipid
component of the tear film. Medially ,on the upper and lower lids,
two small puncta form the initial part of the lacrimal drainage
system
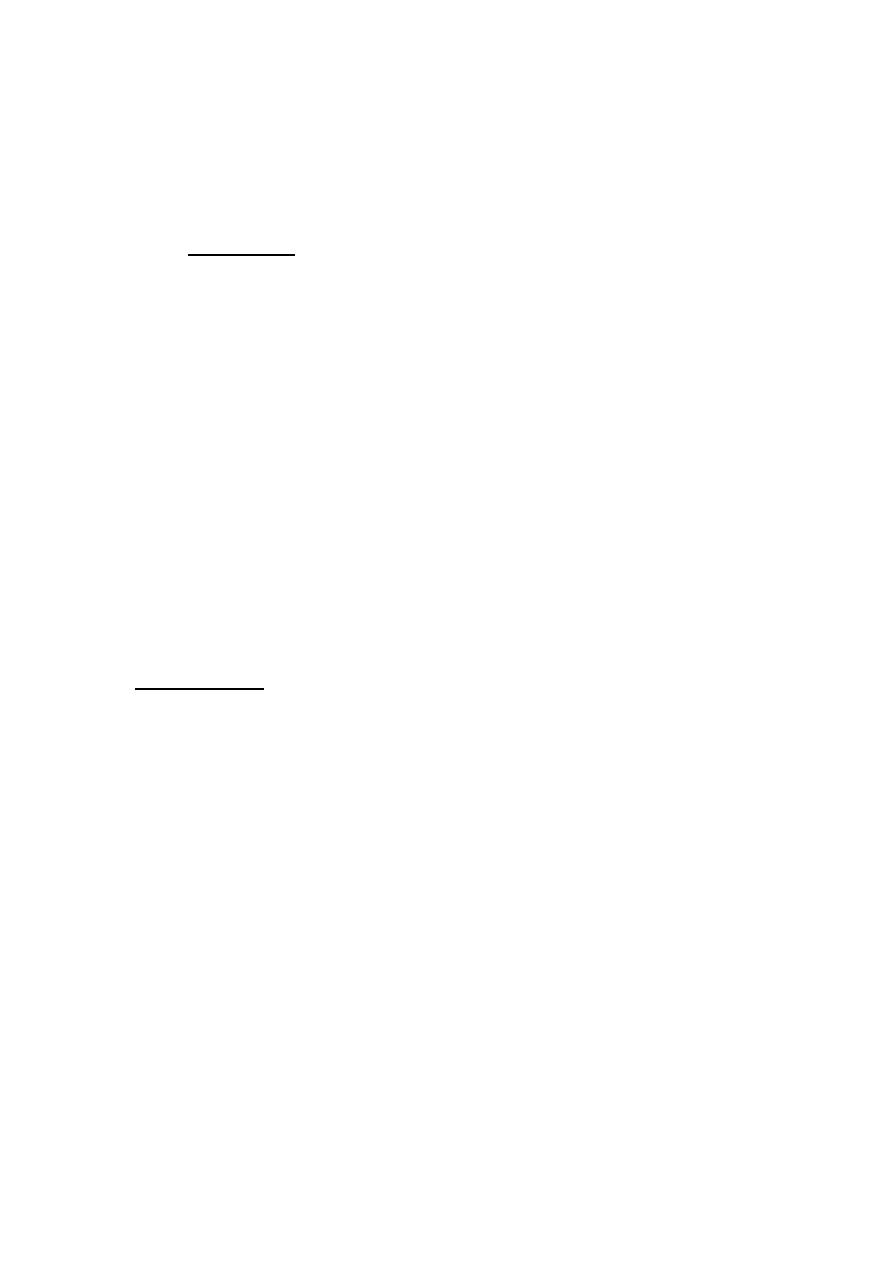
THE LACRIMAL DRAINAGE SYSTEM (Fig. 1.4)
Tears drain into the upper and lower puncta and then into the
lacrimal sac via the upper and lower canaliculi. They form a
common canaliculus before entering the lacrimal sac. The
nasolacrimal duct passes from the sac to the nose. Failure of the
distal part of the nasolacrimal duct to fully canalize at birth is the
usual cause of a watering, sticky eye in a baby. Tear drainage is an
active process. Each blink of the lids helps to pump tears through
the tears
DETAILED FUNCTIONAL ANATOMY
The tear film
The tear film (10 µm thick) covers the external ocular surface and
comprises three layers:
- a thin mucin layer in contact with the ocular surface and produced
mainly by the conjunctival goblet cells;
an aqueous layer produced by the lacrimal gland;
a surface oil layer produced by the tarsal meibomian glands and
delivered to the lid margins.
The functions of the tear film are as follows:
it provides a smooth air/tear interface for distortion free refraction
of light at the cornea;
it provides oxygen anteriorly to the avascular cornea;
it removes debris and foreign particles from the ocular surface
through the flow of tears;
it has antibacterial properties through the action of lysozyme,
lactoferrin and the immunoglobulins, particularly secretory IgA.
.
The cornea (Fig. 1.5)
The cornea is 0.5 mm thick and comprises:
The epithelium, an anterior squamous layer thickened peripherally
at the limbus where it is continuous with the conjunctiva. The
limbus houses its germinative—or stem—cells.
An underlying stroma of collagen fibrils, ground substance and
fibro- blasts. The regular packing and small diameter of the
collagen fibrils accounts for corneal transparency.
The endothelium, a monolayer of non-regenerating cells which
actively pumps ions and water from the stroma to control corneal
hydration and transparency.
The difference between the regenerative capacity of the epithelium
and endothelium is important. Damage to the epithelial layer, by an
abrasion for example, is rapidly repaired. Endothelium, damaged
by disease or surgery, cannot be regenerated. Loss of its barrier and
pumping functions leads to overhydration, distortion of the regular
packing of collagen fibres and corneal clouding.
The functions of the cornea are as follows:
it refracts light and together with the lens, focuses light onto the
retina;
it protects the internal ocular structures.
The sclera
:
is formed from interwoven collagen fibrils of different widths lying
within a ground substance and maintained by fibroblasts;
is of variable thickness, 1 mm around the optic nerve head and 0.3
mm just posterior to the muscle insertions.
The choroid
is formed of arterioles, venules and a dense fenestrated capillary
network;
is loosely attached to the sclera;
has a high blood flow;
nourishes the deep, outer layers of the retina and may have a role in
its temperature homeostasis.
Its basement membrane together with that of the retinal pigment
epithelium (RPE) forms the acellular, Bruch’s membrane, which
acts as a diffusion barrier between the choroid and the retina.
The retinal pigment epithelium
The retinal pigment epithelium (RPE):
is formed from a single layer of cells;
is loosely attached to the retina except at the periphery (ora
serrata) and around the optic disc;
phagocytoses the redundant external segments of the rods and
cones;
facilitates the passage of nutrients and metabolites between the
retina and choroid;
takes part in the regeneration of rhodopsin and cone opsin, the
photoreceptor visual pigments recycling vitamin A;
melanin granules absorb scattered light.
The retina
(Fig. 1.7)
Is a highly complex structure divided into ten separate layers
comprising photoreceptors (rods and cones) and neurones, some of
which (the ganglion cells) give rise to the optic nerve fibres.
Is responsible for converting light into electrical signals. The initial
integration of these signals is also performed by the retina.
Cones are responsible for daylight vision. Subgroups of cones are
responsive to different short, medium and long wavelengths (blue,
green, red). They are concentrated at the fovea which is responsible
for detailed vision
Rods are responsible for night vision. They are sensitive to light
and do not signal wavelength information (colour).
They form the large majority of photoreceptors in the remaining
retina.
The vitreous
The vitreous:
Is a clear gel occupying two-thirds of the globe.
Is 98% water. The remainder consists of hyaluronic acid and a fine
collagen network. There are few cells.
Is firmly attached anteriorly to the peripheral retina, pars plana and
around the optic disc, and less firmly to the macula and retinal
vessels.
Has a nutritive and supportive role.
Detachment of the vitreous from the retina, which commonly occurs
in later life, increases traction on the points of firm attachment. This
may occasionally lead to a peripheral retinal break, when the vitreous
pulls away a piece of the underlying retina.

The ciliary body
This is subdivided into three parts:
1. the ciliary muscle;
2. the ciliary processes (pars plicata);
3. the pars plana.
THE CILIARY MUSCLE
This:

• Comprises smooth muscle arranged in a ring overlying the ciliary
processes.
• Is innervated by the parasympathetic system via the third cranial
nerve.
• Is responsible for changes in lens thickness and curvature during
accommodation .The zonular fibres
supporting the lens are under
tension during distant viewing. Contraction of the muscle relaxes
them and permits the lens to increase its curvature and hence its
refractive power.
THE CILIARY PROCESSES
( PARS PLICATA )
There are about 70 radial ciliary processes
arranged in a ring
around the pos -
terior chamber.They are responsible for the
secretion of aqueous humour.
• Each ciliary process is formed by an epithelium two layers thick
(the outer pigmented
and inner non-pigmented )with a vascular
stroma.
• The stromal capillaries are fenestrated, allowing plasma
constituents ready access.
• The tight junctions
between the non-pigmented epithelial cells
provide a barrier to free diffusion into the posterior chamber. They
are essential for the active secretion of aqueous by the non-
pigmental cells.
THE PARS PLANA
• This comprises a relatively avascular stroma covered by an
epithelial layer two cells thick.
• It is safe to make surgical incisions through the scleral wall here to
gain access to the vitreous cavity.
The iris
The iris:
is attached peripherally to the anterior part of the ciliary body;
forms the pupil at its centre, the aperture of which can be varied by
the
sphincter and dilator muscles to control the amount of light
entering the eye;
has an anterior border layer of fibroblasts and collagen and a
cellular stroma in which the sphincter muscle is embedded at the
pupil margin.
The sphincter muscle is innervated by the parasympathetic system.
The smooth dilator muscle extends from the iris periphery towards
the sphincter. It is innervated by the sympathetic system.
Posteriorly the iris is lined with a pigmented epithelium two layers
thick.
The iridocorneal (drainage) angle
This lies between the iris, cornea and the ciliary body. It is the site
of aqueous drainage from the eye via the trabecular meshwork.
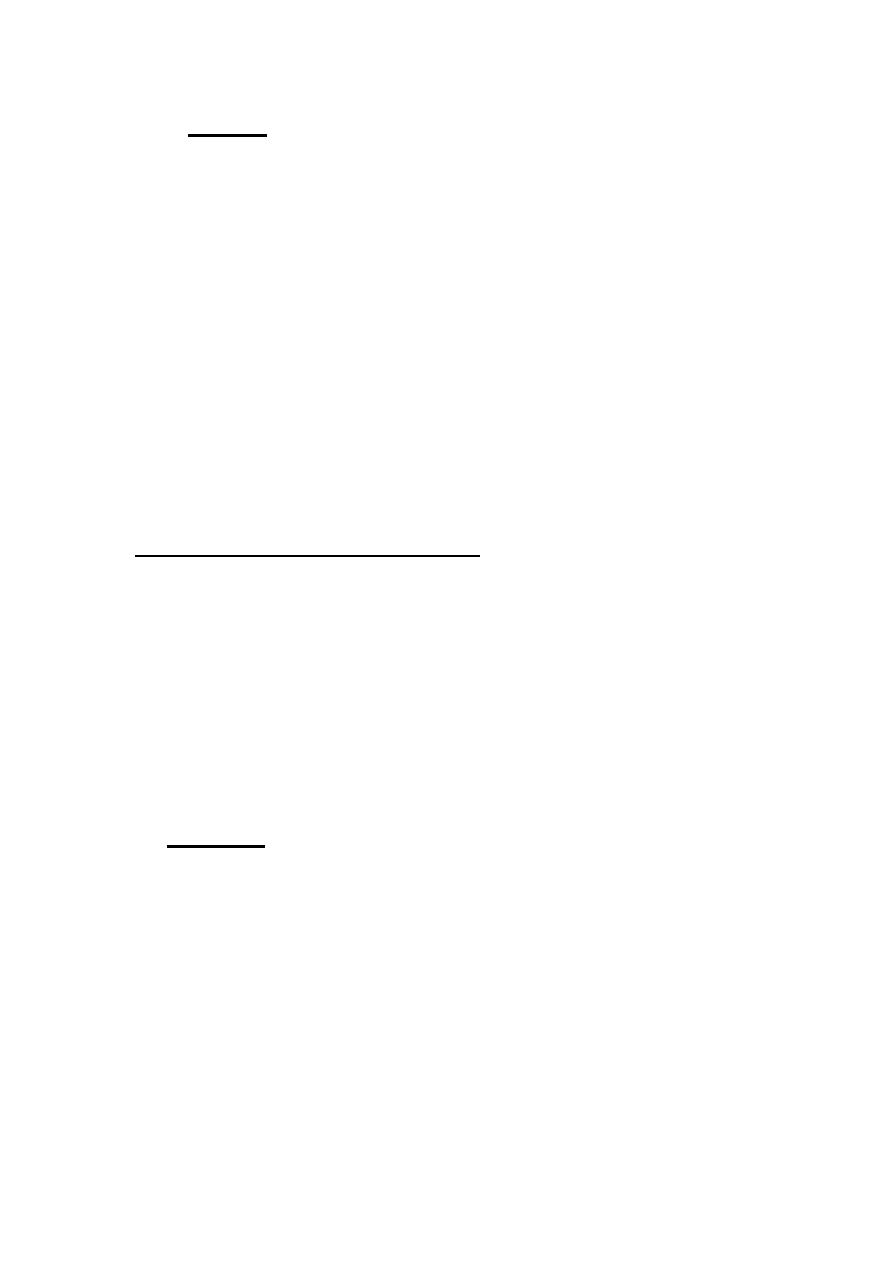
THE TRABECULAR MESHWORK (Fig. 1.9)
This overlies Schlemm’s canal and is composed of collagen beams
covered by trabecular cells.. This meshwork accounts for most of
the resistance to aqueous outflow. Damage here is thought to be the
cause of the raised intraocular pressure in primary open angle
glaucoma.
. The lens
(Fig. 1.10)
The lens:
Is the second major refractive element of the eye; the cornea, with
its tear film, is the first.
Grows throughout life.
Is supported by zonular fibres running between the ciliary body and
the lens capsule.
Comprises an outer collagenous capsule under whose anterior part
lies a monolayer of epithelial cells. Towards the equator the
epithelium gives rise to the lens fibres.
The zonular fibres transmit changes in the ciliary muscle allowing
the lens to change its shape and refractive power.
The lens fibres make up the bulk of the lens. They are elongated
cells arranged in layers which arch over the lens equator.
Anteriorly and pos- teriorly they meet to form the lens sutures.
With age the deeper fibres lose their nuclei and intracellular
organelles.
The oldest fibres are found centrally and form the lens nucleus; the
peripheral fibres make up the lens cortex.
The high refractive index of the lens arises from the high protein
content of the fibres.
The optic nerve
(Fig. 1.11)
This is formed by the axons arising from the retinal ganglion cell
layer, which form the nerve fibre layer, the innermost layer of the
retina.
Passes out of the eye through the cribriform plate of the sclera, a
sieve- like structure.
In the orbit the optic nerve is surrounded by a sheath formed by the
dura, arachnoid and pia mater continuous with that surrounding the
brain. It is bathed in cerebrospial fluid.
The central retinal artery and vein enter the eye in the centre of the
optic nerve.
The extraocular nerve fibres are myelinated; those within the eye
are not.
THE OCULAR BLOOD SUPPLY
(Fig. 1.12)
The eye receives its blood supply from the ophthalmic artery (a
branch of the internal carotid artery) via the retinal artery, ciliary
arteries and mus- cular arteries (see Fig. 1.12). The conjunctival
circulation anastomoses anteriorly with branches from the external
carotid artery.
The anterior optic nerve is supplied by branches from the ciliary
arteries. The retina is supplied by arterioles branching from the
central retinal artery. These arterioles each supply an area of retina
with little overlap. Obstruction results in ischaemia of most of the
area supplied by that arteriole. The fovea is so thin that it requires
no supply from the retinal circulation. It is supplied indirectly, as
are the outer layers of the retina, by diffusion of oxygen and

metabolites across the retinal pigment epithelium from the choroid
The endothelial cells of the retinal capillaries are joined by tight
junc- tions so that the vessels are impermeable to small molecules.
This forms an ‘inner blood–retinal barrier’. The capillaries of the
choroid, however, are fenestrated and leaky. The retinal pigment
epithelial cells are also joined by tight junctions and present an
‘external blood–retinal barrier’ between the leaky choroid and the
retina.
It is the breakdown of these barriers that causes the retinal signs
seen in many vascular diseases.
THE THIRD, FOURTH AND SIXTH CRANIAL NERVES (Fig.
1.13)
THIRD NERVE
The third nerve leaves the midbrain ventrally between the cerebral
peduncles. It then passes between the posterior cerebral and
superior cerebellar arteries and then lateral to the posterior
communicating artery. Aneurysms of this artery may cause a third
nerve palsy. The nerve enters the cav- ernous sinus in its lateral
wall and enters the orbit through the superior orbital fissure.
FOURTH NERVE
The nerve decussates and leaves the dorsal aspect of the midbrain
below the inferior colliculus. It first curves around the midbrain
before passing like the third nerve between the posterior cerebral
and superior cerebel- lar arteries to enter the lateral aspect of the
cavernous sinus inferior to the third nerve. It enters the orbit via the
superior orbital fissure.
SIXTH NERVE
Fibres leave from the inferior border of the pons. It has a long
intracranial course passing upwards along the pons to angle
anteriorly over the petrous bone and into the cavernous sinus where
it lies infero-medial to the fourth nerve in proximity to the internal
carotid artery. It enters the orbit through the superior orbital fissure.
This long course is important because the nerve can be involved in
numerous intracranial pathologies including base of skull fractures,
invasion by nasopharyngeal tumours, and raised intracranial
pressure.
