
1
Surgery
THYROID &PARATHYROID
GLAND
Part1
Prof.DR.NASHWAN
Q.MAHGOOB
4th Stage
MMC&NMC
2015-2016
NAME:________________________________________
College :________________________________________
2
4th stage
جراحة عامة
Lec-1
6/10/2015
Thyroid gland
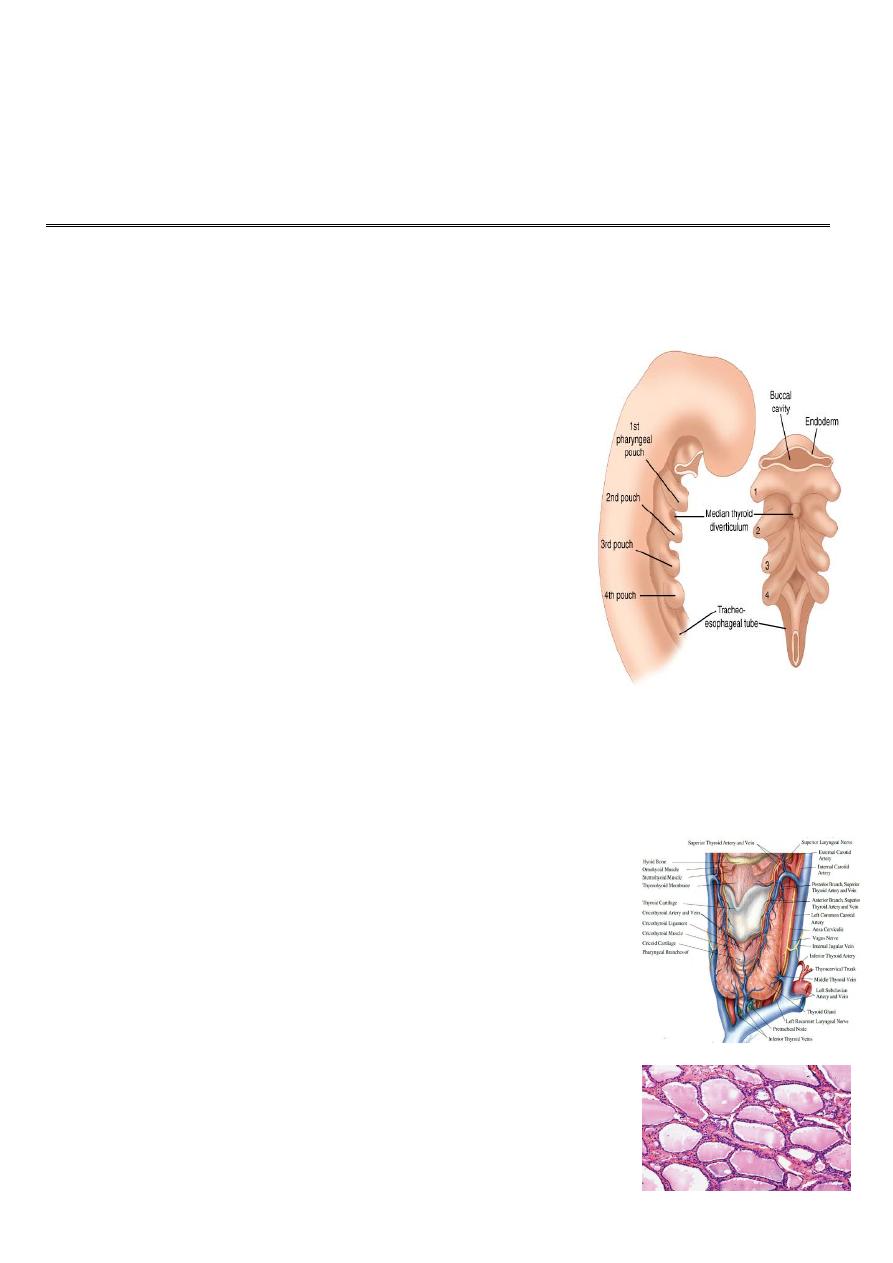
Embryology:
The thyroid gland developed at the fourth week of
gestation.
A diverticulum from the floor of the primitive pharynx,
(thyroglossal duct ) passes from foramen caecum at
junction of anterior 2/3 and posterior 1/3 of the tongue
and descend anterior to neck structures toward the
root of the neck forming two lobes linked by isthmus.
During the fifth week of gestation, the thyroglossal
duct lumen starts to obliterate, and disappears at
eighth week of gestation.
The fourth pharyngeal pouch give rise to Para follicular
cells ( C cell) which amalgamate with the lobes of The
gland
.
Anatomy:
It composed of 2 lobes linked by isthmus, it lies over the
second, third and fourth tracheal rings. WT about 20 to
25 gm, its heavier in female, its just visible in normal
person(not palpable normaly).
A pyramidal lobe is a long, narrow projection of thyroid
tissue extending upward from the isthmus. It represents a
vestige of the embryonic thyroglossal duct. It present in
50% of individuals
.
The functioning unit is the lobule, which composed of
follicles lined by cubical epethelium which synthesize
thyroglobulin that released into the colloid and secreted
3
to the circulation
.
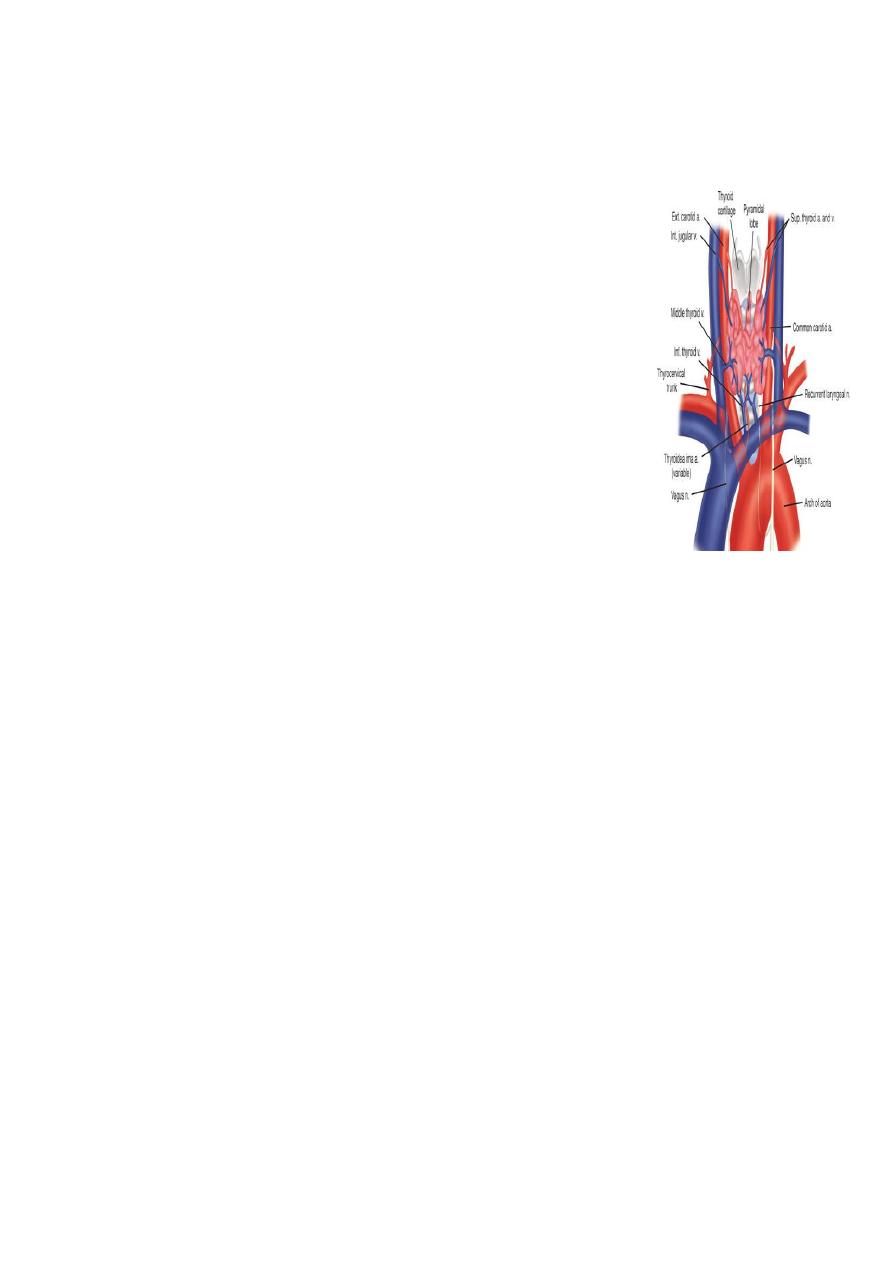
Arterial supply:
1-superior thyroid arteries, which arise from the external carotid
arteries.
2- inferior thyroid arteries, which arises from the thyrocervical
trunk
of the subclavian artery.
venous drainage:
1- Superior thyroid vein at the upper pole.
2- Middle thyroid vein at the middle part of the lobe, enter the
internal jugular vein.
3- inferior thyroid veins from each lower pole are which drain into
the innominate vein
Lymphatic drainage
is to level II, III. IV. VI and VII
Physiology:
Steps of thyroid H formation
1- Trapping of iodide from blood.
2-Oxidation of iodide by the effect of peroxidase Enz.
3-Binding to tyrosene to form monoiodotyrosene.
4-Coupling of monoiodotyrosene to form diodotyrosene.
5- Formation of tri and tetra iodo tyrosene (T3, T4)
6- Storage of H in form of thymoglobulin
7- Release of H in response by effect of dehalogenase Enz
8-Binding of most of the released H to binding protein, small amount remain free in the
circulation

4
The chief stimulator of thyroid hormone synthesis and
secretion is thyroid
stimulating hormone (TSH) from the anterior pituitary.
TSH is under control of Thyroid-releasing hormone (TRH)
from the hypothalamus
Both under negative feed back of T3.
The function of thyroid gland are
1- Secrete thyroid hormones.
2- Secrete calcetonen hormone.
The functions of thyroid H are
1- Facilitate growth and development.
2- Facilitate carbohydrate protein and fat metabolism.
3- Increase oxygen consumption by the tissue, basal metabolic rate, and heat production.
4- Increase oxygen release from HB.
5- Increase oxidative phosphorelation.
6- Augmentation of adrenalin and noradrenalin function.
7- Positive inotropic and chronotropic effects on the heart.
Daily requirement of iodide is 0.1 to 1.5mg .
The free form of T3 and T4 are the active form.
T3 is four times more powerful than T4
T3 less adherent to the binding protein.(98% in comparison with 99.9% for T4)
Half life of T3 is 1 to 3 days (8 to14 days for T4).
All T4 change to T3 at the cellular level.
The normal thyroid gland produces about 80% T4
5
Thyroid function tests:
A-Hormone measurement,
B-Thyroid scanning,
C- Biopsy,
D-Imaging study)
A- Hormone measurement
:
1-Total T3 = 1.2 to 2.8 nmol\L
2-Total T4 = 150 nmol\L
3-TSH test: IV dose of TSH causing elevation of T3 and T4 normally but not in
hypothyroidism.
4-TRH stimulation test: injection of TRH causes secretion of TSH from pituitary gland
normally but not in case of Thyrotoxicosis (suppression) niether in pituitary failure.
These tests become obsolete by now and replaced by measuring of:
1-freeT4=10-30nmol\L
2-freeT3=0.3-3.3nmol\L
3-TSH = 0.5 to 5 mU\L which is the most sensitive and specific test for the diagnosis
of hyper or hypothyroidism and for optimizing T4 therapy.
4-Autoantibody assessment: include TPO (thyroid peroxidase) normally less than
25nmol\l, and anti thyroglobulin anti body.
They do not determine thyroid function, but indicate the underlying disorder, usually
an autoimmune thyroiditis.
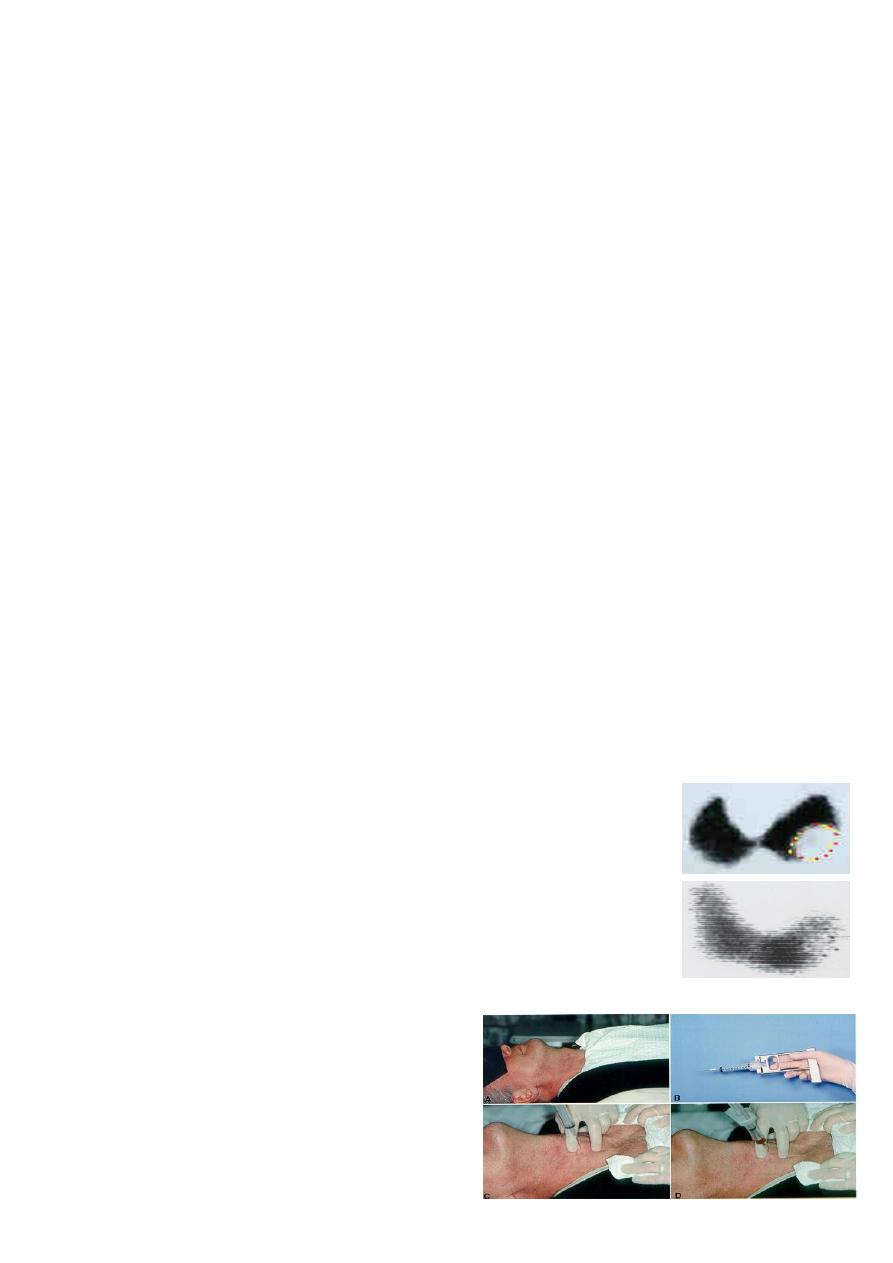
B-Thyroid scanning:
iodine 123 (123I) and iodine 131 (131I) and Technetium Tc
99m
The images Provides size and shape of the gland and
functional activity.
Its principal value is in the toxic patient with a nodule or
nodularity for localization of over activity in the gland
C- Biopsy
1- FNA.
2-Core biopsy
3- Incisional biopsy.
4-Excisional biopsy.
6
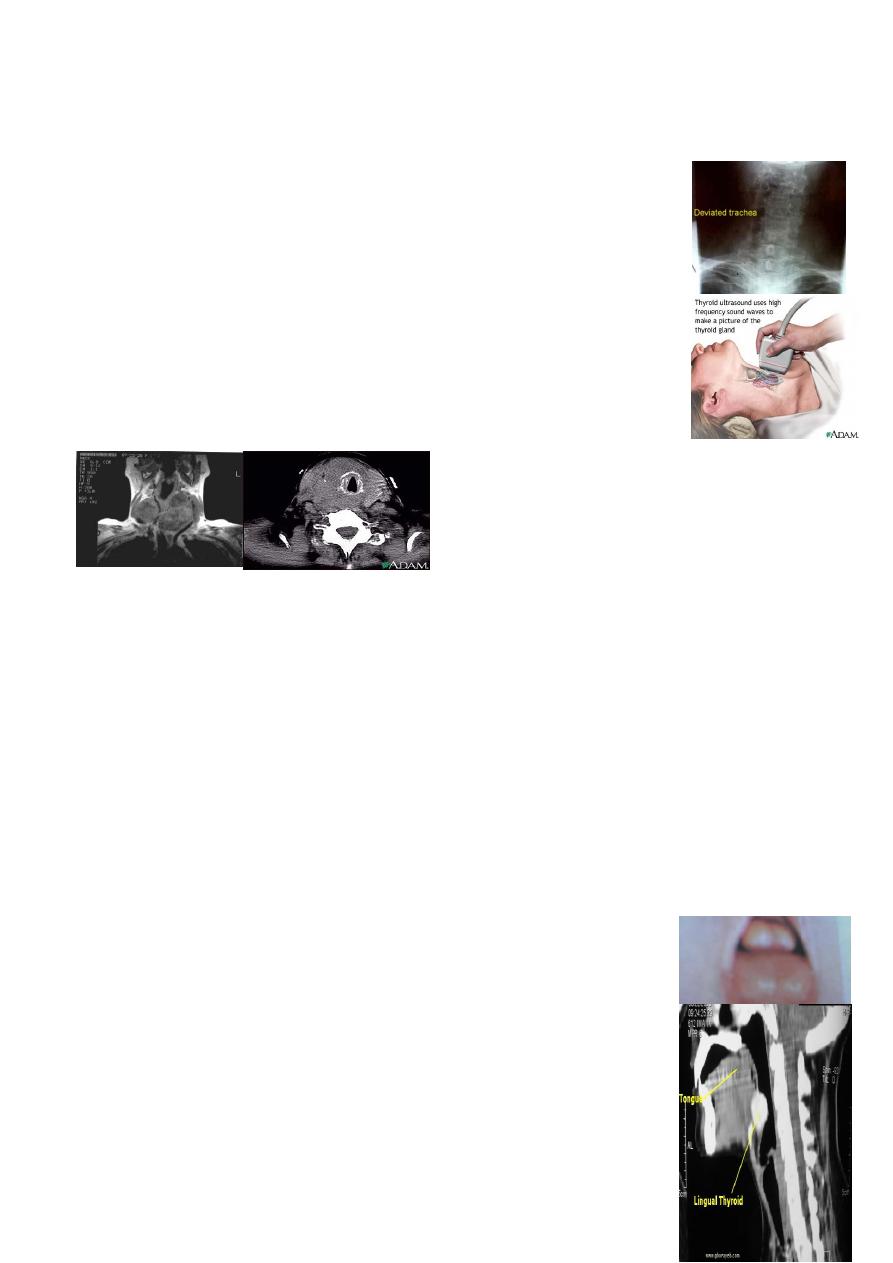
D-Imaging study
:
1-plan X ray of the neck: to evaluate the trachea, retrosternal
extension and cervical spine .
2-Ultrasound: distinguishing solid from cystic masses, information
about size and multicentricity, assess cervical lymph nodes and guides
for FNAC.
3-CT scan and MRI: assessment of known malignancy, extent of
retrosternal and occasionally recurrent Goiters.
Congenital anomalies
:
1-Ectopic location:
2-Thyroglossal cyst
1-Ectopic location:
due to arrest of descend of the thyroglossal duct. It my be Lingual, supra or infrahyoed or
mediastinal.
Lingual thyroid
Thyroid tissue arrested at the posterior third of the tongue. Its more
common in female.It may be the only thyroid tissue.
Clinically: The mass causes dysphagea, dysphonea and
dyspnea,Degeneration or bleeding may result in sudden increase in
size and suffocation.
Diagnosis: by RAIU (radio active isotope uptake)or by CT.
Treatment :
thyroid ablation using I
131
with life long replacement therapy.

7
Surgery (intra-oral excision of the mass) is indicated in very large mass or in case of
suffocation or suspicious of malignant changes.
2-Thyroglossal cyst:
Persistent of part of thyroglossal duct causing cyst, sinus, or fistulae.
40% present < 10 years of age.
75% present as midline swellings.
The most common site is sub-hyoid.
Can occur at the base of the tongue, supra or infra hyoid, or at thyroid cartilage.
Male : female ratio is equal, Often present as an infected cyst due lymphoid tissue in
the cyst wall.
Most fistulae are acquired following rupture or incision of infected cyst
The cyst move upward on protrusion of the tongue as well as on swallowing
.
Complication:
1-Infection, and abscess formation
2-Fistula which is either due to incision of an abscess or inadequate surgical removal
3-Malignant changes
Treatment:
(Sistrunk Operation) excision of the cyst middle 1/3 of hyoid bone up to the base of tongue
.
8
Simple defuse goiter:
Due to excessive TSH secretion in response to low circulating T3 andT4, result in
uniform increase in the size of the thyroid gland. its more common in female owing
to the presence of oestrogen receptors in thyroid tissue.
Causes:
1- Iodine deficiency: due to low intake (endemic goiter).
2- Increase demand to hormone : in pregnancy, lactation and teenage (physiological goiter).
3- Goiterogenic food: Brasseca family like cabbage, kale, rape, and yellow turnips.
4- Drug: antithyroid, PAS, high dose of iodine.
5- Dyshormogeneses: deficiency in Enz responsible for hormone production (sporadic
goiter).
6- Failure of intestinal absorption may produce iodine deficiency.
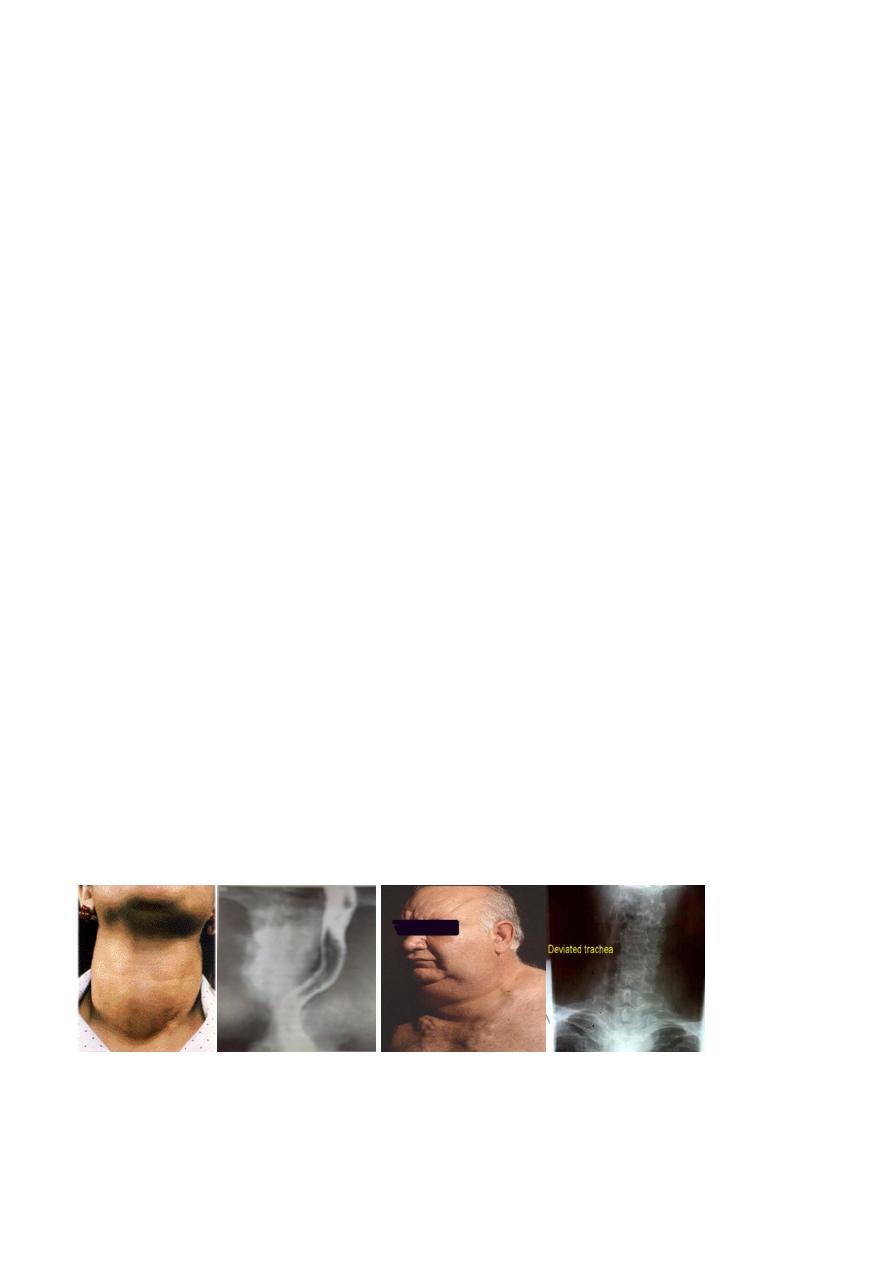
clinical picture:
The gland is soft, smooth, move with swallowing, not tender with universal enlargement,
no picture of toxicity.
There may be pressure manifestation inform of:
1- Dyspnoea due to pressure on the trachea.
2- Dysphagea due to pressure on the esophagus.
3- Dilatation of veins at Supra-sternal area due occlusion of SVC in case of mediastinal
extension.
Investigation :
normal H level and RAU, no antibody .
The condition is preventable by: increase iodine intake and can be treated by thyroxin for
long time.
Surgery indicated in presence of pressure symptoms or for cosmetic reason.
9
Simple multinoduler goiter:
Due to fluctuation in the TSH secretion after prolonged defuse simple goiter, result
in activation of part of the gland and inactivation of other.
The active portions underwent hemorrhage, necrosis or degeneration result in
multiple cystic and solid lesions of various size and shape.
Clinically: The patient is euthyroid with painless cystic and solid (not hard neither fixed)
masses of variable size and shape and may show pressure manefistations.
Investigation: Revealed normal H level and RAU. No antibody. ULS revealed
multinodularity of the gland.
Surgery Is always indicated because:
1- Possibility of changing to toxicity (3o%) after 10 to 20 years.
2-Posibility of malignant changes (5 to 8%) after 10 to 20 years.
3- No response to thyroxin medication.
4- Presence of pressure symptoms.
Solitary thyroid nodule:
The gland show one visible or palpable mass. within a normal gland with
euothyroid state.
Thyroid nodule present in 4 % of individuals.
15 per cent of isolated swellings prove to be malignant, and 30–40 per cent are
follicular adenomas.
The remainder are non-neoplastic, largely consisting of areas of colloid
degeneration, thyroiditis or cysts.

11
The problem, is to differentiate benign from malignant mass, this can be achieved by
:
1-clinical picture (chriteria of malignancy):
1-Age less than 20 or age greater
than 70.
2- Male gender.
3- Rapid increase in size.
4- Resent onset of swallowing difficulties.
5- Resent onset of hoarseness.
6- History of external neck irradiation during
childhood.
7- Hard, irregular and fixed nodule.
8- Presence of cervical lymphadenopathy.
9-Previous history of thyroid cancer.
10-Nodule that is "cold" on scan.
11-Solid or complex on ULS.
12- Positive FNA cytology for malignancy.
2- investigation:
1- RAIS :show cold (80%) warm (10%) or hot (10%) nodule. 15% of cold, 5% of warm and
1% of hot nodule are malignant.
2- ULS: ultrasonic features in a thyroid swelling associated with thyroid neoplasia,
including micro calcification and increased vascularity, but only macroscopic capsular
breach and nodal involvement are diagnostic of malignancy.
3- FNA:It is the investigation of choice but there is a false negative (1%) and false positive
(3%) results and it cannot differentiate between follicular adenoma and follicular
carcinoma.
4- CT and MRI describe the anatomy rather than the pathology.

11
Indications for operation in salotery thyroid swellings.
1- Neoplasia proved by FNAC positive
2- Clinical suspicion
Age
Male sex
Hard texture
Fixity
Recurrent laryngeal
nerve palsy
Lymphadenopathy
Recurrent cyst
Toxic adenoma
Pressure symptoms
Cosmesis
Patient’s wishes
12
4th stage
جراحة عامة
Lec-2
د.نشوان
20/10/2015
Thyroid gland 2
Hypothyroidism:
Failure of thyroid gland to produce adequate level of H. It is either:
1- Congenital: due to ageneses of the gland.
2-Acquired: due to:
A- Thyroid ablation by drug, RAI, surgery
B-Post thyroiditis (hashimotos)
C-Autoimmune (spontaneous)
D- Secondary to pituitary failure.
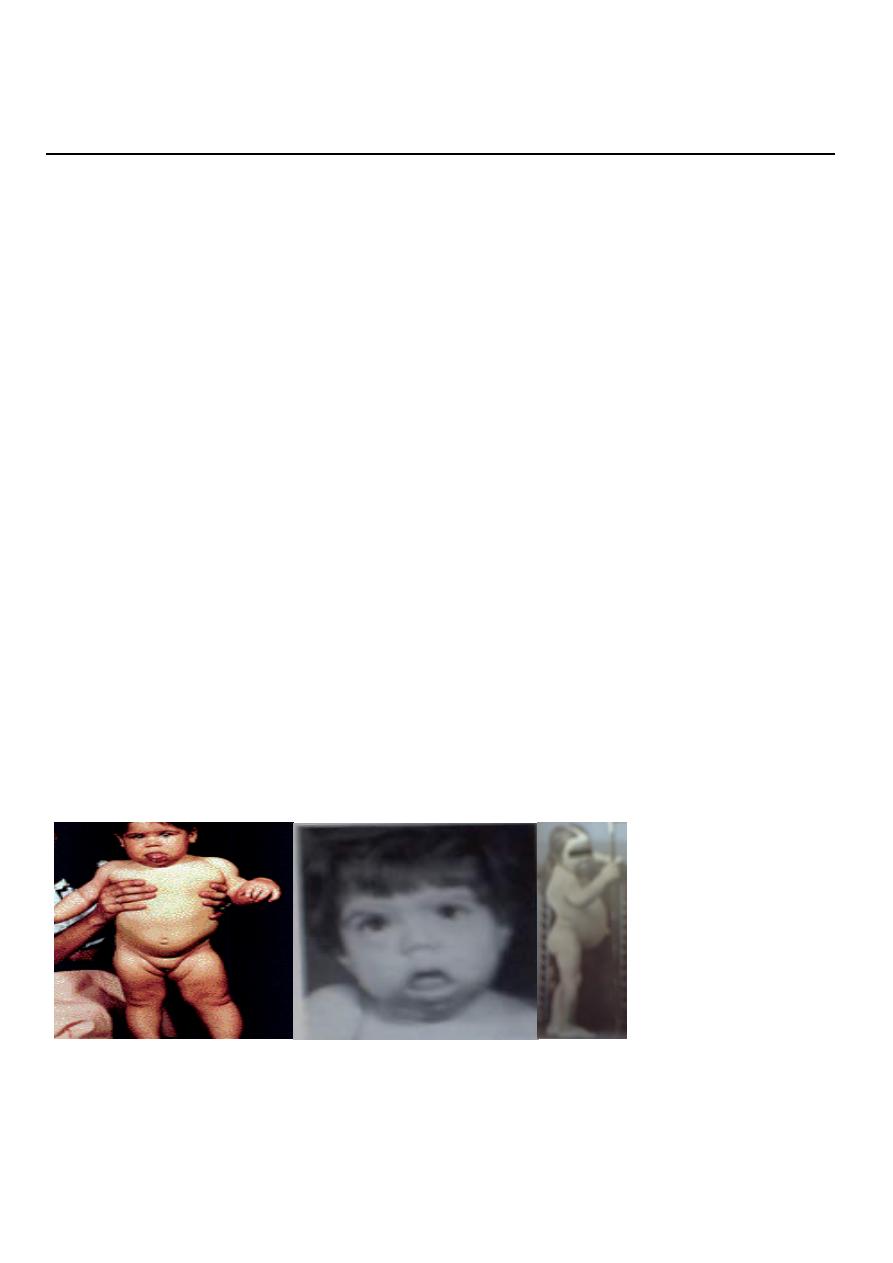
Congenital Hypothyroidism
:
both sex can involved, the patient fail to thrive with mental retardation, poor growth,
large tongue, umbilical hernia, poor feeding and constipation.
Investigation:
high level of TSH, low T3, T4.
Treatment
: Early replacement therapy to prevent permanent and irreversible mental
retardation. The dose should be regulated periodically for long life.
13
Acquired Hypothyroidism (spontaneous type):
Effect female above 50 years, its autoimmune process, it is slowly and progressive disease
with or with out goiter.
Clinical picture:
CVS: bradycardea, cardiomegaly, pericardial effusion, heart failure.
GIT: anorexia, increase WT, and constipation.
CNS: poor performance, somnolence, apathy and dementia.
Dermis: dry thick yellow skin, molar flash, loss of hair, intolerance
to cold.
Genital: decrease libido, impotence, menstrual irregulation,
Investigation:
1- Low T3,T4. high TSH
2- ECG show low voltage,
bradycardea, flat T wave.
3- High serum cholesterol.
Treatment
:Full replacement therapy of thyroxin.

14
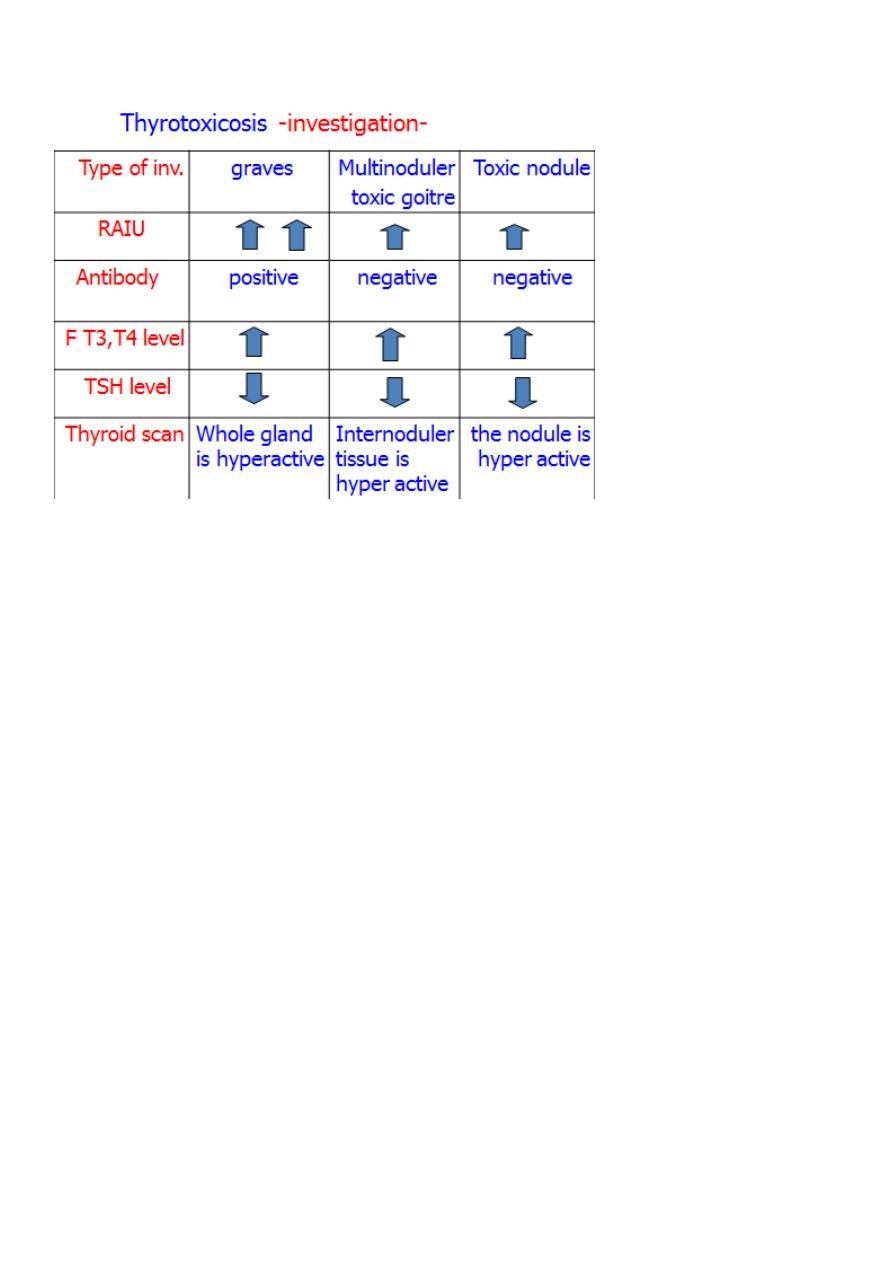
Thyrotoxicosis:
State of hyper functioning thyroid gland due to increase T4 and or
T3 production. Affects 2% of women and 0.2% of men, It is 8 times
more common in female.
The commonest causes are:
1-primary hyperthyroidism (Graves disease)
2-Toxic multinodular goiter (secondary)
4-Toxic solitary nodule (Plummer's disease)
5-Other rare causes:
A-Thyroiditis
B-Post partum
C-Judbassedow syndrome (excessive iodine intake)
D-Thyrotoxicosis factitia (excessive thyroxin intake)
E-Ectopic thyroid H secretion (teratoma (stroma ovari), chorio carcinoma, hydetedform
mole)
F-Thyroid carcinoma.
G- Drug induced like lethium and imudarone.
Types of Thyrotoxicosis:
1-Graves disease (primary thyrotoxicosis)
its autoimmune disease. An antibody to TSH receptor is formed which act like TSH (LATS,
TSI) with long period of action.
It represent 60 to 80% of cases.
May be hereditary, with strong familial predisposition.
The whole gland is hyperactive, its more common in young age female, the condition
appear suddenly, there is sever eye manifestation (50% of patients), pretebial myxodema
and dermopathy.
50% of patients may have other autoimmune conditions such as type I diabetes mellitus,
Addison's disease, pernicious anemia, and myasthenia gravis.

15
2-Toxic multinoduler goitre (secondary thyrotoxicosis)
Due to long standing goiter, the internduler tissue become hyperactive independent
on TSH.
Its more in female above 50 years, the condition is gradual in onset, there is less eye
manifestation but more cardiac problem, its less sever than primary type, not
associated with autoimmune diseases.
3-Toxic nodule :
usually in female 30 to 40 years, a localized mass in the thyroid become hyperactive
independent on TSH, other thyroid tissue is suppressed.
Clinical features of Thyrotoxicosis
1- systemic pictures:
CNS : Tremor, hyperkinetic movements, nervousness ,Irritability, emotional
disturbance, insomnia, behavioral abnormalities, psychoses.
CVS: Palpitation, tachycardia, cardiac arrhythmias, cardiac failure .
Locomotor: Myopathy, wasting, tiredness and lethargy.
GIT: increase appetite with loss of WT and diarrhea.
Dermis: warm moist skin, intolerance to heat, facial flushing, loss of hair, fragile and
soft nails.
Genital: increase libido, but decrease fertility, miscarriage, amenorrhea ,
gynecomastea, impotence .
2-local pictures:
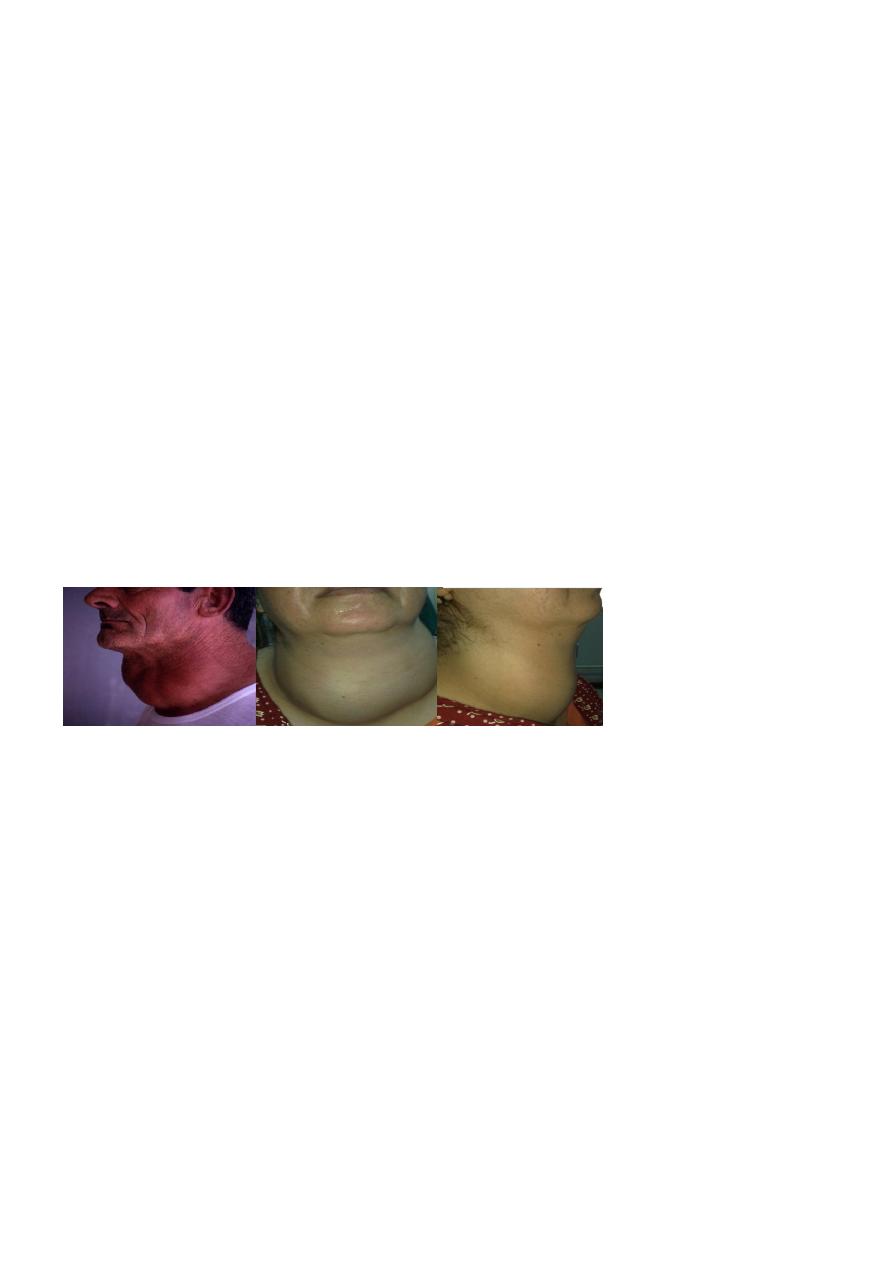
In case of graves disease the gland is universally enlarged ,smooth firm or soft, it may show
bruit and thrill at its upper pole.
In toxic nodule a single mass at thyroid gland is found.
In toxic multinoduler goitre, multiple masses of deferent size and consistency may be
found.
Pressure pictures inform dyspnoea due to pressure on the trachea or dysphagea due to
pressure on the esophagus, or occlusion of SVC in case of mediastinal extension may be
present.
16
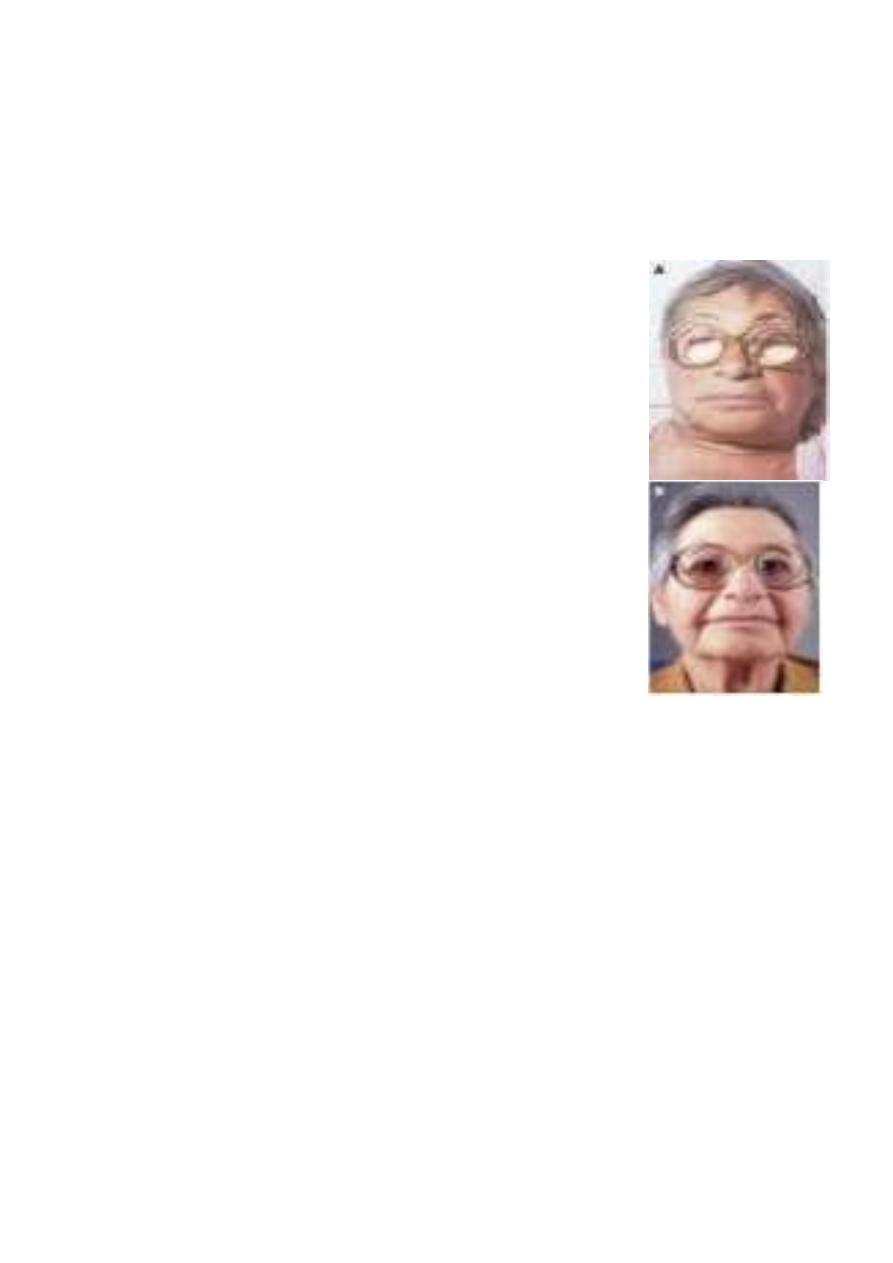
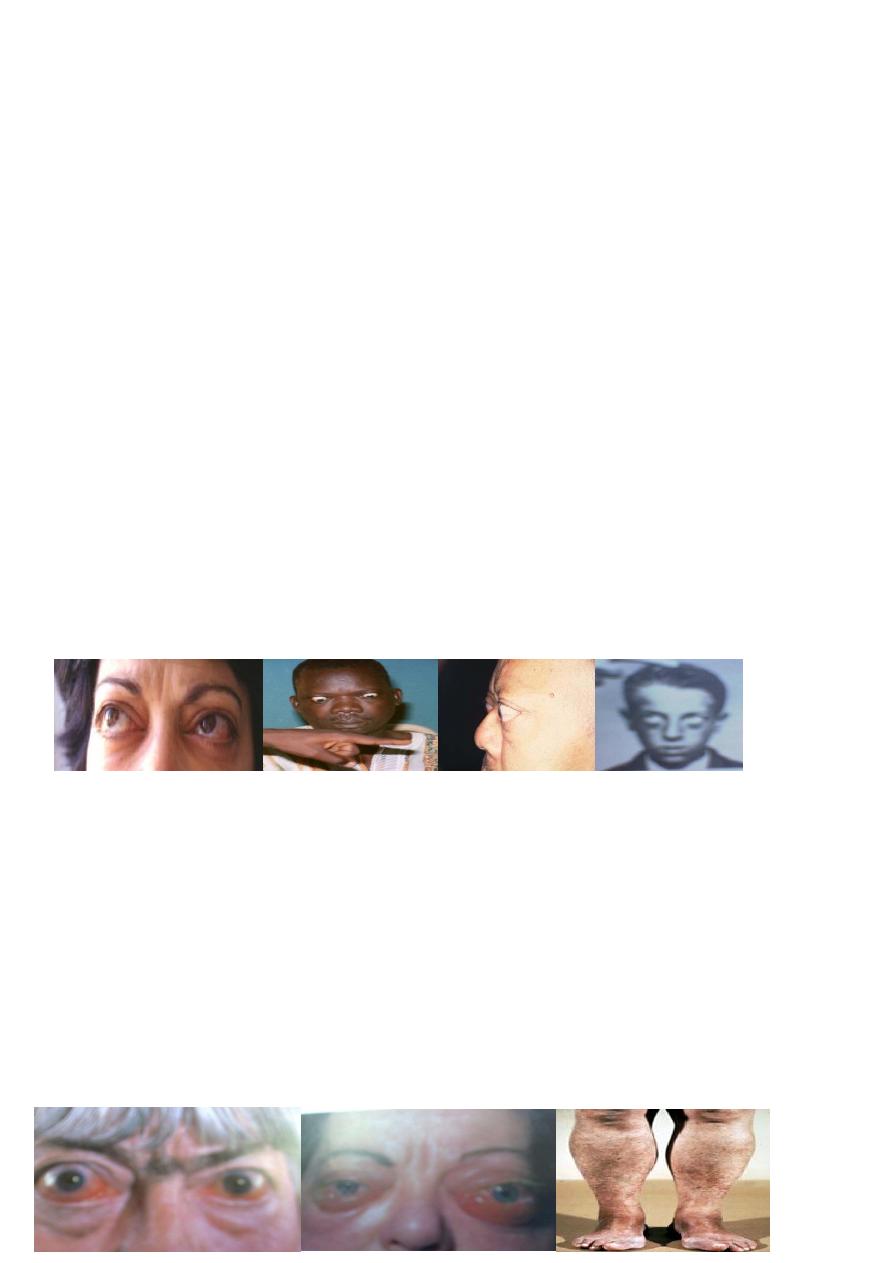
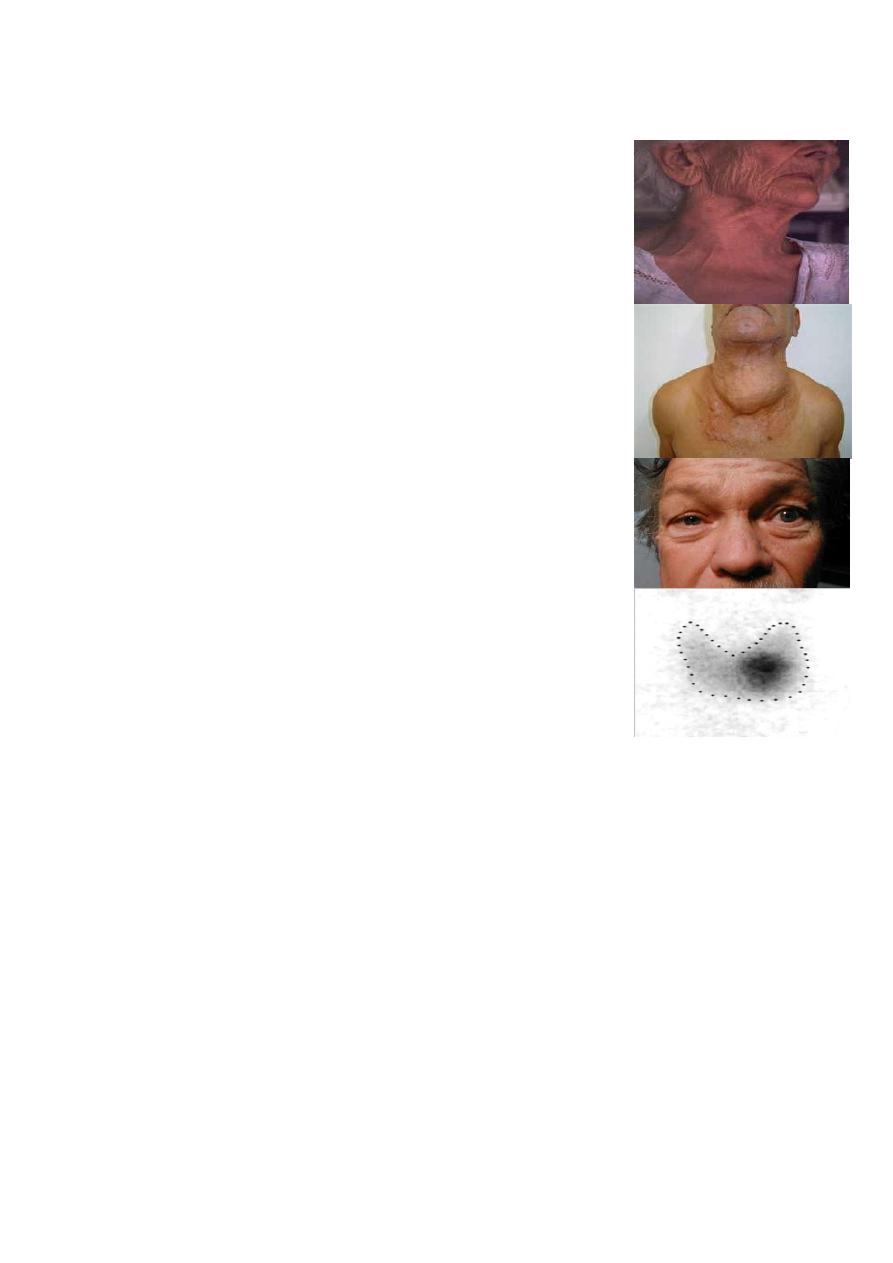
3-Ophthalmic pictures:
1- mild exophthalmoses:
A- bulging of the eye ball due to deposition of fluid in the retrobalber space.
(exophthalmoses)
B- lid retraction: widening of palpabral fissure due to retraction of upper eyelid (stellwag
sign).
C- lid lag: lagging of the upper eyelid in following finger during looking downward
(vonegrefe sign).
Both B and C are due to continuous contraction of levator plapabri superiors
2- Moderate exophthalmoses:
Excessive bulging of the eye ball because of deposition of fat.
Absence of wrinkling at forehead on looking upward (joffroy sign).
3-Severe exophthalmoses:
Increase of intraocular pressure result in double vision.
Difficulty in convergence (mobius sign)
4- progressive exophthalmoses:
appear after surgical treatment of thyrotoxicosis, result in chemosis, corneal ulceration and
intraocular muscle paralyses.
Pretibial myxoedema
Occurs in 1-2% patients with Graves' disease as painless thickening of the skin, nodules .
or plaques due to deposition of glycos-amino-glycans substance
Usually occurs on shins or dorsumof foot Strongly associated with ophthalmopathy, there is
high level of antibody.
Respond to local steroid and disappear after treatment of thyroid toxicity.
17
Treatment of thyrotoxicosis:
(Anti-thyroid drugs,
Radioactive iodine, surgery )
Anti-thyroid drugs:
Inhibit synthesis of thyroxin by interfering with trapping, oxidation and coupling of
iodide.
Most commonly used drugs are: carbimazole ,methmazol and propylthiouracil,
it can be used as:
1- short-term (3-4 months) prior to definitive treatment by radioiodine or surgery.
2-long-term (12-24 months) to induce remission in Grave's disease.
3-Block and replacement therapy: large dose of carbimazol (40mg) with thyroxin (100
micro-gm) for 1-2 years to decrease size of the gland, prevent hypothyroidizm, and
decrease relapse.

18
Advantage :
no surgery or radioactive material
Disadvantages:
1-Treatment is prolonged.
2-Failure rate after 2 years treatment is 50% specially in large goiter with high level of
antibody.
3-Impossible to predict which patients will remain in remission.
4-Of no use in multinoduler or in toxic nodule.
5- Side effect like Agranulocytosis or aplastic anaemia (Patients advice to seek medical
attention if they develop sore throat), hepatitis, peripheral neuritis and polyarteritis,.
6- Goitergenic
7-Crosses the placenta and appear in the milk.
Radioactive iodine
I131 is commonest isotope used, the aim is to destroy the thyroid tissue.
Dose 200–600 MBq, 20% need 2 doses.
Advantage :
no surgery or prolonged drug therapy.
Disadvantages
1-Isotope facilities must be available.
2-80% of patients become hypothyroid after10 years.
3-Indefinite follow up required.
4-Need 3 to 4 months to exert its action.
5- May cause genetic abnormalities.
6-Contraindicated in children, pregnancy, breast feeding and below 25 years and those
with ophthalmopathy.
7- Pregnancy to be avoided 4 months after treatment.
8- Increase overall cardiovascular mortality rates.

19
9- progression of Graves' ophthalmopathy
Indications of RAI:
old patients with small or moderate-sized goiters, those who have relapsed after medical
or surgical therapy, and those in whom antithyroid drugs or surgery are contraindicated.
Surgery;
The aim is to remove the thyroid tissue to decrease hormone production.
Indications of surgery:
1-Relapse after adequate course of anti-thyroid drugs, or its side effect in Grave's disease
or presence of pressure manifestation.
2-In toxic multinoduler and toxic nodule
Advantages:
Goiter is removed, high and rapid cure rate.
Disadvantages:
5% develop recurrent thyrotoxicosis
20 to 80% develop postoperative hypothyroidism
0.5% develop parathyroid insufficiency
Side effect of surgery.
Guide in thyrotoxicosis treatment:
The choice of therapy depends on:
1-Age of the patient
2-Size of the thyroid
3-Type of thyroxicosis
4-The patient intelligence,
personality and wishes.
5-The ability of follow up
6- The availability of medication
7- The cost effectiveness

21
Preoperative preparation:
A-The patient should be euthyroid at time of operation, this can be achieved by:
1- Propranalol 40mg tds to decrease sympathetic over activity, and prevent change of T4 to
T3 at cellular level, its given for 2 weeks preoperatively and continuo for 10 days post
operatively to compete the T4 which has half life of 10 days.
2- Carbimazol 10 to 40mg till the patient become euthyroid (4 to 6 weeks) then 5 to 10mg
till the day of operation.
3-Logul iodine drops- 3 drops 3 times a day for 10 days to render thyroid less vascular and
firm.
B-Investigation
1- Indirect laryngoscopy to asses the vocal cord since 3% of patients may have symptom
less cord paralyses.
2- Thyroid antibody in case of graves disease.
3- TSH level , which should be normal.
3- Serum calcium.
4- Cervical x ray to asses thyroid extension and cervical spine for any OA changes.
5- ECG, Hb, serum urea, FBS, blood group.

21
4th stage
جراحة عامة
Lec-3
د.نشوان
20/10/2015
Thyroid gland 3
Post operative complications:
1- Hemorrhage
:
A reactionary bleeding may occur in the first 24 hours. Its due to slipping ligature or
from remnant ofthyroid tissue. The patient suffer from suffocation, dyspnea and
restlessness,with or with out neck mass.
Treatment is by rapid and adequate evacuation of the hematoma and controlling the
bleeding.
2- Respiratory obstruction
: due to laryngeal edema caused by excessive manipulation,
intubation injury or tracheomalecia. The patient suffer from suffocation after removal of
the endotracheal tube. Treatment by reinsertion the tube with steroid, rarely tracheostomy
3-Recurrent laryngeal nerve injury:
its technical fault, its either transient or permanent, unilateral or bilateral.Transient
unilateral type due to traction or compression on the nerve, recovery is suspected in 3
months. Permanent unilateral injury is due to division of the nerve which causes horsiness
of the voice.
Bilateral injury causes sever dyspnea and suffocation that necessitate immediate
tracheostomy.
4- External branch of superior laryngeal nerve injury
:
leads to inability to tense the ipsilateral vocal cord and hence difficulty in "hitting high
notes," projecting the voice, and voice fatigue during prolonged speech.
5- parathyroid insufficiency:
Its either temporarily due to ischemiaof or permanent due to infarction or inadvertent
removal.
Early manifestation (temporary) is tetany which is presented as cercum oral numbness,
carpopedial spasm and strider due to spasm of laryngeal muscle (laryngesmus striduolus)
Treatment: IV infusion of 10% calcium gluconate which can be repeated each 8 hours
Late type (permanent) presented as repeated carpopedial spasm, trousseas and schvostic
signs. Needs long term vit D and calcium.

22
:Treatment
IVF, cooling the patient with ice packs, oxygen, diuretics for cardiac failure, digoxin for atrial
fibrillation, sedation and IV hydrocortisone. Specific treatment is by carbimazole 10–20 mg
6-hourly, Lugol’s iodine 10 drops 8-hourly by mouth or sodium iodide 1 g i.v. Propranolol
intravenously (1–2 mg) or orally 40 mg 6-hourly) to block -adrenergic effects.
7- wound complication:
like infection or keloid formation or granuloma formation.
Post operative follow up:
1- fibro-optic laryngoscope before leaving the hospital.
2-Serum calcium after 6 weeks.
3- Six months follow up to determine thyroid function for 1 year then yearly for long time.
Thyroiditis:
Its inflammation of thyroid tissue, its either acute sub-acute or chronic form
:Acute form could be
Supurative more common in children followed URTI. Streptococcus and anaerobes account
for 70% of infection.
MO reach the gland via: a-hematogenous or lymphatic route, direct spread , penetrating
trauma .
clinically: sudden painful enlargement of the gland with fever, chills, dysphonia and
odynophagia.
Treatment: Paranteral antibiotic, drainage if abscess is formed.
Non supurative infection may result from bacterial or viral infection.
subacute thyroiditis: dequrvain disease

23
Chronic form: hashimotos, or riedels thyroiditis
Sub-acute thyroiditis - dequarvain disease
:
Self-limited disease may be due to viral infection.
Its more common in female around 40 years.
Pathology: There is infiltration of the gland by monocyte, lymphocyte and epetheloid cells.
Clinical picture: The condition may pass into 4 stages:
1- Acute toxic stage characterized by sudden painful goiter with hyperthyroidism for 2 to3
months.
2-Euthyroid stage there is only goiter
3-Hypothyroid stage remain for 2 to 4 months.
4-Recovary stage within 1 to 6 months.
Investigation: High ESR, absent thyroid antibodies,
RAI-131- uptake is low, H level depending on the stage of the disease, FNA is diagnostic.
Treatment : NSAI, prednesolone 40 mg for 1 month tapered in 2 months. replacement
therapy in hypothyroid stage.
Chronic thyroiditis –hashimotos:
Its autoimmune disease with inherited predisposition, an antibody formed against thyroid
gland, like antimicrosomal (antiperoxidase) and antithyroglobulin antibody.
Pathology: excessive lymphoid tissue infiltration with degeneration of the follicles.
Clinical picture: female at 50 years, may associated with other autoimmune disease like
DM,SLE,RA.
There is painless and firm goiter which is defuse or nodular with pressure symptoms, later
there is picture of hypothyroidism. Thyroid lymphoma is a rare but well-recognized,
ominous complication.
Investigation: low T3,T4,elevated TSH. low RAIU. High AB titer. FNA is diagnostic.
Treatment: Replacement therapy by thyroxin. Surgery indicated in large goiter, or
suspicion of malignancy.
24
Chronic thyroiditis – Riedels disease:
Extensive infiltration of thyroid gland by fibrous tissue extend to trachea and surrounding
structures, may associated with other focal sclerosing syndromes like mediastinal and
retroperitoneal fibrosis or sclerosing cholangitis.
Clinically: painless, hard mass, which progresses over weeks to years to produce pressure
symptoms and hoarseness. Patients may present with hypothyroidism and
hypoparathyroidism due to replacement of the glands by fibrous tissue.
Physical examination hard, "woody" thyroid gland with fixation to surrounding tissues.
Investigation: low H level, low RAIU, AB may be positive, FNA is diagnostic but open
biopsy may needed.
Treatment: replacement therapy.
Surgery indicated in pressure symptoms (esthmusectomy) to release the trachea or if
malignancy cannot ruled out. reported experience show dramatic improvement with
corticosteroids and tamoxifen.
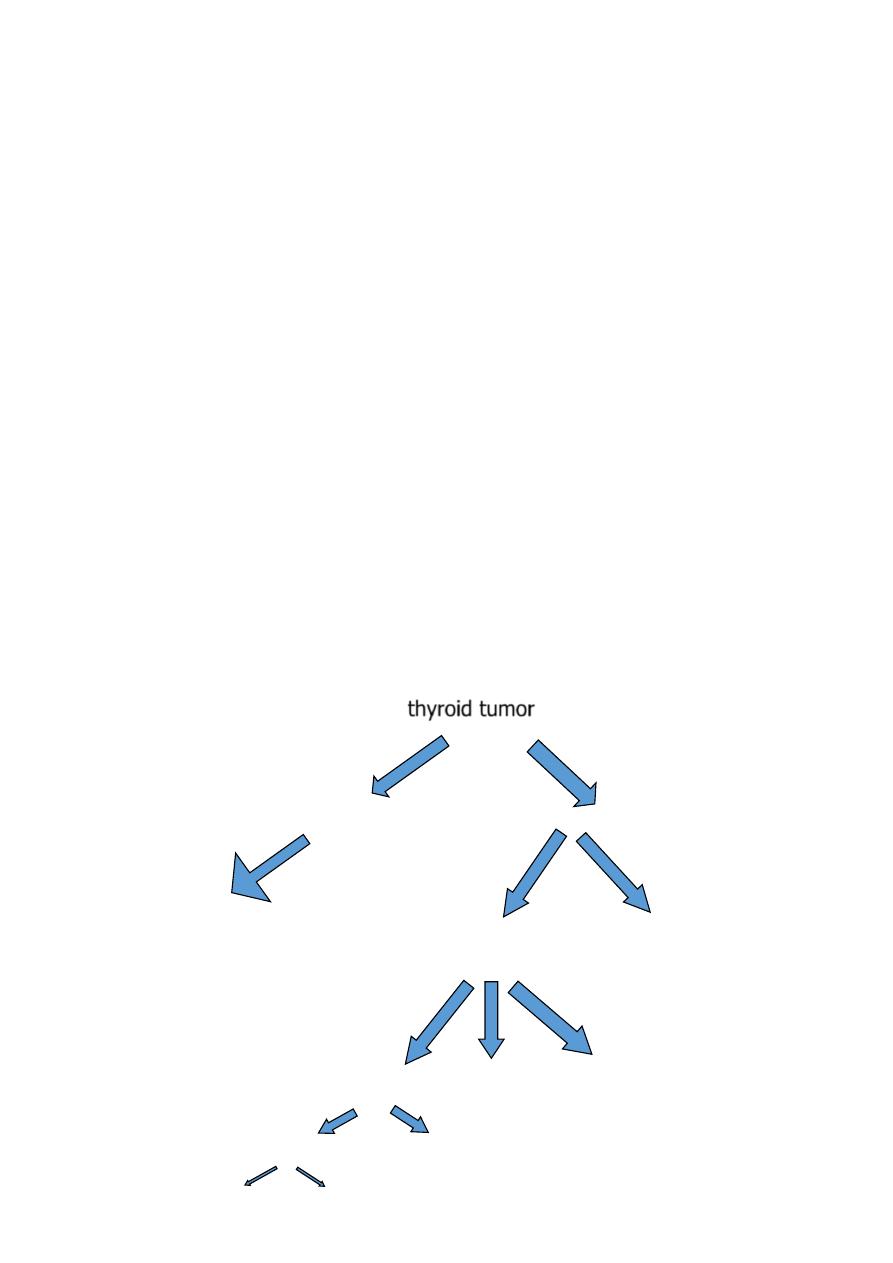
thyroid tumor
Papillary ca
Follicular adenoma
Primary
secondary
Carcinoma lymphoma modularly
Differentiated undifferentiated
Benign
malignant
25
Thyroid carcinoma:
Type of ca
Papillary ca
Follicular ca
Anaplastic ca
Age
30-40
40-50
60-80
Sex ratio (f:m)
3:1
3:1
1:1.3
Percentage
60%
20%
10%
Spread
lymphatic
blood
both
Predisposing F
neck radiation
long standing goiter
Not known
Multi focal lesion
positive
negative
negative
H dependency
TSH
TSH
non
Prognoses
good
fair
poor
26
Clinical picture:
Thyroid cancer accounts for <1% of all malignancies (2% of
women and 0.5% of men) its usually presented as:
1- Painless rapid growing mass (painful mass radiate to ear in case
of local invasion).
2-Horsiness of the voice.
3-Hard and irregular on palpation.
4-may not move with swallowing.
5-Carotid pulsation may be absent (Berry sign)
6-Horner syndrome due to local invasion of sympathetic nerve.
7-There may be hard lymph node in neck.
8-pressure manifestation may exist.
Investigation:
1- Normal thyroid H
2- Cold mass by RAIU
3- Positive AB
4- FNA is diagnostic in most condition except for follicular type
Prognostic factors in Deferential thyroid cancer:
age, sex, size, capsular invasion and histopathology of the tumor play in important rule in prognosis.
1- Low risk group represent 80% of the condition with 98% 25 year survival rate. It include
A- Male less than 40, or female less than 50 years without distal metastasis.
B- Older age with intra thyroid papillary Ca, or follicular Ca less than 5 Cm without capsular invasion, no
distal metastasis.
2- High risk group represent 20% of the condition with 46% 25 year survival rate. It include
A- All patients with distal metastasis.
B- Extra thyroid papillary Ca.
C- Follicular Ca more than 5 Cm or with capsular invasion
Lymphatic involvement not associated with bad prognosis.

27
Surgical management of differentiated thyroid CA
The surgical strategy of patients with low-risk cancers remains controversial.
A- Total thyroidectomy
B- Lobectomy
1-The benefit of total thyroidectomy are
1- Enables the use of RAI to detect and treat residual thyroid tumor or metastatic
disease.
2- Makes serum Thymoglobulin level a more sensitive marker for recurrent or
persistent disease.
3- Eliminates contra lateral occult cancers as sites of recurrence.
4- 33 to 50% of patients who develop a recurrence die from their disease
5- Reduces the need for re-operative surgery with its attendant risk of increased
complication rates
.
2-The benefit of lobectomy are:
1-Total thyroidectomy is associated with a higher complication rate like hypothyroidism,
RLN injury and hypoparathyroidism (10-30%)
2-Recurrence in the remaining thyroid tissue is unusual (5%) and most are curable by
surgery.
3-Tumor multicentricity seems to have little prognostic significance, and its rare in
contra lateral lobe.
4-Patients who have undergone lobectomy still have an excellent prognosis.
5-In case of recurrence, or suspicious secondaries, the remaining thyroid can be ablated
by high dose of RAI
High-risk group or bilateral tumor should undergo total thyroidectomy.
Presence of LN necessitate modified radical neck dissection.
28
Follow up:
1- It is standard practice to prescribe thyroxine in a dose of 0.1–0.2 mg daily, to suppress
endogenous TSH production, for all patients after operation for differentiated thyroid
carcinoma on the basis that most tumors are TSH dependent.
2- The measurement of serum thyroglobulin is invaluable in the follow up and detection
of metastatic disease in patients who have undergone surgery for differentiated
thyroid cancer.
Indications for post operative RAI study
:
1- All patients with high risk group.
2- Incomplete removal of tumor
3- Recurrence of tumor
4- Suspicion of secondaries.
5- High level of thymoglobulin post operatively.
External Beam Radiotherapy
EBR indicated in:
1- Unrespectable tumor.
2- Locally invasive or recurrent disease .
3- Bone metastases to decrease the risk of fractures.
4-Controlling pain from bony metastases.
Chemotherapy has been used with little success in disseminated thyroid cancer, and there
is no role for chemotherapy.
Thyroid lymphoma:
Accounts for 1% of thyroid malignancies.
Often arises with Hashimoto's thyroiditis or non-Hodgkin's B-cell lymphoma
presents as a painless and rapid enlarging goiter with pressure effects.
Diagnosis made by FNAC
Chemo and Radiotherapy is treatment of choice
Prognosis is good - often more than 50% 5 year survival
29
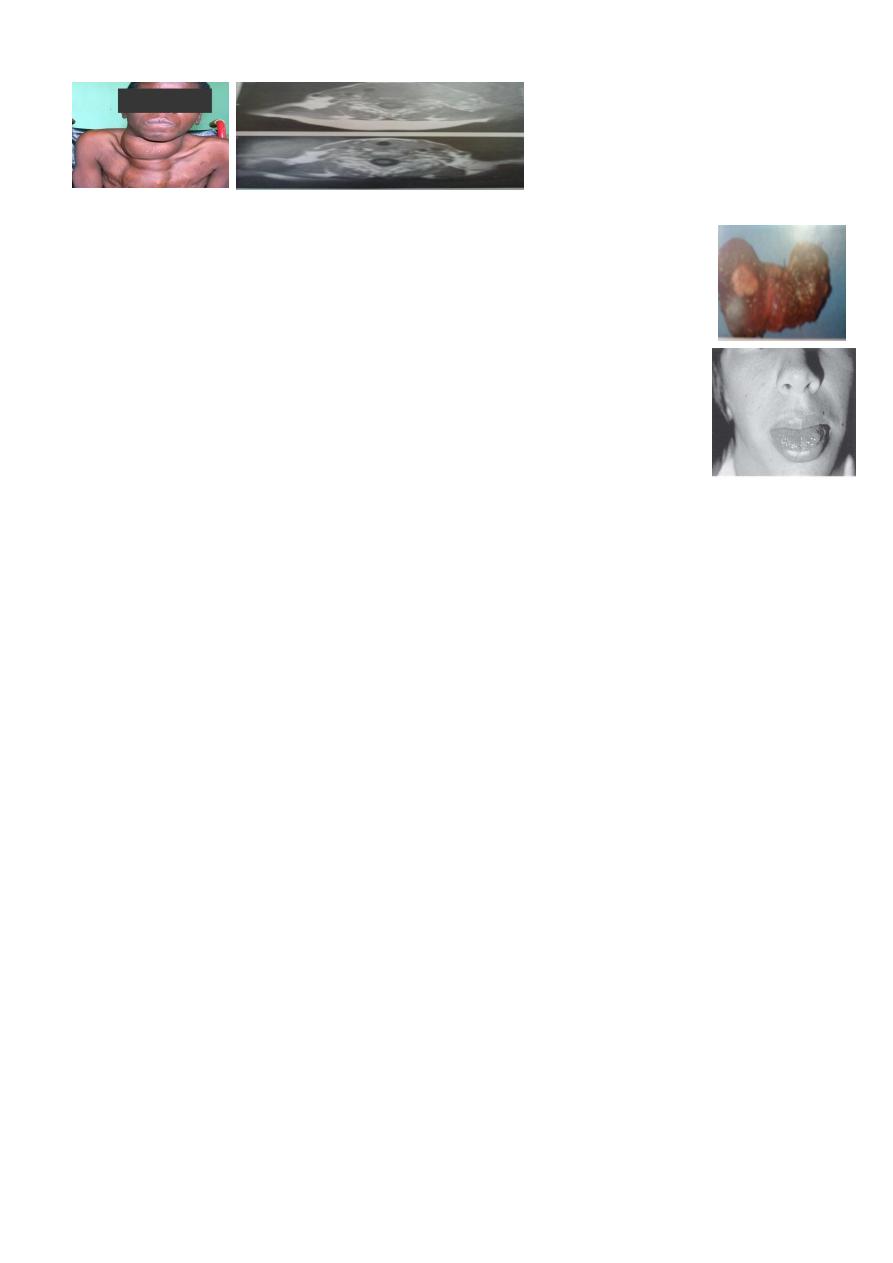
Medullary Carcenoma :
Arise from parafolliculer cells.
There is high level of calcitonen and 5HT, which may cause diarrhea.
Represent 5% of thyroid tumor.
It may be sporadic ( 80% )or familial which is occur in children and young
age, its more invasive, multifocal and may associated with(MEN-2- A) as
parathyroid hyperplasia medullary carcinoma, Phiochromcytoma , or with
(MEN-2-B) as parathyroid hyperplasia or tumor, Phiochromcytoma with
skin pigmentation, multiple neuromas in the tongue and mucous
membrane and marfanoid habits.
It metastasize by lymph and blood.
Prognoses is good without metastases.
FNA is diagnostic.
Surgery is the treatment of choice.
Family screen in case of familial type.
Anaplastic Carcinoma:
Accounts for approximately 1% of all thyroid malignancies.
Male and female equally affected Most age involved at seventh and eighth decade of life.
Clinically: Rapidly enlarging mass and may be painful.
The tumor is large and may be fixed to surrounding structures or may be ulcerated.
Associated symptoms: dysphonia, dysphagia, and dyspnea
Lymph nodes usually are palpable at presentation.
Evidence of metastatic spread also may be present.
Diagnosis is confirmed by FNAB
Treatment :
The tumor is the most aggressive thyroid malignancies, with few patients surviving 6
months beyond diagnosis.
All forms of treatment have been disappointing.
31
In respectable mass, thyroidectomy may lead to a small
improvement in survival, especially in younger individuals. Combined radiation and
chemotherapy may be used as palliative management..
4th stage
جراحة عامة
Lec-4
د.نشوان
20/10/2015
PARATHYROID GLAND
Anatomy:
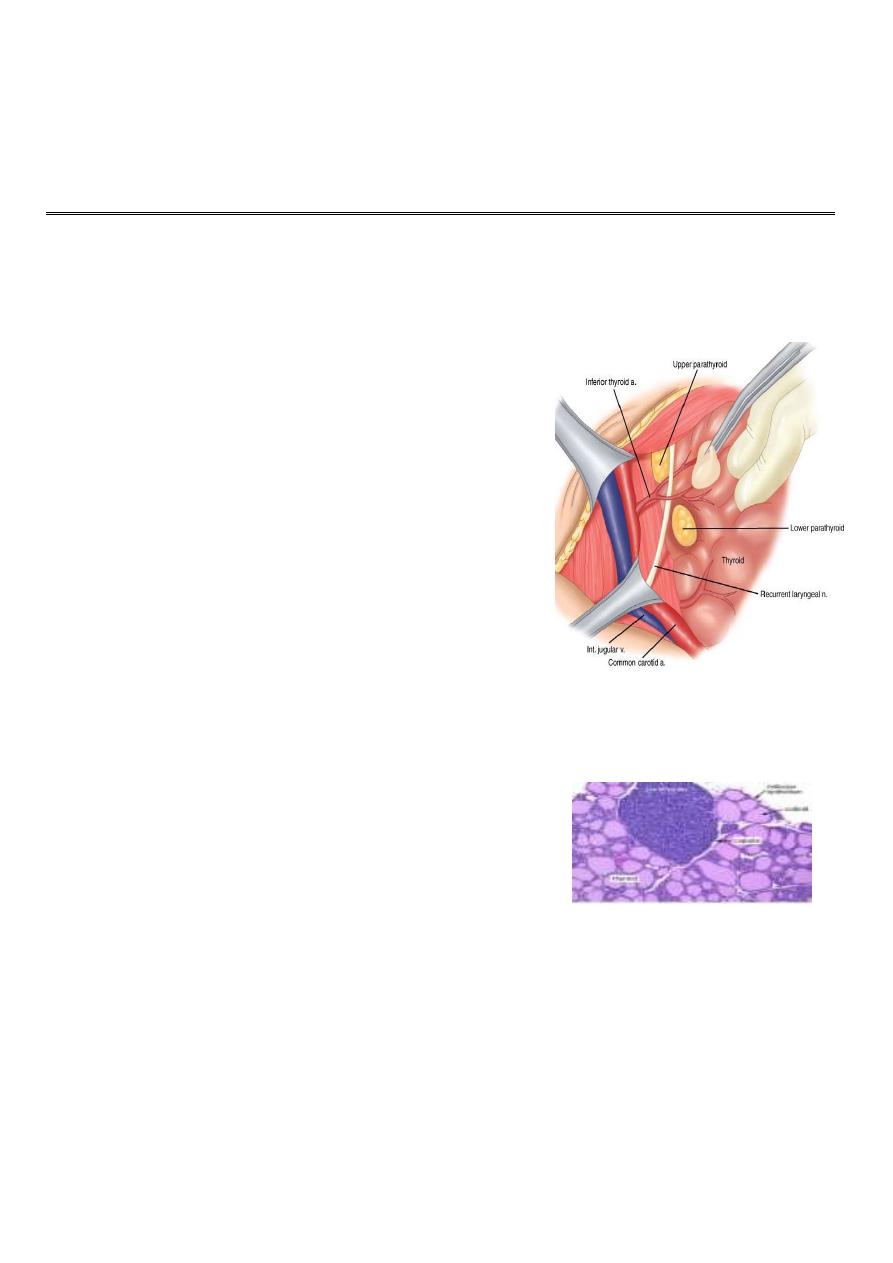
Parathyroid glands are usually 4 in number in 85%,
more than4 in 10% and less than 4 in 5%.
1About 0.6-1 cm in size, 30-50 gramthey are yellowish
brown in color
.
The upper pair derived from IV pharyngeal pouches,
they lies just above the inferior thyroid A, posterior to
RLN, posterior to thyroid gland.
The lower pair from III pharyngeal pouches, and they
are less constant in position, usually at lower pole of
thyroid, inferior to inferior thyroid A, anterior to RLN
Arterial supply: by branches from inferior thyroid A,
venous drainage towered thyroid veins.
The glandular structures are:
1-Chief cells that produce PARATH H
2-Oxyphil cells.
PTH is released in response to a low serum calcium or high serum magnesium level.
Calcium is most abundant extracellular cation.
The total serum calcium levels range from (2.1 to 2.6 mmol/L)
50% of serum calcium is in ionized form, which is the active component. The remainder is
bound to albumin.
Function of Calcium : excitation-contraction of muscle tissues, synaptic transmission in the
nervous system, coagulation.

31
Physiology:
Function of parath H
1- Stimulate ostiolytic activity (mobilization of
Ca from bone)
2- Stimulate reabsorbtion of Ca from renal
tubule, decrease urine excretion of Ca.
3- Augment Ca absorption from GIT.
4- Increase execration of Ph from renal tubule.
Hypoparathyroidism:
Etiology:
Congenital
1- Digeorge syndrome (absence parath gland and thymus with cardiac defect).
2- Autoimmune polyglanduler syndrome.
Acquired
1- Idiopathic: mostly due to autoimmune disease.
2- Inadvertent removal of parathyroid gland during thyroid or parathyroid operation(MOST
COMMON).
3- Wilson disease (hemochromatosis) familial disease characterized by deposition of cupper
in liver and CNS
Clinical picture:
Transient
hypoparathyroidism occur in the second post thyroidectomy day, started as
circumoral numbness, carpopedal spasm, convulsion like movement, laryngesmus stridulus.
Permanent
hypoparathyroidism result in repeated carpopedal spasm, anxiety, fatigue,
muscle pain mental changes and cataract formation
.
32
Classical signs are trousseas and Chvostek’s signs
.
Investigation:
1- ECG: prolonged QT interval.
2- serum Ca is low.
3- serum Ph increase.
Treatment for acute or transient attack:
IV calcium gluconate 10%(10 Ml ) in 200 cc glucose water infusion which can be repeated
each 8h.
Treatment of permanent type:
by oral intake of active Vit D3 (1 to 4 ugm), the dose regulated by frequent Ca level
checkup
.
Hyperparathyroidism:
Primary hyperparathyroidism:
Elevated PTH. increased serum Ca Due to:
A- sporadic hyperparathyroidism (80%): cause either:
Parathyroid adenoma (85%)
Parathyroid hyperplasia (14%)
Parathyroid carcinoma (<1%)
B-familial: mostly in form of
hyperplasia, usually associated with other endocrine disease:
1-MEN1(neuro-endocrine tumors inform of pancreatic and pituitary adenoma and
adrenocortical tumors).
2-MEN2A (parathyroid hyperplasia, medullary thyroid ca, Phiochromcytoma)
Secondary hyperparathyroidism
Elevated PTH. Low serum Ca Due to chronic renal failure, malabsorption, rickets.
Tertiary hyperparathyroidism
33
Elevated PTH following correction of cause of secondary hyperparathyroidism (renal
transplantation)
Clinical picture:
(kidney stones, painful bones, abdominal groans, psychic moans, and fatigue overtones
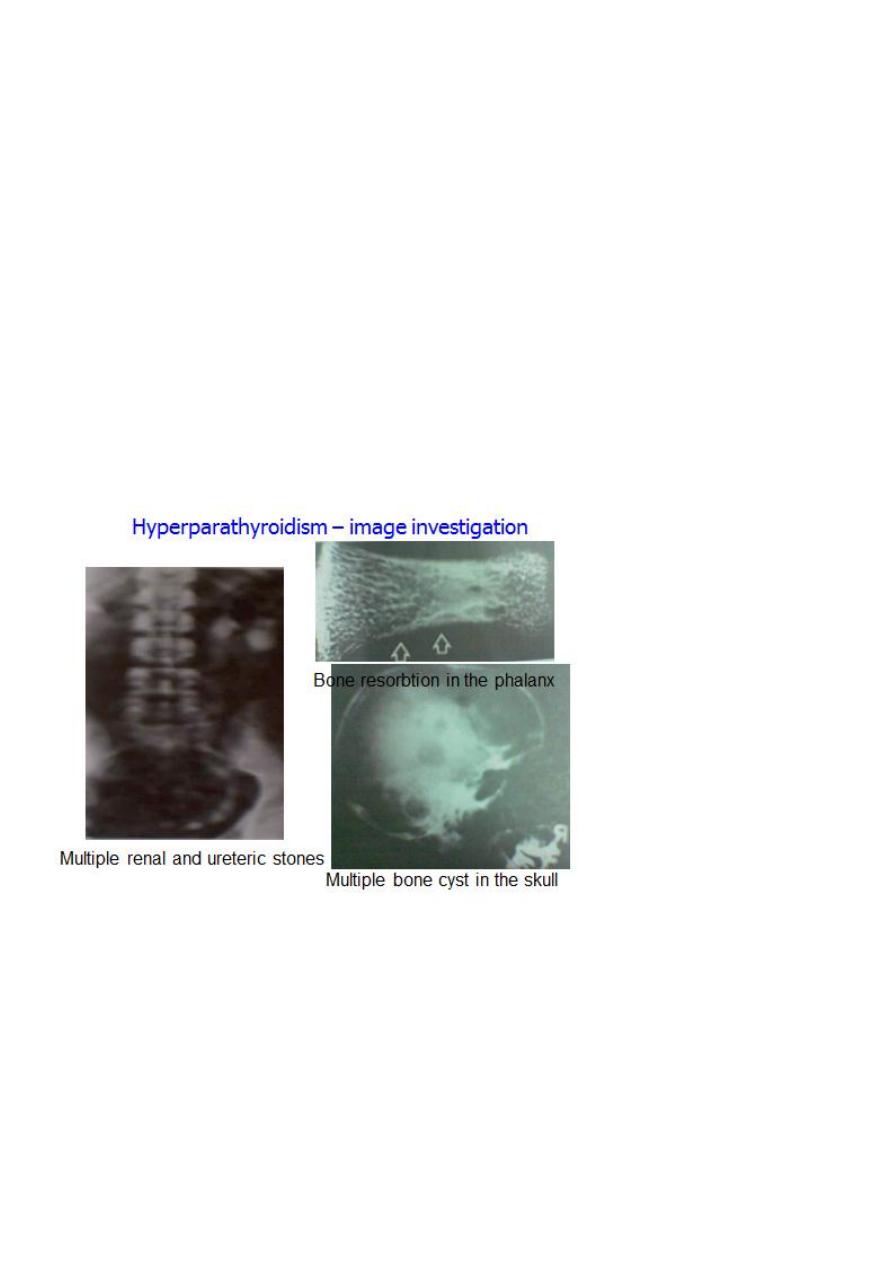
Renal :Colic, haematuria, back pain, polyuria, renal stones, nephrocalcinosis.
Cardiovascular :Hypertension, heart block, palpetation.
Musculoskeletal :Bone pain, pathological fractures, cyst, osteopenia, osteoporosis.
Gastrointestinal: Anorexia, nausea, dyspepsia, Polydipsia, weight loss constipation, Peptic
ulcer, pancreatitis, cholelithiasis.
Neurological Depression, lethargy, apathy, weakness, psychosis.
-
Hyperparathyroidism – chemical investigation :
1- High scrum Ca (normally 2.6 mmol\L)
2- low serum level of Ph (normally 0.8mmol\L)
3- Increase level of Alkaline phosphatase Enz.
4- Increase urine excretion of Ca (normally 6.2 mmol\L)
5- Increase serum level of chloride.

34
6- Increase level of Parath H (normally 0.5ugm\L).
Deferential diagnosis of hypercalsaemia:
1-. Hypercalsaemia of malignancy
2- Myeloma
3- Immobility
4-Vit D toxicosis.
5- Sarcoidosis
6- Hyperthyroidism
7- Phiochromcytoma
8- Milk alkali syndrome
9- Thiazid therapy.
Medical treatment
:
1- Adequate hydration
2- Avoid food with high calcium concentration.
3- Bisphosonate tablet.
4- Steroid and estrogen therapy.
5- calcium receptor agonist cinacalcet
6- Follow up of calcium level.
Indication of surgery
surgery is the only curative option and should be offered to all patients with significant
hypercalcaemia it is highly indicated in:
1- Bone involvement.
2- Repeated stone formation.
(3- High level of serum calcium (more than 2.85 m mol/l

35
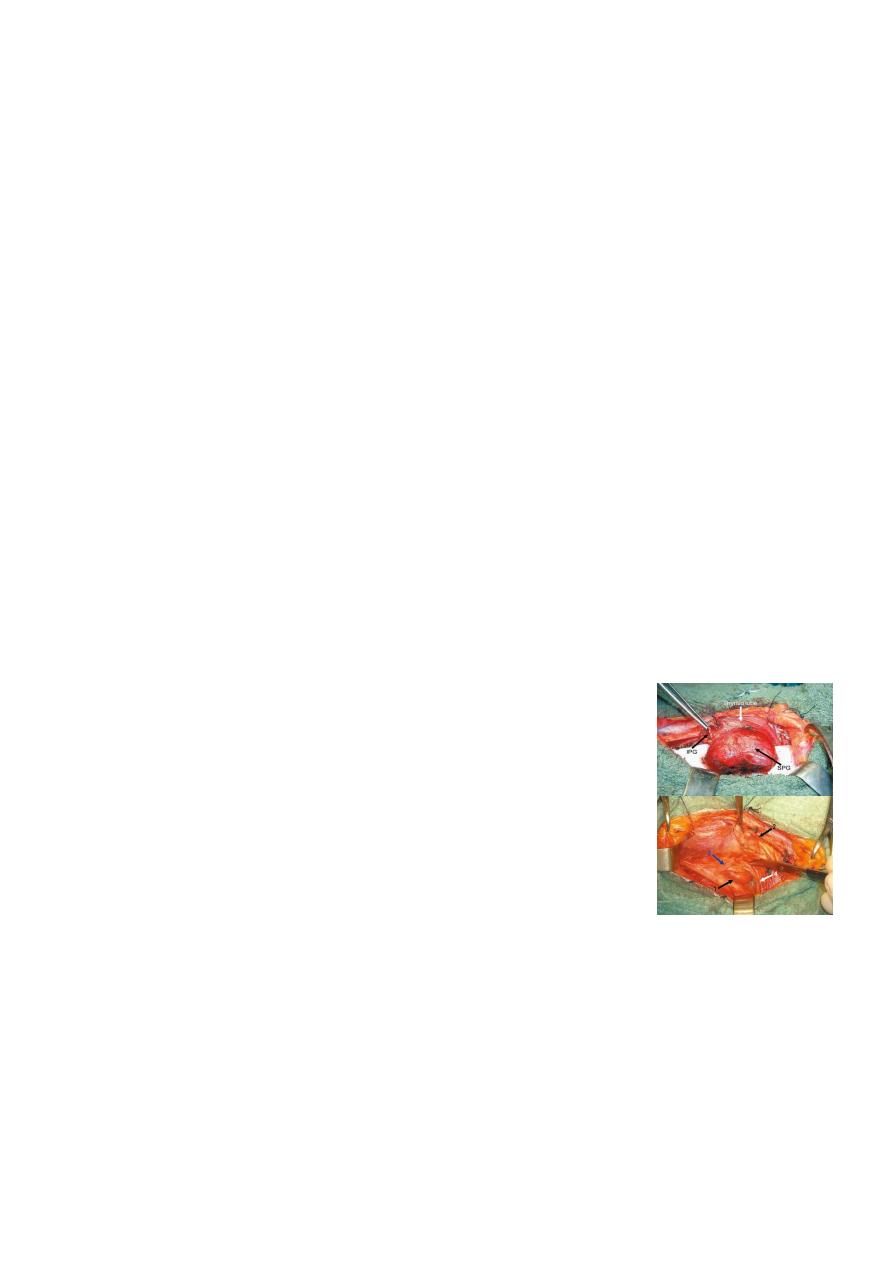
Surgical management:
Every attempt must be made to identify all four glands. Treatment depends upon the
number and pathology of abnormal glands.
1- If single adenoma is found and other parathyroid glands are normal, excision of the
tumor is enough.
2- If all parathyroid glands are enlarged, (parathyroid hyperplasia) ,treatment by
subtotal parathyroidectomy or by total
parathyroidectomy wiath autotransplantation.
3-In malignant tumor, en bloc excision of the tumor and the ipsilateral thyroid lobe.
Modified radical neck dissection is recommended in the presence of lymph node
metastases.
Complication of surgery
1- RLN injury
2- permanent hypoparathyroidism
3- recurrence of hyperparathyroidism which may result from:
missed parathyroid gland, graft dependent recurrence, parathyromatosis.
Pituitary gland:
The master endocrine gland, attached by a stalk to the base of the brain.
Its two lobes adenohypophysis and neurohypophysis
The anterior portion, controlled by the hypothalamus it secretes Prolactine, GH, LH, FSH,
ACTH, TSH, and MSH,,
The posterior pituitary secretes ;(ADH) and Oxytocin
Function of the hormones:
Thyroid stimulating hormone (TSH), stimulates the secretion of the thyroid
hormones; deficiency leads to
36
Adrenocorticotrophic hormone (ACTH), acts on the
release of cortisol; deficiency leads to
Prolactin cause milk production in the breasts.
Growth hormone necessary for growth and metabolism throughout life. over
secretion cause
if it occurs before growth of the long bones is complete, or
if it begins during adulthood. Under secretion can lead to
experienced during childhood, and decreased endocrine function accompanied by
lethargy and loss of sexual capacity in adult.
Gonadotrophins LH and FSH, which act on the
and
In female, FSH stimulates growth of the ovarian follicle and LH stimulates production of oestrogen
and progesterone from the ovary.
In male; FSH stimulates sperm production and LH stimulates testosterone production by the testes.
Deficiency of (LH) and (FSH), in female causes
In male it results in lose facial, scrotal and trunk hair, decrease muscle mass and
Both sexes may experience a decrease in
Lack of LH/FSH in children is associated with delayed puberty.
(ADH) (Vasopressin) plays a role in water balance and maintenance
of blood pressure, normal circulating concentrations causing water to be retained by the
kidney and higher concentrations causing blood vessels to constrict, thus raising blood
pressure. deficiency leads to the syndrome of
, leading to
, as well as
Oxytocin is important for the birth as stimulator for uterine contraction and for delivery of
the milk supply. Deficiency causes few symptoms, as it is only required at the time of
Pituitary tumors:
Account for 10–15% of all intracranial tumors.
The majority are benign adenomas.
37
Tumors less than 1cm diameter are microadenomas; larger tumors are macroadenomas.
Pituitary tumors may be functional or nonfunctional.
Functional tumors are often diagnosed when quite small size, due to endocrine
dysfunction, the most common are Cushing's disease, due to adrenocorticotropic hormone
secretion, Forbes-Albright syndrome, due to prolactin secretion, and Acromegaly, due to
growth hormone secretion.
Nonfunctional tumors are larger lesions causing mass effects such as visual field deficits due
to compression of the optic chiasm or panhypopituitarism due to compression of the gland.
Hemorrhage into a pituitary tumor causes abrupt symptoms of headache, visual
disturbance, decreased mental status, and endocrine dysfunction. This is known as pituitary
apoplexy.
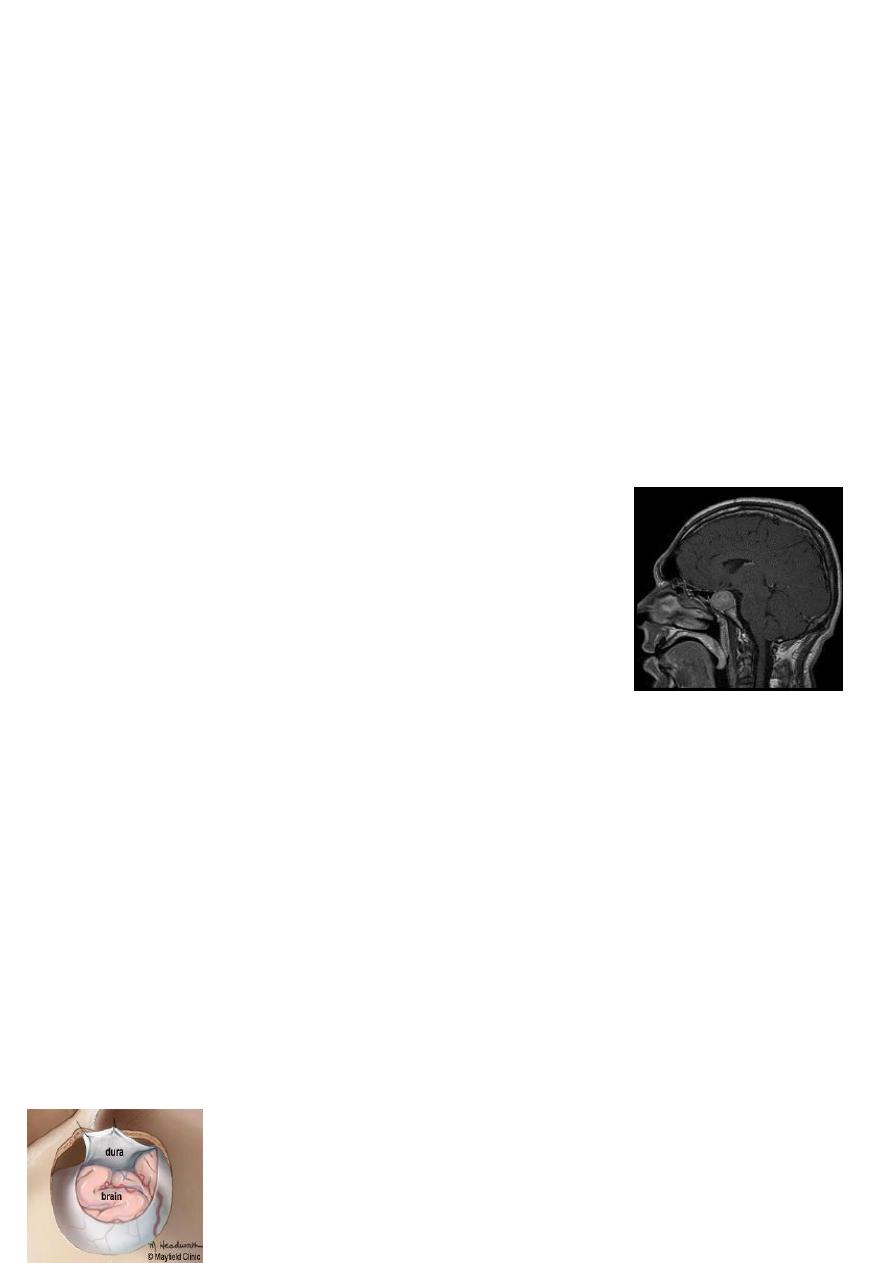
Investigation
Formal visual field and acuity testing.
MRI scan of the pituitary region
Baseline assessment of pituitary function including : Prolactin,
fasting serum and urinary free cortisol, GH, FSH, LH and TSH
Treatment
The aim is to alleviate mass effect, restore endocrine function and prevent recurrence.
Prolactinomas initially treated with dopamine agonists such as cabergoline or
bromocryptine.
Growth hormone-secreting tumors may treated with somatostatin analogues such as
octreotide.
Surgical management of pituitary tumors requires trans-sphenoidal surgery with an
operating microscope or endoscope assisted.
Large tumours with suprasellar extension
may need craniotomy.
