
1
Lecture 3
Professor Dr Numan Nafie Hameed Al-Hamdani
االستاذ الدكتور نعمان نافع حميد الحمداني
Neonatal Birth Traumas or injuries:
These are avoidable and unavoidable injuries to the NB that occurs during the birth
process. These are less common now because of more use of C/S. They can occur
during prenatal, natal, or postnatal period.
Risk factors for birth injuries include:
prim-parity,
maternal pelvic anomalies,
prolonged or unusually rapid labor,
oligohydraminos,
malpresentation of fetus,
use of mid-forceps or vacuum extraction,
versions and extractions,
VLBWT or extreme prematurity,
fetal macrosomia or large fetal head, and fetal anomalies.
Evaluation of Birth injuries:
1. History
2. Thorough examination, including neurologic examination
3. Special attention to symmetry of structure and function, cranial nerves, range of
motion of joints, integrity of scalp and skin.
Types of birth injuries:
1. Soft tissues injuries:
a. Caput succedaneum: it is subcutaneous, extra-periosteal fluid collection
over the presenting part in vertex presentation. It extends beyond the suture
lines, usually associated with molding of the skull bones, it appears at birth
and resolve in few days, it requires no treatment.
b. Cephal hematoma: it is sub-periosteal Hg due to rupture of vein of Galen
between the skull and periostium. It is confined to suture lines, usually over
parietal bones, the centre feel soft, it becomes visible on second or third day
of life, it resolves over several weeks(8 weeks), when they are extensive can
cause jaundice and anemia. Occasionally associated with linear fracture of
skull (5-20%), it requires no treatment, but treats infection, anemia and
2
jaundice. Aspiration of blood collection is contraindicated as it will induce
infection.
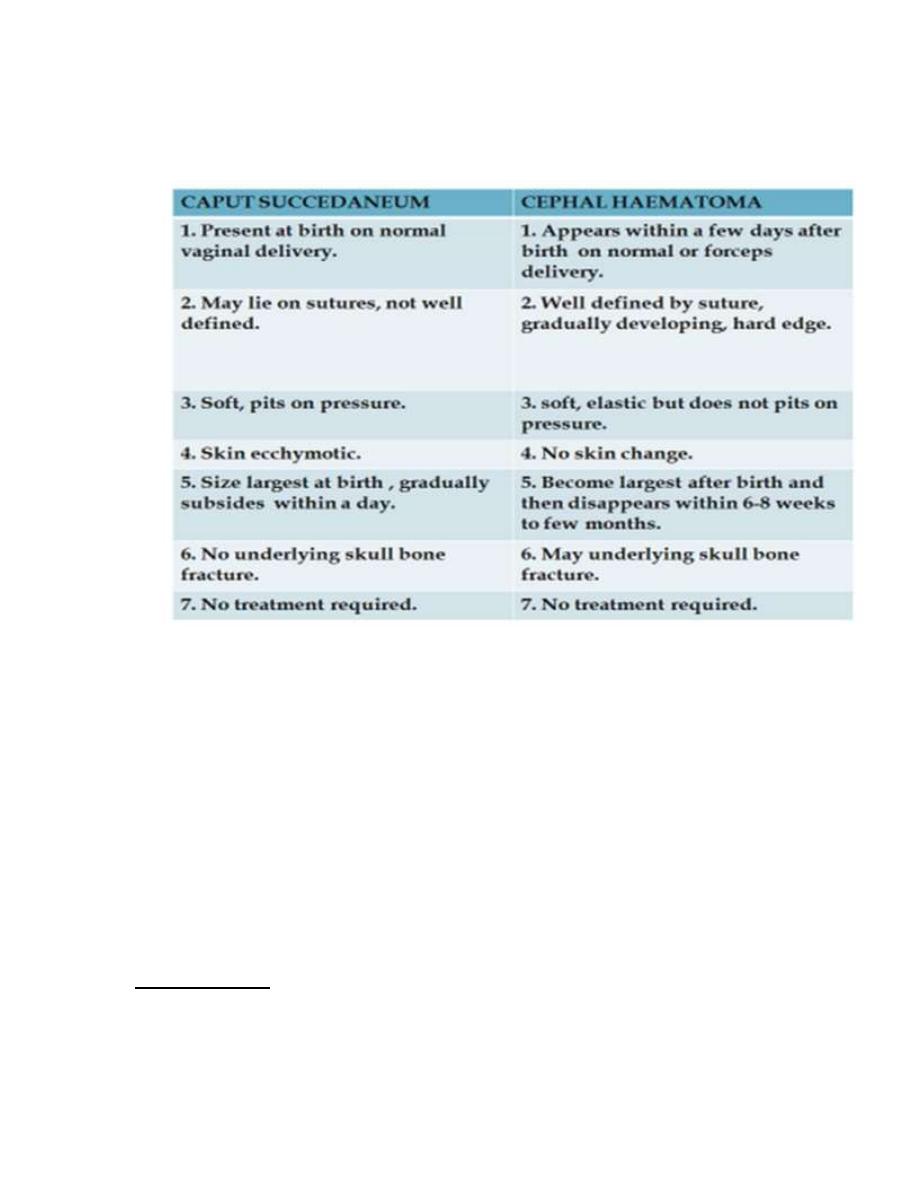
Table showing the difference between caput and cephalohematoma
c. Chignon: bruising edema from ventose extraction delivery.
d. Bruising of face after face presentation, and Bruising of genitalia after
breech delivery due to repeated PV exam.
e. Abrasion of the skin from scalp electrodes applied during labor, or
accidental scalpel incision at C/S.
f. Subgaleal Hg: it is sub-aponeurotic Hg (under skull aponeurosis), spread
rapidly over head downward to the eye, very uncommon, may be associated
with serious blood loss, and may be associated with ICH, 90% associated
with vacuum extraction. It requires no treatment unless there is shock or ICH
that require blood transfusion.
g. Severe or fatal injuries (very rare) from tear of the tentorium cerebelli or
fax cerebri.
h. Subconjuctival or Retinal Hg: frequent and common. It requires no
treatment.
2. Nerve injuries:
A. Brachial plexus nerve injuries: this result from traction to the cervical nerve
roots. They may occur after breech delivery or with shoulder dystocia.
3
Erbs`palsy (waiters` tip posture): it is upper nerve roots injury (C5-C6). The
moro, biceps reflexes are absent, but grasp reflex is preserved.
Klumpks` palsy (C7,8,T1): the lower nerve roots are involved less frequently,
resulting in weakness of long flexors of wrists and fingers and intrinsic muscles
of the hand. The grasp reflex is absent.
Immobilize for one week, then passive range of motion exercise of all joints of
limb. It needs physiotherapy from second week of life. Most palsies resolve
over few weeks. Occasionally following severe injury, paralysis is permanent.
Surgical reconstruction of the nerve is attempted.
B. Facial nerve injury: most common peripheral nerve injury in neonates. May
result from compression of the facial nerve by forceps blades or against
mothers` pelvis. It is usually transient, seen as asymmetrical crying face.
C. Phrenic nerve injury: it involves 3
rd
, 4
th
, 5
th
cervical nerves. There is
ipsilateral diaphragm paralysis, 75% have brachial plexus injury, present with
respiratory distress and cyanosis, diagnosed by U/S, fluoroscopy.
3. Fractures:
A. Skull fractures: They are rare, usually linear, usually in parietal bones, they
requires no treatment, just observation. Depressed fracture usually in
parietal or frontal bones, they are unusual, but may be seen with
complicated forceps delivery. If no neurologic deficit ---- no treatment. If
neurologic deficit--- do CT scan –surgical elevation.
B. Fracture clavicle: usually from shoulder dystocia. a snap may be heard at
delivery, or infant may have reduced movement of the arm on affected side,
or a lump from callus formation over clavicle may be felt. The prognosis is
excellent.
C. Fracture of humerus and femur: usually mid-shaft, occurring at breech
delivery, they present with loss of spontaneous arm or leg movement, pain
and swelling in passive movement if displaced. Diagnosis by x ray,
treatment by splinting, close reduction and casting.
4. Visceral trauma: Trauma to liver, spleen, and adrenals: they are
uncommon, seen in macrosomic infants, very premature infants, with or without
breech or vaginal deliveries. They may be asymptomatic, or present with shock,
pallor, jaundice. They are diagnosed by ultrasound. Sub-capsular hematoma of
liver is the most common, may follow macrosomia, hepatomegaly, breech
presentation. It is suspected if infant had anemia, hypovolemia, shock, but no
evidence of IVH. It is usually seen in 1-3 days after birth. Serial PCV is needed
suggesting blood loss. Management by restoring blood volume, correct
coagulation disorder, and surgical consultation for possible laprotomy.
4
5. Intracranial Hg: subdural Hg, subarachnoid Hg, per-ventricular Hg, intra-
ventricular Hg, Intra-parenchymal Hg or cerebral Hg.
Subdural Hemorrhage (SDH): usually seen in association with birth trauma,
cephalo-pelvic disproportion, LGA babies, forceps deliveries, skull fracture,
and postnatal head trauma. It may be asymptomatic initially as Rbcs undergoes
hemolysis; the water is drawn into the Hg resulting in expanding symptomatic
lesion. Anemia, vomiting, seizure, macrocephaly may occur in infants who is
1-2 months old with SDH. Occasionally massive SDH in neonate by rupture of
the vein of Galen or by inherited coagulation disorder as hemophilia.
Treatment of all symptomatic SDH is surgical evacuation.
6. Neonatal Cold injury: LBWT neonates and full term neonates with CNS
disorders are risk groups, usually in inadequately heated homes and damp cold
spells. Neonates presents with apathy, refusal to feed, oliguria, coldness to
touch, low body temperature of 29.5- 35C. They had immobility, edema,
redness of extremities, bradycardia, apnea, facial erythema (due to failure of
oxyHb to dissociate at low temp.), and local hardening over areas of edema.
Serious metabolic disturbances especially hypoglycemia, acidosis.
Hemorrhages especially pulmonary Hg may occur. Management includes
gradual re-warming and correct hypotension by normal saline 10-20 mls/kg,
correct hypoglycemia, and metabolic disturbances by NAHCO3 and treating
infection and bleeding. Prevention by providing adequate environmental
temperature. Outcome 10% mortality, 10% of survivors got brain damage.
Quiz:
A consultant in the neonatal intensive care unit is recommending a trial of pyridoxine for a
patient. Which of the following problems in a newborn infant might respond to a
pharmacologic dose of pyridoxine?
(A) blindness
(B) seizures
(C) jaundice
(D) rash
(E) urinary retention
NEONATAL SEIZURES
Definition. A seizure is defined clinically as a paroxysmal alteration in neurologic
function (i.e. behavioral, motor, or autonomic function).
Incidence. Neonatal seizures are not uncommon. The incidence ranges from 1.5 -
14 in 1000 live births.
Causes of neonatal seizures
A. Perinatal asphyxia and HIE
5
B. Intracranial hemorrhage (Subarachnoid hemorrhage, Periventricular or
intraventricular hemorrhage, Subdural hemorrhage)
C. Metabolic abnormalities: Hypoglycemia, Hypocalcaemia, Electrolyte
disturbances (hypo- and hypernatremia), Amino acid disorders
D. Infections: Meningitis, Encephalitis, Syphilis, cytomegalovirus infections,
Toxoplasmosis, Cerebral abscess
E. Drug withdrawal F. Toxin exposure (particularly local anesthetics)
G. Inherited seizure disorders: Benign familial epilepsy, Tuberous sclerosis,
Zellweger syndrome, Pyridoxine dependency
H. Congenital malformations
Clinical presentation.
It is important to understand that seizures in the neonate are different from those
seen in older children. The differences are perhaps due to the neuroanatomic and
neurophysiologic developmental status of the newborn infant. In the neonatal
brain, glial proliferation, neuronal migration, establishment of axonal and dendritic
contacts, and myelin deposition are incomplete.
Four types of seizures, based on clinical presentation, are recognized:
Subtle, clonic, tonic and myoclonic seizures.
A. Subtle seizures. These seizures are not clearly clonic, tonic, or myoclonic and
are more common in premature than in full-term infants. Subtle seizures are more
commonly associated with an electroencephalographic seizure in premature infants
than in full-term infants.
Seizure is differentiated from nonconvulsive apnea (which is due to sepsis, lung
disease, or metabolic abnormalities) by the absence of electroencephalographic
abnormalities. Apnea as a manifestation of seizures is usually accompanied or
preceded by other subtle manifestations. In premature infants, apnea is less likely
to be a manifestation of seizures.
B. Clonic seizures are more common in full-term infants than in premature infants
and are commonly associated with an electroencephalographic seizure. There are
two types of clonic seizures.
1. Focal seizures.
2. Multifocal seizures. Several body parts seize in a sequential, nonjacksonian
fashion (eg, left arm jerking followed by right leg jerking).
C. Tonic seizures occur primarily in premature infants. Two types of tonic seizures
are seen.1. Focal seizures.
2. Generalized seizures.
D. Myoclonic seizures are seen in both full-term and premature infants and are
characterized by single or multiple synchronous jerks. Three types of myoclonic
seizures are seen.1. Focal seizures
6
2. Multifocal seizures
3. Generalized seizures
Note: It is important to distinguish jitteriness from seizures. Jitteriness is not
accompanied by abnormal eye movements, and movements cease on application of
passive flexion, movements are stimulus sensitive and are not jerky.
Diagnosis
A. History
1. Family history. A positive family history of neonatal seizures is usually
obtained in cases of metabolic errors and benign familial neonatal convulsions.
2. Maternal drug history is critical in cases of narcotic withdrawal syndrome.
3. Delivery. Details of the delivery provide information regarding maternal
analgesia, the mode and nature of delivery, the fetal intrapartum status, and the
resuscitative measures used. Information regarding maternal infections during
pregnancy points toward an infectious basis for seizures in an infant.
B. Physical examination
1. A thorough general physical examination and neurologic examination.
Determine: Gestational age, Blood pressure, Presence of skin lesions, Presence
of hepatosplenomegaly.
2. Neurologic evaluation
3. Notation of the seizure pattern. When seizures are noted, they should be
described in detail, including the site of onset, spread, nature, duration, and level of
consciousness. Recognition of subtle seizures requires special attention.
C. Laboratory studies. We must use the information obtained by history taking
and physical examination and look for common and treatable causes.
1. Serum chemistries. Estimations of serum glucose, calcium, sodium, blood urea
nitrogen, and magnesium and blood gas levels.
2. Spinal fluid examination.
3. Metabolic disorders. Blood ammonia levels, urine and plasma Amino acids and
urine for reducing substances, urea cycle disorders, maple syrup urine disease
D. Radiologic studies
1. Ultrasonography of the head is performed to rule out IVH or periventricular
hemorrhage.
2. CT scanning of the head provides detailed information regarding intracranial
disease. CT scanning is helpful in looking for evidence of infarction, hemorrhage,
calcification, and cerebral malformations. Experience with this technique suggests
that valuable information is obtained in term infants with seizures, especially when
seizures are asymmetric.
E. Other studies 1. Electroencephalography (EEG) EEGs obtained during a
seizure will be abnormal. Interictal EEGs may be normal. The diagnostic value of
7
an EEG is greater when it is obtained in the first few days because diagnostic
patterns indicative of unfavorable prognosis disappear thereafter. EEG is valuable
in confirming the presence of seizures when manifestations are subtle or when
neuromuscular paralyzing agents have been given. EEGs are of prognostic
significance in full-term infants with recognized seizures. For proper interpretation
of EEGs, it is important to know the clinical status of the infant (including the
sleep state) and any medications given.
Management.
Because repeated seizures may lead to brain injury, urgent treatment is
indicated.
The method of treatment depends on the cause.
common and treatable causes.
A. Hypoglycemia. Hypoglycemic infants with seizures should receive 10%
dextrose in water, 2-4 mL/kg intravenously, followed by 6-8 mg/kg/min by
continuous intravenous infusion.
B. Hypocalcemia is treated with slow intravenous infusion of calcium gluconate.
If serum magnesium levels are low (
1.52 mEq/ L), magnesium should be given.
C. Anticonvulsant therapy. Conventional anticonvulsant treatment is used when
no underlying metabolic cause is found.
Loading doses of phenobarbital and phenytoin control 70% of neonatal seizures.
1. Phenobarbital is usually given first. When phenobarbital alone fails to control
seizures, another agent is used. If seizures are not controlled at a serum
phenobarbital level of 40 mcg/ mL, it is recommended to administer a second
agent (eg, phenytoin).
2. Phenytoin is used next by many practitioners. Fosphenytoin may be a preferred.
3. Pyridoxine trial with EEG monitoring is recommended.
4. Diazepam (Valium) has not been used extensively in the control of neonatal
seizures.
5. Lorazepam, given intravenously, has been quite effective and safe, even when
repeated 4-6 times in a 24-h period
6. Intravenous midazolam and oral carbamazepine have been found to be
effective.
7. Paraldehyde, given rectally, has been used as an effective anticonvulsant.
D. Duration of anticonvulsant therapy. The optimal duration of anticonvulsant
therapy has not been established. Although some clinicians recommend
continuation of Phenobarbital for a prolonged period, others recommend stopping
it after seizures have been absent for 2 weeks.
Prognosis.

8
As a result of improved obstetric management and modern neonatal intensive care,
the outcome of infants experiencing seizures has improved. The mortality rate has
decreased from 40 to 20% but neurologic sequelae are still seen in 25-35% of
cases.
As would be expected, the prognosis varies with the cause.
Infants with hypocalcaemic convulsions have an excellent prognosis.
Seizures secondary to congenital malformations have a poor prognosis.
Symptomatic hypoglycemia has a 50% risk of death or complications.
CNS infection carries a risk of 70%.
Asphyxiated infants with seizures have a 50% chance of a poor outcome.
17% of patients with neonatal seizures have recurrent seizures later in life.



