
Radiology L:2 د.نجالء
Radiology of bone disease :
Osteomyelitis :
- Osteomyelitis is most often caused by staphylococcus aureus ( blood borne infection )
- usually affects infants & children.
- Site : most vascular area where is the metaphysis so the lesion seen around the long bone (
femur , tibia , knee joint )
The Imaging technique
1. Plain x-ray : selayed signs in it for 1014 days accourding to each child and immunity
2. TC-99 radioisotope bone scan : is sensitive
3. MRI : if there is no bone scan, the most sensitive imaging is MRI for early stages of
osteomyelitis
The radiological signs :
1. the earliest sings on plain radiographs are soft tissue swelling , and bone destruction in the
metaphysis with zone of transition which ill define
2. periosteal reaction: is solid type that eventually may become very extensive and become
very thick and surround the bone( infected area ) to form a second cortex and called an
involucrum ( which is specific sign of osteomyelitis that consist of thick layer of second
cortex composed of periosteum which separated from the original cortex by thin layer of
pus )
3. The bone sequestrum : dense piece of bone in the lytic area which is part of the original
bone but separated from it and floating within the lesion , the cause of this sign is the
devascularization to this area . its pathognomonic and sometimes discharging to skin
Radiology L:2 د.نجالء
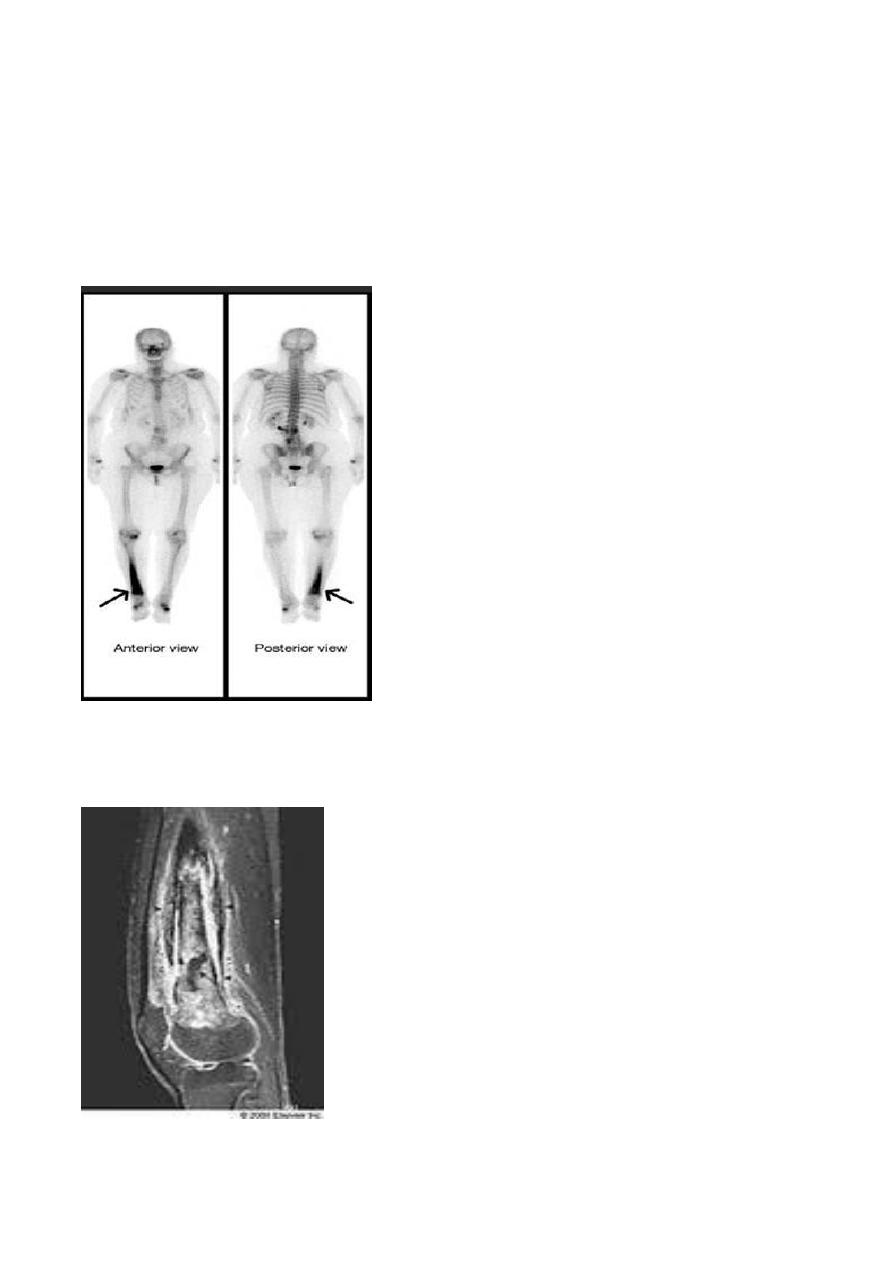
4. In All body bony scan : we have two phases
A.early blood pooling phase : imaging the stain that entre to the lesion area with the blood
*the infected area increase the uptake so appear as black or increase the black color (hyperaemia)
B.Delayed bone scan phase : after the blood out from area , each active cell will uptake the stain
**** so in osteomyelitis we have : increase uptake + delayed bone phase
5. U/S :can demonstrate sub periosteal collections of pus( or in adjacent soft tissue ) well
before bone changes are evident on plain film,
Radiology L:2 د.نجالء
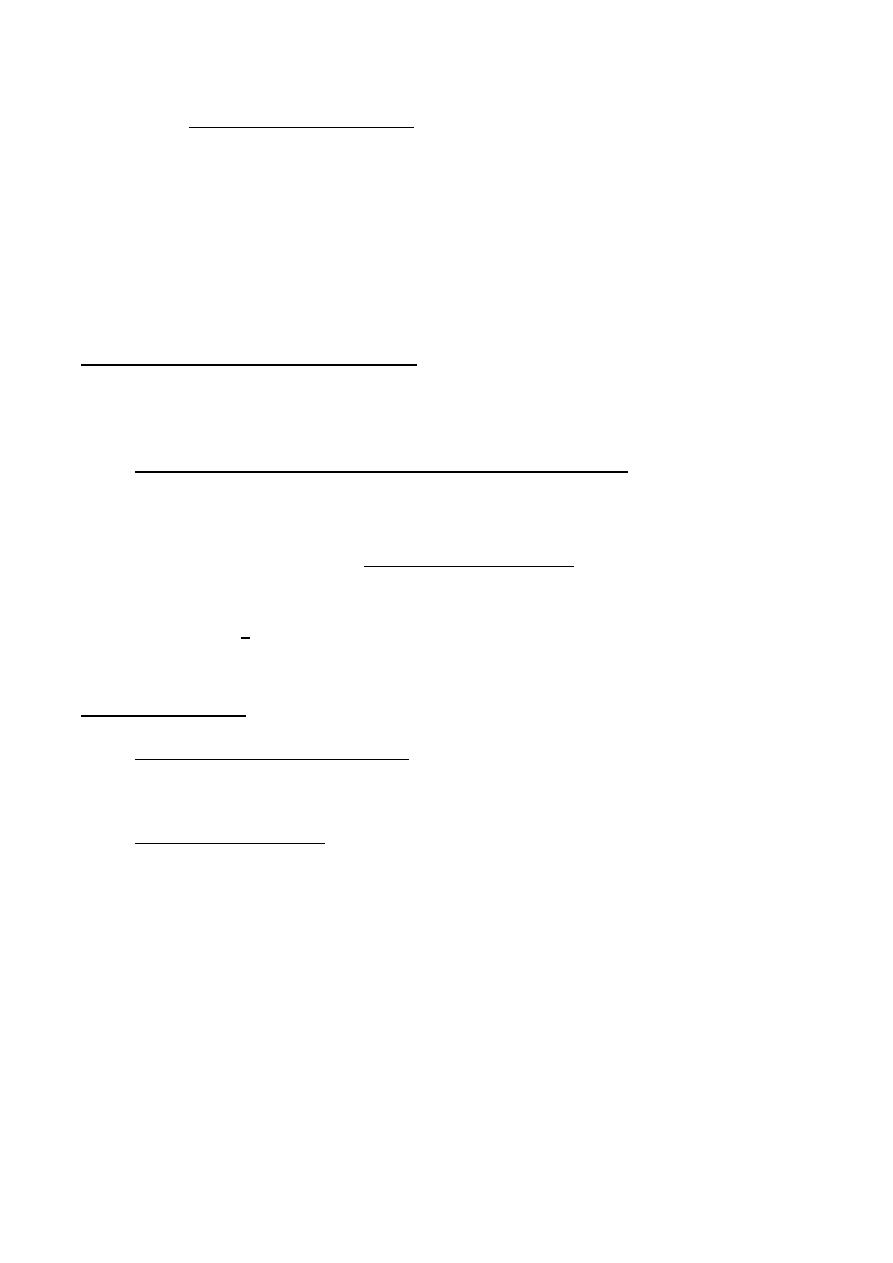
6. MRI :is the imaging modality of choice . in early stages before pus ,damage occur & shows
evidence of bone odema and pus accumulation in the bone & soft tissue .
- In chronic osteomylitis the bone becomes thickened & sclerotic with loss of differentiation
between the cortex & the medulla . within the bone there may be sequestra & areas of
bone destruction ,this type of a lesion is known as bodies abscess.
- Tuberculous osteomyelitis affects most frequently the spine & large joints , but any bone
can be affected , produces large areas of bone destruction which , unlike pyogenic
osteomyelitis , may be relatively asymptomatic in the early stages .
Distinction of neoplasm from osteomyelitis : It is not always possible using imaging tests to
distinguish osteomyelitis from bone tumor
1. The most important thing to distinguish is to asked history , the infection presented normal
in x-ray till 10 – 14 days / while tumors have + signs on x-ray at time of presentation .
With malignant bone tumor the radiographs are usually abnormal
2. The clinical signs and symptoms of the patient : infection presented with fever , bone pain ,
discharging from skin / while tumors have no sign or symptoms except ewing sarcoma
3. If there is an infection with late presentation and not have early film to make comparison ,
we use US for discharge or pus CT & MRI more informative.
4. biopsy is then needed .
5. Bone scanning is positive in both osteomyelitis & malignant tumour and can not be used in
differentiation .
bone infarction :
- Solitary or multifocal lesion
-
Occurs most often in the intra -articular portions of the bones Can occur in the shaft of a
bone
-
The predeposing factors :
1. Hemplytic anaemia ( sickle cell disease )
2. Steroid therapy
3. caisson disease : specific disease affect small vessles in people who applied to high
pressure environment ( diving , coal workers ) where the nitrogen escape from the
vessles to medullary area and cause infarction
4. radiation therapy.

Radiology L:2 د.نجالء
Radiological finding :
First onset : no signs
Later : once healed , they appear as irregular calcification in the medulla of along bone
Multifocal Boney Lesion
: DDx : metastasis + myloma
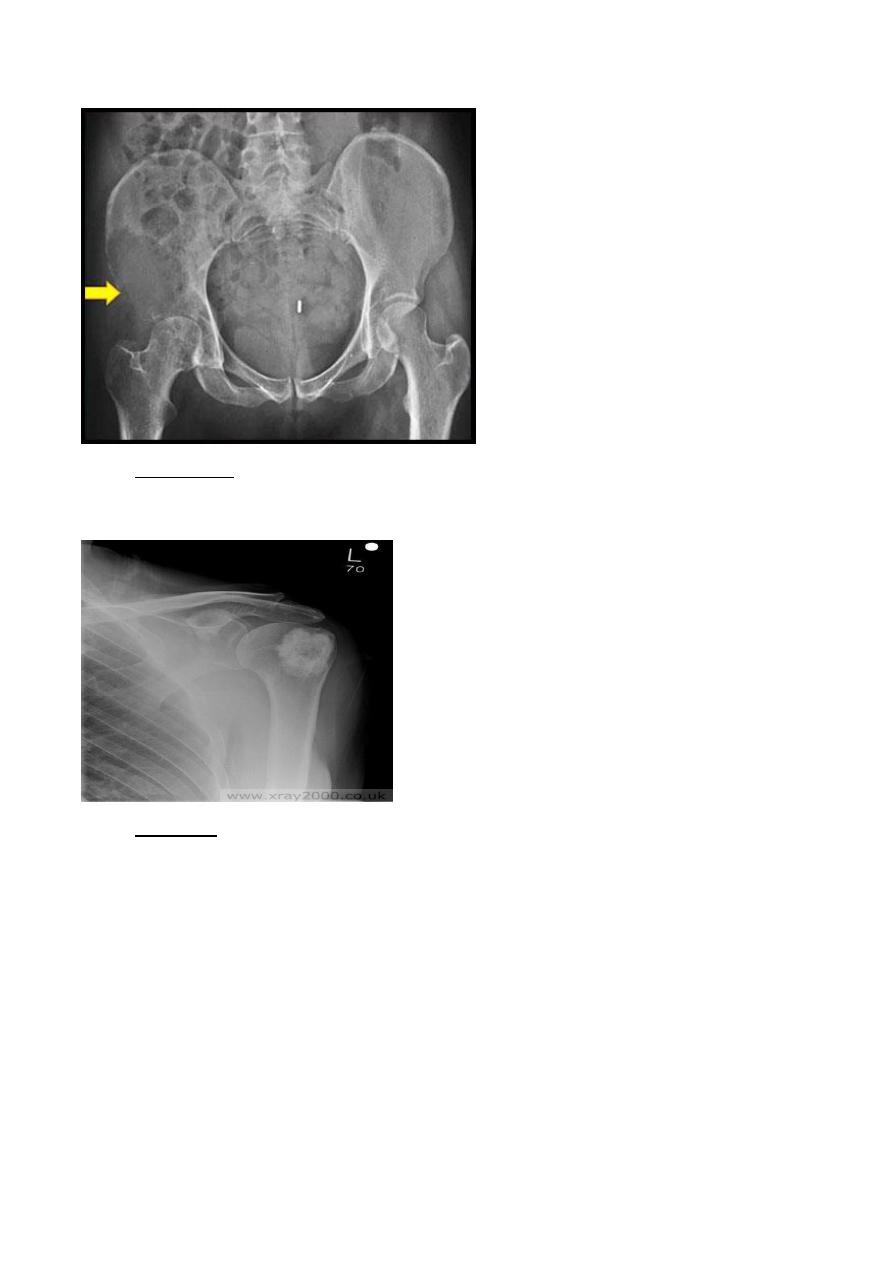
1. Metastasis :
Affect the areas that have red marrow : spine , skull , ribs , pelvis, humeri , femora
The pattern of presentations :
Lytic type : reduce density of the bone , given rise to well-define or ill-define lesion without
sclerotic rim
DDx : 1. Commonest bronchogenic carcinoma in male and breast cancer in female
2.to less incidence thyroid cancer , colon cancer , kidney
3.in children : neuroblastoma ( which only cause periosteal reaction) and leukemia
Radiology L:2 د.نجالء
Sclerotic type : which give rise to whit lesion in x-ray, areas increase density of bones m ill-
define area with ill-define margin , solitary or multifocal
DDx : prostate in male and breast cancer in female .
Mixed type : less incidence , like in breast cancer 10%
Imaging modalities :
1. MRI the most sensitive and specific & it is better than radionuclide scanning for the
detection of metastases. But it more difficult to survey whole skeleton by MRI
2. Radioisotope : to detect all the body ,is much more sensitive then plain film
3. CT : less sensitive
** they don’t give rise to periosteal reaction except nuroblastoma
Radiology L:2 د.نجالء
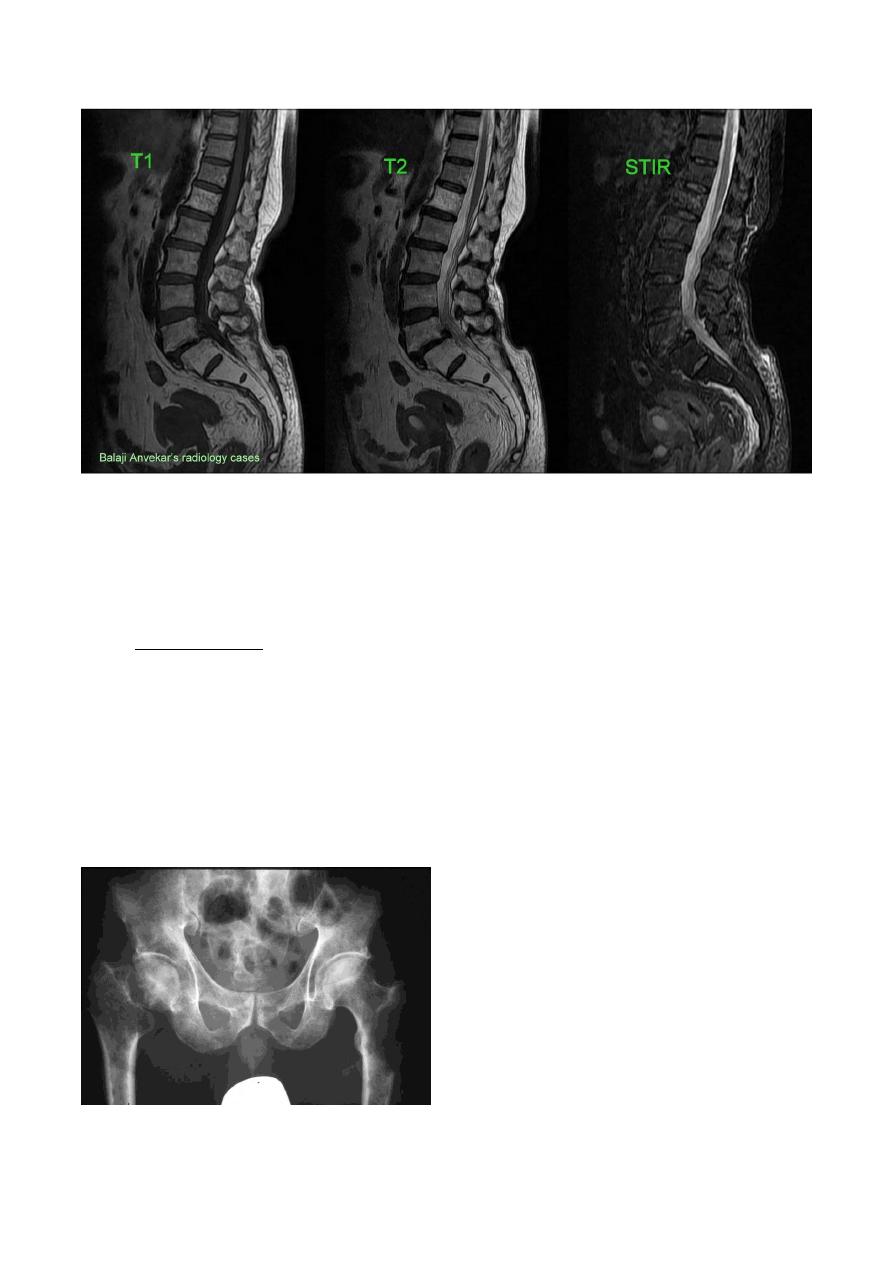
T1 weighted : fluid is black and fat black , bone white
T2 : fluid white , fat black , bone white
STRI : fluid and bone black , fat white
2. Multiple myloma
- frequently seen in bones with active haemopoiesis , so in axial skeleton ( skull , spine , ribs ,
pelvis , proximal portions of humeri and femora )
- in old age group , male more than female
- lesions may resemble lytic metastases in every way but are often better defined
- diffuse marrow involvement may give rise to generalized loss of bone density
- two types of presentation , the commonest type is multiple lytic roumded lesion with
variable sizes , without sclerotic rim
***MRI has good role in detecting multiple myeloma lesions. + Plain X-Ray
Radiology L:2 د.نجالء
3. Lymphoma & leukemia
Lymphoma : multifocal , aggressive , present as same as the primary tumors but it multifocal
Leukemia : occur in child , in metaphyseal regions and it bilateral
lesions closely resembling metastases in all imaging modalities Bone involvement in acute leukemia
in children is not uncommon
Leukemic deposits produce ill-defined permeative bone destruction , , bone lesions are very rare in
adult leukemia .
4. 4. Multiple periosteal reactions
DDx of multiple ( solid ) periosteal reaction are
1. osteomyelitis
2. osteoid osteoma
3. non-accidental injury.
4. widespread bone infection ,e.g. congenital syphilis.
5. venous stasis & ulceration of legs (usually involving tibia & fibula).
6. hypertrophic pulmonary osteoarthropathy. Like in bronchogenic carcinoma but occur in
other / site: bones of forearm and legs ( tibia,fibula,ulna,radius) when become extensive it
reach small bones
7. scurvy disease.
Diseases that cause Generalize reduction in bone
density (osteopenia )
DDx:
1. Osteoporosis 2. osteomalacia and rickets 3. hyperparathyroidism 4. multiple myeloma
1. osteoporosis :
reduction in the amount of osteoid tissue in the bone matrix , but when take biopsy and send
histopathology study the bone is normally mineralized ( Ca++ level normal but osteoid decrease )
The Causes :
1. Idiopathic : according to the age it divided into :
a. In childhood : idiopathic juvenile osteoporosis
b. In Female postmenopausal : idiopathic postmenopausal osteoporosis
c. In both male and female but above 60Yrs : Idiopathic senile osteoporosis
2. Steroid therapy + Cushing syndrome
3. Disuse : immobilization for long period will decrease the blood supply to specific areas and
cause osteoporosis

Radiology L:2 د.نجالء
Radiological signs :
- site : early sign seen in spine
1. generalized reduction in bone density
2. cortex appear stand out clearly ( penciled in )
3. compression fracture so decrease in the height of vertebrae and presented as biconcave
appearance or wedge shape because of the collapse of vertebral bodies
4. widening of the disc space
5. in long bones generalized reduction in bone densities , have thin cortices and many
trabeculae resorbed and stand out clearly m and deformity of bones ( softening )
** screening by measuring bone mass b DEXA
2. osteomalcia and rickets
the osteoid matrix remain at same amount in the normal bones but Ca++ decrease and reduce
density
Rickets : before closure of epiphyseal palate
Osteomalacia : after closure
the Causes :
1. vitamin D deficiency or decrease sun exposure
2. malabsorption
3. renal disease
osteomalacia :
signs :
1. generalized reduction of bone density
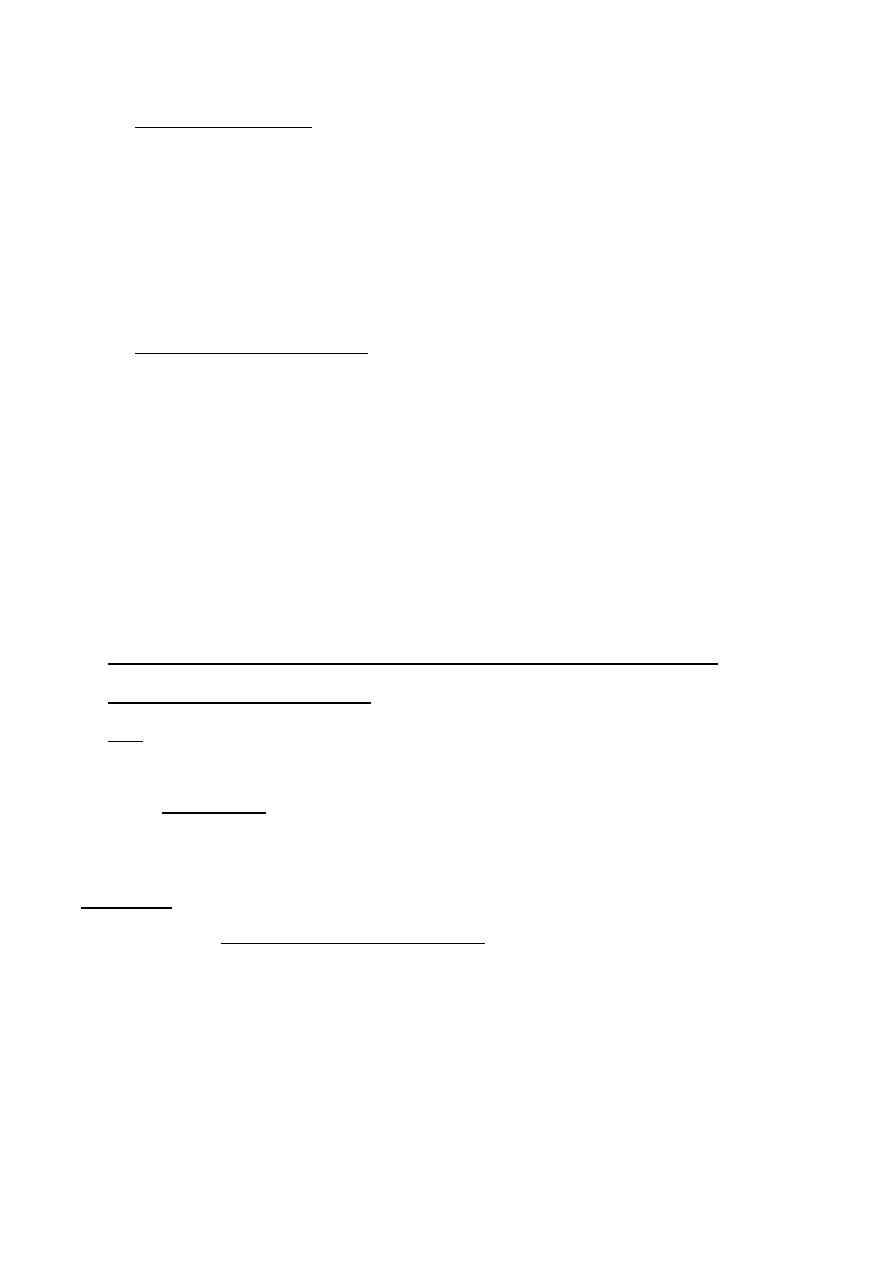
2. looser zone : pseudo fracture : it is characteristic for osteomalacia
pseudo fracture : linear band which is lucent in x-ray then become sclerotic
Radiology L:2 د.نجالء
sites : 1. Median border of upper femoral neck 2. Border of scapula 3. Border of pubic
bone
3. the bone softening , spine and vertebrae are biconcave , femora may be bowed and in
severe cases the side wall of pelvis may bend inwards and give rise to Tri-Radiate pelvis (
sometimes occur in osteoporosis )
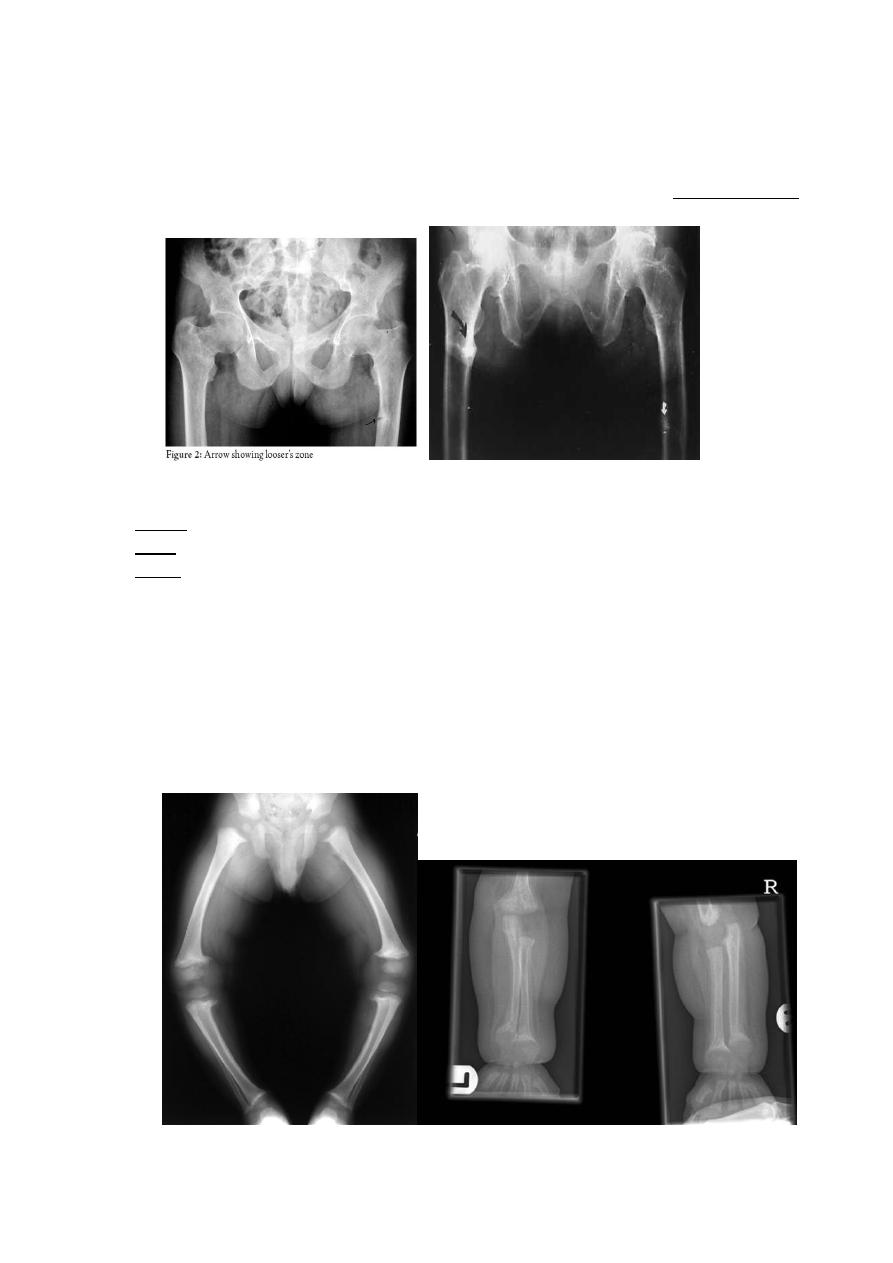
Rickets
Site : higher growth rate area ( knee , wrist , chest " in severe cases " )
Signs :
1. Generalized reduction in bone density
2. Loss of provisional zone of calcification : we have epiphyseal palate between metaphysis
and epiphysis , found it on the metaphysis .. so the provisional zone is the upper most
area of metaphysis ( it very early sign )
3. Widening of metaphysis
4. Cupping of metaphysis
5. Increase distance between metaphysis and epiphysis
6. Deformities in bones
Radiology L:2 د.نجالء
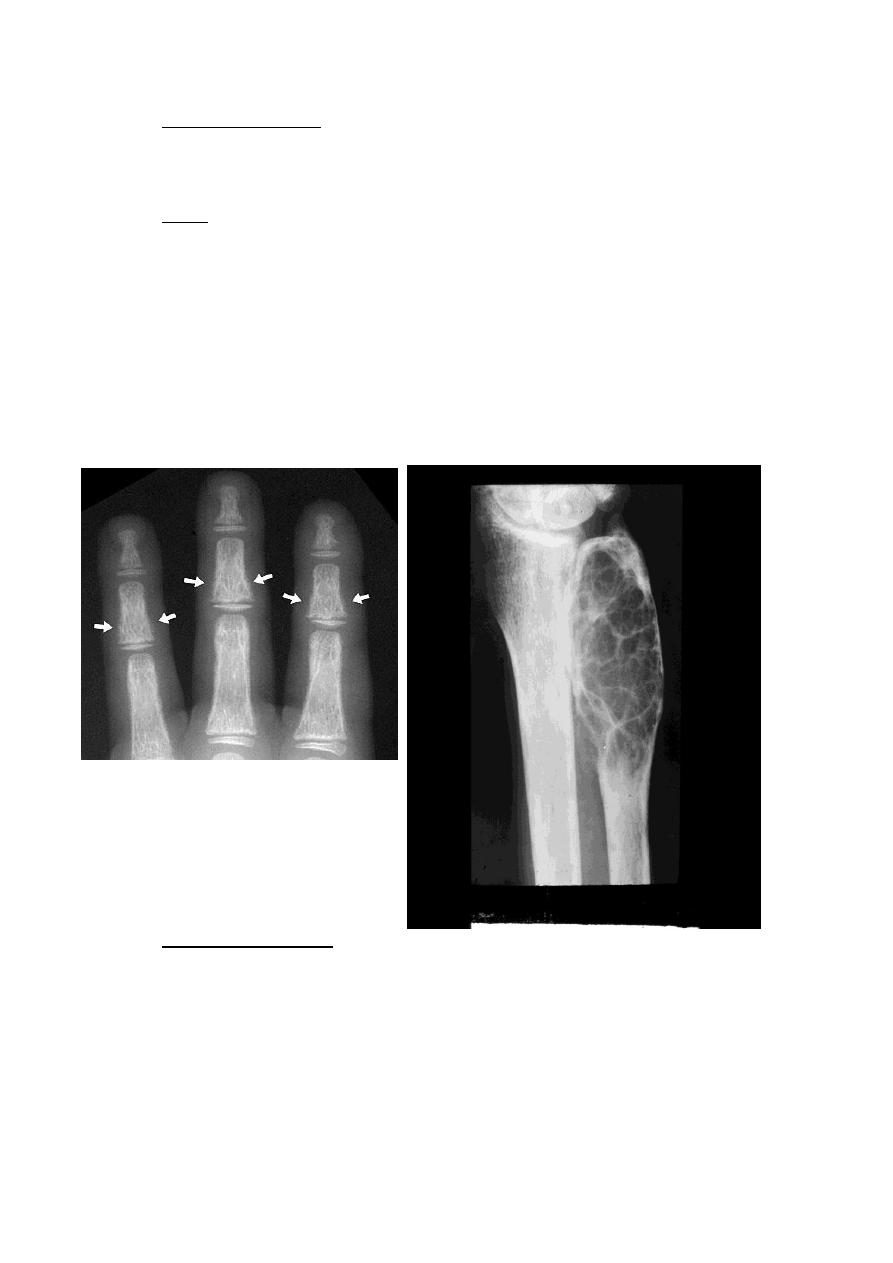
3. Hyperparathyroidism
This endocrine disease that affect on bones ,, increase in PTH will mobilize Ca++ into
blood so secondary cause osteopenia
Signs :
1. Generalized loss of bone density with loss of the differentiation between the cortex
& medulla , in advanced disease there may be marked deformity of the skeleton
(early sign )
2. The hallmark is sub periosteal bone resorption Which occurs particularly in the
hands on the radial side of the middle phalanges and at the tips of the terminal
phalanges, may associated with resorption of the outer end of the
3. Soft tissue calcification, vascular calcification & chondrocalcinosis sometimes occurs..
4. Brown tumour are occasionally present : are lytic lesions which may be single or
multiple occur more commonly in the mandible & pelvis but any bone may be
involve , its rare in the in secondary hyperparathyroidism .
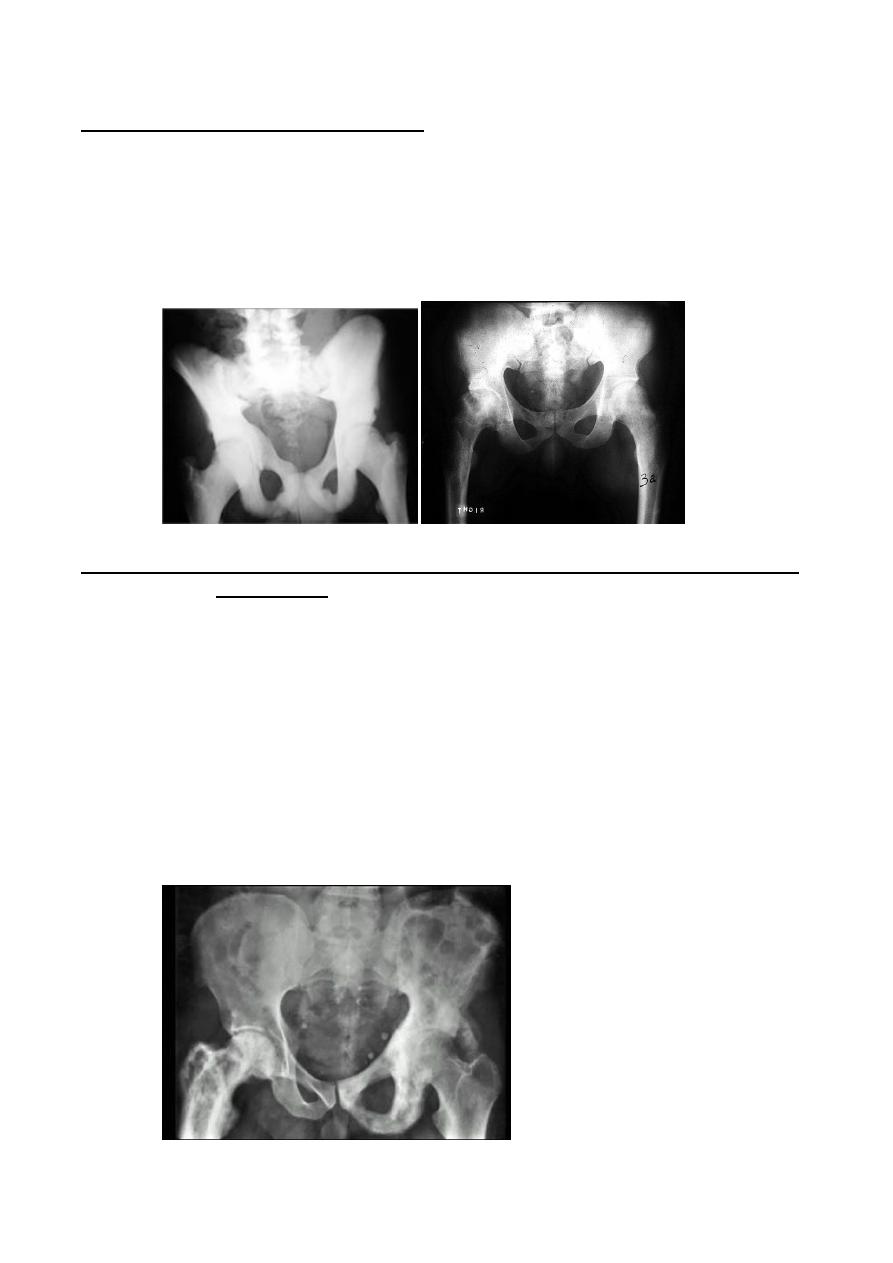
4. Renal osteodystrophy :
Patient with chronic renal failure can has the following bony lesions either in
isolation or together :
1. Osteomalacia in adult , rickets in children .
2. Hyperparathyroidism .
3. Sclerosis , less common feature , usually affect the spine producing the so
called rugger –jersey spine& at the metaphyses of the long bones.
Radiology L:2 د.نجالء
Generalized increase in bone density :
The conditions producing this appearance
1. sclerotic metastases are by far the commonest cause , from prostatic & breast
2. osteopetrosis ( marble bone disease ) :it is a congenital disorder in which the
bones are densely sclerotic the bones are brittle and may fracture readily but also
healed easily
3.myelosclerosis , replacement of the bone marrow by fibrous tissue & lay down
of extratrabecular bone in patchy fashion , associated with spleenomegaly .
Alteration of the trabecular pattern & change in shape : occur in the following :
I-
Paget disease :
- It is usually a chance finding in an elderly patient .
- One or more bones may be affected, the usual site being the pelvis , spine , skull &
long bones , bone softening causes bowing & deformity of the bones with pathological
fracture may occur .
- Radiologically the affected bone showing thickening of the trabeculae and of the cortex
leading to loss of corticomudellary differentiation & increased bone density together
with enlargement of the affected bones
- In the skull there are many circumscribed areas of sclerosis scattered in the skull
vault giving mottled appearance ,
- the most important DX are metastases due to prostatic or breast carcinoma which
also occur in elderly but no bone expantion seen as with paget disease ,
- pagets disease may mimic tumor on radionuclide bone scans as well as on plain film .

Radiology L:2 د.نجالء
II.Haemolytic anemia :
Radiological bony changes are seen in two main types ( thalassaemia & sickle cell
disease ) & both show changes of marrow hyperplasia , but sickle cell disease can
also showing signs of bone infarction & infection .
These sings including :
1. Thinning of the cortex and resorption of some of the trabeculae with thickening &
stand out of that which are remain.
2. The skull showing widening of the diploe with perpendicular striation giving an
appearance known as hair –on-end .
3.Ribs may be enlarge and the phalanges may become rectangular.
4. infarction at bone ends causes flattening & sclerosis of the humeral and femoral
heads .
5. areas of bone destruction with periosteal new bone formation may be seen in the
shaft of long bones due to infarction .
III.Sarcoidosis :
- Occasionally involving the bones , the phalanges of the hands & feet are virtually the
only bones involved
- the sings are either small cyst or areas of destruction showing a lace – like pattern
, bony involvement usually associated with chest & skin sarcoidosis .

Radiology L:2 د.نجالء
Changes in bone shape :
- Occur in many form of congenital dysplasia , which all of them being rare , e.g of which is
diaphyseal aclasia : in the diaphyseal aclasia ( multiple exostoses ) there are multiple
bony projection known as osteochondromas or exostoses , they have cartilaginous cup
which may contain calcification ,
- when occur in the long bones they are near the metaphyses & directed away from the
joint , occasionally chondrosarcoma may develop in the cartilage cup .
Noor Rahman
