Fifth stage
PEDIATRICLec-4
د.اثل
1/11/2015
Celiac disease (Gluten Sensitive Enteropathy )is an immunemediated enteropathy caused by permanent sensitivity to gluten in genetically susceptible individuals
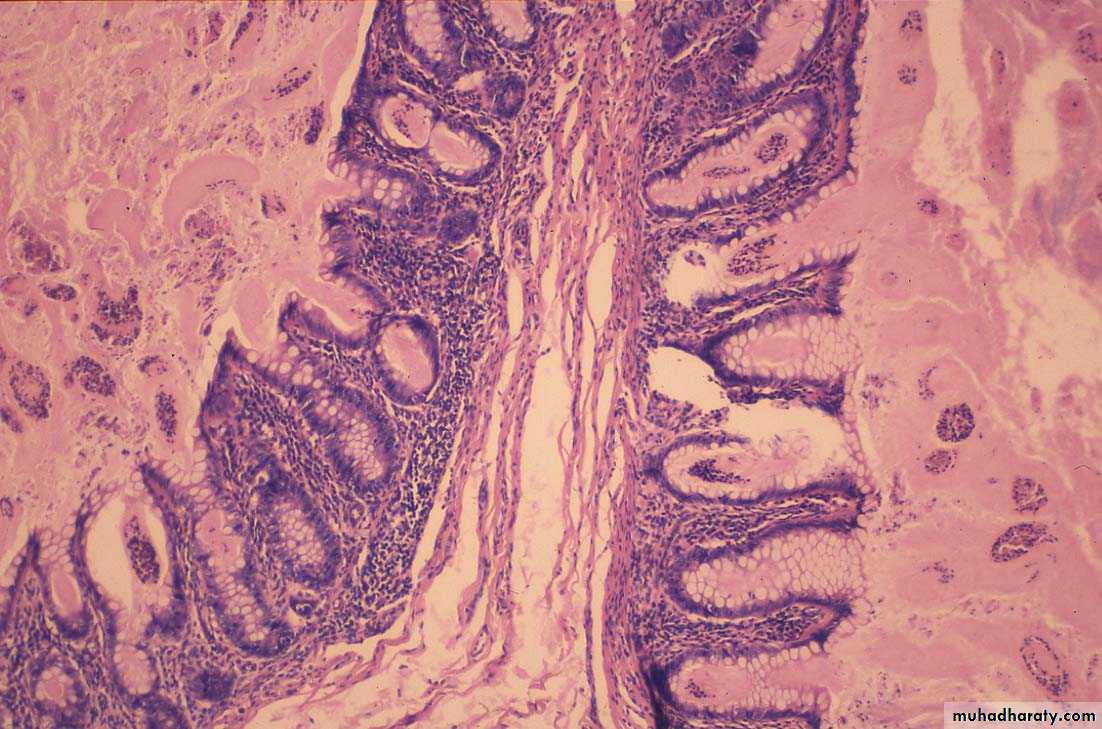
PATHOGENESISCeliac disease develops only afterdietary exposure to the proteingluten, which is found in wheat, rye,and barley. The activity of glutenresides in the gliadin fraction, thatlead to sensitization of laminapropria lymphocytes.• The inflammatory response results in villusatrophy, crypt hyperplasia, and damage to thesurface epithelium in the small bowel. The injury isgreatest in the proximal small bowel and extendsdistally for a variable distance.• Celiac disease results in a decrease in theabsorptive and digestive capacity of the smallintestinal surface area and a relative increase inimmature epithelial cells.
Genetic predisposition• Concordance in monozygotic twins approaching100%. Two to 5% of first-degree relatives havesymptomatic gluten-sensitive enteropathy, and asmany as 10% of first-degree relatives haveasymptomatic damage to small bowel mucosaconsistent with this disorder.• Celiac disease is associated with– (HLA) types (DQ8 and DQ2)– Down syndrome– Type 1 diabetes– Viruses
CLINICAL PRESENTATION
• The typical presentation of celiac disease (diarrhea,abdominal distention, & FTT) appear in toddler (6-24 mo.)after introduction of gliadin containing diet.• The stools are characteristically pale, loose, and offensive.• Neurologic symptoms do occur; many children areemotionally withdrawn, irritable, and fretful.• Other Manifestations: smooth tongue , oral ulcers,excessive bruising, finger clubbing, peripheraledemaNon-Intestinal Manifestations andAssociation of Celiac Disease• Osteopenia/osteoporosis• Short stature & delayed puberty• IDA not responding to oral iron therapy• Hepatitis• Arthritis• Epilepsy• Ataxia• Autoimmunity: DM1, thyroiditis, 1 ry biliarycirrhosis, addison disease & dermatitisherpetiformis• Syndromes: Turner, Down• MalignancyDIFFERENTIAL DIAGNOSISGIARDIASISMALNUTRITIONCOWS MILK PROTEIN ALLERGY
laboratory investAnaemia usually IDA but dimorphic anaemiamay occur.Hypoproteinaemia, hypoprothrombinaemia,↑fecal fat estimation
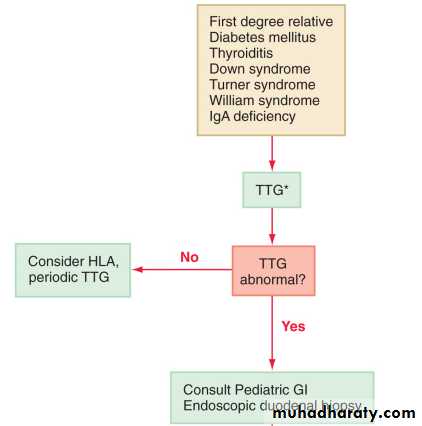
SCREENING AND DIAGNOSIS• Screening for celiac disease has beenrecommended for specific risk factors.• Serologic tests such as anti-endomysium IgAantibody test (EMA), anti-tissue transglutaminaseIgA antibody test (TTG), and HLA DQ2 or DQ8genotype testing are useful for evaluation ofasymptomatic subjects with diabetes mellitus,thyroiditis, Down syndrome, Turner syndrome,William syndrome, or IgA deficiency who have ahigher incidence of celiac disease, and first-degreerelatives of patients with celiac disease (CD).
Serologic tests
The anti-endomysium IgA antibody andanti-tissue transglutaminase IgA antibodytests are highly sensitive and specific inidentifying individuals with celiac disease.Some 10% of patients whose disease isdiagnosed earlier than 2 yr of age showabsence of IgA anti-TG2. For them, themeasurement of serum antigliadin antibodies isgenerally advised. Antibodies against gliadinderived deamidated peptides (D-AGA) have been assessed. Compared with conventionalAGA, the peptide antibodies (IgG and IgA) have a greater sensitivity and specificity. A problem with serology is represented by theassociation of celiac disease with IgA deficiency (10-fold increase compared to the general population). Serum IgA should alwaysbe checked, and in the case of IgA deficiency,D-AGA, IgG anti-endomysium, or TG2 shouldbe sought. Negative serology should not preclude abiopsy examination when the clinical suspicion is strongGenetic tests
have an increasing role in thediagnosis. Less than 2% of celiac patients lackboth HLA specificities; at the same time,approximately one third of the “normal”population has one or the other marker; thatmeans that the measurement of HLA DQ2and/or DQ8 has a strong negative predictivevalue but a very weak positive predictive valuefor the diagnosis of celiac disease.
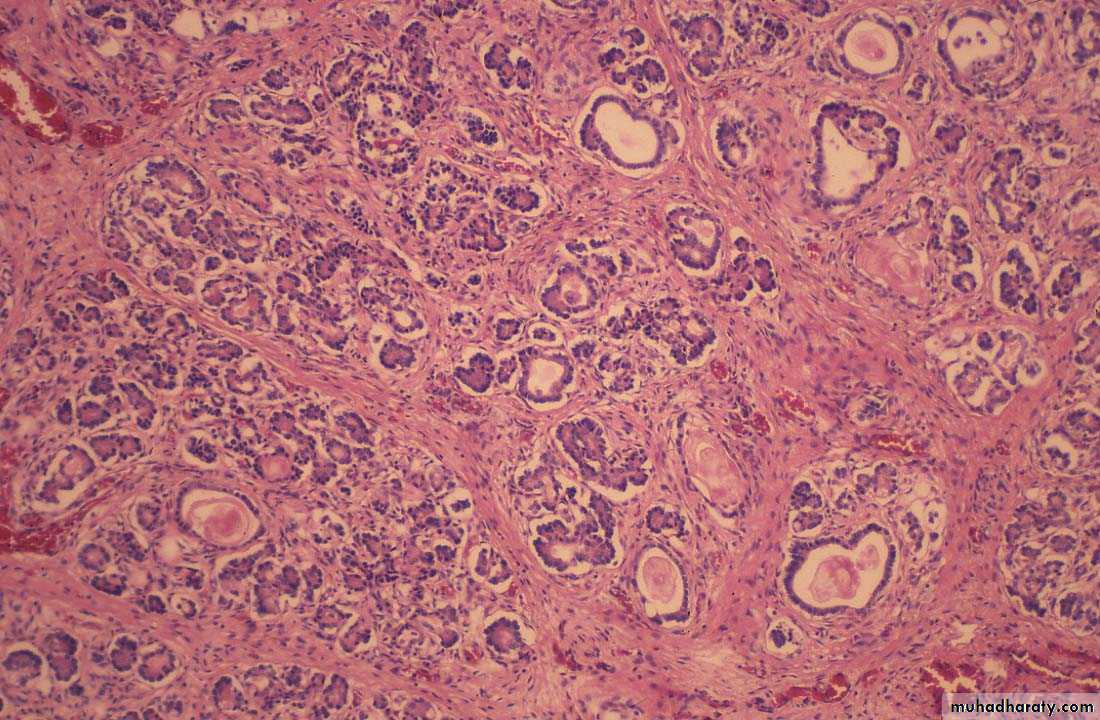
Small Intestinal Biopsy• Definitive diagnosis of celiac disease requiressmall intestinal biopsy, as none of the availableserologic tests are 100% reliable .• The characteristic histologic changes includepartial or total villous atrophy, crypt elongationand decreased villous/crypt ratio, increasednumber of intraepithelial lymphocytes .• The mucosal involvement can be patchy, somultiple biopsies must be obtained.ESPGHAN current criteria,The 2 requirements mandatory for thediagnosis of celiac disease are:– characteristic histologic features +– full clinical remission after withdrawal ofgluten from the dietReversal of positive serologic tests aftergluten withdrawal is considered supportiveevidence .• In children <2 yr of age, milk protein–sensitiveenteropathy can produce changes similar to celiacdisease; confirmation of diagnosis after a glutenchallenge is sometimes required. This necessitatesthree biopsies: an initial biopsy at presentation, the2nd to document healing with gluten withdrawal, andthe 3rd to show recurrent damage with reintroductionof gluten.• Gluten challenge is not considered mandatoryexcept in situations where there is doubt about theinitial diagnosis
TREATMENT• The only treatment for celiac disease is lifelongexclusion of gluten. This requires a wheat-,barley-, and rye-free diet.• After gluten withdrawal, there is rapid remissionof symptoms, improved bone mineralization,and reversal of growth failure and nutritionaldeficiencies.• It is recommended that children with celiacdisease be monitored with periodic visits forassessment of symptoms, growth, physicalexamination, and adherence to the gluten-freediet.
PROGNOSIS• The clinical response to a gluten-free dietusually results in improvement of mood,appetite, and lessening of the diarrhea within aweek. Reduced bone mineral density alsoimproves with gluten exclusion. No long-termcomplications from a gluten-free diet have beenrecognized.• Celiac disease is associated with intestinallymphoma and other forms of cancer, especiallyadenocarcinoma of the small intestine, of thepharynx, and of the esophagus.• Several follow-up studies suggest that a gluten-freediet protects from cancer development, especially ifstarted in the 1st years of life. Therefore, earlydiagnosis and strict dietary restrictions appear to bethe only possibility of preventing risk for rare but veryaggressive forms of cancer associated with celiacdisease.CYSTIC FIBROSIS• A multisystem disease• Autosomal recessive inheritance• Commonest lethal genetic conditionaffecting Caucasian people.• DEFECT IN CHLORIDE TRANSPORT INEPITHELIAL TISSUE . This result inrelative dehydration of airway secretions.
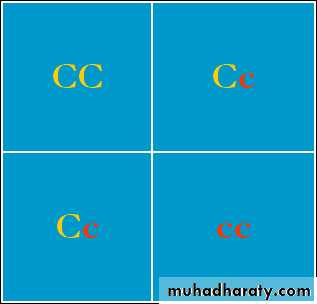
GENETICS• CF is inherited as an autosomal recessive trait.Let C= normal CFTRLet c= mutant CFTR
If mom and dad are both carriers then:
C c
With mom and dadcarriers, then:50% chance of havingchild who is a carrier25% chance of childbeing affected25% of child with nomutant copies of CFTR
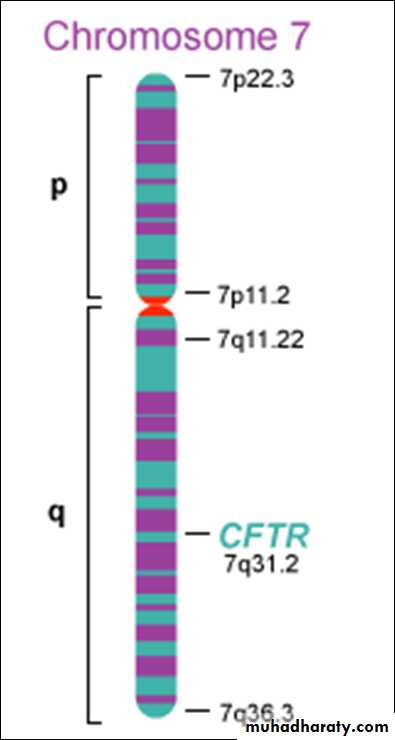
GENETICS• The CF gene codes for a protein of 1,480 aminoacids called the CF transmembrane regulator(CFTR). CFTR is expressed largely in epithelialcells of airways, the gastrointestinal tract(including the pancreas and biliary system), thesweat glands, and the genitourinary system.
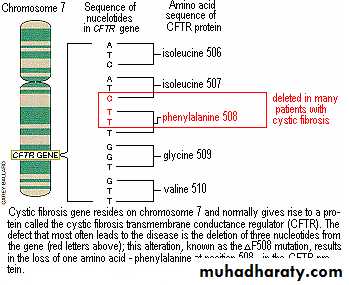
Cystic fibrosis transmembraneconductance regulator (CFTR) gene The most comm CFTR gene islocated on the long arm ofchromosome 7. There are >1500 mutations inCFTR. Commonest mutation is Δ F508---70% CF alleles in caucasians(deletion of a single phenylalanineresidue at amino acid 508 )
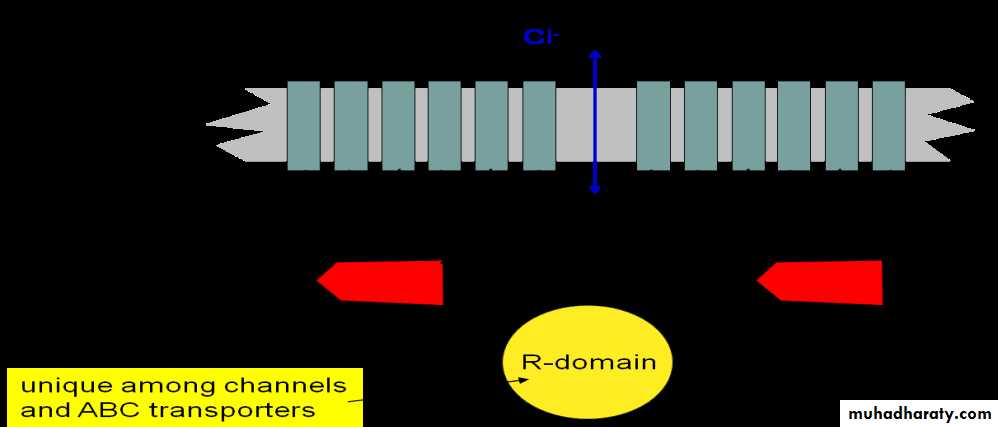
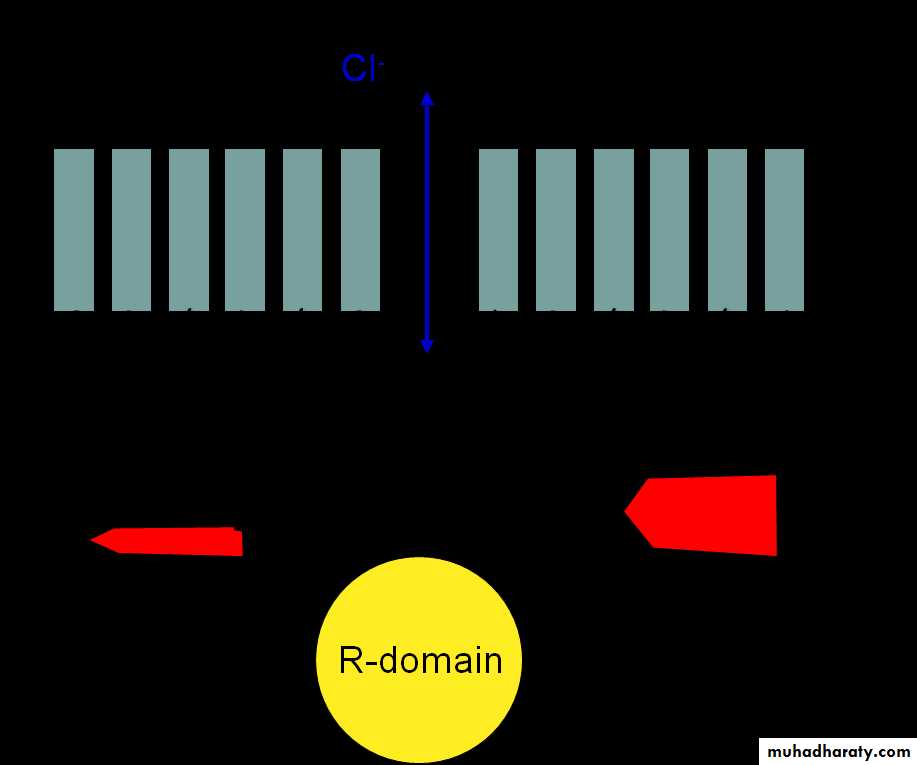
Cystic Fibrosis TransmembraneConductance Regulator (CFTR)• A Cl- channel• 2 sets of 6 transmembrane domains• 2 “ATP-binding cassettes” (thus “ABC transport protein”)ATPATP
What’s wrong with DF508?The most common mutation (70% ofmutants): A phenylalanine (F) isdeleted at position 508in ATP-binding cassette #1
PATHOGENESIS• Four long-standing observations are offundamental pathophysiologic importance:failure to clear mucous secretionsa paucity of water in mucous secretionsan elevated salt content of sweat and otherserous secretionschronic infection limited to the respiratory tract.
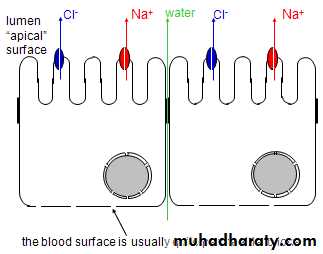
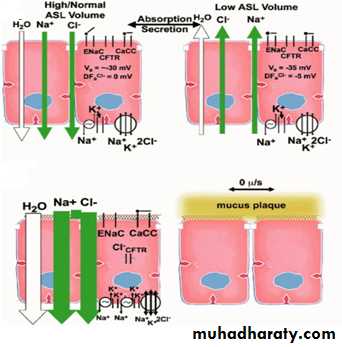
CFTR helps to control bulk water flow across epithelia1. Na+ channels are usuallyopen, but extensive Na+flux requires a counterion.2. If CFTR is open, Clbecomes the counterion.Therefore NaCl flowsacross the membrane.3. Water then flows aroundthe cells to maintainosmotic pressure.4. Result: isotonic NaClsolution flows from theblood to the lumen (orvice-versa)
CFTR and Airway Surface Liquid
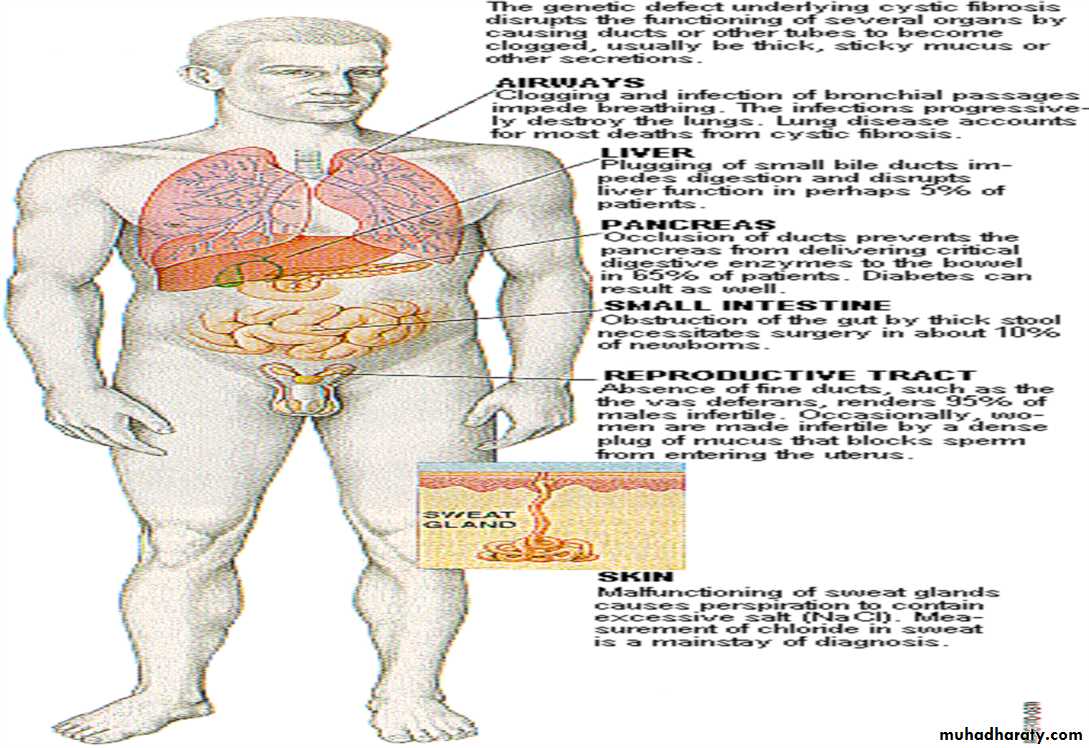
Clinical features of Cystic FibrosisChronic Sino-Pulmonary DiseaseNutritional deficiency/GI abnormalityObstructive AzoospermiaElectrolyte abnormalityCF in a first degree relative
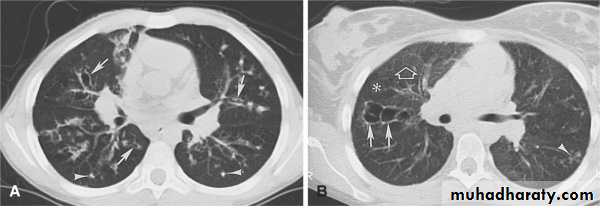
Bronchiectasis
Mucous in the airways cannot be easily cleared fromthe lungs
Nasal PolypsDigital ClubbingSchamroth sign +v
Colon Sticky mucus secretion
Pancreas Ducts are filled with sticky mucus. Scaring of tissue.
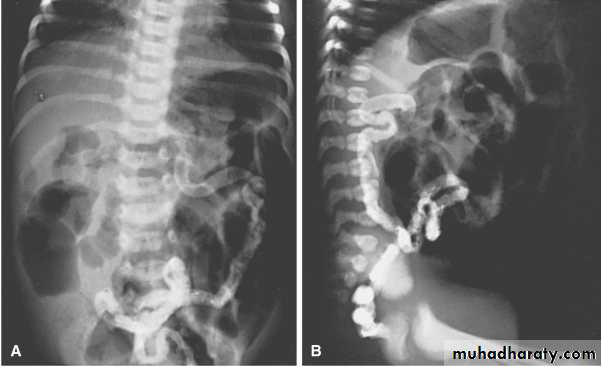
Meconium ileus
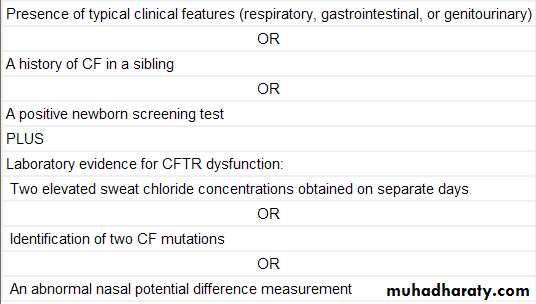
Diagnostic MethodsSweat chloride• Chemical that stimulates sweating placed under electrodepad; saline under other electrode pad on arm• Mild electric current is passed between electrodes• Sweat collected Positive Sweat chloride:> 60 meq/L
Genetic testingDNA Testing for most common CFTR mutationsOther Diagnostic Tests
• increased potential differences acrossnasal epithelium• Prenatal diagnosis is possible byAmniotic fluid or Chorionic villoussampling• Newborn Screening for CF:– Immunoreactive trypsinogen usually firstfollowed by either sweat or DNA testing
Diagnostic Criteria for CysticFibrosis
TREATMENTMultidisciplinary• Pulmonary Therapy.• Infection• Nutrition• Gastrointestinal• Infertility• Social IssuesNutrition• High calorie supplemental• Vitamin supplementation• Pancreatic enzymes