
SERONEGATIVE SPONDARTHRITIS 1
Assistant Professor Dr. Khudair Al-Bedri
Consultant Rheumatology &Consultant
Internal Medicine.

Learning objectives
1. Definition of seronegative spondarthritis
2. Classification
3. Common features
4. AS: definition, epidemiology, etiology,
pathogenesis, C/F, DDx
5. Modified New York criteria for AS
6. ASAS Criteria
7. Ix, Rx , and prognosis of As
8. Quiz

Definition
Seronegative spondarthritis are group of
inflammatory joint diseases that share
distinctive clinical, radiographic and genetic
features.
They all have a strong association with Human
leukocyte antigen (HLA)-B27.

Classification
Ankylosing
Spondylitits
Psoriatic
Arthritis
Undifferentiated
SpA
Reactive
Arthritis
Enteropathic
Arthritis
Enthesitis-
Related JIA

Clinical Features 1
1) Familial aggregation.
2) Seronegative RF.
3) Asymmetrical inflammatory
oligoarthritis (lower>upper limbs) &
episodic.
4) Inflammatory sacroiliitis &
spondylitis.
5) Inflammatory enthesitis.
6) Absence of nodules & other extra
articular features of RA.
AS
ReA
Enteropathic
Arthritis
PsA
Clinical features
common to all
seronegative
spondarthritis

Spondarthritis
& HLA-B27
Disease
Approximate
prevalence
of HLA-B27
Ankylosing spondylitis (AS)
90 %
Reactive arthritis (ReA)
40-80%
Juvenile spondyloarthropathy
70%
Enteropathic spondyloarthropathy
35-75%
Psoriatic arthritis
40-50%
Undifferentiated spondyloarthropathy
70%
HLA-B27 is an
HLA Class I
molecule
found in 8% of
healthy white
caucasians
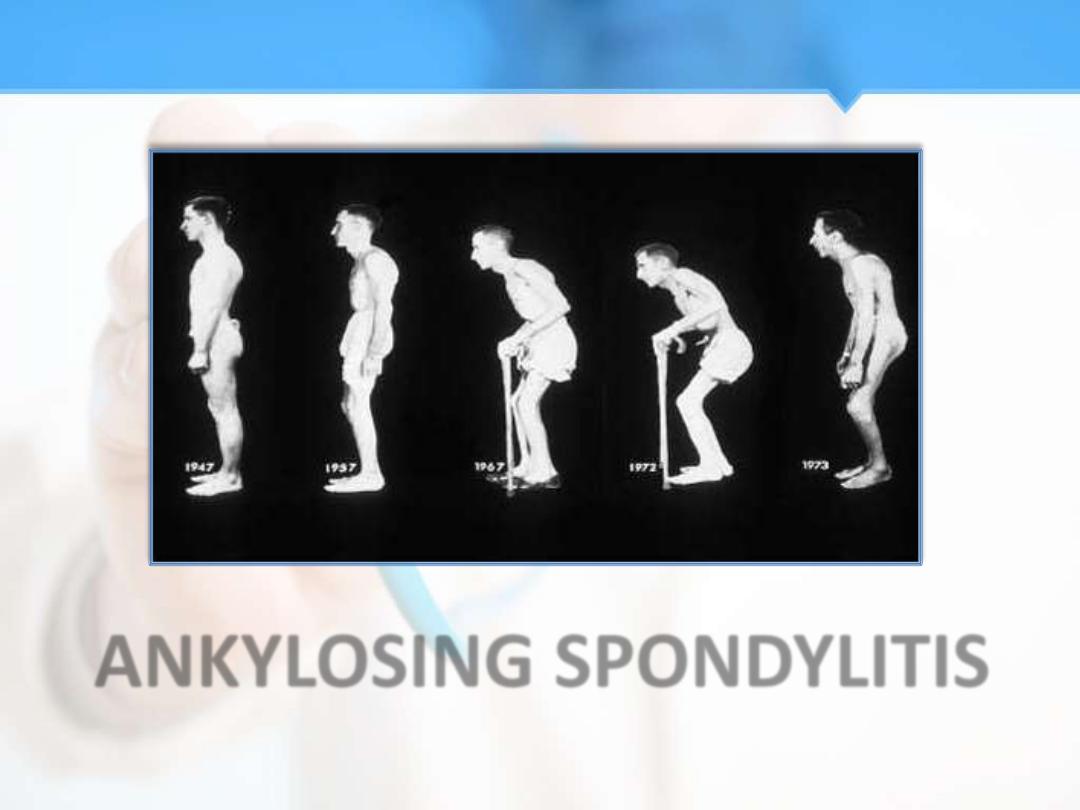
ANKYLOSING SPONDYLITIS
Nomenclature
The term ankylosing spondylitis is derived
from the Greek roots ankylos, or “bent”
(although it now usually implies fusion or
adhesions), and spondylos, or “vertebral disk”

Definition
It is a chronic inflammatory disease of the
sacroiliac joints & spine as well as extra-spinal
lesions involving the eye, bowel & heart.
Epidemiology
•
Ranges from 1-6% across different populations.
•
The peak onset is in the 2nd &3rd decades.
•
Male to female ratio is 3:1.

Etiology
Genetic
•
Human leukocyte antigen (HLA)-B27 is a strong
genetic risk factor for .
•
90% persons of affected persons in Europe are HLA
B 27+ve.
Environmental
•
Infective triggers have not clearly been linked to
cause AS.
•
Increased fecal carriage of Klebsiella aerogenes
was found in AS.
Immunological

Role of HLA B27 in Pathogenesis
4 Theories:
•
The arthritogenic peptide hypothesis: HLA-B27
binds a unique set of antigenic peptides, bacterial or
self
activate cytotoxic T-cell
arthritis
•
Self-association of the HLA-B27 molecule: HLA-B27
binds to itself
homodimers
intracellular stress
activation of immune system
•
Alteration of intracellular handling of microbes due
to HLA-B27: e.g.; Salmonella
cytokines
•
Recognition of HLA-B27 as an autoantigen: HLA-B27
presented by APC to T-helper lymphocyte

Role of HLA-B27
• 1-The chance of developing AS if one have
HAL-B27 positive is 1-5% and this increasing to
15-20% in case of an affect first degree
relative.
• 2- HLA-B27 positive 90% in AS and it is not
diagnostic (since 8% of healthy individual
positive of HLA-B27).
• HLA-B27 not mandatary in clinical assessment
but helpful in ASAS criteria.

Role of Cytokines in Pathogenesis
•
TNF alpha, interferon gamma and IL-6, 17 & 23 play a
role in pathogenesis of AS
•
Their role is not fully understood yet.
•
TNF-α and IFN-ɣ are potent antibacterial Th1
cytokines, in AS patients ? delayed elimination of
bacteria.
•
Abnormal IL-23 and its receprtor (IL-23R) was
detected in AS patients.
•
Higher serum levels of IL-6 were demonstrated in
patients with active AS.

Clinical Features 1
•
Spinal features of AS seldom appear before
age 16-18 years.
•
Inflammatory backache 75% (presenting ):
insidious in onset, persist for >3/12, worsened
by rest & improved by exercise & night pain is
frequent.
•
Sacroiliitis is the most common initial feature,
causes pain in buttocks, radiates sometimes to
thighs but never below knees.

Clinical Features 2
•
Planter fasciitis with heel pain, achilles
tendonitis & tenderness over bony
prominences as iliac crest reflecting
enthesopathy.
•
Fatigue is common.
•
Peripheral arthritis in 40% of AS patients.
•
10% of AS cases have peripheral arthritis
preceding spinal symptoms.

Clinical Features 3
Synovitis in AS:
Peripheral oligoarthritis, episodic &
asymmetrical.
•
Lower limbs > upper limbs.
•
Temporomandibular joints may be affected.
•
Dactylitis may lead to pain at one toe or more
toes lasting many months but usually resolve
spontaneously.
•
Enthesitis is hallmark of SPA .

Clinical Features 4
Enthesitis
(Achillis
tendinitis)
Dactylitis
Peripheral
arthritis
(Synovitis)

Clinical Features 5
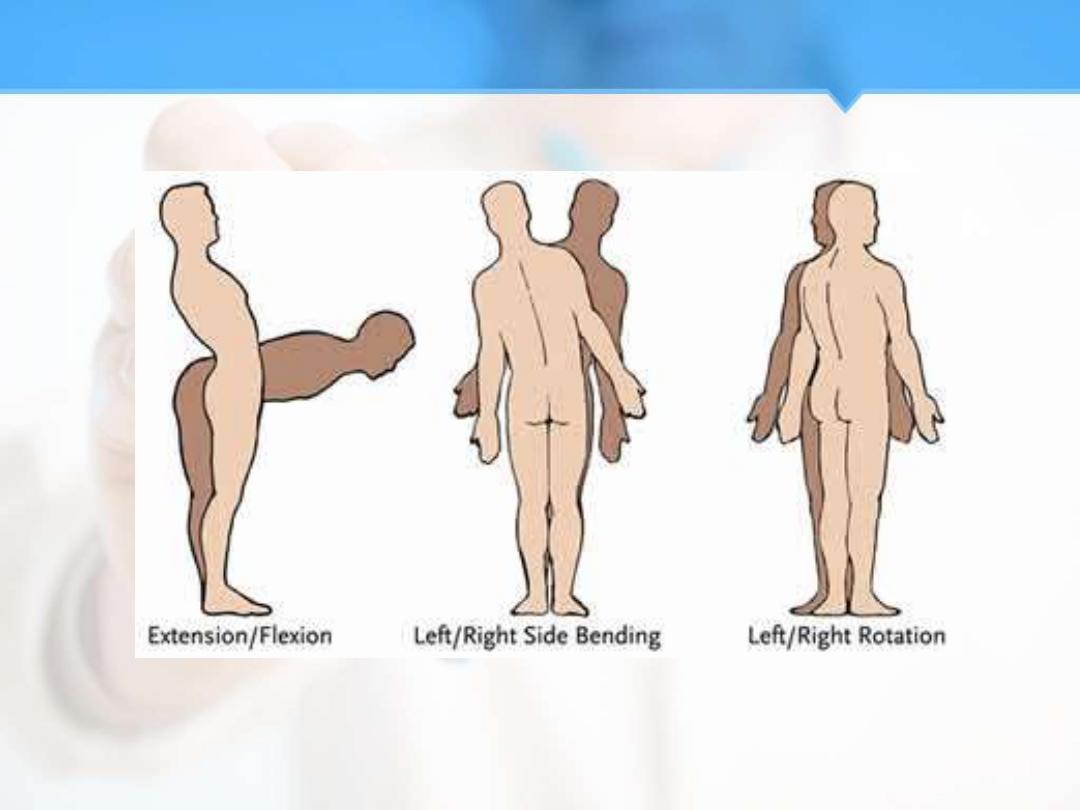
Early physical signs include:
1.
Restriction of lumbar spine movement:
lateral rotation 1
st
, then progression to all
directions.
2.
Pain on sacroiliac compression.
3.
Failure to obliterate the lumbar lordosis on
forward flexion.
Clinical Features 6

Clinical Features 7
Late physical signs include:
1.
Increased stiffness throughout the spine.
2.
Restriction of chest expansion.
3.
Few patients may develop marked kyphosis
of dorsal & cervical spine.

Clinical Features 8

Modified New York criteria for AS
1.
Low backache at least 3/12 duration
improved by exercise & not relieved by rest.
2.
Limitation of lumbar spine motion in sagittal
& frontal planes.
3.
Chest expansion decrease.
4.a
Unilateral sacroiliitis grade 3-4.
4.b
Bilateral sacroiliitis grade 2-4.
Definite diagnosis: if 4a or 4b + any clinical
criterion of 1-3

ASAS Criteria
1- Possible diagnosis AS pre-radiographic.
2- Diagnosis of AS is still even when negative
MRI for sacroiliac joint with HAL-B27 positive
with two SPA features .
3- IN ASAS criteria that inflammatory backache
no longer a compulsory .
4- Diagnosis of AS is unlikely in the negative
image and a negative HLA-B27.

Clinical Features 9
Extra articular manifestations:
1.
Acute anterior uveitis 25%.
2.
Conjunctivitis 20%.
3.
Prostatitis (usually asymptomatic) 80%.
4.
AR, MR, pericarditis, conduction defect.
5.
Amyloidosis.
6.
Apical fibrosis in the lungs.
7.
IBD (subclinical 60%, overt 15%).

Differential Diagnosis
1.
Prolapsed intervertebral disc
*
.
2.
Fibromyalgia.
3.
Infection in the spinal or sacroiliac joints e.g.; TB,
Brucellosis
*
.
4.
Spinal tumors e.g.; chondroma, ependyoma.
5.
Bone tumors e.g.; osteoid, plasma cytoma,
secondary carcinoma, leukemic infiltration
*
.
6.
Metabolic bone disease e.g.; osteomalacia,
hypophosphatemic rickets.
7.
Diffuse interstitial spinal hyperostosis (DISH,
Forrestier's disease)
*
.

Delayed Diagnosis? 1
•
Low awareness of AS among non-
rheumatologists [AS is a rare cause of a
common complaint (backache)]
•
NY modified criteria Need for radiographic
sacroilliitis to diagnose definite AS while X-rays
are normal or equivocal in early disease
•
Absence of pathognomonic C/F or lab test
•
Underestimation of women with AS
•
Negative HLA-B27 in ~10% of AS patients
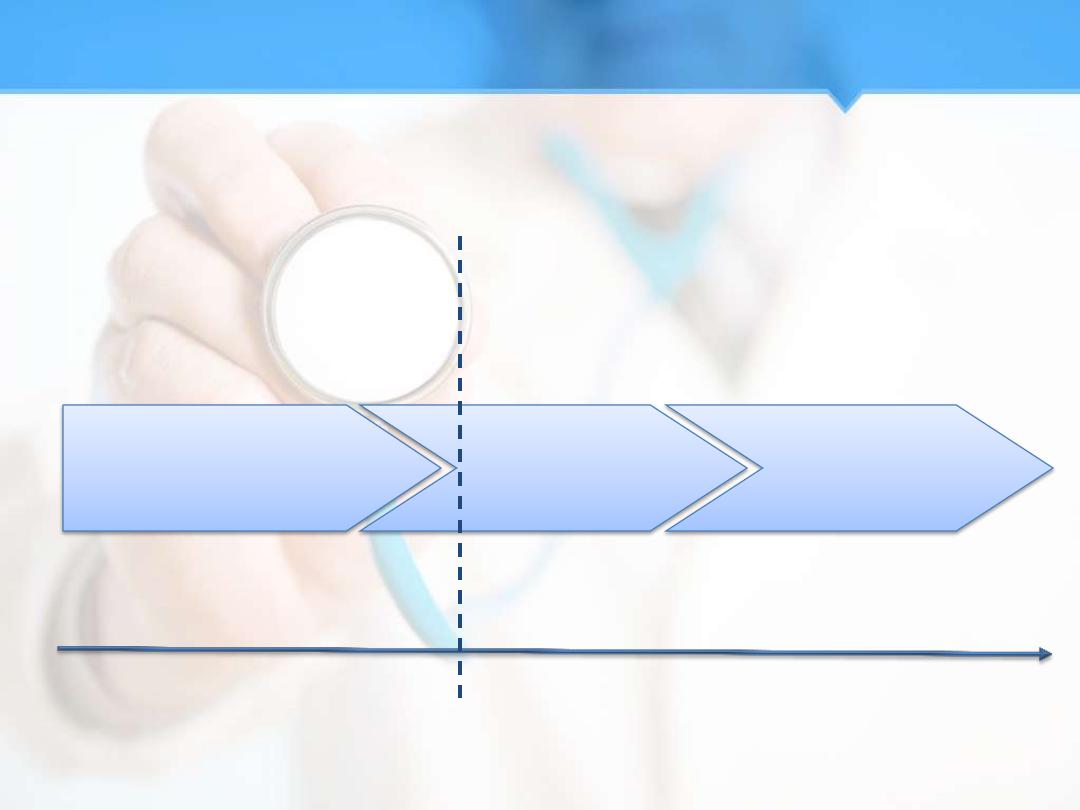
Time (years)
Back pain
IBP
MRI active sacroiliitis
Back Pain
Syndesmophytes
Radiographic stage
Pre-radiographic stage
(Axial undifferentiated SpA)
Back Pain
Radiographic
sacroiliitis
Modified NY criteria (1984)
Delayed Diagnosis? 2

Investigations
1.
ESR & CRP are usually raised.
2.
RF is –ve.
3.
Radiographic signs:
i.
Sacroiliitis is the 1st abnormality: starts in lower
synovial parts of the joints.
ii.
Anterior squaring of the vertebrae in lateral views of
thoracolumbar spine.
iii.
Bridging syndesmophytes.
iv.
Ossification at antero-longitudinal ligament with
bamboo spine formation.
v.
Osteoporosis & atlanto-axial dislocation can occur.

Imaging 1
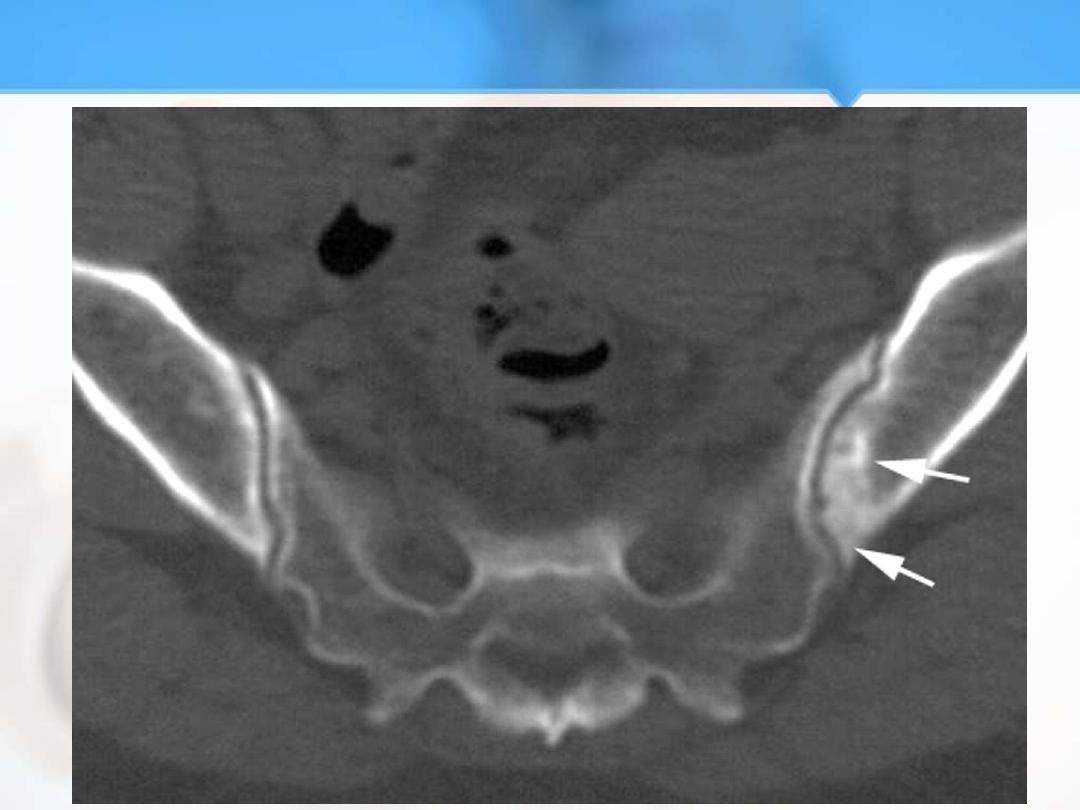
Imaging 2

Imaging 3
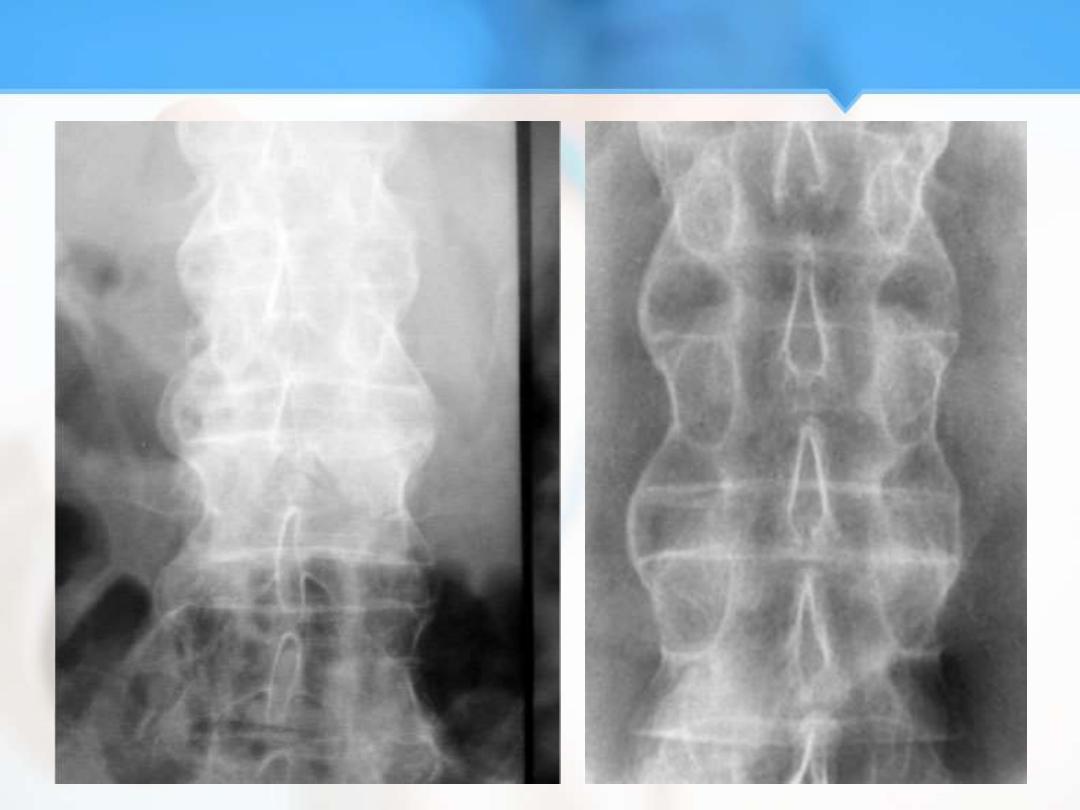
Imaging 4

Imaging 5
Imaging 6

Treatment 1
The aim is to relieve pain & stiffness while
maintaining skeletal mobility & avoiding
deformity.
Education & appropriate physical activity are
the corner stones of management.
Regular daily back extension exercises.
Avoid poor bed & chair posture.
NSAIDs to symptoms especially stiffness but
they do not alter the natural course of the
disease.

Treatment 2
Sulfasalazine with /without Methotrexate may
be effective for peripheral joints synovitis but
not useful for axial disease.
Local steroid injection for planter fasciitis &
enthesopathy.
Oral steroid for anterior uveitis.
Biologic agents (TNF alpha blockers):
Etanercept.
Infliximab.
Adalimumab.

Surgical Intervention
• 1-Total hip replacement ,1/3 of long standing
AS after 10 years ,5% need total replacement.
• 2- Fusion to prevent instability of the spine .
• 3- Atlanto – axial& Atlanto occiputal
subluxation and spinal canal stenosis.
TNF blockers
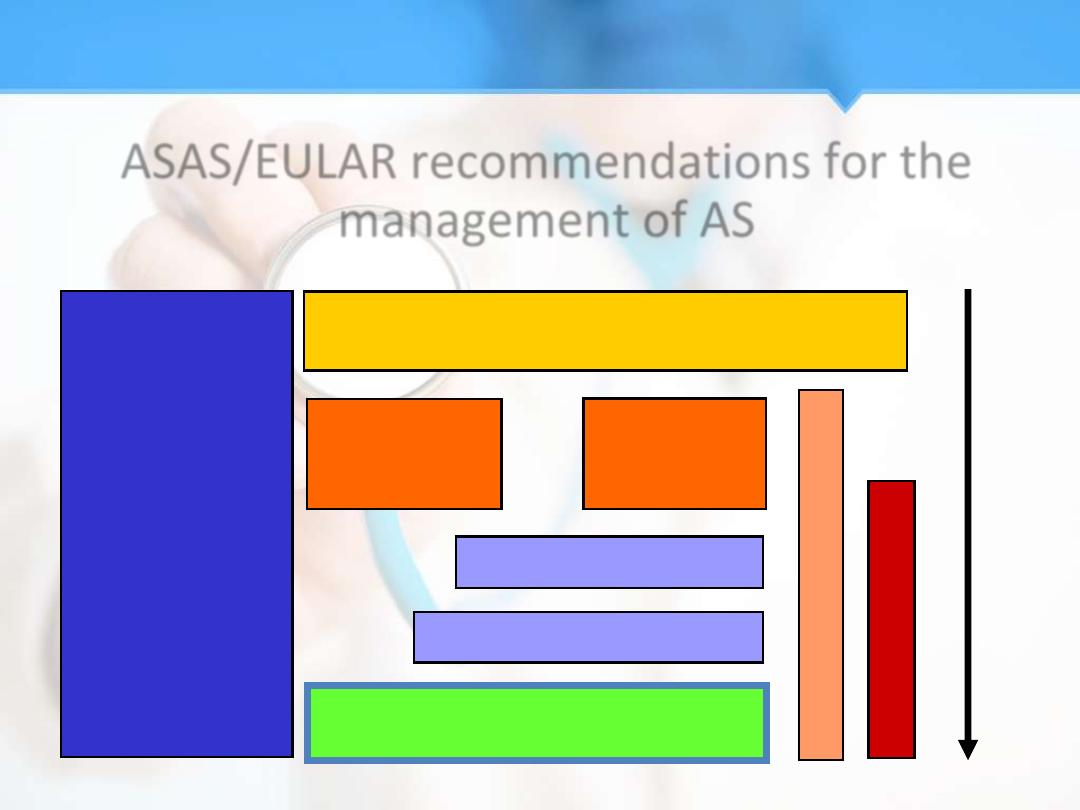
ASAS/EULAR recommendations for the
management of AS
Education,
exercise,
physical
therapy,
rehabilitation,
patient
associations,
self-help
groups
Non steroidal anti inflammatory drugs
(NSAIDs)
Peripheral
Disease
Axial
Disease
Sulfasalazine (SSZ)
A
n
a
l
g
e
s
i
c
s
Local corticosteroids
S
u
r
g
e
r
y
D
I
S
E
A
S
E
P
R
O
G
R
E
S
S
I
O
N
Treatment 3

Prognosis
AS patients have decreased life expectancy due
to:
1.
Amyloidosis.
2.
Malignancy with multiple courses of
radiotherapy.
3.
Aortic valve disease.
4.
Traumatic spinal fractures.
5.
Risk of drugs & surgical procedures.
6.
Associated diseases e.g.; IBD.
7.
Increased risk of atherosclerosis IHD.

Note
• In contrast to RA,
pregnancy does not
improve the
symptoms of AS.
• In the majority of
patients disease
activity is not
substantially altered
during pregnancy.
REACTIVE ARTHRITIS

Reactive arthritis
• Reactive arthritis is an acute aseptic arthritis
that develops in response to an extra –
articular infection ,typically originatingfrom
gastrointestinal or genitourinary tract.
• It is aseronegative spondyloathropathy
classically presenting with asymmetrical
oligoarthritis, usually in the lower limbs.

Pathophysiology
• Reactive arthritis is thought to be caused by
an infectious trigger usually a bacterial GI or
GU infection in genetically individuals.
• This leads to immune activation and cross-
reactivity with self-antigens causing acute
inflammation in the affected joint and other
tissues approximately 2-6 weeks after the
initial infection.
• GI infection (Salmonella ,Yersinia, Shigella and
Campylobacter ).
• GU infection (Chlamydia).

Pathophysiology
• As well as inflammation of joints
,inflammation of entheses,axial
skeleton,skin,mucous membranes ,GI tract
and eyes may also occur.
• HLA-B27 is positive in most patients and its
not only a strong risk factor of reactive
arthritis , but it may also predict the severity
and chronicity of the disease.
20% of HLA-B27 positive men will develop Reactive
Arthritis if they are exposed to an epidemic of Shigella
dysentery.
Risk factors for reactive arthritis.
Reactive arthritis occurs after exposure to
certain GI or GU infections.
GI/GU infection
There is a 9:1 male : female incidence ratio
of Chlamydia –induced reactive arthritis and
1:1 for post-dysentery reactive arthritis.
Gender
HLA-B27 is positive in approximately 75% of
reactive arthritis patients .
HLA-B27
Most patients with reactive arthritis are
aged 20-40 .
Age
Reactive arthritis is more common in
Caucasians.
Ethnicity

ReA, Clinical Features 1
• Reactive Arthritis characteristically involves
the lower limbs with asymmetrical
oligoarthritis, the pattern may be additive.
• Hip disease is uncommon.
• Exclusive upper extremities involvement is
extremely rare.
• Dactylitis pattern in the feet is uncommon.
• Arthritis is sterile synovitis.

ReA, Clinical Features 2
• Enthesitis is a characteristic of Reactive
Arthritis, Achilles‘ tendonitis and plantar
fasciitis are most common sites of
involvement, but pain in the iliac crest and
ischial tuberosities is also detected.
• Low back pain and buttock pain reflecting
sacroiliitis occurs in up to 50%, but
progression to AS is an uncommon and late
event & it is strongly associated with HLA-B27.

Clinical Features3
• Lower back pain due to sacroiliitis and
spondylitis.
• Reiter’s syndrome –triad of reactive arthritis ,
conjunctivitis and urethritis .Although rare, it
follows a GU or GI infection .

ReA, Extra-atricular Features 1
Extra-articular features can be helpful in
establishing the diagnosis particularly in
circumstances when it is difficult to identify a
triggering infection.
•
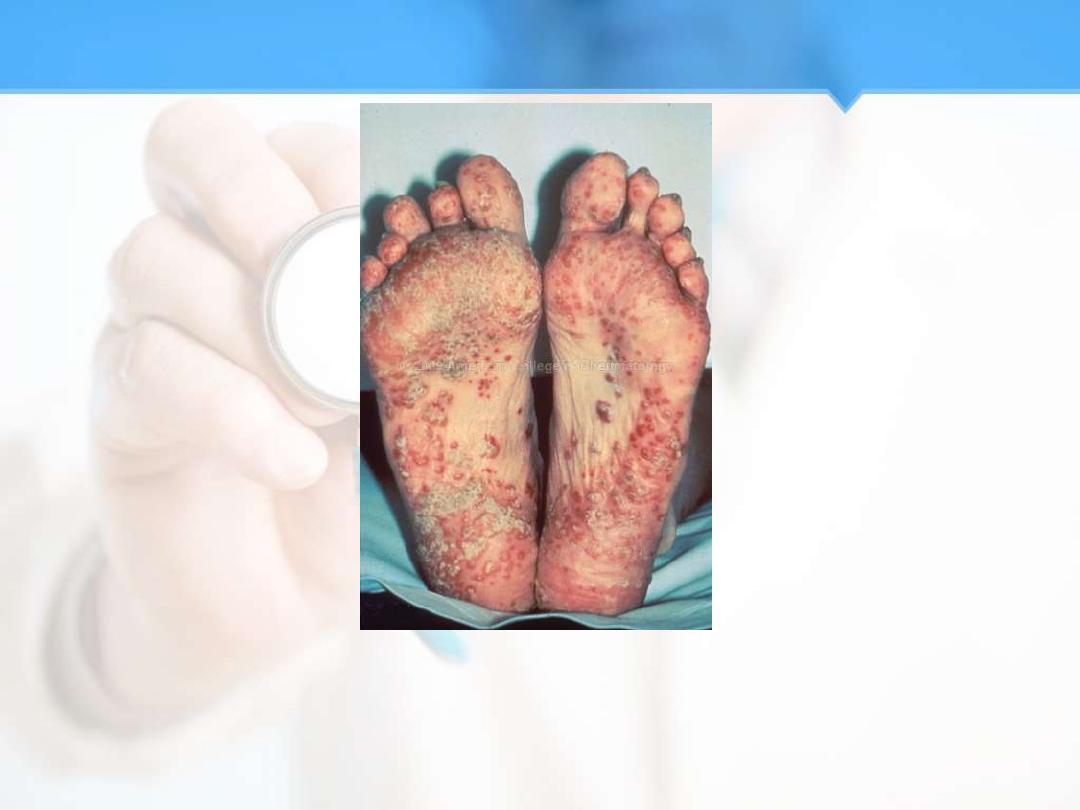
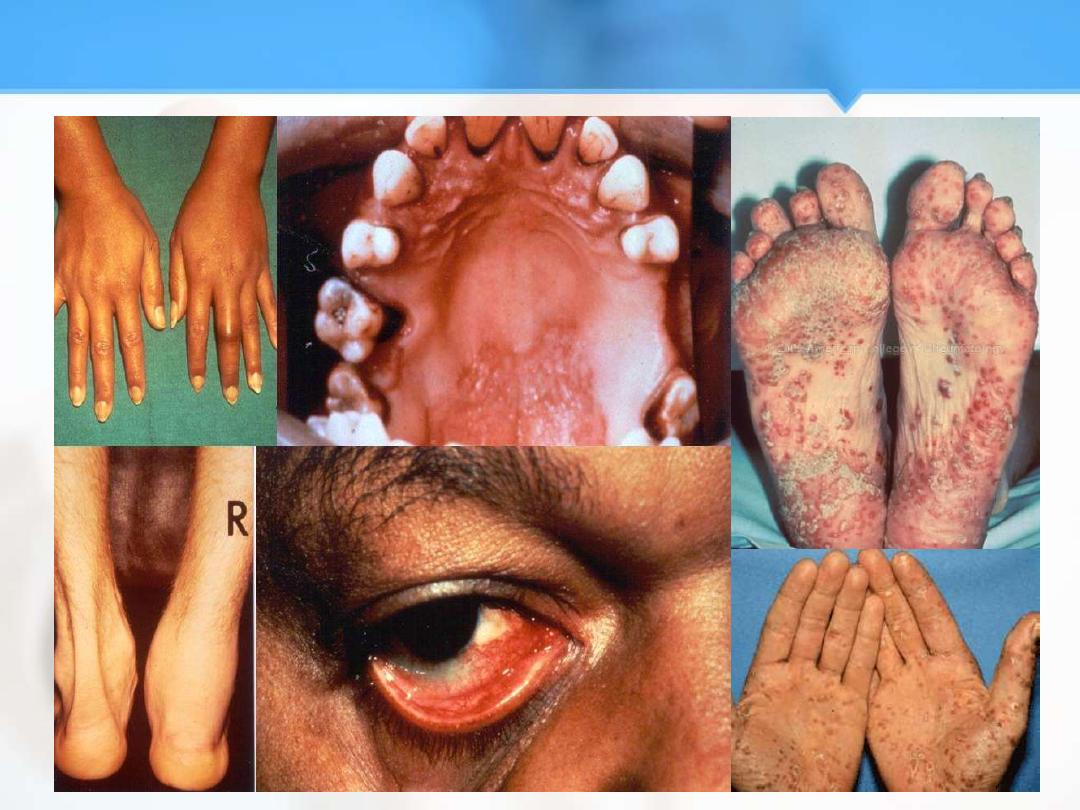
Keratoderma blenorrhagicum (15%) is
papulosequamous rash most commonly
affecting the palms and soles. The lesions can
be indistinguishable clinically and
histopathologically from pustular psoriasis.

ReA, Extra-atricular Features 2
•
Nail dystrophy can occur with ReA (Reactive Arthritis),
further highlightening the clinical overlap of some features
with PsA.
•
Circinate balanitis occurs in (20-50%) of patients and is
usually painless.
•
Buccal erosions occurs in (10%) and are usually painless red
patches.
•
Oral ulcers on the hard palate or tongue, typically painless.
•
Dysuria and pyuria present clinical features of urethritis.
•
Acute anterior uveitis occurs in 20% of ReA patients,
•
And usually unilateral .
•
Conjunctivitis usually bilateral.
ReA, Clinical Features 3

ReA, Uncommon Complications
•
Aortic Incompetence.
•
Conductive Defect.
•
Pleuro-pericarditis.
•
Peripheral Neuropathy.
•
Seizures.
•
Amyloidosis.

ReA, Investigations
•
ESR and CRP are raised.
•
RF and ANA are negative.
•
Normochromic normocytic anaemia.
•
Sterile and inflammatory synovitis.
•
Stool culture.
•
Urine culture.
•
Urethral culture.
•
High vaginal swab.
•
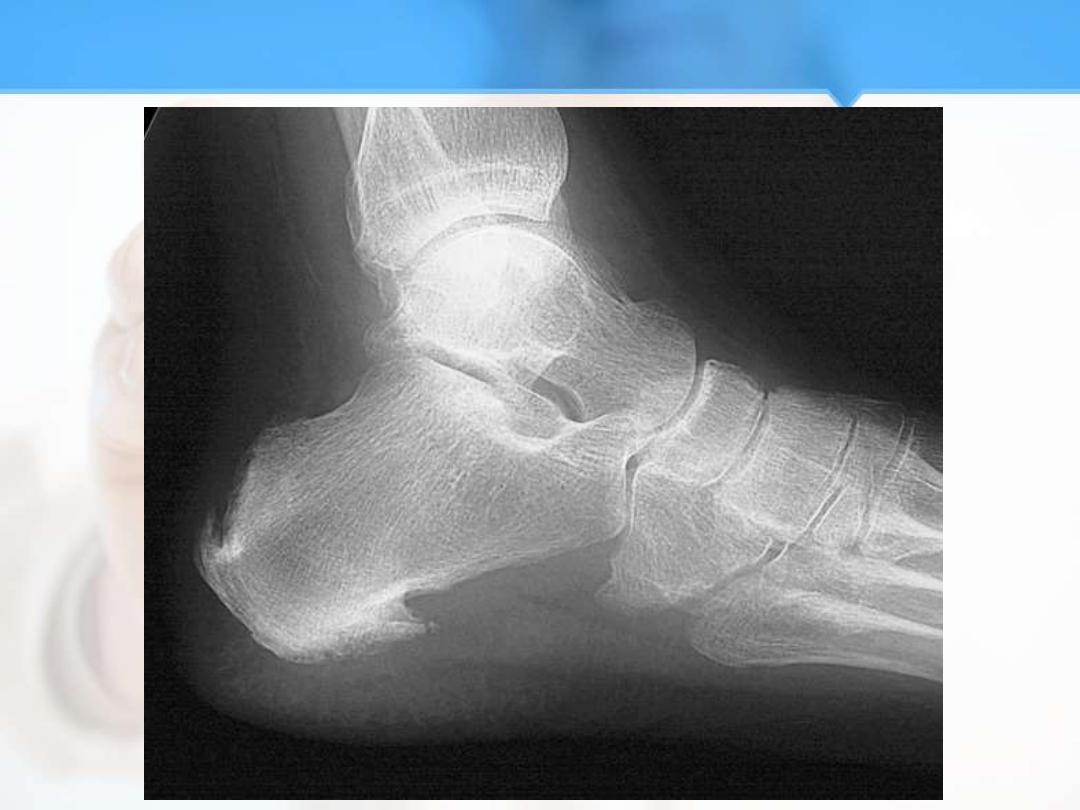
Radiological, the most important findings are:
–
Fluffy calcaneal spur.
–
Asymmetrical and unilateral sacroiliac joint involvement.

ReA, Treatment
•
NSAIDS.
•
Local and intra-articular steroid injection.
•
Topical and systemic steroids for anterior
uveitis.
•
ReA after 4/52 of treatment without
improvement (persistent synovitis):
Sulfasalazine and Mehtotrexate are used.
•
Antibiotics for infections.
•
Anti-TNF-a therapy.

ReA, Prognosis
•
The first attack of arthritis is self-limiting with
spontaneous remission within 2-4/12 of onset,
representing (60%) of patients.
•
15% of patients of ReA relapse.
•
15% of patients of ReA continue to a chronic
state.
•
10% of patients develop ankylosing
spondylosis.
•
Mortality in ReA results from cardiac
complications and amyloidosis.

THANK YOU



