1
Dr.SHATHA AL-KAWAZ
PEDIATRIC SURGERY
Abdominal wall defects in neonate
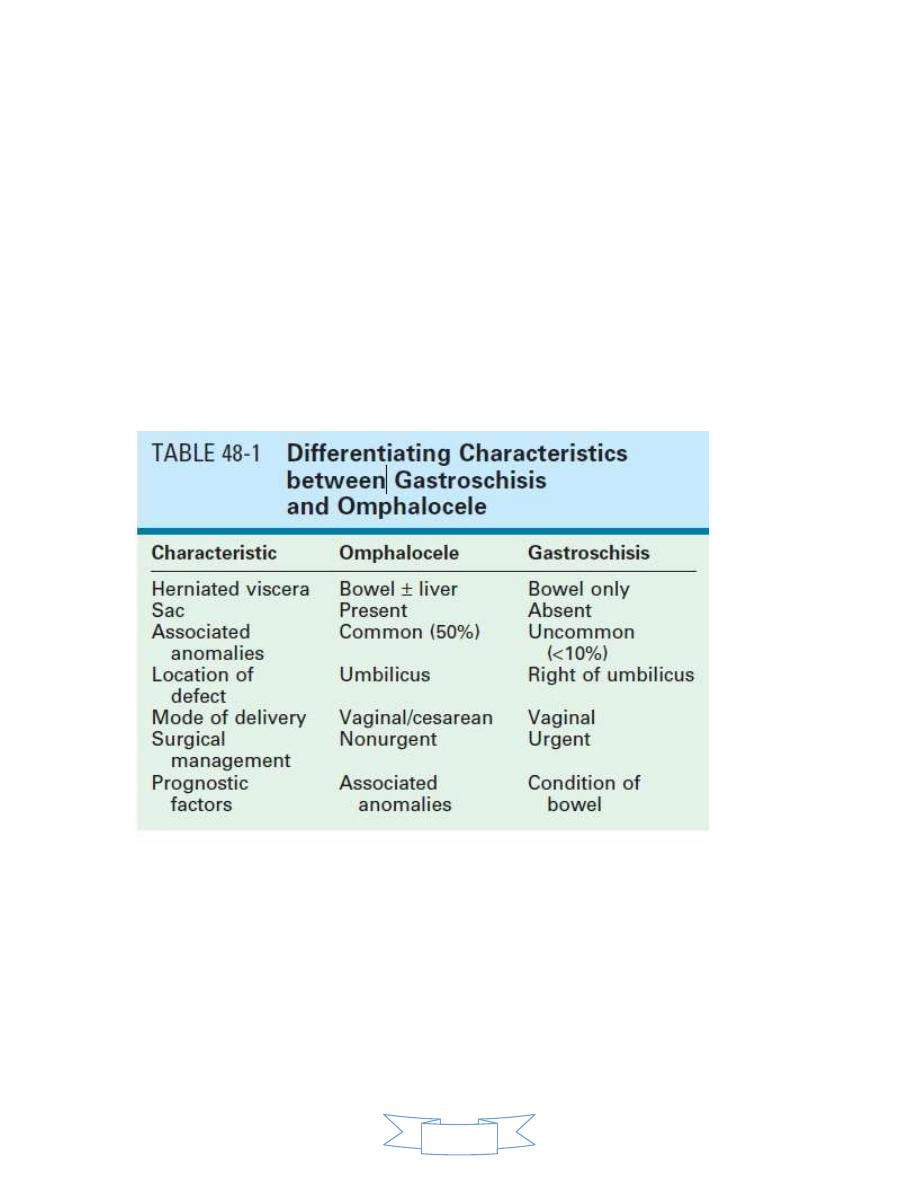
Gastroschisis and omphalocele are the two most common congenital
abdominal wall defects.
The incidence is 1:4000 live births.

2
Embryology:
The abdominal wall forms during the 4
th
week of gestation from differential
growth of the embryo causing infolding in the craniocaudal and
mediolateral direction. The lateral abdominal folds of the embryo meet in
the anterior midline and surround the yolk sac eventually constricting the
yolk sac into yolk stalk that becomes the umbilical cord.
During the 6
th
week of gestation rapid growth of the intestine causes
herniation of the midgut into the umbilical cord. Elongation and rotation of
midgut occurs. By week 10, the midgut has returned to the abdominal
cavity.
Failure of the viscera to return to the abdominal cavity result in
omphalocele. Other intra-abdominal viscera including liver, bladder,
stomach, ovary and testis can also be found in omphalocele sac.
The sac consists of the covering layer of umbilical cord and includes
amnion, Wharton’s jelly and peritoneum.
The location of the defect is in the mid abdominal region.
The etiology of gastroschisis less clear, two theories
1. Failure of mesoderm to form in the anterior abdominal wall.
2. The ventral body theory, which suggests failure of migration of the
lateral folds (more frequent on right side), is more accepted.
Diagnosis
U/S these two conditions are often diagnosed on prenatal
ultrasonography and are easily differentiated by the location of the
defect and by the presence or absence of a
surrounding sac .
Elevation of maternal α-feto protein.
3
Gastroschisis:
Occurs with an increased incidence in mothers younger than 21 years of
age.
Can be diagnosed sonographically prenatally by age of 20 weeks,
intrauterine growth retardation (IUGR) also noted by U/S.
Bowel atresia is the most common associated anomalies with gastroschisis.
Perinatal care:
Due to prolong exposure of the bowel of a neonate with gastroschisis to
the damage effect of amniotic fluid, bowel edema, poor motility and
malabsorption is noticed significantly.
The optimal mode and time of delivery for fetuses with gastroschisis has
been debated for many years, but it better to be carried in tertiary
perinatal center so as to provide immediate neonatal and pediatric surgical
experience.
Neonatal resuscitation and management:
Intravenous fluid resuscitation, the neonates with gastroschisis have
significant evaporative water loss from the open abdominal cavity
and exposed bowel.
Nasogastric decompression to prevent gastric and intestinal
distension.
The herniated bowel should be wrapped in warm saline soaked
gauze.
The infant placed with the bowel and legs in a plastic bag to reduce
evaporative losses.
Although gastroschisis most often is an isolated anomaly, thorough
examination of the neonate should be done to exclude the
coexistence of other congenital anomalies. And the bowel must be
examined carefully for bowel atresia, necrosis, and perforation.
4
Surgical management:
The primary goal is to return the viscera to the abdominal cavity while
minimizing the risk of damage due to direct trauma or to increased intra
abdominal pressure.
Options
Primary closure
Is practiced for neonate in whom reduction of the herniated viscera
is thought to be possible.
Traditionally the attempt of primary closure been done in operating
room, but some surgeons prefer to close the skin only and leave the
fascia separated, on bedside and without general anesthesia.
Or using the prosthetic options when primary fascial closure cannot
be achieved, using non-absorbable mesh or bio prosthetic material
such as dura or porcine small intestinal sub mucosa can be used.
Staged closure
A prefabricated silo with a circular spring that is positioned under the
fascial opening, without the need for suturing or general anesthesia.
Can be inserted in delivery room or bedside. After placement, the
bowel is reduced daily into the abdominal cavity as the silo is
shortened by sequential ligation. When the content are completely
reduced, fascial and skin closure are performed. This process takes
between 1-14 days.
This procedure
is used to avoid ischemic injury to the viscera due to
the high intra-abdominal pressure.

5
Postoperative course
Gastroschisis is associated with abnormal intestinal motility and
nutrient absorption, both of which gradually improve with time
Enteral feeding is delayed for few weeks while awaiting return of
bowel function.
Nasogastric decompression.
Parenteral nutrition.
Prokinetics for treatment of GIT dysmotility e.g erythromycin,
metoclopramide, domperidone, cisapride.
The long term outcomes for patients born with gastroschisis are
generally excellent.
The presence of bowel atresia is the most important prognostic
determinant for poor outcome.
Omphalocele
Perinatal care
Mode of delivery should be decided by the obstetrician. But in giant
omphalocele cesarean section is preferable because of the fear of
liver injury.
Delivery at a tertiary center is preferable for immediate access to
neonatal and pediatric surgical expertise.
Neonatal resuscitation and management
A thorough search for associated anomalies should be done,(cardiac
evaluation ,renal, neonatal hypoglycemia for possibility of Bechwith-
Weidemann syndrome ,and blood sample for genetic evaluation if
indicated.

6
Intravenous access and fluid resuscitation, infants with omphalocele
do not have as significant fluid and temperature losses as those with
gastroschisis but the loss are higher than those with intact
abdominal wall.
The omphalocele itself can be dressed with saline soaked gauze to
minimize those losses.
Nasogastric tube.
Surgical management
Immediate primary closure: treatment options depend on the size of the
defect, gestational age and the presence of associated anomalies.
In infants with small defects primary closure may be appropriate.
In infants with larger defects but still easy to close without much loss
of abdominal domain can also be closed soon after birth,
Staged neonatal closure:
The loss of domain in the peritoneal cavity prevent primary closure without
an undue increase in intra-abdominal pressure
Staged closure in the neonatal period involves the use of different
technique, of these the use of the existing amniotic sac with serial
inversion which allows gradual reduction of the sac followed by sac
excision and primary or mesh closure, or the amniotic sac is excised
and replaced with mesh (use to bridge the fascial gap) and then
closed over time.
Delayed staged closure
Used for large omphalocele , the sac is excised and a silastic ‘silo’
sewn to the abdominal wall ,serial reduction once or twice daily

7
similar to that of gastroschisis done until definitive closure can be
obtained
Scarification treatment
Escharotics therapy which result in gradual epithelialization of the
omphalocele sac, used for neonates who cannot tolerate operation.
Iodine, silver sulfadiazine, and nystatine powder used for sac to
granulate and epithelialize ,once the patient is stable then ventral
hernia can be repaired by one the previously mentioned method.
Postoperative course
Most of patients require mechanical ventilation after primary closure
for few days.
Nasogastric tube for gastric decompression.
feeding can begin when nasogastric tube output is no longer bilious
and bowel activity has occurred
antibiotics for 48 hours (if there is no infection)
If a hernia develops, closure usually can be done after age of one
year.
Post-operative complications
1. increase intra abdominal pressure
2. acute hepatic congestion
3. renal failure
4. bowel infarction



