LECTURE TWO
ORAL SURGERY“CASE SHEET, ARMAMENTARIUM, AND PRINCIPLES OF ORAL SURGERY”
Dr. Mohammed Amjed
BDS, MSc, PhD
3.11.2015
Diagnosis, the key to understanding and treating disease, is a systematic process by which we uncover the identity of a patient's problem, leading to reliable predictions of its behaviour and possible therapy.
● The process is a detective story in which the information obtained is matched with patterns of known disease.
● A standard framework is used to record findings and acts as a checklist and an aid to communication between colleagues.
● Special investigations may be required to lead you to a definitive diagnosis, which must relate directly to the reason for attendance (chief complain).
● A treatment plan should be based on the diagnosis and agreed with the patient.
● The diagnosis or identity of a disease is used— to predict its behavior or natural history
— to plan treatment— to support the patient in understanding their condition
— to link similar cases for research purposes
— to enable communication between professionals
Why is the diagnosis?
RECORD KEEPING
The following sections are divided according to commonly used subdivisions in a patient record.The concept of this progression and the written record certainly help to keep one’s thoughts in a logical order.
Demographic details (Personal information)
The patient’s full name, address, date of birth, gender, ethnic origin and marital status should be recorded.PRESENTING COMPLAINT (CHIEF COMPLAIN)
• Write the complaint in the patient’s own words,
• Ensure you put it in inverted commas—for example, ‘I’ve pain in upper right jaw area’. Complaints can be multiple and should be dealt with one at a time.Listen first and listen second
Listening does not just involve using your ears.
Also use facial expression,body language
and verbal fluency to help understand what is really troubling someone and to suggest other areas in which the history might need to proceed.
Remember that speech is not the only means of communicating. Make full use of communication aids such as picture boards, drawings done by the patient showing where the pain is, when this is a more appropriate form of discourse.
What questions used during history taking ?
Open questions- These are seen as the gold standard of historical inquiry. They do not suggest a 'right' answer to the patient. It give patients a chance to express what is on their mind. Examples include questions such as 'How are you?'. There are other similar open questions but it may be effective just to let the patient start speaking sometimes.
• Open questions can be used to obtain specific information about a particular symptom as well. For example: 'Tell me about your cough'.
• Open questions cannot always be used, as sometimes you will need to delve deeper and obtain discriminating features about which the patient would not be aware.
Questions with options
Sometimes it is necessary to 'pin down' exactly what a patient means by a particular statement.
In this case, if the information you are after cannot be obtained through open questioning then give the patient some options to indicate what information you need.
Leading questions
These are best avoided if at all possible. They tend to lead the patient down an avenue that is framed by your own assumptions.For instance, a male patient presents with episodic chest pain. You know he is a smoker and overweight so you start asking questions that would help you to decide if it's angina. So you ask: 'Is it worse when you're walking?', 'Is it worse in cold or windy weather?'. The patient is not sure of the answer, not having thought of the influence of exercise or the weather on his pain, but answers yes, remembering a cold day when walking the dog when the pain was bad. You may be off on the wrong track and find it hard to get back from there. It is much better to ask an open question such as: 'Have you noticed anything that makes your pain worse?'. When the patient answers: ‘some food types', you are on firmer ground in suspecting that this may be chest pain of gastrointestinal origin.
History of presenting illness
Record the history chronologically, beginning with the onset and detailing the progress of the complaint to the present day.In oral surgery the common complaints are of pain, swelling or lump, or ulcer.
Allow the patient to tell the story in her or his own way and do not ask leading questions. Main points to cover include:● What was the first thing that was noticed?
● Are there any other symptoms?● What is the main trouble today?
● Does anything worsen or improve the symptoms?
● Does the complaint incapacitate the patient (i.e. does it stop the patient from sleeping, working, eating, carrying out normal activities)?
It is important to note recurrence of problems. For example, wisdom tooth infections may settle spontaneously, but tend to recur at intervals of weeks to
months, whereas malignant tumours tend to be relentlessly progressive.
Medical history
• It is essential in order to assess the fitness of the patient for any potential procedure.
• The history will also help to warn you of any emergencies that could arise.
• Possible contribution to the diagnosis of the presenting complaint.
The medical history should be reviewed systematically.
In physical medicine it is common, after initial open questions about the patient’s general health, to ask questions in relation to each body system in turn:
cardiovascular, respiratory, CNS, gastrointestinal tract (including the liver), genitourinary tract (including the kidneys), etc.
It is essential also to ask specific questions about drug therapy, allergies and abnormal bleeding.
Social history
Occupation, home circumstances and travelling arrangements should be reviewed so they can be used to help formulate the details of the treatment plan.For example, planning third molar surgery as an outpatient, for a parent with small children, with a one-hour journey to the surgery by public transport, returning to an empty house would be unsympathetic and unwise as the patient would have difficulty in dealing with postoperative complications such as haemorrhage or fainting.
Smoking and alcohol consumption should also be considered under this heading.
Past dental historyIf the patient is new to your practice then you should note details of previous attendance and treatment.
This would include the name and address of their previous practitioner, frequency of attendance and any problems relevant to the presenting complaint.
The reason for discontinuing attendance at that practice should also be noted.
In case of tooth extraction, ask about the difficulty of the last extraction if any, and the postoperative bleeding.
● Character
● Severity● Site
● Radiation (spread)
● Onset
● Duration
● Periodicity
● Aggravating factors
● Relieving factors
● Associated phenomena
Features of pain worth noting in the history
EXAMINATION
There are two ways of approaching the examination.-You may look at the site of complaint first and subsequently carry out extraoral and intraoral examination.
-Alternatively you may do a systematic extraoral
examination followed by a systematic intraoral examination, which will encompass the area of complaint.Extraoral examination
The general appearance of the patient should be considered.
Do they look ill or well; are they anxious?
Note the skin complexion and mucosal colour for signs of anaemia or jaundice.
Assess the body in general and the head and neck for signs of deformity or asymmetry.
In trauma cases look carefully for lacerations and abrasions.
Look systematically at, or for:
● lymph nodes: these should be palpated for enlargement or change in texture● TMJ function & trismus: defined as limitation of mouth opening of musculoskeletal origin, trismus can be partial or complete. Normal mouth opening is at least 40 mm
● rima oris (oral entrance): a small mouth opening can make surgery difficult. Limitation could be due to scarring or the patient may naturally have a small mouth
● swellings or deformity.
Intraoral examination
The size of the oral cavity and the distensibility of the soft tissues should be noted.The soft tissues should then be examined in sequence, and this sequence should always be used by that clinician, so no area is omitted. A suggested sequence is:
● buccal sulci (upper and lower)
● floor of the mouth
● tongue (dorsal and ventral surfaces)
● palate (hard and soft)
● oropharynx
● gingivae.
Next, the teeth may be examined and charted .
The surgical or problem area (offending tooth) should now be examined.
Redness or swelling or inflammation should be noted, as should any discharge of pus. Look specifically for ulceration, erosion or keratosis of mucosal surfaces and for any lumps or deformity.
DIFFERENTIAL DIAGNOSIS
When many diagnoses might explain the signs and symptoms of the chief complaint, a differential diagnosis is made.This is a list of possible diagnoses written in order of probability.
It is unhelpful to arrange special tests unless there is a list of different possible diagnoses that must be distinguished.● Duration
● Change in size● Any possible cause
● Exact anatomical site
● Associated lymph nodes
● Single or multiple
● Shape
● Size
● Colour
● Definition of periphery
● Consistency
● Warmth
● Tenderness
● Attachment to skin
● Attachment to deeper structures
● Fluctuance
● Inflammation
● Pulsation
● General well-being of the patient
FEATURES WORTH NOTING DURING HISTORY AND EXAMINATION OF A LUMP OR SWELLING
Features worth noting on examination of an ulcer
● Anatomical location● Single or multiple
● Size
● Shape
● Base
● Edge
● Adjacent tissues
● Discharge
● Is it painful?
● General condition of the patient
FURTHER INVESTIGATION
Often the history and clinical examination are not sufficient to clarify the diagnosis and enable a sound treatment plan to be drawn up. Further investigation might involve a wide range of measures, such as:
● haematological investigations
● microbial culture
● temperature, pulse, respiratory rate, blood pressure, weight
● urinalysis
● biopsy—incisional or excisional.
● radiography and other imaging
● vitality tests
CONSENT
All patients must be fully informed before any decisionconcerning treatment is made and no treatment should be performed without a patient’s full consent.
Surgery is regarded as an assault on the body. Adults
may give consent to such a process, but cannot be regarded as having consented if they do not fully understand the implications.What a patient should be told should be influenced by what a reasonable patient could be expected to want to know. This is difficult to judge, so it is proper to offer more rather than less information.
- For example, surgery for an impacted wisdom tooth has potential complications of pain, swelling, trismus, altered sensibility of the lip and/or tongue.
- Patients should also be advised as to the likelihood of incidence, the approximate extent and probable duration of each of the problems.
- For patients under 16 years of age it is generally accepted that a parent or legal guardian will give consent on the child’s behalf. Consent may be withdrawn at any time. The patient’s wishes must be respected.
ARMAMENTARIUM FOR BASIC ORAL SURGERY
CONTENTS
Instruments for Transferring Sterile InstrumentsInstruments for Incising Tissue
Instruments for Elevating Mucoperiosteum
Instruments for Retracting Soft Tissue
Instruments for Controlling Hemorrhage
Instruments for Grasping Tissue
Instruments for Removing Bone
Instruments for Removing Pathologic Tissue
Instruments for Suturing Mucosa
Instruments for Holding the Mouth OpenInstruments for Suctioning
Instruments for Irrigating
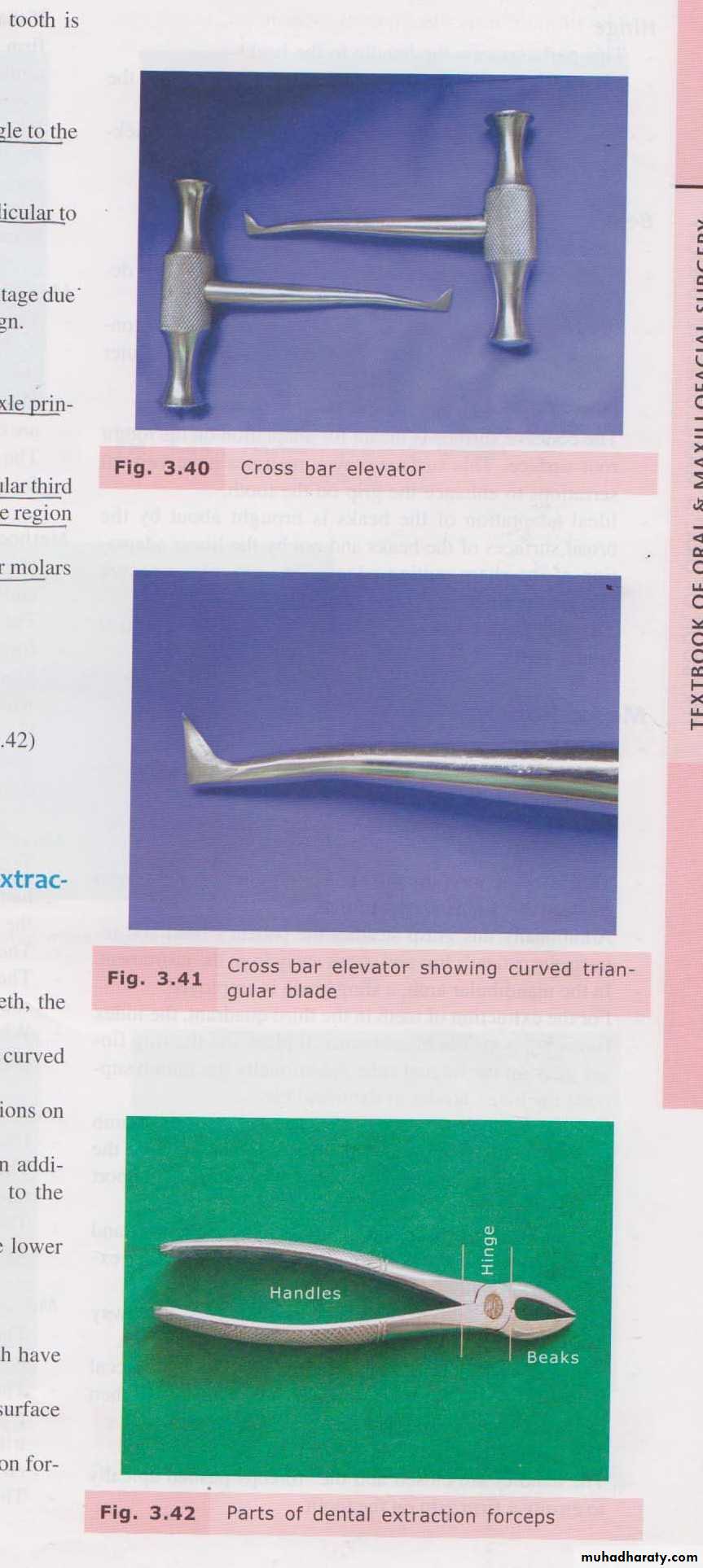
Instruments for Extracting the Teeth
-Local Anesthetic instruments
-Dental elevators
-Extraction forceps
Instrument trays
INSTRUMENTS FOR TRANFERRING STERILE INSTRUMENTS
CHEATLE FORCEPS
Long handlesLong, angulated beaks: serrated
Beaks: dipped in antiseptic solution
Lift up sterile instruments from autoclave/ drum
INSTRUMENTS FOR INCISING TISSUE
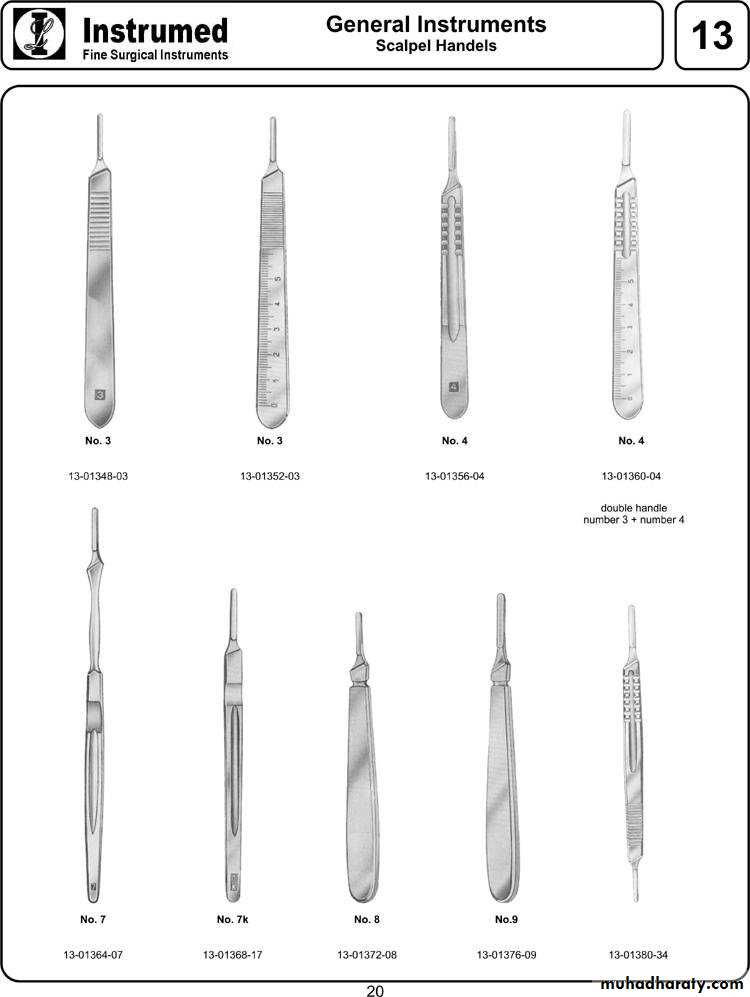
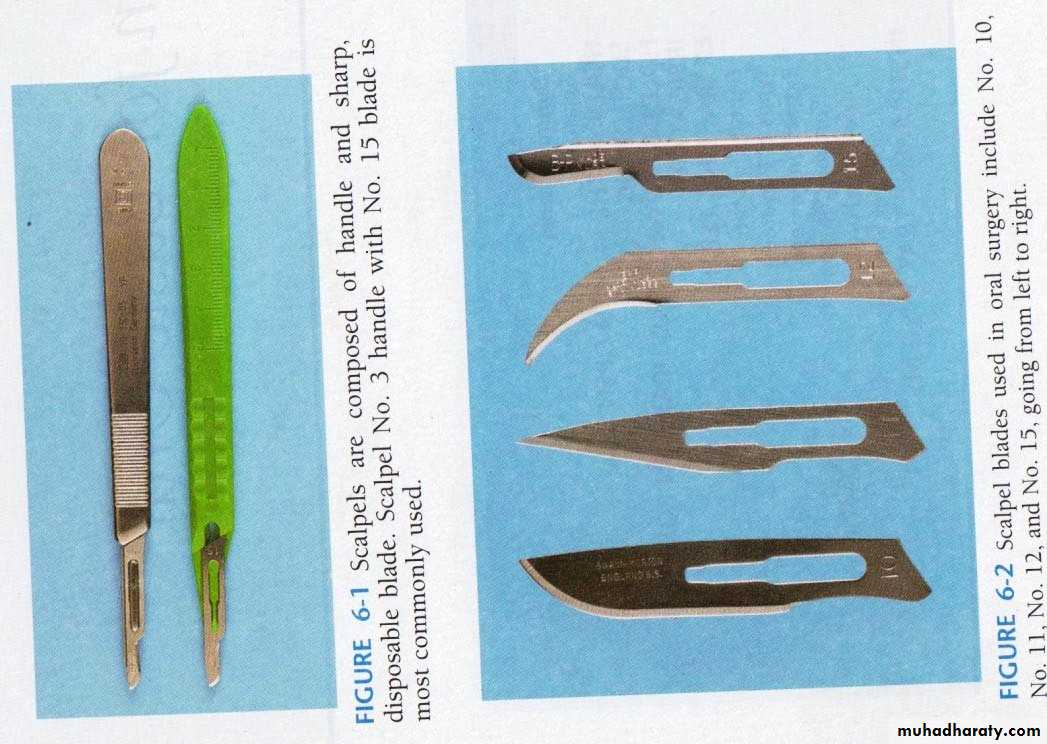
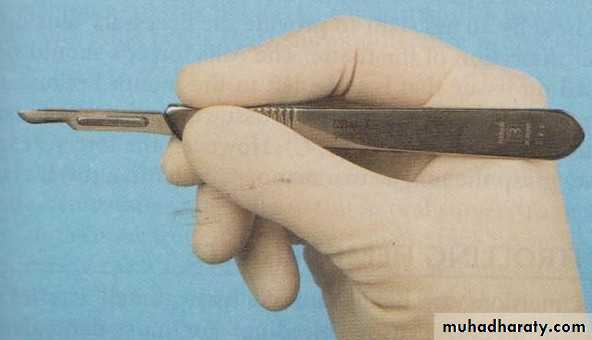
SCALPEL:Handle like No. 3, No.7
Differently shaped
2. No.10- similar to No.15
Large skin incisions
3.No. 11
Sharp, pointed
Incising an abscess
4.No.12
Hooked
Operculectomy
Posterior aspect of teeth/maxillary tuberosity
Disposable, sterile sharp blade
• 1. No.15- most commonly usedRelatively small
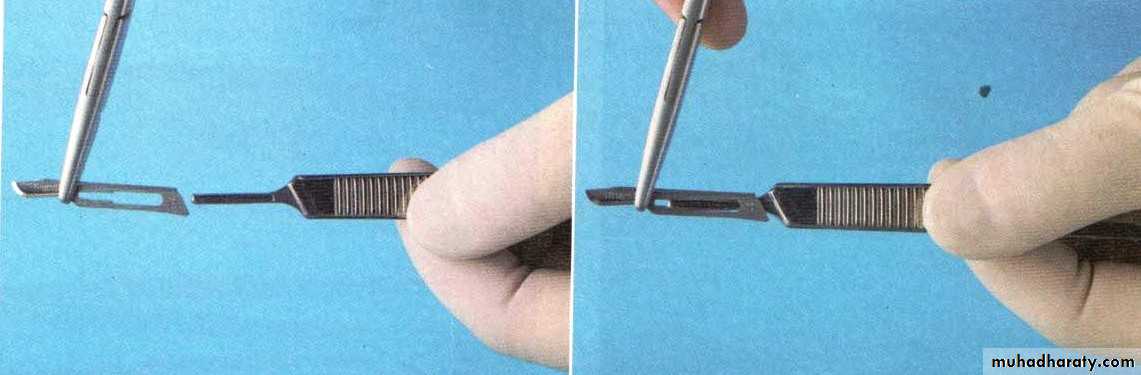
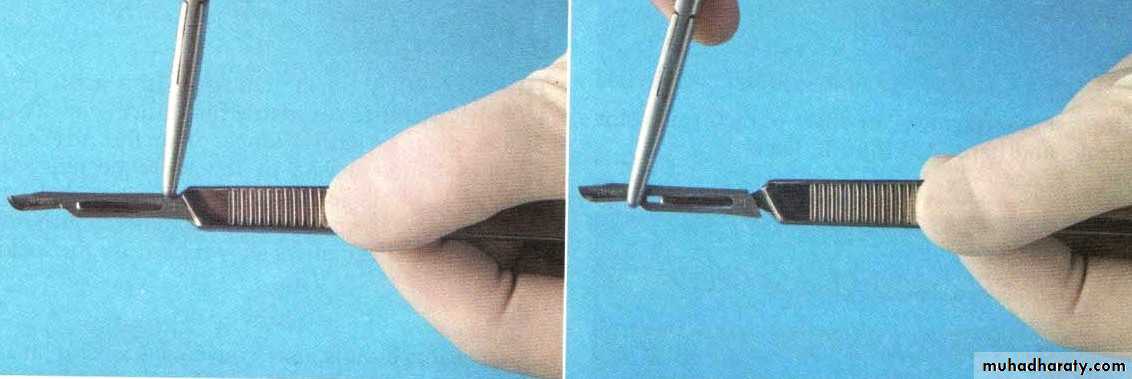
Blade loaded
Blade removedPen Grasp: Allow maximal control
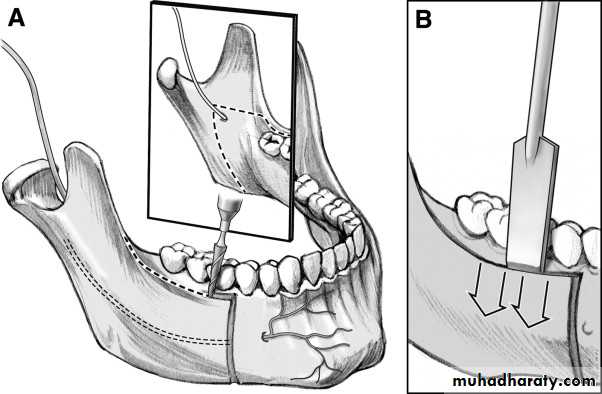
Hold mobile tissue firmlyINSTRUMENTS FOR ELEVATING MUCOPERIOSTEUM
Mucosa & Periosteum reflected in single layer: Periosteal Elevator• No.9 Molt periosteal elevator
sharp, pointed end: reflect papillae from between teeth, loosen soft tissues via gingival sulcus
Broader, flat end: elevating the tissue from bone
Thin, sharp cutting edge- clean separation of periosteum from bone
Also used as retractor
II. Howarth’s Periosteal Elevator
Double-endedOne end: flat, broad, spatulate- sharp edge
Other end: Rugine end; flat & rectangular. Small tip – sharp projection perpendicular
INSTRUMENTS FOR RETRACTING SOFT TISSUE
Good vision & accessCheeks, tongue & mucoperiosteal flaps
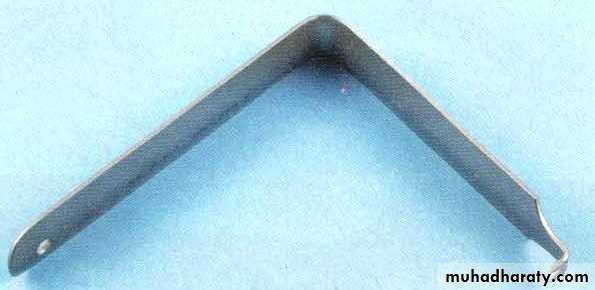
Right angle Austin retractor
‘L’-shaped- no handleRetraction of small intraoral flaps: removal of impacted teeth
Offset broad Minnesota retractor
Both Austin’s & Minnesota : retract cheek & mucoperiosteal flap simultaneouslyLangenback’s Retractor
‘L’ shaped retractor- long handleRetraction of flap edges : improved visualization of deeper layers & structures
Different sizes: handle length & blade width
Tongue Depressor
‘L’- shapedBroad, flat, rounded blade
Retraction & depression of tongue
Improve visibility- posterior pharyngeal wall & tonsillar region, lingual side of mandible
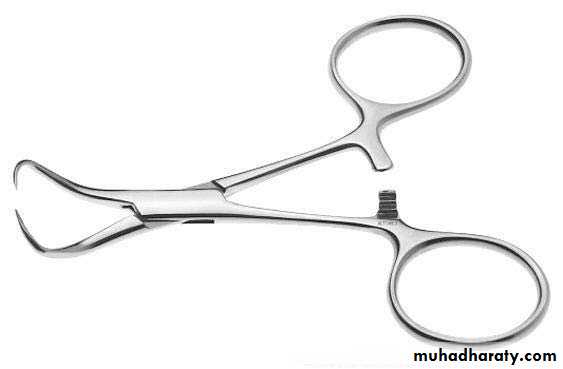
INSTRUMENTS FOR CONTROLLING HEMORRHAGE
Arteries & veins- bleeding : pressure not enoughHemostat
Variety of shapes
Small or delicate/ Larger
Straight/ Curved
Curved hemostat- common
Long, delicate beak to grasp tissue & a locking handle
Locking handle: clamps onto a vessel; then let go & remains clamped onto tissue
Removes granulation tissuePicks up root tips, pieces of calculus, fragments of amalgam restorations, any other small
particles dropped into the mouth
Small hemostat: Mosquito forceps
INSTRUMENTS FOR GRASPING TISSUE
Used for Soft tissue stabilization- pass suture needleCollege/Cotton forceps
AngledSmall fragments of tooth/amalgam/foreign material
Placing/removing gauze packs
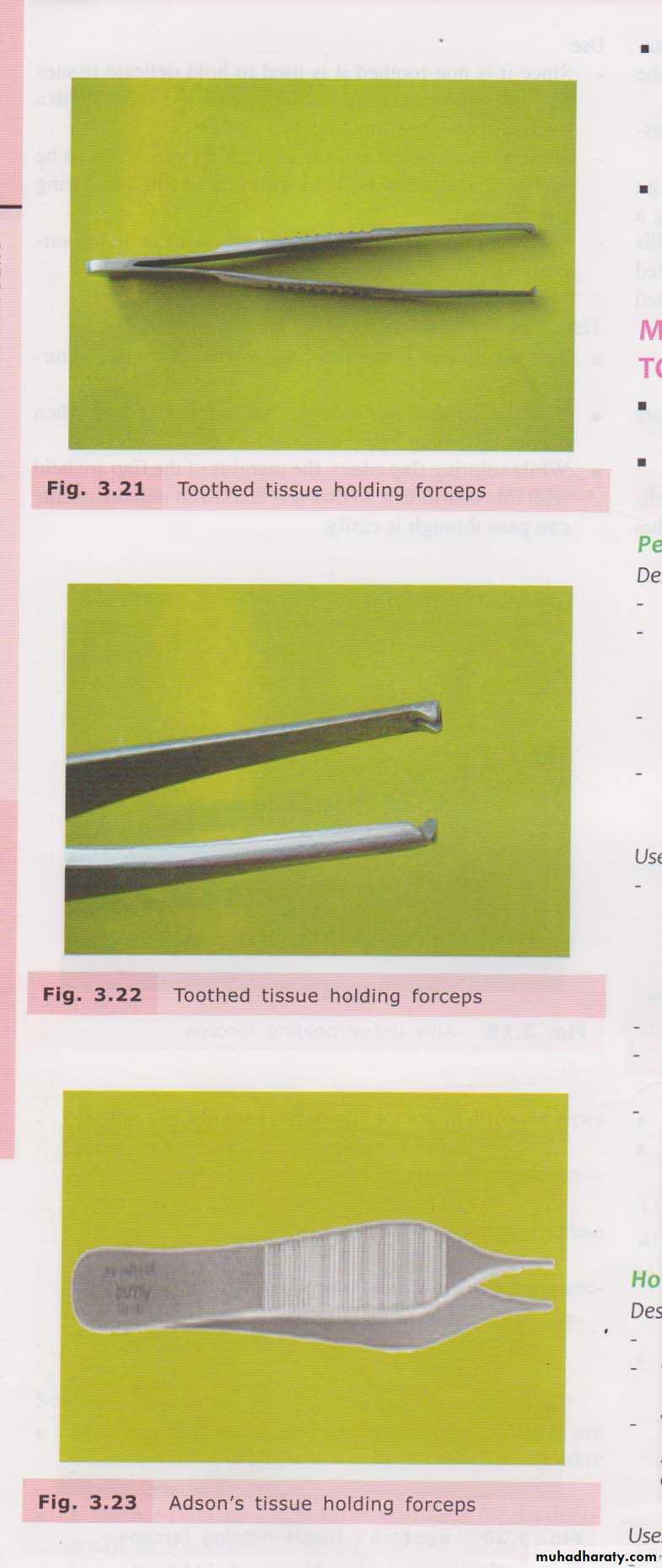
Tissue Holding Forceps
Toothed/ Non- toothedToothed: periosteum, muscle, aponeurosis
Non- toothed: fascia, mucosa, pathological tissues
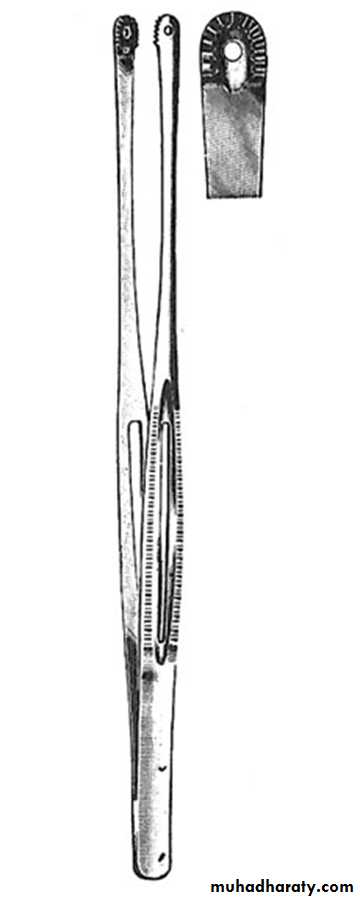
Allis Tissue forceps
Allis Tissue forcepsLocking handles
- proper placement
- held by asstisstant :necessary tension
Teeth which will firmly grip the tissue
Removal of large amounts of fibrous tissue: Epulis fissuratum
Russian Tissue forceps
Large, round-endedTeeth elevated from sockets
Round end: positive grip, avoids slippage; unlike hemostat
Placement of gauze: isolation
INSTRUMENTS FOR REMOVING BONE
Rongeur forcepsMost commonly used
Sharp blades- squeezed together; cutting/pinching through bone
Leaf spring between the handle : instrument opens when hand pressure is released
Repeated cuts without manually reopening
2 major designs:
Side-cuttingSide-cutting & end-cutting
Do not :
-remove large amounts of bone in single bites
- use to remove teeth
Small amounts- multiple bites
Success: sharpness- sharpen before sterilisation
Carbide tips- use more than once, before sharpeningCylindrical handle- serrated with flat end: struck with mallet
Flat & rectangular: cutting edge in different sizes
Single bevel- cutting edge
Transalveolar extraction/ removal of impacted tooth
Shape/ contour irregular bony surfacesBevel faces- bone to be cut
Cutting edge- perpendicular to bone
Chisel
OsteotomeSplitting bone
Cylindrical handle- serrated for good grip
Flat end- tapped with mallet
Flat & rectangular blade
Bibivelled cutting edge- converge to a sharp edge
Osteotomy cuts: orthognathic surgery/ refracturing malunited fractures
Osteoplasty/ bone recontouringSplit impacted tooth for easy removal
Surgical Mallet
Cutting bone with osteotome/ chiselStainless steel- strong cylindrical handle
Tapped : ‘pull-back’ action- force from wrist
Fracture jaw: inadvertent force
Bone file
Final smoothing of bone before suturing of mucoperiosteal flapDouble-ended: small & large
Removes bone: pull stroke
Avoid push motion- burnishing & crushing the bone
Bur and Handpiece
Surgical removal of teethHigh-speed + sharp carbide burs: cortical bone removal
Completely sterilizable in a steam autoclave: ensure on purchase
Relatively high speed & torque: rapid bone removal & efficient sectioningMust not exhaust air into the operative field
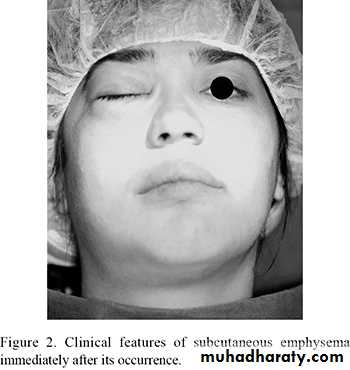
Avoid high-speed turbine drills used in restorative dentistry (tissue emphysema)
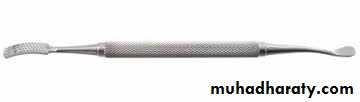
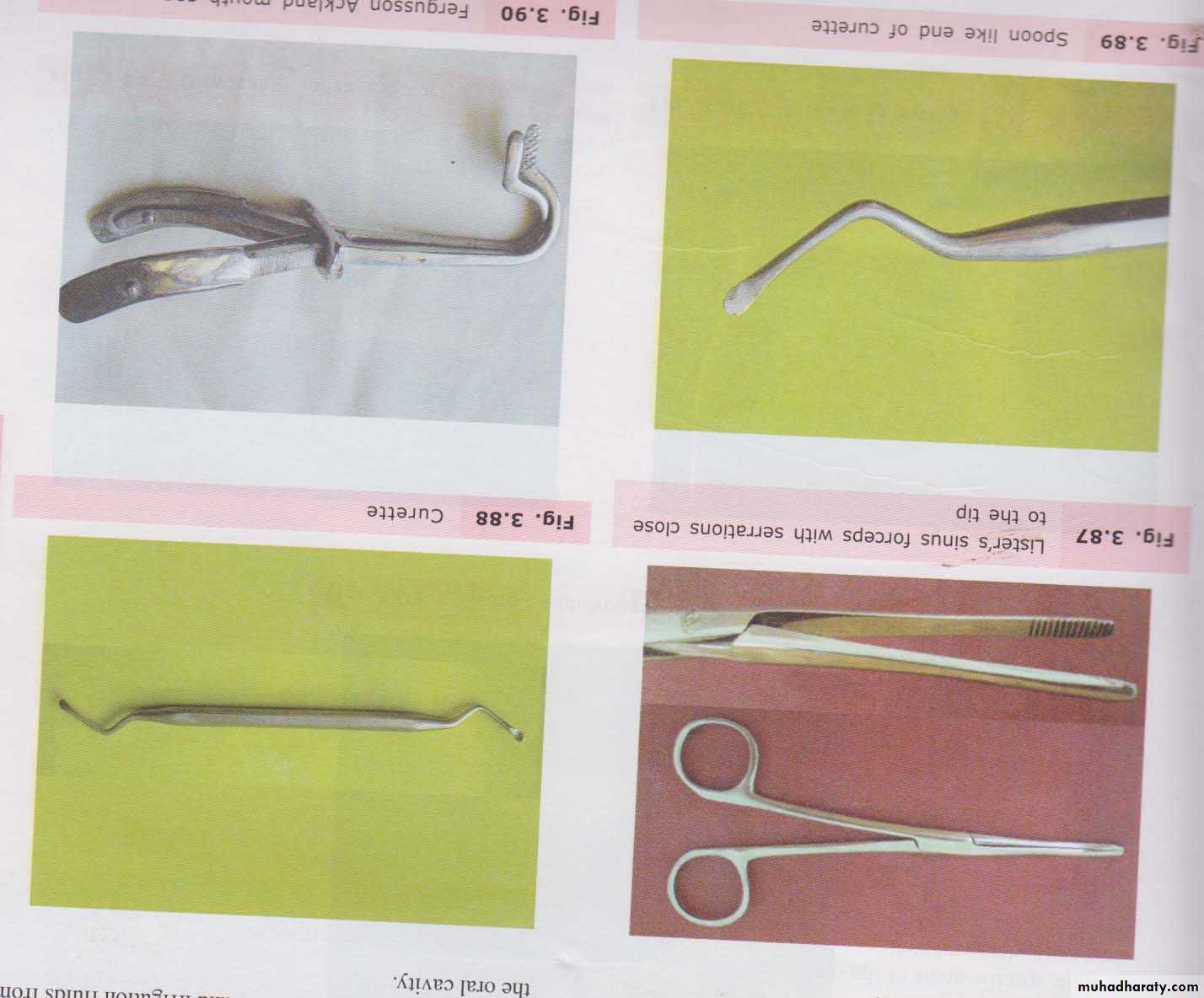
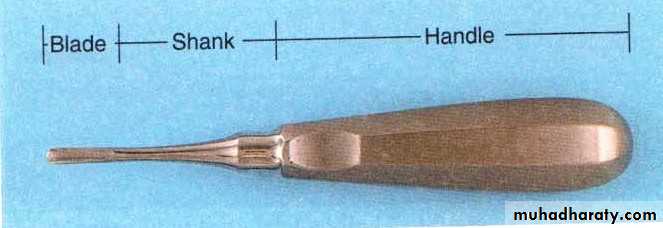
INSTRUMENTS FOR REMOVING PATHOLOGICAL TISSUE
Periapical CuretteAngled, double-ended
Removal of granulomas/small cysts from periapical lesions
Small amounts of granulation tissue debris from tooth sockets
Sinus Forceps
Handles with rings at the endNo lock/ ratchet
Narrow, long, slender beaks
Inner surface- transverse striations: close to the tip
Draining pus from an abscess
Inserted by blunt dissection & opened up
No lock: blind insertion & closure- injure structures
INSTRUMENTS FOR SUTURING MUCOSA
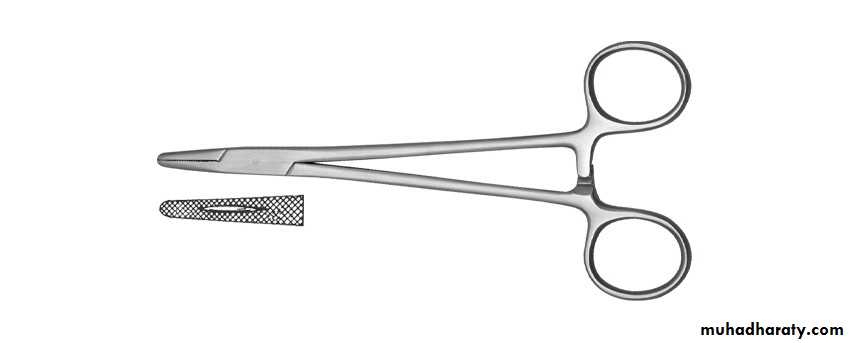
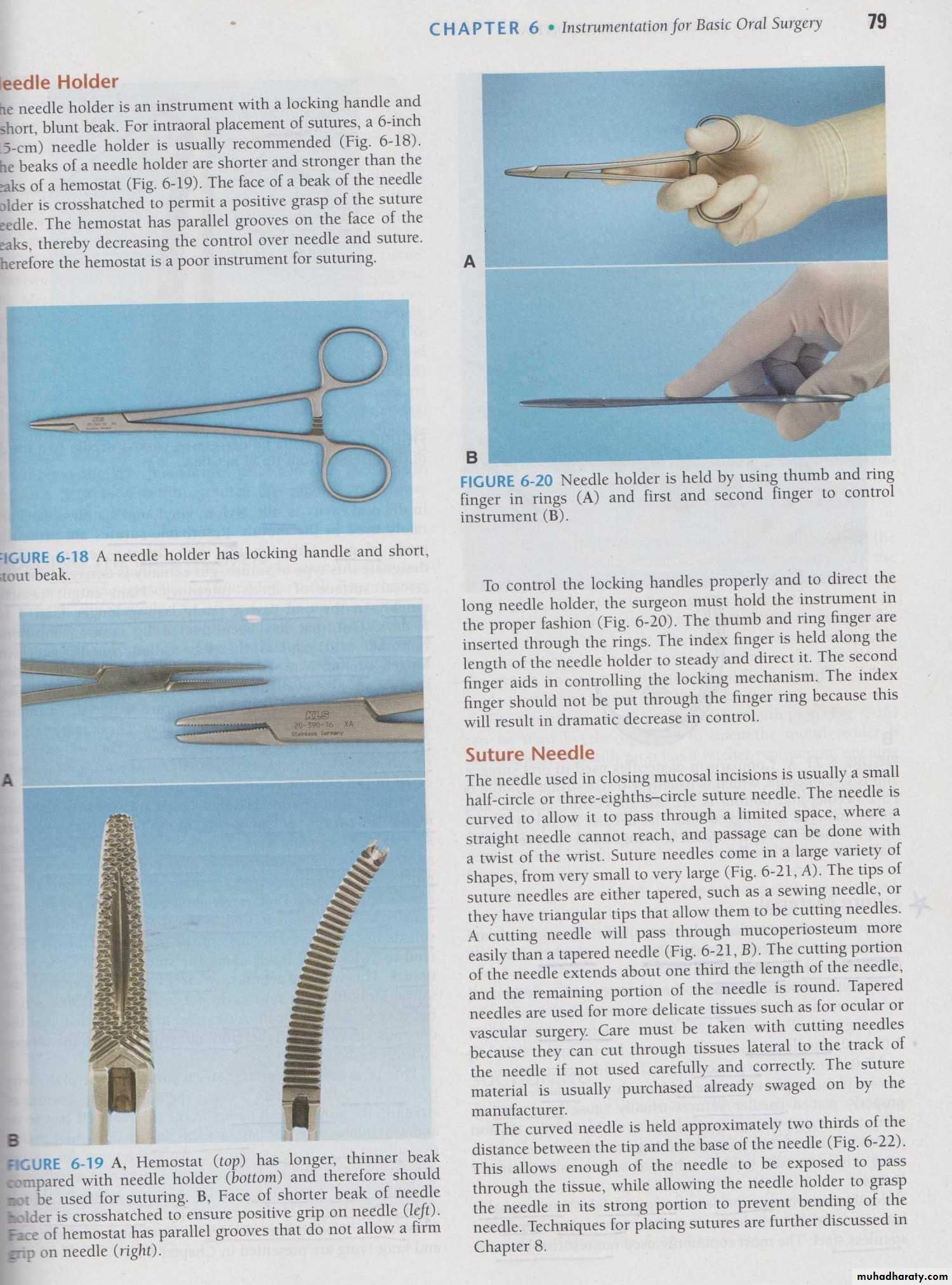
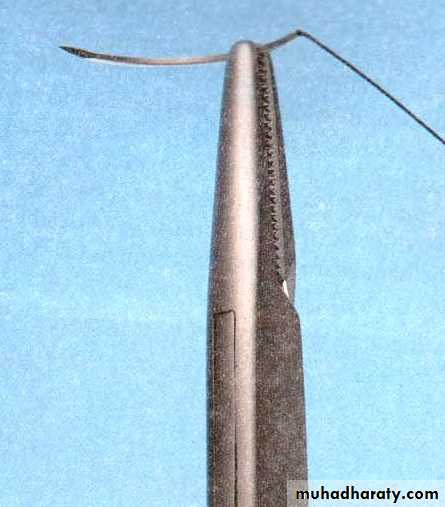
Flap returned to its original position & held by suturesI. Needle holder
Instrument with a locking handle, short, stout beak
Beak- shorter & stronger than hemostat
Face of the beak crosshatched :
positive grasp; unlike hemostat
COMPARISON
Hemostat: Beaks smaller than sinus forceps, longer than needle holder; transverse striations; ratchet
Needle holder: Criss-cross striations; ratchet
Sinus forceps: striations only near the tip; no ratchet
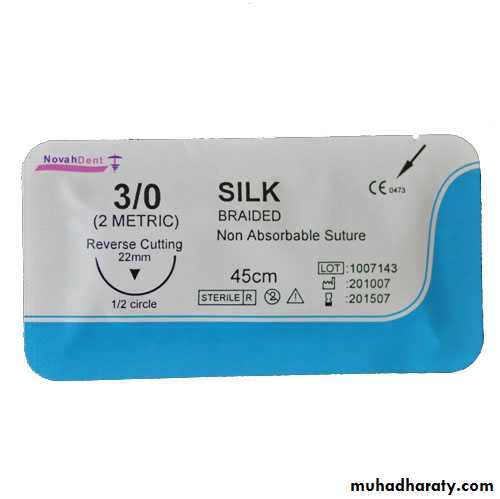
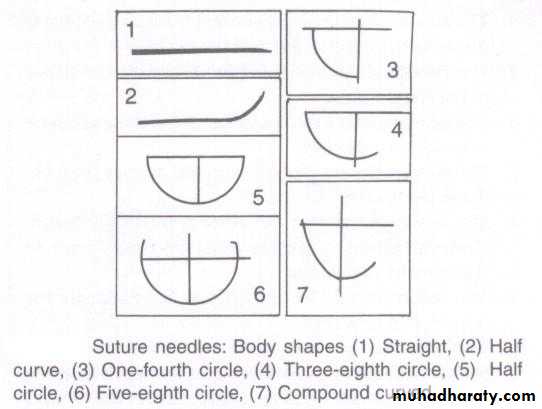
INSTRUMENTS FOR SUTURING MUCOSA
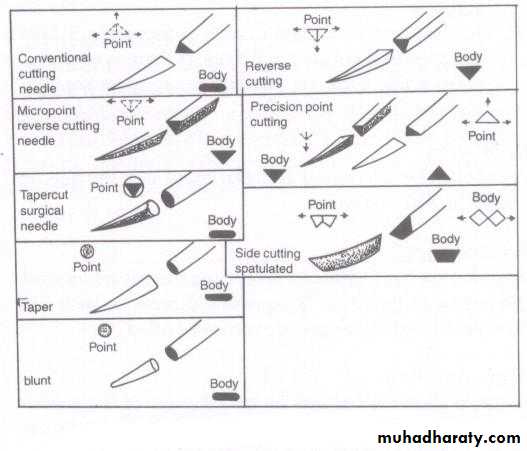
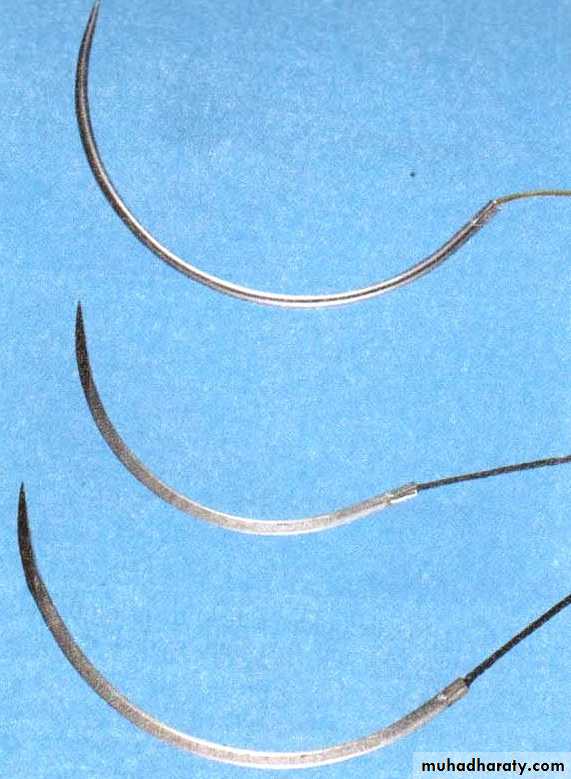
II. Suture needleMucosal closure: ½ circle or 3/8 circle
Curved: pass through a limited space; twisted wrist
Large variety of shapes
Very small – very large
Tips: (i) tapered- sewing needle
(ii) triangular – cutting needle
Cutting needle: pass through mucoperiosteum more easily than a tapered needle
1/3 – cutting; remaining- roundTapered :vascular, ocular
Suture material: usually swaged on
Held 2/3rd – between the tip & the base:- enough exposed to pass through the tissue
- grasp in the strong portion to prevent bending
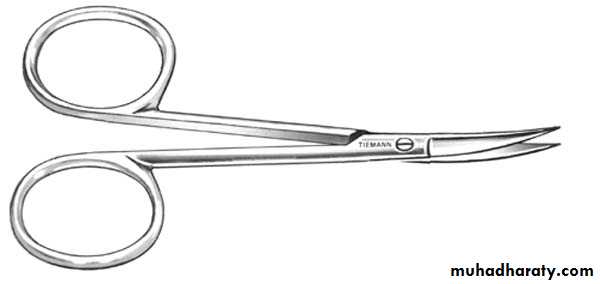
IV. Scissors
Short cutting edgesLong handles
Thumb & ring fingers
Held same as needle holder
Dean scissors
Slightly curved handles
Serrated blades
Mayo scissors
Straight-bladed Mayo scissors are designed for cutting body tissues near the surface of a wound. As straight-bladed Mayo scissors are also used for cutting sutures, they are also referred to as "suture scissors"Tissue scissors
Straight or curved bladesDon’t cut sutures: dull the edges- less effective & more traumatic
INSTRUMENTS FOR HOLDING THE MOUTH OPEN
Soft, rubberlike block- patient rests teethPatient opens to comfortably wide position- block inserted: holds in the position
Protects patient’s TMJ, while mandibular teeth
Mouth Gag
Forcefully open mouth: trismusBroad, serrated blades: rest on occlusal surface of molars: instrument opened : slow, gradual force
Keep mouth open: procedures under G/A
INSTRUMENTS FOR HOLDING TOWELS & DRAPES IN POSITION
Towel clipHolds together, drapes placed around a patient
Stabilizes suction tubes, micromotor etc.
Hold & retract tongue: unconscious patient
Locking handle + finger & thumb rings
Sharp/blunt action ends
Curved points- penetrate towels & drapes
Caution: not to pinch patient’s skin