Ophthalmology
Baghdad medical college 2015 – 2016
Strabismus (Squint)
Anatomy of extraocular muscles:
There are four recti, two oblique's and levator palpebrae superioris. The Recti
muscles are originated from a fibrous ring called "Annulus of Zinn" in the apex of
the orbit which surrounds the optic nerve.
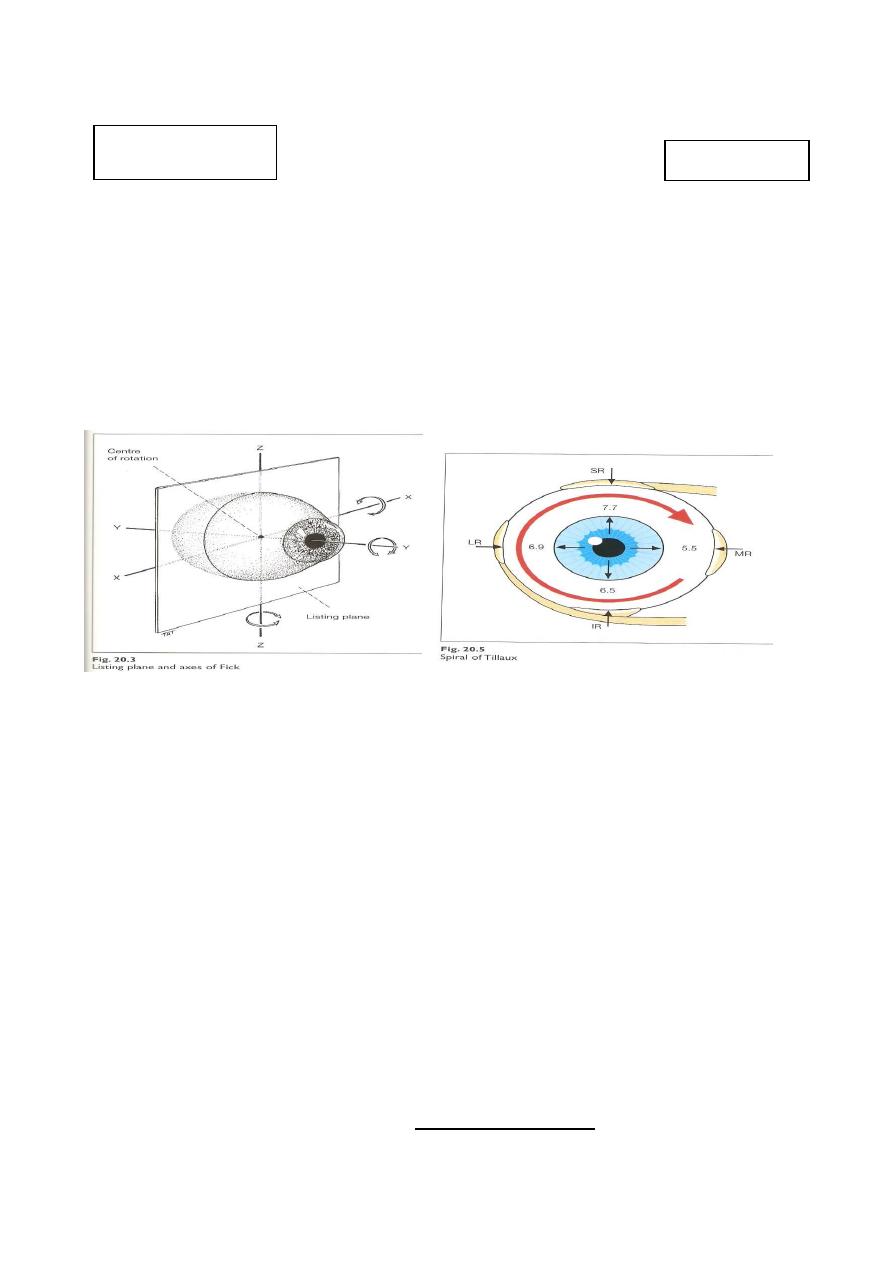
* Listing plane: Imaginary plane dividing the eyeball into anterior and posterior
halves, passing through the centre of rotation.
Axes of Fick:
Axes around which the movements of eyeball are occur. They are three; X
(horizontal axis parallel to the iris plain), Y (horizontal axis perpendicular to the iris
plain ) & Z (vertical axis).
- Movements around X-axis are elevation and depression.
- Movements around Y-axis are Intorsion and extorsion.
- Movements around Z-axis are adduction and abduction.
The recti muscles:
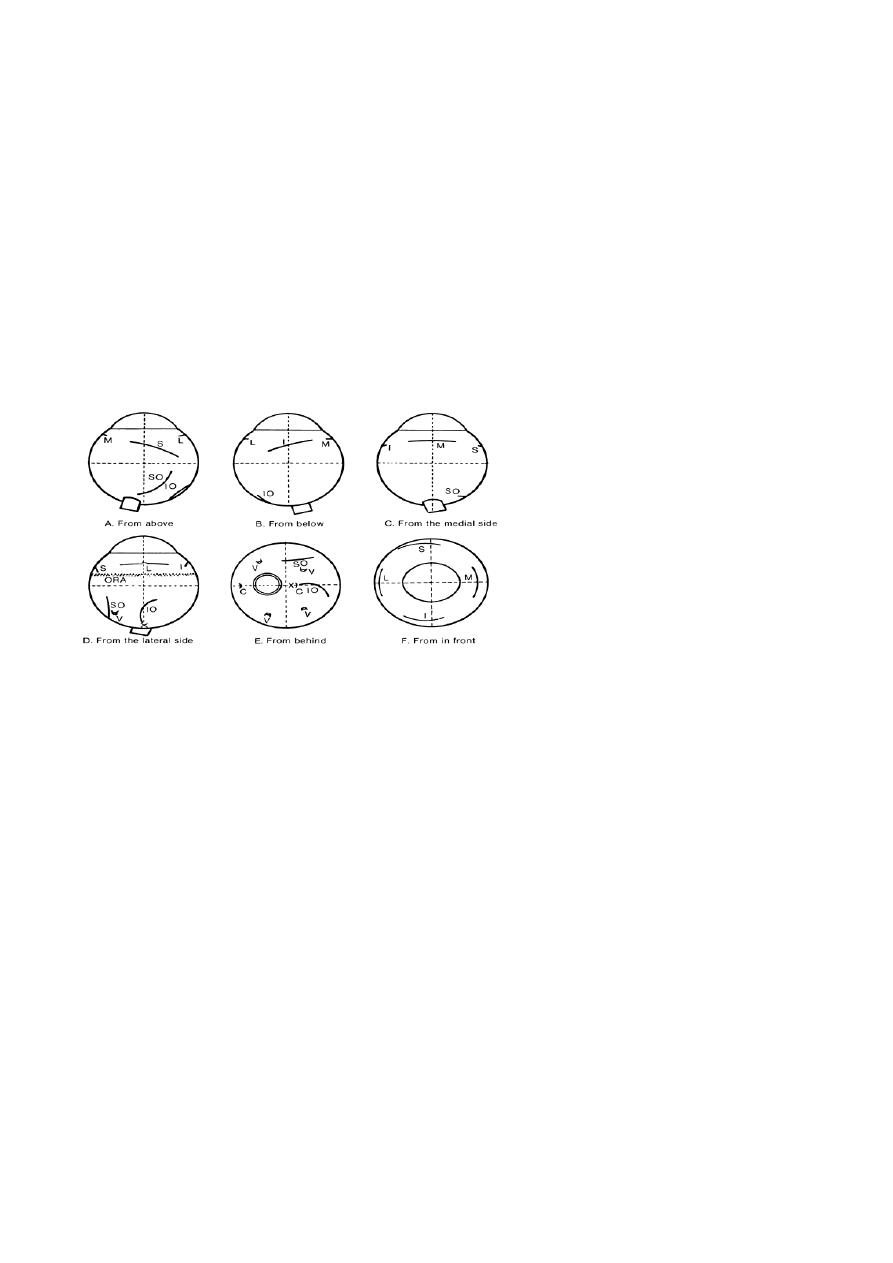
- Medial rectus: originates from the medial side of the annulus to be inserted on the
medial side of the eyeball 5.5 mm posterior to the limbus.
- Inferior rectus: originates from the inferior side of the annulus to be inserted on
the inferior surface of the eyeball 6.5 mm posterior to the limbus.
- Lateral rectus: originates from the lateral side of the annulus to be inserted on the
lateral side of the eyeball 6.9 mm posterior to the limbus.
- Superior rectus: originates from the superior surface of the annulus to be inserted
on the superior surface of the eyeball 7.5 mm posterior to the limbus.
* The insertions of all muscles are anterior to equator and covered by tenon's
capsule and conjunctiva, so, they cannot seen externally.
Dr. Najah
Lecture: 4 & 5
2
Innervations of the recti: medial, inferior and superior recti are innervated by
oculomotor nerve, the lateral rectus in innervated by abducent nerve.
Action:
- Medial rectus: Adduction.
- Lateral rectus: Abduction.
- Superior rectus: elevation (primary action) and intortion (2
nd
action) in primary
position of the eye. It is pure elevator in abduction and pure intorter in adduction.
- Inferior rectus: depression (primary action) and extortion (2
nd
action) in primary
position of the eye. It is pure depression in abduction and pure extortion in
adduction. So. the best position to examine superior and inferior recti muscles is
abduction to assess elevation and depression respectively.
The Oblique muscles:
- Inferior oblique: originates from angle between medial and inferior walls of orbit
posterior to inferior orbital margin just lateral to the lacrimal sac, and then it passes
below the eyeball and laterally to be inserted on the posterior lower temporal
quadrant of eyeball (posterior to equator).
* It is inserted at area corresponding to macula and any aggressive manipulation for
this muscle during operations might lead to macular hemorrhage.
- Superior oblique: originates from roof of orbit just superior to annulus of Zinn,
passes forward and medially to the angle between the roof and the medial wall to be
reflected by passing through the trochlea and then directed backward, downward and
laterally to be inserted in the posterior upper temporal quadrant.
Innervation:
- Inferior oblique: Oculomotor nerve.
- Superior oblique: Trochlear nerve.
Action:
- Inferior oblique: extortion (primary action) and elevation (2
nd
action) in primary
position of the eye. It is pure elevation in adduction and pure extorter in abduction.
- Superior oblique: intortion (primary action) and depression (2
nd
action) in
primary position of the eye. It is pure depressor in adduction and pure intorter in
abduction. So the best position to examine inferior and superior obliques muscles is
adduction to assess elevation and depression respectively.
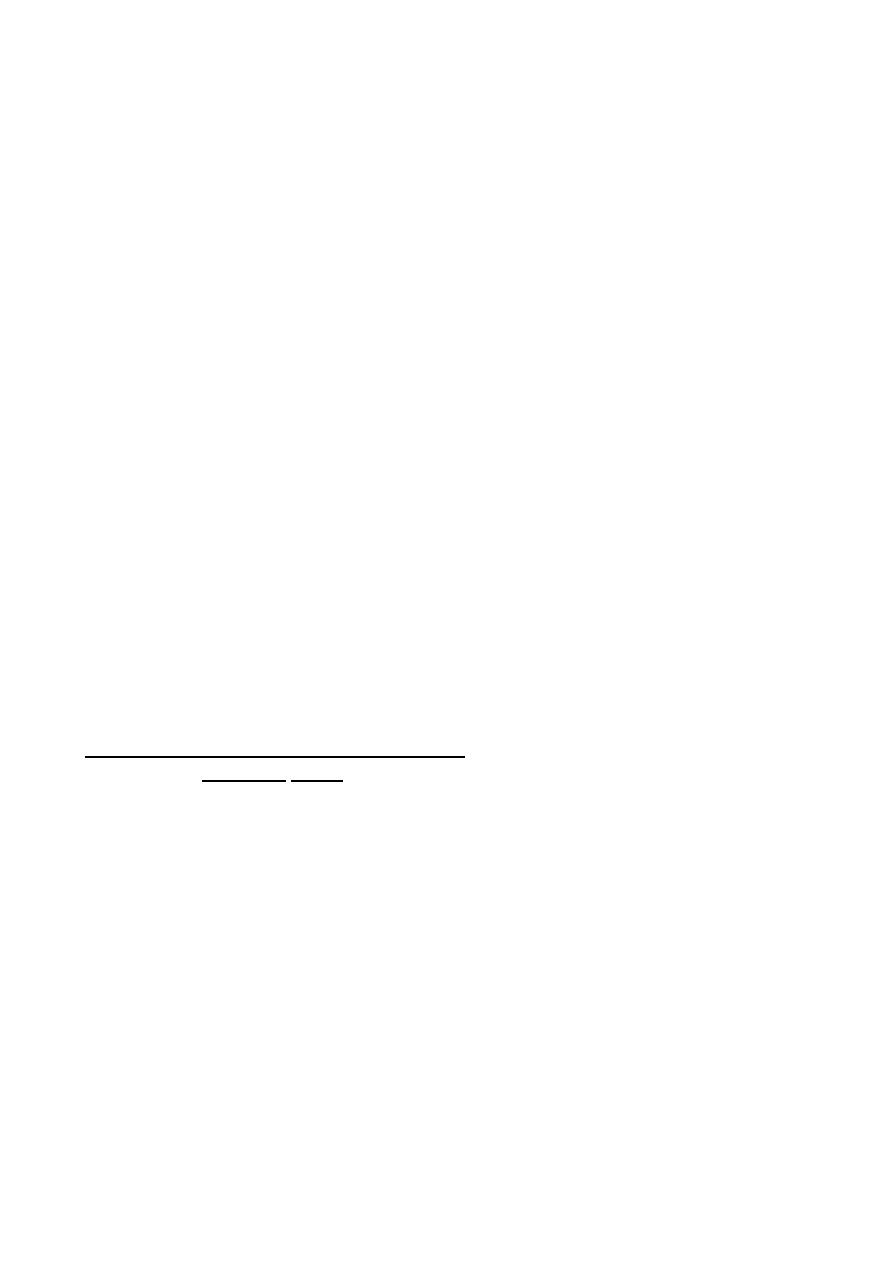
Insertion of eye muscles onto the
right eye. Note position of the optic
nerve (ON); its center is just above
the horizontal meridian. Position of
the macula (X); long ciliaries (C);
vortex veins (V); superior oblique
(SO); ora serrata (ORA); inferior
oblique (IO); medial rectus (M);
lateral rectus (L); inferior rectus (I);
superior rectus (S).

3
* For movement of one eye, the terms "Adduction" (for inward movement) and
"Abduction" (For outward movement) are used.
* For simultaneous movement of both eyes, the terms "Dextroversion" (for
movement to right) and "Levoversion" (for movement to left) are used.
* Combined movement are: dextro-elevation, dextro-depression, levo-elevation and
levo-depression.
Squint:
is a misalignment of the visual axes.
Visual axis: is a line between the point of fixation and the fovea passing through
nodal point. The normal visual axes intersect at the point of fixation.
The squint is either: Manifest (-tropia): is a squint present when both eyes are open.
Or: Latent (-phoria): is a squint seen only when one eye is covered.
* Latent squint is not seen normally when both eyes are open, but it can be seen only
when one eye is covered by occluder duo to interruption of fusion compartment of
binocular single vision. Corrective movement of this deviated eye is occur
immediately if the occluder is removed.
* squint (tropia or phoria) is either Eso-= inward, Exo-= outward, Hyper-=
Elevation, Hypo-= depression according to the direction of deviated eye.
Manifest squint is of two types:
1- Comitant (or Concomitant): when the angle of squint is the same in all
directions of gaze.
2- Incomitant (paralytic): when angle of squint varies in various direction of gaze
and it become larger in the direction of paralytic muscle.
Comitant squint:
It can be:
1- Uniocular: same eye deviate all the time and the fellow eye always fixated.
2- Alternating: each eye fixes and deviates alternately.
Acquired comitant esotropia:
Classification of comitant esotropia: which can be accommodative or non
accommodative depend on where the accommodation having role or not.
1- Accommodative esotropia: related to accommodation, starts at age of 6 months
to 5 years and mostly at age of 2 years. It is divided into:
a- Refractive accommodative esotropia with a normal AC/A ratio (which is
normally, 4 prism Δ accommodative convergence for each 1Diopter of
accommodation) is a physiological response to excessive hypermetropia (usually
4
between +4 and +7 D). For example, a 4-year old boy has a refractive error of +5 D
in each eye. Without spectacles there is esotropia measures 20 Δ (4 Δ /1D). As
spectacles control the deviation for distance and near, the esotropia is of the fully
accommodative type. In these cases the eyes usually remain straight with spectacles
and surgery is not required and has no role.
b- Non-refractive accommodative esotropia is associated with a high AC/A ratio
(> 4 Δ /1D) e.g. (10 Δ /1D). The refraction is usually normal for the age of the child
(1.5 -3.0 D) and there is little or no deviation for distance, but there is a significant
esotropia for near. It is corrected by bifocal glasses (Its upper part is made of 0 D
glasses (for distant) and has a lower part of 3D, to avoid accommodation for near).
c- Mixed accommodative esotropia: caused by the 2 mechanisms above, and it is
treated by bifocal lenses, its upper part has the refractive power which corrects the
hypermetropia for far and its lower part has additive 3D for near.
2- Non-accommodative esotropia:
- Essential infantile esotropia (congenital):
It is esotropia with onset since birth or during the first six months of life
- Convergence excess.
- Convergence spasm.
- Divergence insufficiency.
- Consecutive: patients with divergent squint who are underwent an operation for
correction of exotropia and ends with convergent squint due to overcorrection.
Management of Accommodative esotropia:
(refractive, non-refractive and mixed)
Aims of management of child with Squint:
1- Restore binocular single vision (BSV).
2-
Cosmetic
.
`
a- History:
- Diplopia: it means squint develop in old children age when there is development
of BSV. If squint develops early in life there is suppression and ignorance of the
central nervous system to the image coming from squinting eye. Continuous
suppression leads to amblyopia called strabismic amblyopia.
- Age of onset. Most of congenital need surgery while many cases of acquired can
be treated with spectacles because it is related to the use of accommodation.
- General health. Other systemic diseases should be excluded prior to surgery if
needed and also other neurological diseases which are can be associated with
squint.
- Family history. We should search for any previous family history of squints and
the way of their treatment because the recent case is most likely corrected by the
same way.
- Way of delivery: forceps delivery may cause 6
th
nerve palsy.

5
b- Visual acuity: it is the corner stone, as our aim in management of child with
squint is to restore his binocular single vision (BSV). Good VA in both eyes are
mandatory for development of BSV.
* Binocular single vision is represented by simultaneous perception at level of
retinae, fusion of image at level of occipital cortex and stereopsis (sense for depth).
BSV is affected in squinting child even if the visual acuity is 6/6 in both eyes ( e.g.
alternating squint), because the child using the one fixating eye at one moment and
don’t using both eyes simultaneously.
c- Motor examination: to exclude nerve palsy and other congenital abnormalities
of muscles.
d- Refraction: for assessment and determining its type and the way of treatment
(e.g. there is refractive error or not). This is done objectively by using retinoscope
or autorefractrometer instrument under complete cycloplegic effect by using
atropine or cyclopentolate or homotropine.
e- Fundoscopy: to exclude retinal diseases e.g. retinoblastoma, congenital optic
disc anomaly, and macular hypoplasia.
f- Correction of amblyopia: occlusion or penalization.
i- Correction of refractive errors: by giving the patient spectacles.
ii- Occlusion of the fellow eye: this is done to inforce the amblyopic eye to send
stimulus to CNS by occlusion the fixating eye in uniocular squint. In this method,
occlusion of the normal eye is usually done for 1week/1year of age of the child,
and then opening of the eye should be done at least for three days. This maneuver
can be repeated many times until improvement of VA to its normal level (6\6).
Don’t forget that continuous occlusion of normal eye without rest and for long
time can lead to another more serious type of amblyopia in this eye called
deprivation amblyopia which is more serious than strabismic amblyopia .
iii- Penalization: it means partial occlusion to normal eye by daily instillation of
cycloplegic drugs (mostly atropine), which leads to blurring of vision. This is
done instead of occlusion if the amblyopia is mild.
g- Surgery: if the squint is not corrected or corrected partially by contiuous
wearing of spectacle for 2 to 3 months, the residual angle should be corrected by
surgery (recession and resection). In recession (weakening), the muscle from is
disinsert from its normal insertion and reinsert into a new site more far posteriorly
from the limbus, while in resection (strengthen), cutting of a part or all the tendon
or may be part of muscle itself with its tendon and re-insert the muscle in its normal
insertion site.
* In alternating squint, the surgery done depends on the severity of squint, so we
may do:
- Unilateral medial rectus recession (weakening).

6
- Bilateral medial rectus recession (weakening) with or without unilateral or
bilateral lateral rectus muscles resection (strengthening).
* In squint surgical correction, the child's parents should be informed that their child
might need more than one operation to get full correction.
Essential infantile esotropia (congenital):
Signs (or criteria):
a- Large angle.
b- Alternating in primary position and cross fixation in side gaze.
c- Usually associated with Nystagmus.
d- Not associated with refractive error.
e- Associated with inferior oblique overaction (if we have convergence, then
there will be elevation of the eye on adduction).
f- Usually it is squint per se, there is no neurological defect.
Management: the same way of accommodative esotropia but here the surgery is
most likely is the treatment and few cases are corrected by spectacles.
Treatment: bilateral medial rectus recession as soon as possible, but we have to
check for refractive errors (and correct any if found) and to do fundoscopy to
exclude retinal diseases as we do in all types of squint prior to surgery.
Exotropia (Divergent squint):
Classification:
1- Constant: see when both eyes are open all the time.
- Congenital.
- Sensory: This is usually associated with myopia.
- Consecutive: duo to surgical overcorrection of esotropia.
2- Intermittent: present in some times of the day and sometimes the eyes looks
normal (no squint). The diagnosis is just from the history taken from parents and
there may be no squint seen during the moment of examination. We should trust
parents in squint till improve otherwise because they live with the child 24 hours/
day and we examine him in few minutes.
- Divergence excess.
- Convergence weakness.
- Basic exotropia.
Congenital exotropia:
Signs:
1- Normal refraction.
2- Large and constant angle.
3- Usually associated with Neurological anomalies.
7
Treatment:
It is mainly surgical and done by bilateral lateral rectus recession ± resection of one
or two medial recti.
Intermittent exotropia:
Management:
1- Spectacles if associated with myopia or any other refractive errors.
2- Treatment of amblyopia.
3- Surgery: recession of both lateral recti.
Paralytic squint (Incomitant squint):
1- Congenital.
2- Acquired: palsy of 3
rd
, 4
th
or 6
th
cranial nerve or combination.
Surgery should not attempt till there is no hope for spontaneous recovery and this is
usually after 6 months to one year.
Pseudosquint:
Causes:
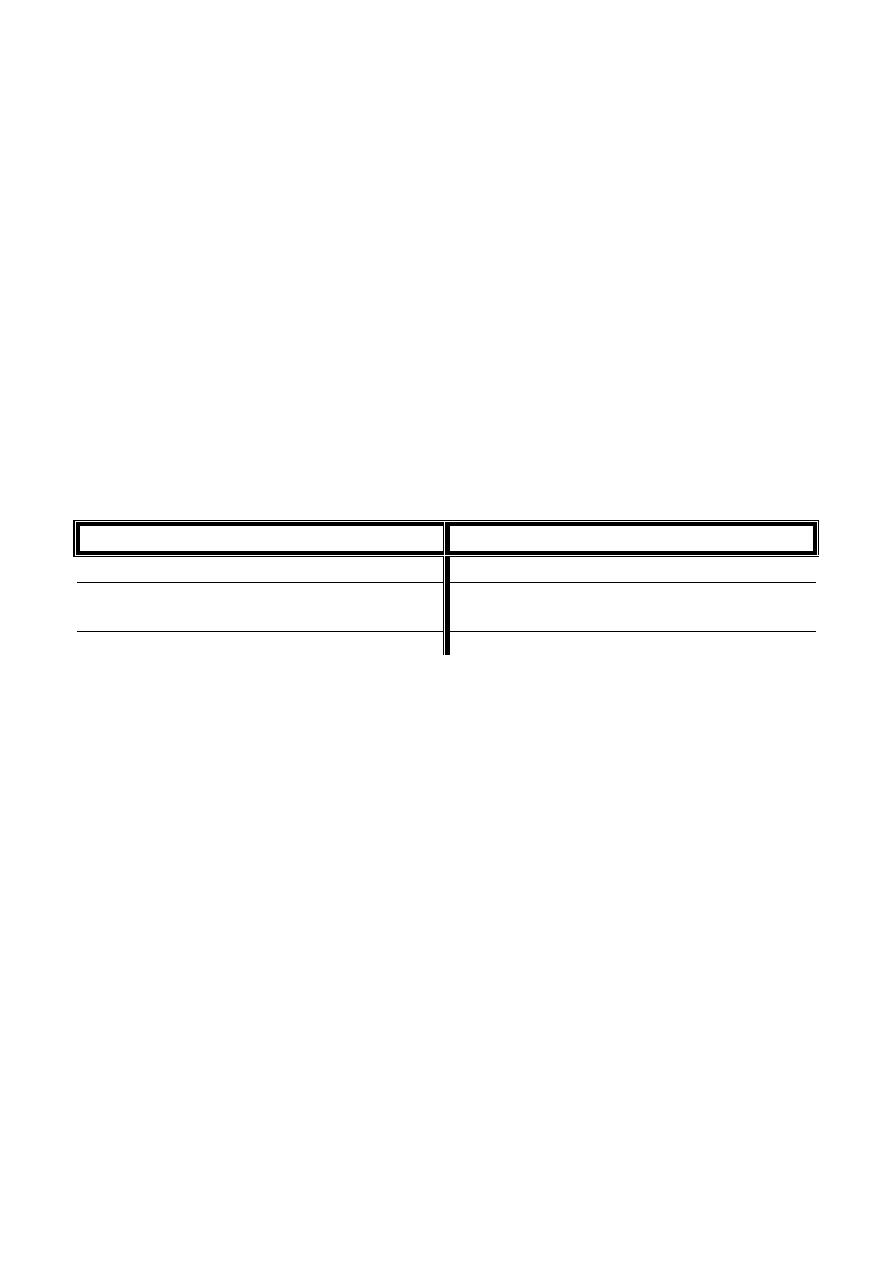
Convergent Pseudosquint
Divergent Pseudosquint
1- Small inter-pupillary distance
Wide inter-pupillary distance
2- Negative angle alpha e.g. myopia
Large
positive
angle
alpha
e.g.
hypermetropia.
3- Wide epicanthic folds



