Local Anesthetics
ByDr. HUSSAM .H.SAHIB , M.Sc
Local Anesthetic:
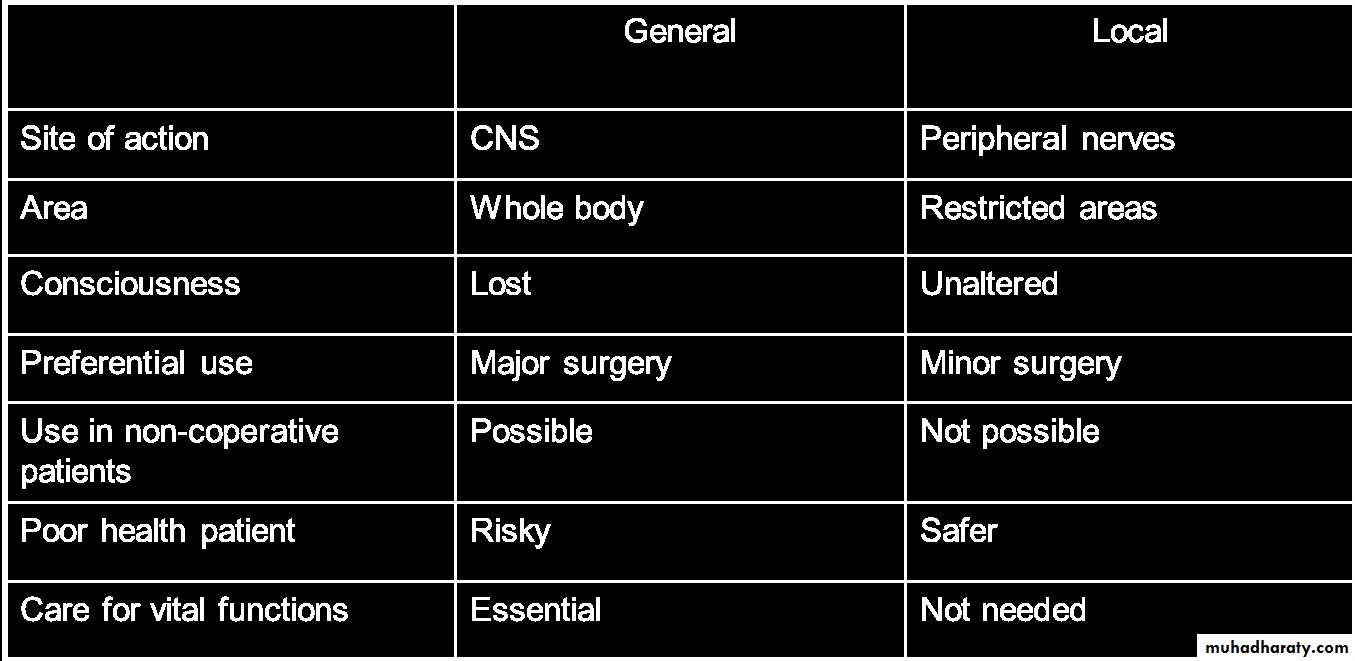
A local anesthetic is produce loss of sensation to pain in a specific region of the body without a loss of patient consciousness. Normally, the process is completely reversible .Local anesthetics desirable characteristics:
1.Rapid onset of action and duration of action should be sufficient to allow time for the surgical procedure.
2.Low degree of systemic toxicity.
3.soluble in water and stable in solution
4.Effective on all parts of the nervous system, all types of nerve fibers and muscle fibers. (When injected into tissue &when applied topically to mucous membranes).
5.It should not be irritating to tissue to which it is applied
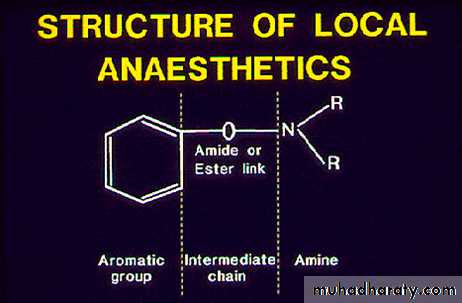
The LAs consists of three parts:
1.A hydrophilic amino group. 2. An intermediate chain (ester or amide).
3.A lipophilic aromatic group.
Mechanism of action:
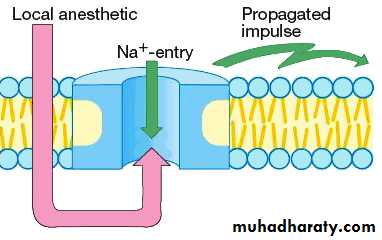
Local anesthetics block nerve conduction of sensory impulses. Na+ ion channels are blocked to prevent the transient increase in permeability of the nerve membrane to Na+ that is required for an action potential. When propagation of action potentials is prevented, sensation cannot be transmitted from the source of stimulation to the brain.Pharmacokinetics:
Absorption: When injected into soft tissue, most local anesthetics produce dilation of vascular bed. Cocaine is the only local anesthetic that produces vasoconstriction; initially it produces vasodilation which is followed by prolonged vasoconstriction.
Vasodilation causes increase in the rate of absorption of the local anesthetic into the blood, thus decreasing the duration of pain control.
NOTE: ALL LA Pass easily mucous membrane except Procaine which effective ONLY by injection
Esters:
They are hydrolyzed in plasma by pseudo-cholinesterase. One of the by-products of metabolism is paraaminobenzoic acid (PABA), the common cause of allergic reactions seen with these agents. Therefore, some people have allergic reactions to the ester class of local anesthetics.Amides:
They are metabolized in the liver to inactive agents. True allergic reactions are rare.
Lidocaine half life is 1.6 hr in normal person while more than 6 hrs in sever liver diseases.
ACTION:
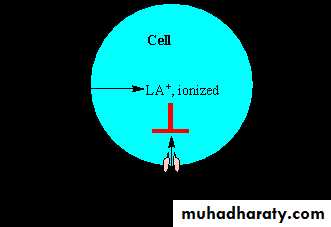
LA are weak bases and their activity increases by increasing PH, This because if large amount of a drug is nonpolar, it will facilitate its penetration through the cell membrane. Once the drug has penetrated the lipid barrier and reaches its site of action it ionized and the ionized form is responsible for LA activity.Acidosis such as caused by inflammation at a wound partly reduces the action of local anesthetics. This is partly because most of the anesthetic is ionized and therefore unable to cross the cell membrane to reach its cytoplasmic-facing site of action on the sodium channel.
Factors affecting on local anesthetic action:
1-Lipid solubilityIncreasing the lipid solubility leads to faster nerve penetration, block sodium channels, and speed up the onset of action.
More lipophilic agents are more potent as local anesthetics.
The more tightly local anesthetics bind to the protein, the longer the duration of onset action.
2-pH influence
Decrease in pH shifts equilibrium toward the ionized form, delaying the onset action.
Lower pH, solution more acidic, gives slower onset of action
3-Vasoconstrictors
Vasoconstrictors decrease the rate of vascular absorption which allows more anesthetic to reach the nerve membrane and improves the depth of anesthesia. consequences of including vasoconstrictor:Prolongation of anesthetic action, decreased risk of toxicity and decrease in bleeding from surgical manipulations
epinephrine appears to be the best vasoconstrictor.
4-Inflammation: tends to produce lower pH in tissues therefore:
are more ionized - don’t penetrate very well so decreased ability of LA to produce effects.
All local anesthetic agents readily cross the blood-brain barrier, they also readily cross the placenta.
Thank you
Any question?• P H R M A C O L O G Y - NOTE 8 - Local Anesthesia
• Amide• • Mepivacaine
• 25
• ءاعدلا مكلأسن |
• • produce local loss without loss of
• consciousness
• • Tetracaine
• • Lidocaine
• (Xylocaine)
• • Bupivacaine
• • Etidocaine
• LOCAL ANESHESIA
• weak Potency & short Duration• moderate Potency & intermediate
• Duration• high Potency & long Duration
• Lidocaine (Xylocaine)• Tetracaine
• Procaine• Chloroprocaine
• Mepivacaine
• Bupivacaine• LA of sensation
• Prilocaine
• Etidocaine• • Procaine
• • Chloroprocaine• Esters • Benzocaine
• Ropivacaine
• • Benoxinate• P H R M A C O L O G Y - NOTE 8 - Local Anesthesia
• vasoconstrictors.• (Xylocaine)
• o as in (wound suturing, cyst removal).
• o as in Dental anesthesia.
• o as in surgery of (LL, abd, pelvis,
• 4)
• Treatment of cardiac dysrhythmia.
•
• NO mydriasis.
• duration
• 26
• ءاعدلا مكلأسن |
• DRUG
• PHARMACOKINETIC
• ACTION
• USES
• SIDE EFFECT
• Weak Potency &
• short duration
• Procaine
• Administration
• Local injection.
• Local application ( solution, powder or cream)
• Absorption
• NOT desirable because:
• It duration.
• It systemic side effects.
• Metabolism
• Easter, fastly metabolized by tissues &
• plasma esterase.
• Into PABA (cause allergy).
• Short duration.
• Amides, slowly metabolized by liver microsomal enzymes.
• Longer duration.
• .
• Mechanism of action
• LA block nerve conduction (initiation
• & propagation of AP) by:
• Binding to Na+ channels &
• prevent Na+ permeability.
• Action
• LA are lipid soluble / weak base.
• At pH= 7.4,
• o they are UNIONIZED molecule.
• o They pass lipid membrane.
• When reach the cytoplasm,
• o They become (ionized +
• unionized).
• o The IONIZED molecules:
• Bind to Na+ channels.
• Block Na+ influx.
• Prevent AP.
• The action are susceptible for (small diameter / unmylinated) fibers more than (large diameter / mylinated) fibers.
• 1) Surface anesthesia:
• o on Skin (wound & ulcer)
• o on MM (mouth or nose).
• o in Ophthalmology (corneal A).
• o powder, solution creams or ointment are used.
• 2) Infiltration anesthesia.
• o as in (wound suturing, cyst removal).
• 3) Individual nerve block anesthesia.
• o as in Dental anesthesia.
• 4) Spinal Epidural anesthesia.
• o as in surgery of (LL, abd, pelvis, rectum).
• 5) Treatment of cardiac dysrhythmia.
• Usually minimum, because:
• o Applied locally.
• o Combinewd with
• 1) Hypotension.
• 2) Bradicardia.
• 3) CNS:
• Tinnitus.
• Lightheadness.
• Headache.
• Convulsion.
• 4) Allergy (in ester type).
• Side effects occur due to:
• o High dose.
• o Injected into BV.
• They are potent & have long duration.
• Chloroprocaine
• Moderate Potency
• & Intermediate duration
• Lidocaine
• Mepivacaine
• Prilocaine
• High Potency &
• long duration• Tetracaine
• 1) Infiltration anesthesia.
• 2) Individual nerve block anesthesia.
• 3) Spinal Epidural anesthesia.
• rectum).
• Bupivacaine
• Etidocaine
• Ropivacaine
• Benoxinate
• It is ester LA.
• In ophthalmology for corneal A because :
• NO corneal injury.
• Benzocaine
• Used as powder or cream.
• Because it is insoluble, it produces less systemic toxicity.
• Surface anesthesia on Skin (wound & ulcer)
•
• INFLUENCING FACTORS
• IF
• Advantage
• Disadvantage
• 1
• Dosage
• High
• Fast onset / long duration
• side effect
• 2
• Site
• BV
• side effect / Short duration
• 3
• Lipid solubility
• LS
• effect
• 4
• Infection/
• inflammation
• pH
• action / ionized /effect
• Vaso- dilation
• absorb / side effect/
• 5
• Type of solution
• Alkali
• Less painful / fast onset /
• non-ionized / action / effect
• 6
• + vasoconstrictors
• duration/ absorb /side effect