Radiology L1 : د.منى عبالغني
Respiratory system
Normal chest
The imaging technique of investigation of respiratory system :
-
1. Plain x- ray film .
-
2. CT scan (computerized tomography).
-
3. U/S : witch used for evaluation of chest wall & plural lesion(particularly plural effusion )
& lung lesion adjacent to the chest wall, its can be very useful to guiding needle to sample or
drain loculated plural fluid collections and for needle biopsy / aspiration cytology of masses in
contact with chest wall .
-
** for chest wall US use the linear probe
-
4. Magnetic resonance imaging (MRI ) : has Limited role in the pulmonary , plural &
mediastinal disease
-
5. Radionuclide imaging : used for diagnosis or exclude of suspected pulmonary embolism in
CT angiogram , there are two types of radionuclide lung scans , perfusion & ventilation scan.
-
6. Pulmonary angiography: used for DX of pulmonary embolism.
Plain x- ray examination:
The most frequently requested radiological examination , visualization of the lungs is excellent
because of inherent contrast of tissue of thorax .
-
PA view : patient faces the film with chin up with shoulder rotated for ward to displace the
scapulae from lungs , exposure is made in full inspiration .
Lateral view : usually is the LT lateral is used to decrease the heart magnification., is not
routinely requested, only when there is abnormality in the PA view need to be further evaluated ,
patient stand with shoulder parallel to the film & arm elevated
-
Other views:
a.
AP view :
used for patient unable to stand or when using portable radiograph , and when
the patient is child
the differences of it from PA view.
-
Ribs projected over different areas of the lung from the PA view
-
Posterior chest is well shown .
-
Scapulae over lie the upper lungs .
-
The clavicles projected above the apices .
-
Magnification of heart shadow.

Radiology L1 : د.منى عبالغني
b.
Supine & decubitus position : for detection of small plural
effusion.
c.
Oblique view: used for - Posterior cost phrenic angle.
-
Rib lesion e.g. fractures.
-
Calcified plural plaques.
d.
Inspiratory & expiratory film: used for detection of air trapping 1 in children
for DX of inhaled foreign body.
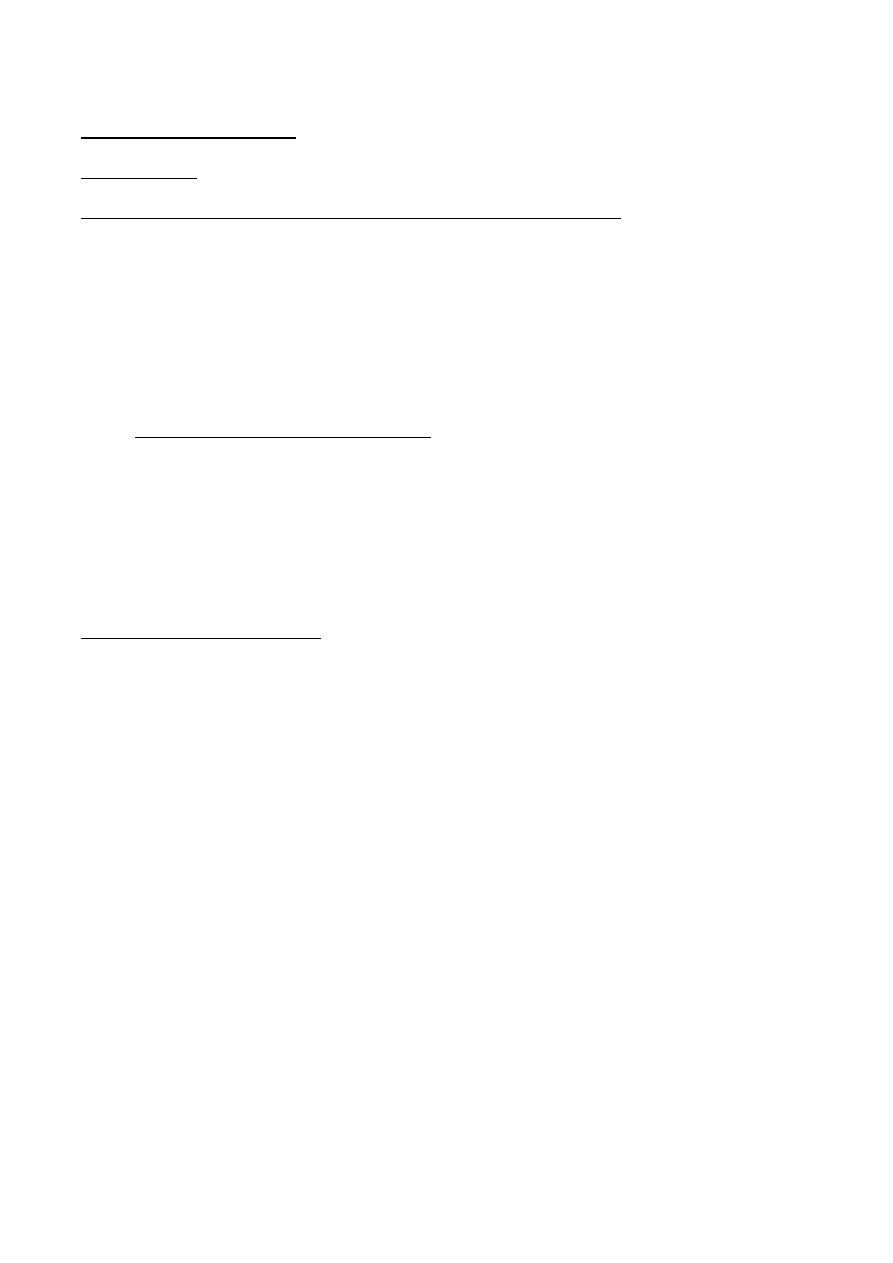
viewing of PA view:
Before DX of abnormality if present knowledge of
normal appearance of chest radiograph is essential , points should be evaluated
routinely including:
-
* Technical factors including
a.
centering : the medial end of clavicles should be equidistance from .the
vertebral spinous process at T4- T5 level
b.
orientation of the aortic arch , gastric bubbles & heart should be assessed to
confirm normal situs & side markers puted are correct
c.
adequate inspiration : film should take in full inspiration i.e the anterior end
of sixth rib or posterior end of the tenth are above the RT hemi diaphragm
d.
Trachea
: central or deviated to the RT normally, should examined for
narrowing , displacement , maximum coronal diameter is 25 in mal , 21 mm in the
female, normal carinal angle 60 - 75 degree
* Mediastinum & heart:
The out line of mediastinum and heart should be clearly seen except when the heart
lies in contact with diaphragm , the RT superior mediastinal border is usually
straight or slightly curved , the LT superior mediastinal border is ill defined above
the aortic arch , with increasing age the aorta elongate causing
unfolding of the aorta
, the unfolding result in the ascending aorta deviating to the right & descending
aorta to the LT, in young children , the normal thymus is often clearly visualized
and sometimes it very large.
Central dense shadow seen in the PA view comprised mediastinum , heart , spine,
sternum.
With good centering two third of cardiac shadow seen to the LT of mid line , one
third to the RT.
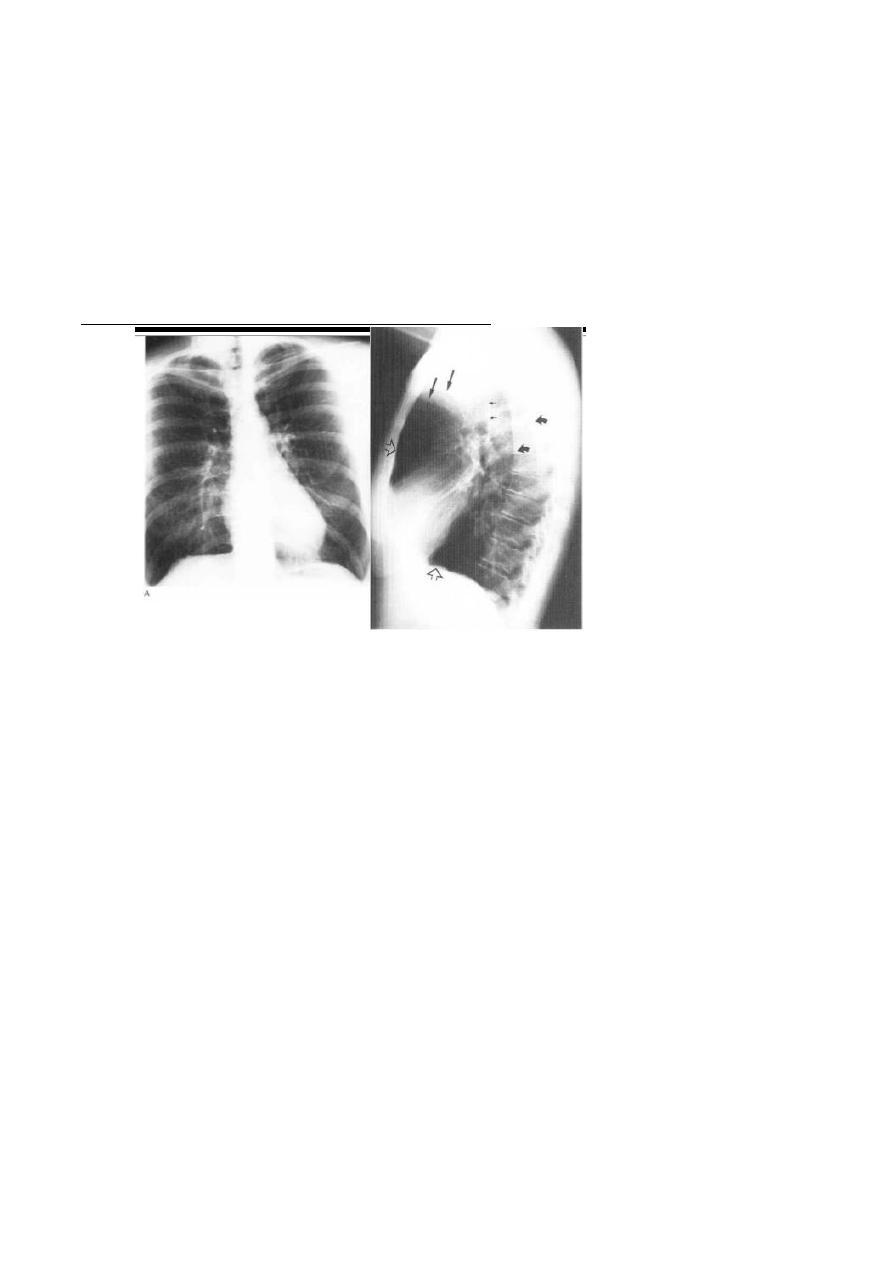
C.T.R is transverse cardiac diameter
Transverse thoracic diameter
Normally less than 50 % for adult.
Normally less than 60 % for infant & young children .
Heart should be evaluated for shape , size & orientation of the apex.

Radiology L1 : د.منى عبالغني
-
Diaphragm:
The upper surface of the diaphragm should be clearly visible from one
costopherenic angle to the other ,except when the heart and mediastinum are in
contact with the diaphragm.
In most population the RT hemi diaphragm higher than the left this is due to the
heart depressing the LT side, but difference should be up to 2.5cm , loss of the
outline mean adjacent tissue doesn’t contain air e.g consolidation or plural effusion.
-
Costo phrenic angle: normally acute & well defiend.
-
Lungs :
by comparing the two lungs zones ( upper, middle
, lower) areas of abnormal translucency or uneven distribution of lung marking are
most easily detected.
-
The hila:
-The hilar shadows represent the pulmonary arteries & veins.
In 97% of subjects the LT hilum is higher than the RT .
Hila should be of equal density & similar size.
Clearly defined concave lateral border.
-
Examination of the lungs
The only structures that can be identified within the normal lungs are the blood
vessels , the inter lobar fissures , and the walls of certain larger bronchi seen end on ,
the only fissure seen in frontal view is the horizontal fissure ( minor fissure ) which
running from the RT hilum to the six rib in the axilla , oblique fissure ( major fissure
) are only visible on the lateral view, in about 1% of population there is an extra
fissure visible on the frontal view -the so called azygos lobe fissure, look for
abnormal pulmonary opacities or translucencies, good method of finding subtle
shadows on the frontal film is to compare one lung
with other, zone by zone.
-
- Below the diaphragm;
Any abnormal gas shadow such pnemoperitoneum , chiliditi syndrome, abscess
-
-Soft tissue of the chest:
-The bones sternum, clavicles, scapulae, ribs.
Radiology L1 : د.منى عبالغني
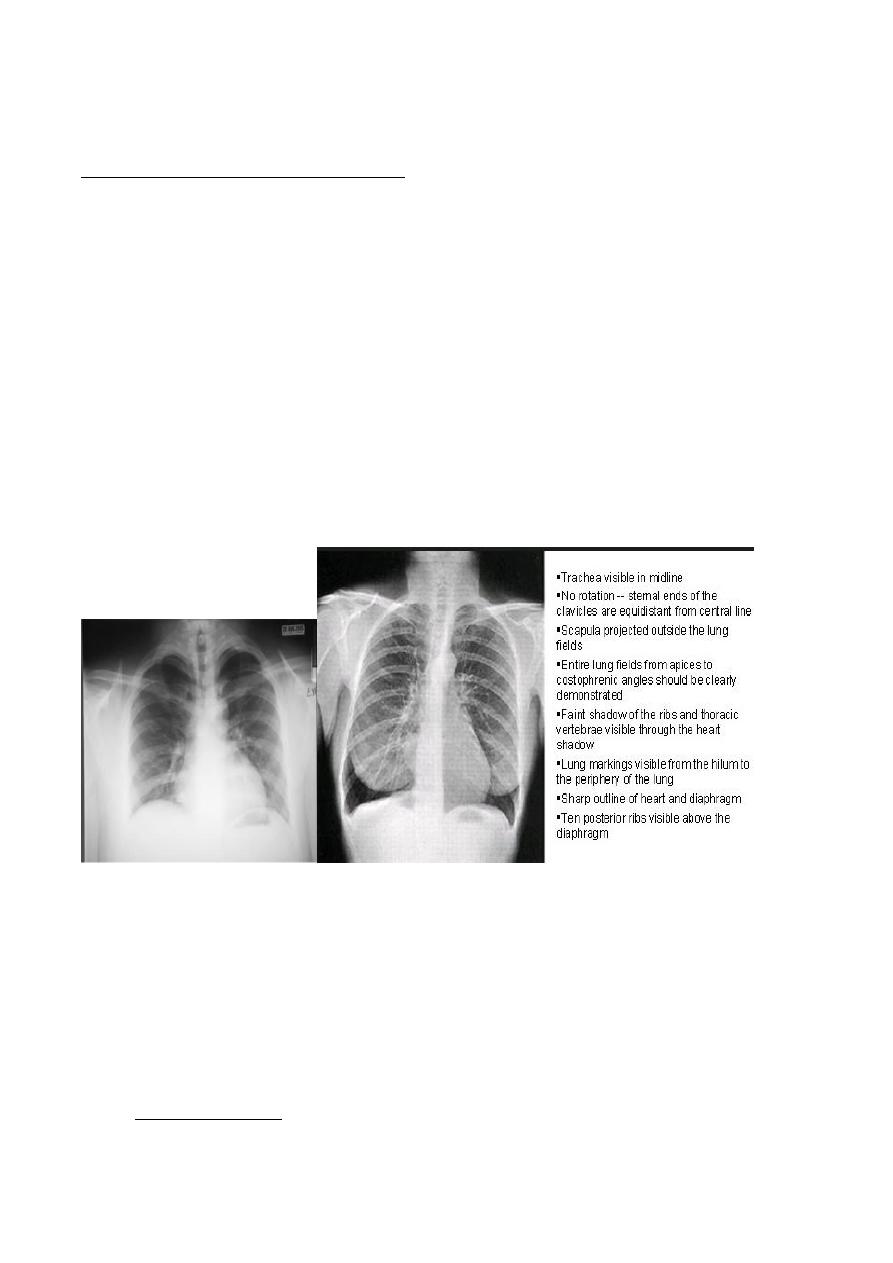
Viewing of the lateral film:
The LT lateral is the routine
The important points to evaluated ;
-
- Clear spaces
a. Retrocardiac space b. retrosternal space; both translucent , loss of this
translucency indicate local pathology , obliteration of retrosternal space occurs
in the anterior mediastinal masses such as thymoma, nodal mass.
-
- Vertebral translucency :
The vertebral bodies
become
progressively more
translucent
caudally, loss of this translucency occurs in the posterior basal lesion (
consolidation).
-
- Diaphragmatic outline :
Posterior ■ costo phrenic angles are acute & small amount of Plural fluid may be
detected by blunting of this angles.
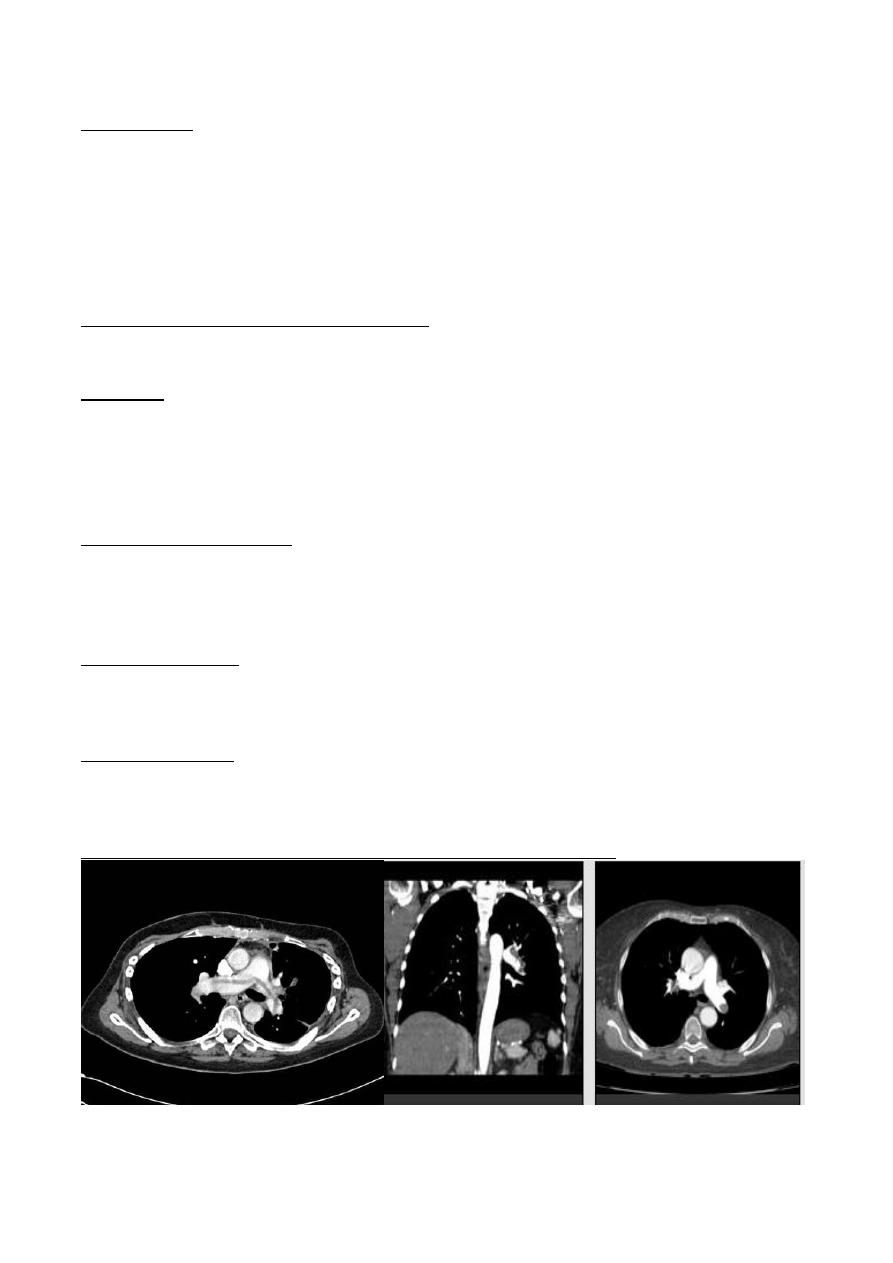
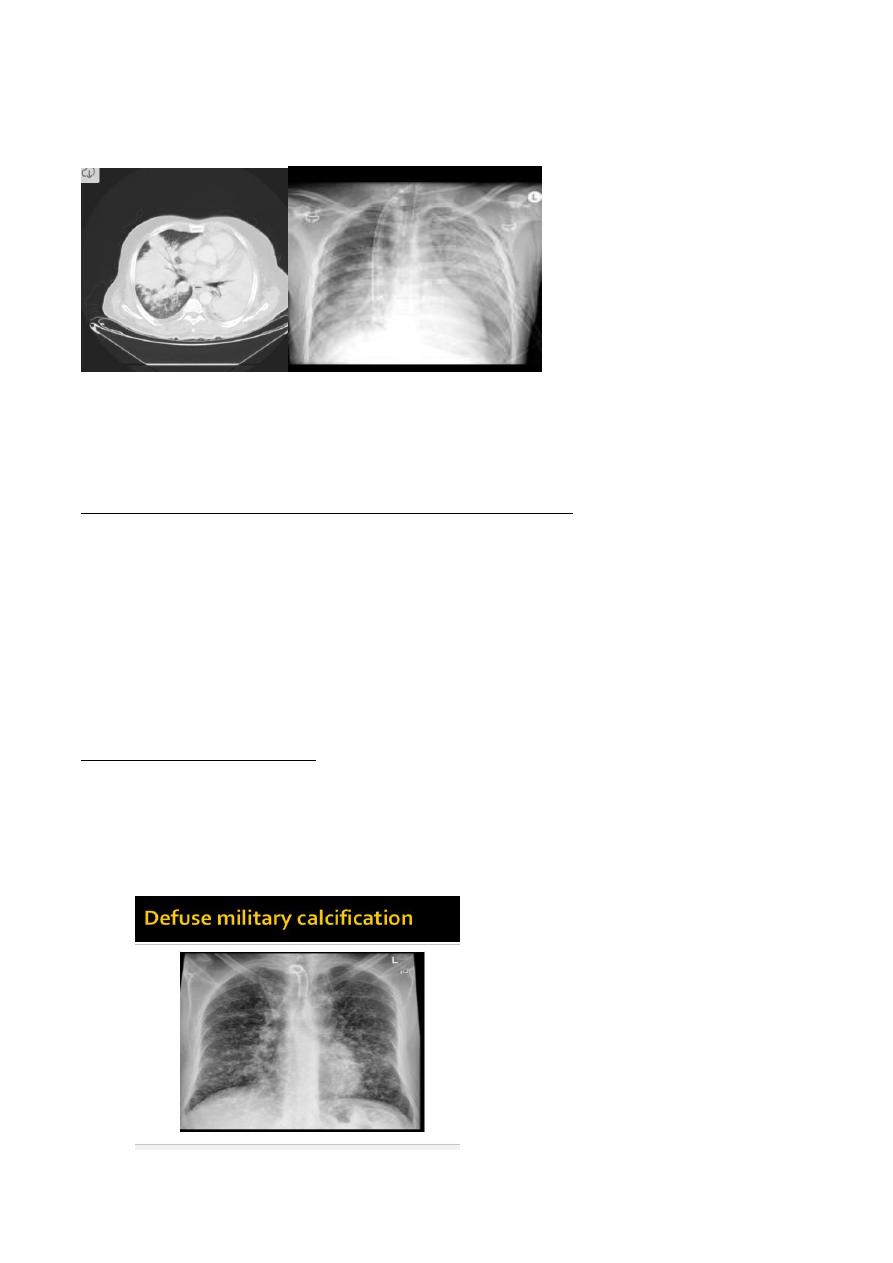
CT scan of the chest
It is cross sectional x-ray imaging modality consisting of contiguous sections, spiral
CT scan of great benefit of imaging of the thorax involving continuous rotation of x-
ray tube & smooth passage of the patient through scanner aperture, the images are
usually viewed at both mediastinal & lung window setting, thin sections can be
used to produced images with higher spatial resolution -so called high resolution CT
(HRCT ) which, allows details of pulmonary parenchymal disease and
bronchiectasis to be shown.
-
Indication of CT scan in the chest including:
e.
Staging malignancy. particularly lung cancer & lymphoma .
Radiology L1 : د.منى عبالغني
f.
Detecting pulmonary metastasis
g.
Assessing chest wall & plural lesions
h.
Assessment of hilar & mediastinal abnormalities seen in the plain film.
i.
High resolution C.T scan used in DX of early stages of diffuse lung diseases
when chest radiograph normal.
j.
Detecting bronchiectasis .
k.
Diagnosis pulmonary emboli using CT pulmonary angiography.
Comparison between adult and child chest
1. The child chest is in small size in relation to heart because that the chest inflated little
by little with time while heart of child when birth is highly specialized because the
lung depend on circulation
2. lateral view : lateral border of chest if look to sternum we have 2 important
chambers which are retro cardiac and retrosternal space , normally in adult the
retrosternal space just see the lower third of it attached to Rt. Ventricle and the other
is free so see the posterior border of sternum but in child the posterior of sternum
not seen
heart border :
1. left border : formed by left ventricle
2. Right heart border : formed by Rt. Atrium
3. Anterior heart border : formed by Rt. Ventricle
4. Posterior heart border : formed by Lt. atrium
3. In superior mediastinum in child we found the thalamus gland so wide anterior
mediastinum is normal in children
4. When take the pain X-Ray for children we have as AP and nor PA because the child
is not cooperative
Radiology L1 : د.منى عبالغني
Diseases of chest with normal chest radiograph
Serious respiratory disease may exist in patients who have a normal chest
radiograph. Sometimes it is only possible to detect abnormality- by comparison with
previous or later examinations, e g subtle pulmonary- shadows from infection or
pulmonary fibrosis. Chest disease with a normal chest radiograph occurs in:
Obstructive airway disease
Asthma and acute bronchiolitis may produce over inflation of the lungs. but in
many cases the chest film is
Emphysema, when the disease is moderate, the chest rad graph may be normal or
very nearly so. Uncomplicated acute or chronic bronchitis does not usually produce
a radiological signs, so if a patient with chronic bronchi has an abnormal film, some
other disease or a complicate has developed, e.g. pneumonia or cor pulmonale.
Many patients with productive cough duo to bronchiectasis show no plain film
abnormality
Radiology L1 : د.منى عبالغني
Small lesions
is usually impossible to see solitary lung masses or consolidations of less than I cm
in diameter* Even 2-3 cm lung cancers may be very difficult to identify on routine
films if they are hidden by ribs or clavicles or if they lie behind the heart or
diaphragm,
endobroncheal lesions, such as carcinoma, cannot be diagnosed on routine films
unless they cause collapse/consolidation.
Pulmonary emboli without infarction
The chest radiograph is often normal even when life-threatening emboli are present
Infections
Most patients with acute bacterial pneumonia present with recognizable
consolidation, but in other infections, notably Pneumocystis carinii pneumonia,
obvious pulmonary consolidation may only develop after the onset of symptoms.
Patients with military tuberculosis may initially have a normal chest film.
Diffuse pulmonary fibrosis
Widespread pulmonary fibrosis may be responsible for breathlessness with
substantial alteration in lung function tests before any clear-cut abnormalities are
evident on chest radiographs.
Pleural abnormality
Dry pleurisy does not produce any radiological findings and small amounts of
pleural fluid may be impossible to recognize on standard PA and lateral chest films.
Mediastinal masses
Plain chest radiography is very insensitive for the diagnosis of mediastinal masses,
lymph node enlargement and mediastinal fluid collections.
Male pt. presented with sudden onset of pleuritic chest pain
Radiology L1 : د.منى عبالغني
This patient have normal x-ray and its mean that the pain is combined with
inspiration or expiration and with exercise and cough (one of presentation of normal
chest radiology)
Radiological signs of lung diseases
Air space filling
Means the replacement of air in alveoli by fluid or rarely by other materials ( infiltrate ) .
the fluid can be exudate ( consolidation ) or transudate ( pulmonary odema )
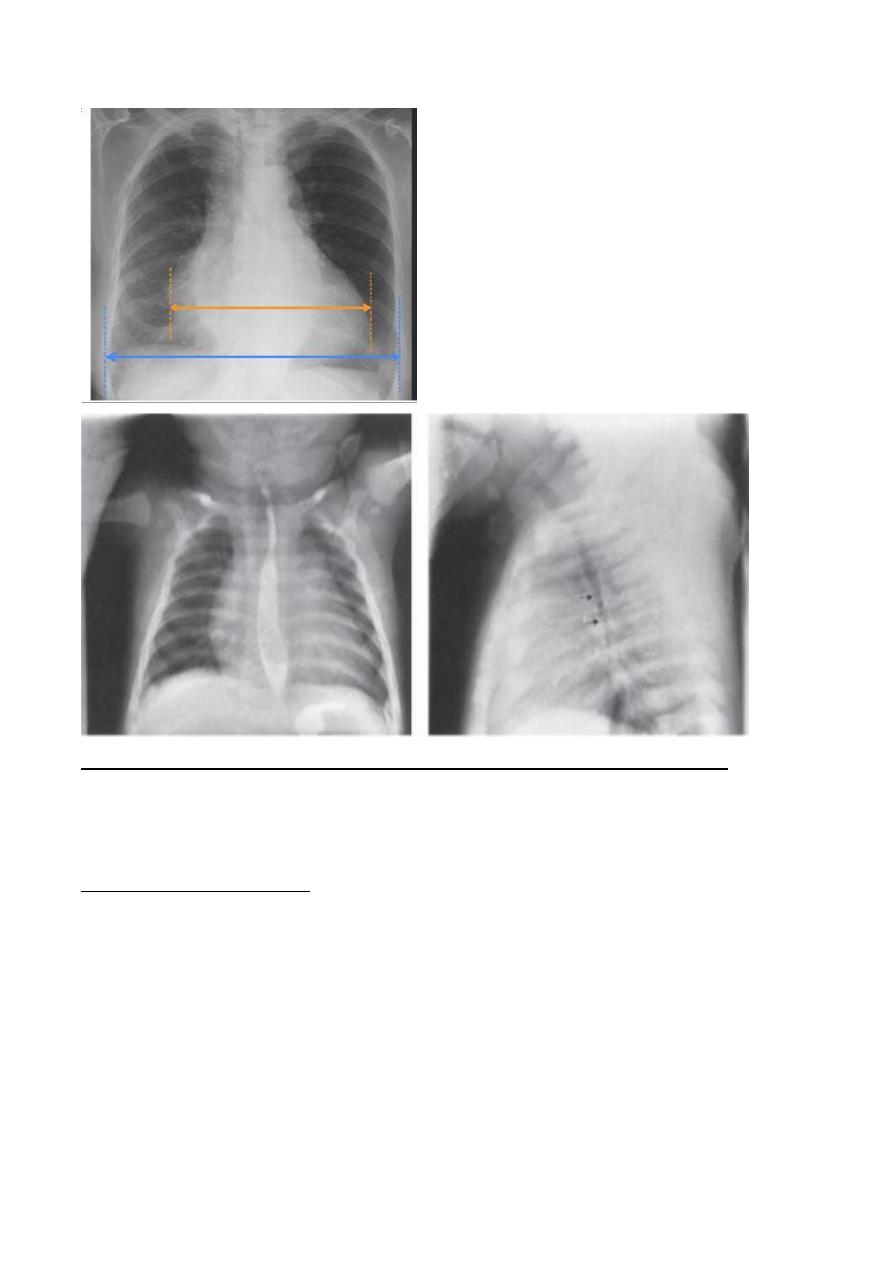
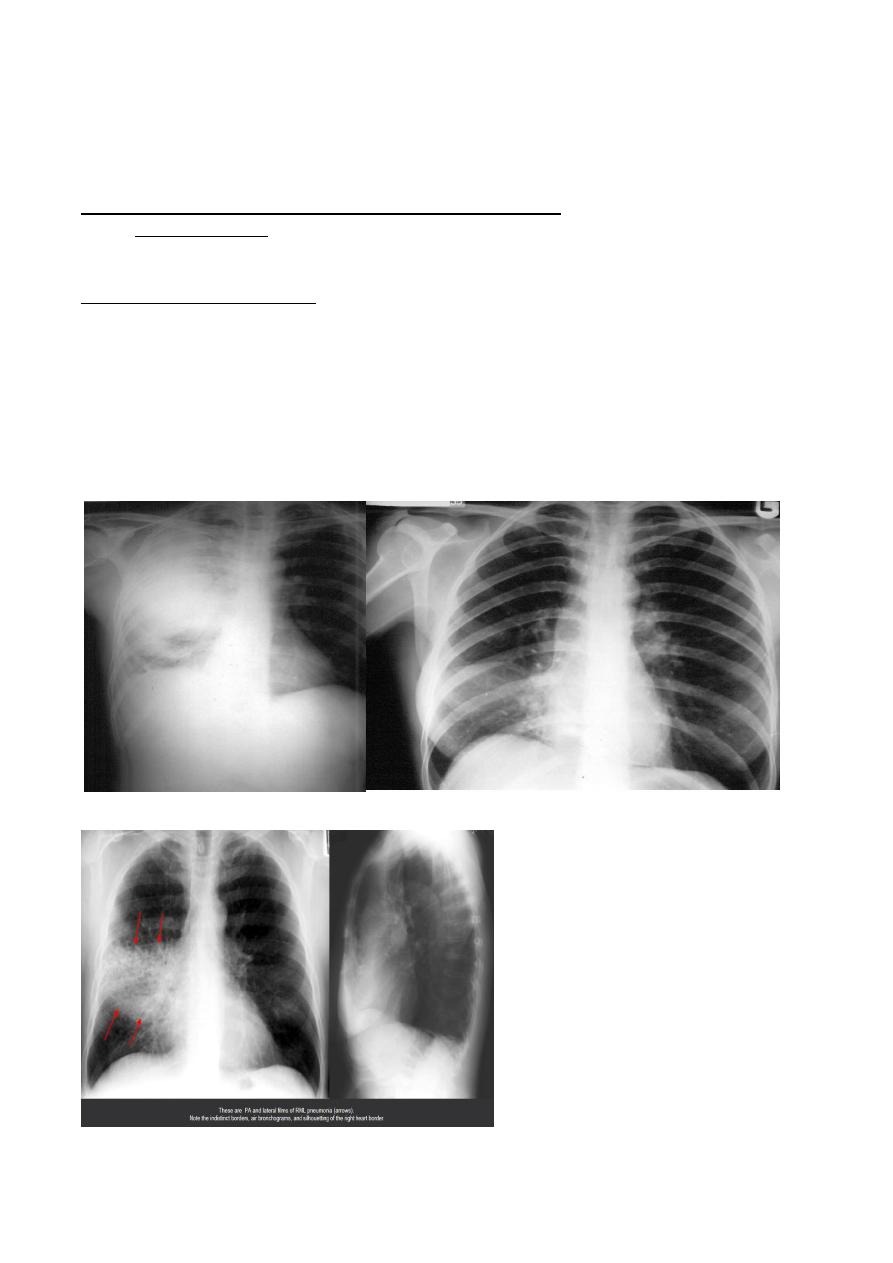
1. The signs of consolidation :
:
1. A shadow with ill-defined borders except where the opacity is in contact with a fissure, in which
cat the shadow has a well-defined edge.
2. An air bronchogram :Normally, it is not possible to identify air in bronchi within normally
aerated lung because the walls of the normal bronchi are too thin and air filled bronchi are
surrounded by air in the alveoli, but if the alveoli are filled with fluid, the air in the bronchi
contrast with the fluid in the adjacent lung. This sign is seen to great *d vantage on CT,
3. The silhouette sign, namely loss of visualization of the adjacent mediastinal or diaphragm
outline (Refers to loss of normal borers between thoracic structures , caused by an intrathorasic
radio- opaque mass that touches the border of the heart or aorta ex, in Rt middle lobe syndrome
the Rt heart border is obscured)
Middle lobe consolidation
Radiology L1 : د.منى عبالغني
4. Consolidation of a whole lobe, or the majority of lobe is virtually diagnostic of bacterial
pneumonia. Lobar consolidation produces an opaque lobe, except for air bronchograms. Because
of the silhouette sign, the boundary between the affected lung and the adjacent heart,
mediastinum and diaphragm is invisible.
5. Patchy consolidation, i.e. one or more patches of ill-defined shadowing, is usually due to:
pneumonia
infarction
contusion
immunological disorders.
6. There is no reliable way of telling from either chest radiographs or CT which of these
possibilities is the cause . in most instances the clinical and laboratory findings pointed to one
or other cause.
7. Cavitation ( abscess formation ) within consulated area in the lung may occur within many
fungal and bacterial infections . abscess formation can recognizable once there is communication
with the bronchial tree allowing the liquid center of the abscess to be coughed up and replaced
by air . this air is then seen a transradiancy within the consolidation and an air-fluid level may
be present . cavitation occasionally seen as a pulmonary consultations e.g. infarction , Wegener
granulmatosis . CT is more sensitive
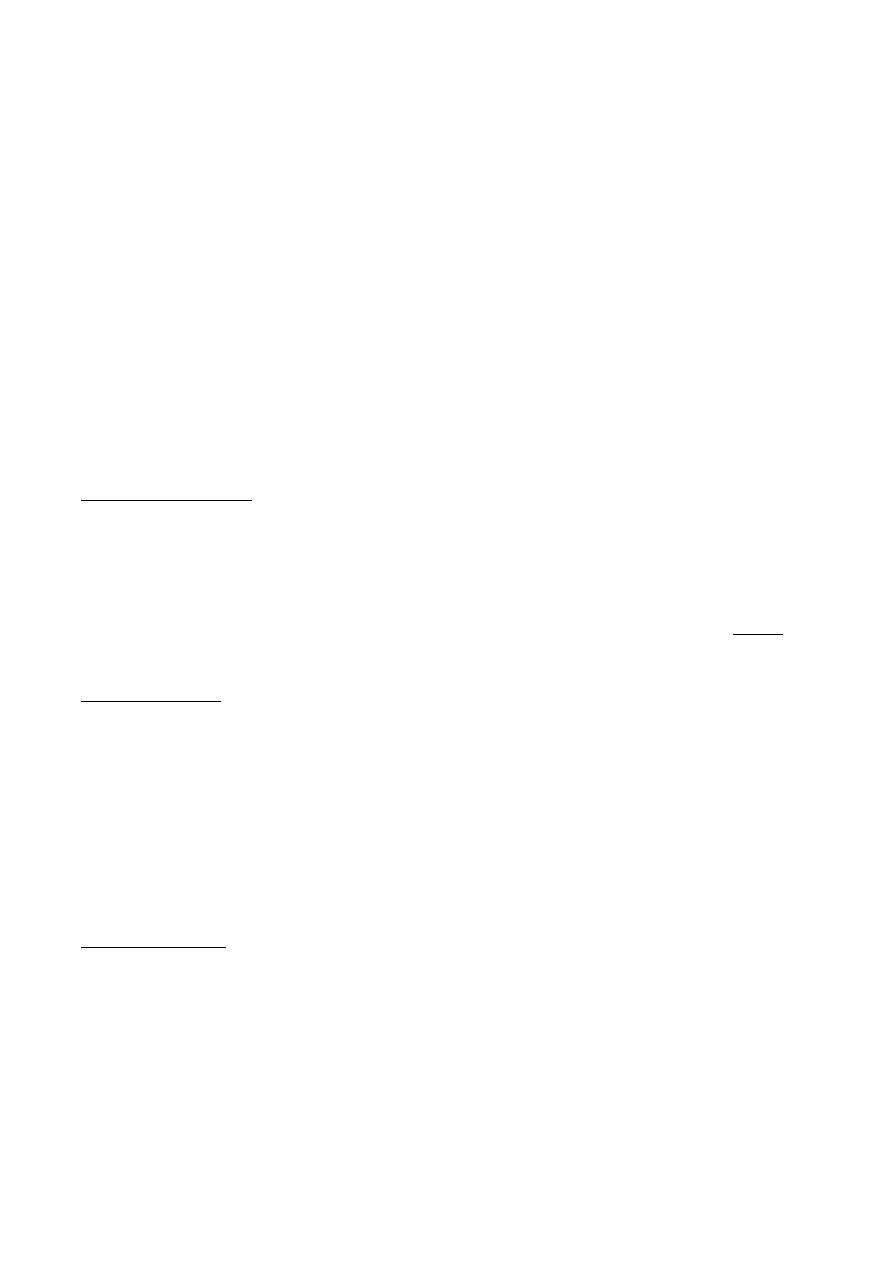
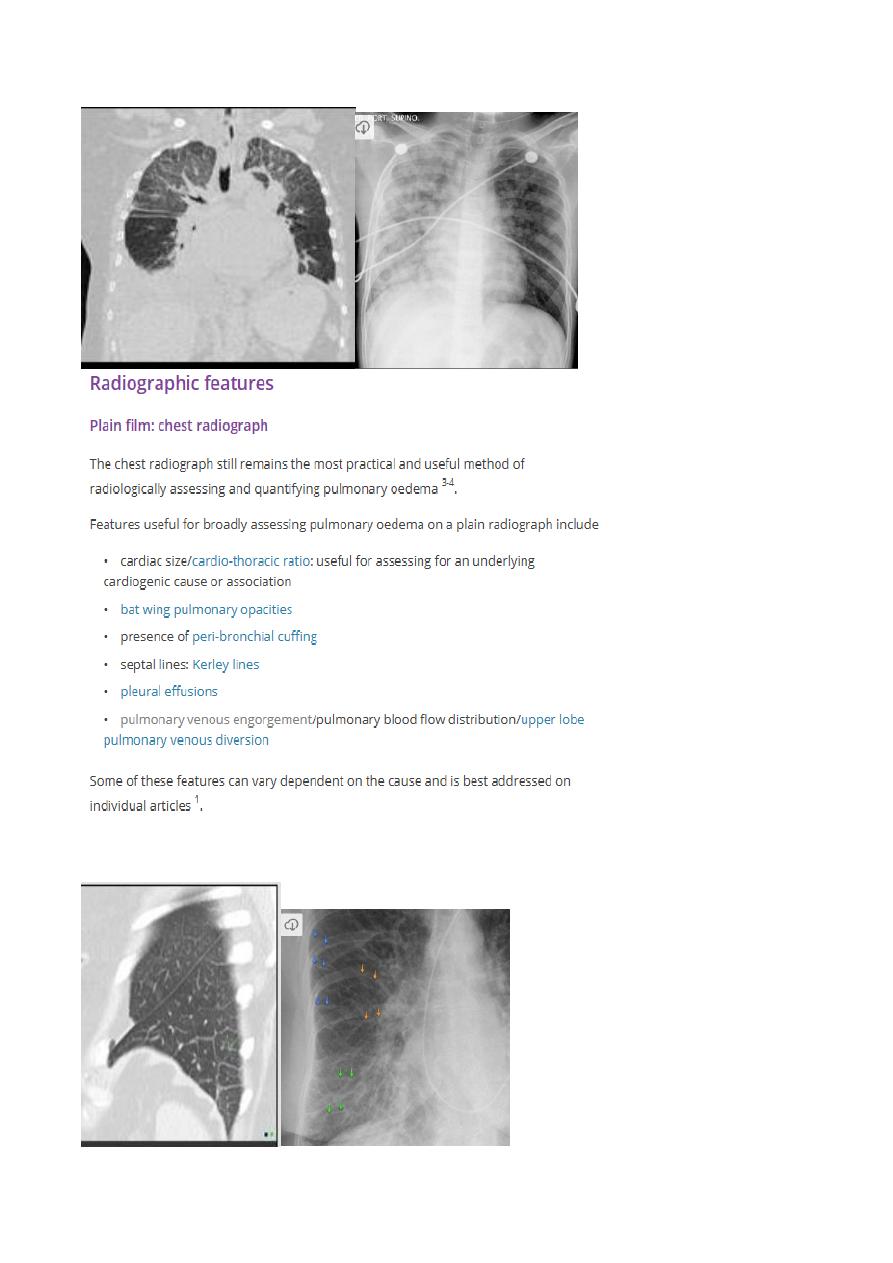
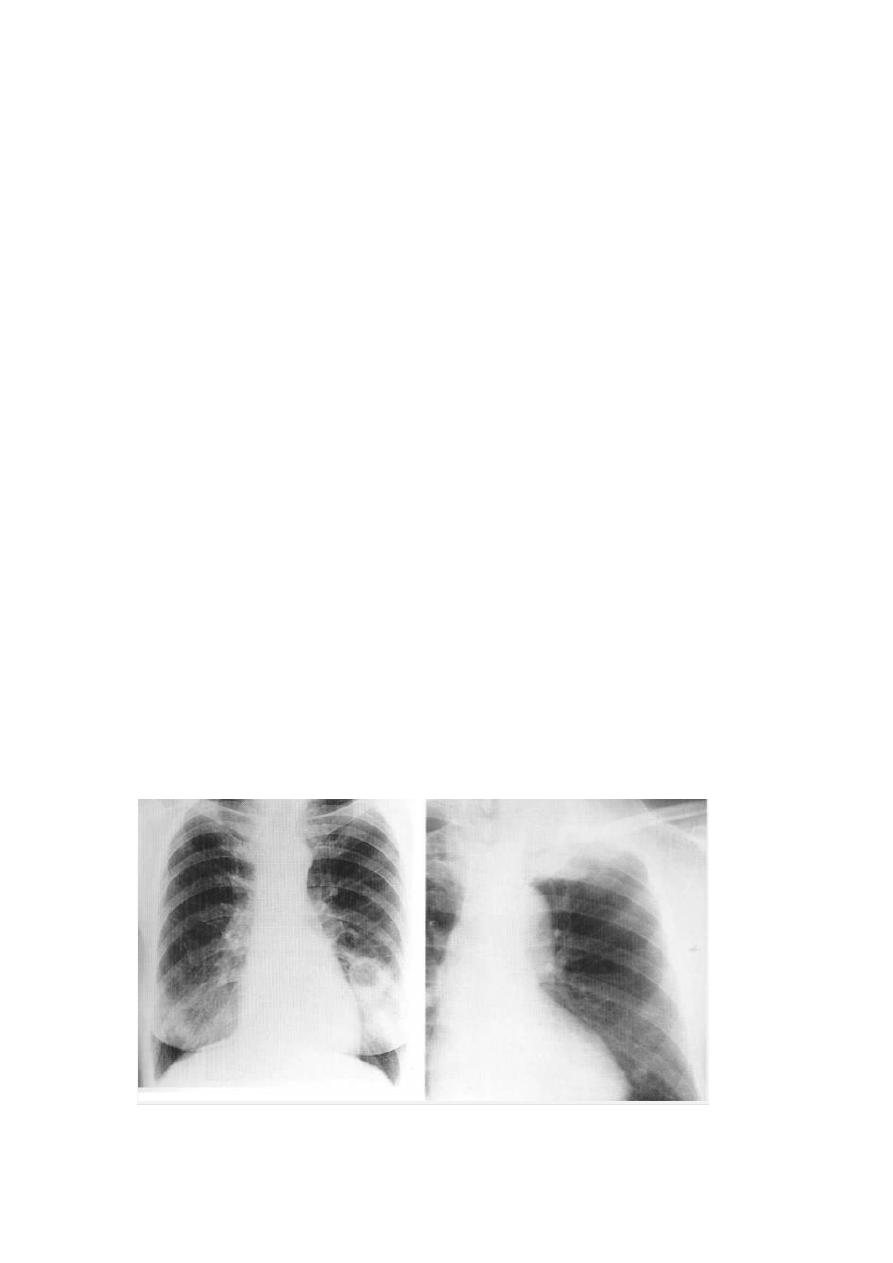
2. pulmonary odema
Any accumulation of fluid in the extra-vascular compartment .
Causes of edema : cardiac and non-cardiac causes
The features :
1. Unilateral or bilateral
2. Symmetrical or not
3. Staging : in the beginning of accumulation at the interlobular septa and for kerley
lines …. But when the fluid not drained it accumulate in the alveoli .. if the alveoli
filled with fluid it will escape to pleural space
Interstitial edema : there are many septa in the ling which are invisible on normal chest
film because they consist of little more than a sheet of connective tissue containing very
small blood and lymph vessels. When these septa thickened by edema , the peripherally
located septa may seen as a line shadow . the lines known as Kerely B lines usually found
in the distal third of lung whatever it apex or base or periphery which refer to early stage of
disease .
Another sign of interstitial edema is that the outline of the blood vessels may become
indistinct owing to edema collecting around them, this sign is difficult to recognize.
Fissure may be thickened because the edema may collect against them '
Alveolar edema : it more severe edema , the fluid collect into alveoli . it always acute and
almost always bilateral , involving all lobed bilaterally . the shadowing is maximal close to
hila and fades out peripherally, leaving a relative clear zone that may contain septal lines
around the edge of lobe . pattern of edema ( butterfly or bat wing ) . later on the shadowing
more widespread bur obvious in the lower zones .
***** long standing edema will caused apical calcification due to end stage hilar or small
vessels atherosclerosis or can see cavitation in lung apex
Radiology L1 : د.منى عبالغني
For the above pic : Rt. Lung edema , loss of definitive Rt. Heart border , costophernic angle
is preserved
this are Kerley lines
Radiology L1 : د.منى عبالغني
Air Broncho gram : are filling bronchi which is made visible by the
opacification of the surrounding alveoli
It feature of local infection or local disease , its not promenant for tumors unless it’s a
pneumonia which is due to small endo bronchial obstruction which result in distal
obstruction , one of presentation of non-resolving pneumonia
MULTIPLE PULMONARY NODULES :
1. Metastasis.
2. Military TB ( infection at all but TB is most prominent )
3. Chicken pox
4. Infectious granuloma ( teberculous )
5. Fungal infection
6. Pulmonary edema
First impression about multiple nodule , its bilateral , not symmetrical involving all lung
field with variable severity
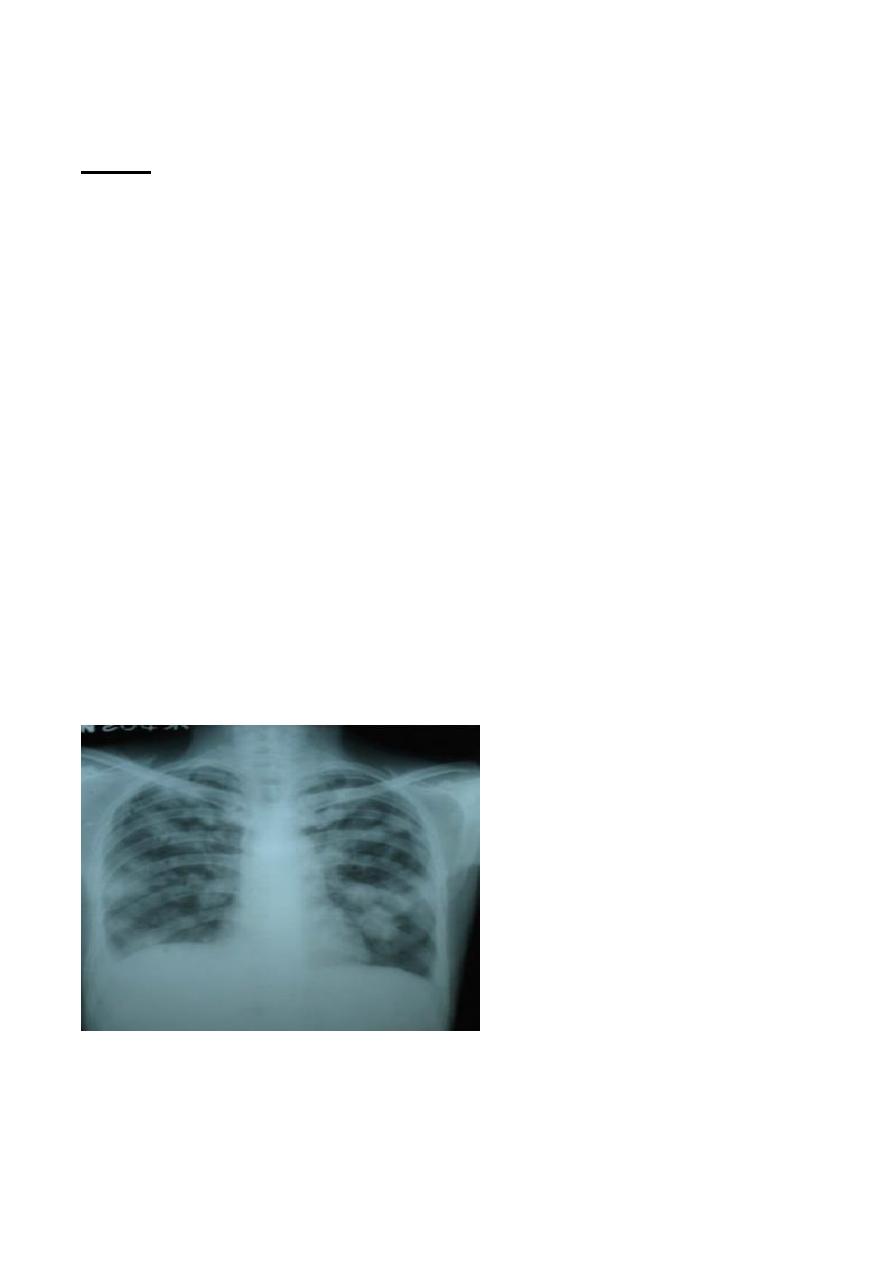
Diffuse military calcification :
Causes :
1. T.B.
2. Viral infection
3. Military metastasis ( breast cancer )
4. Calcified metastasis : thyroid ca. , mucinous adenocarcinoma of colon , osteogenic
sarcoma
Radiology L1 : د.منى عبالغني
T.B.
Infection acquired by droplet inhalation From other individuals.
Predisposing factors;
1. Inner city poverty .
2. Immunodeficiency conditions.
3.
Homeless with immigration from areas with high rate of infection .
4.
Diabetes.
5.
Alcoholism
6.
Silicosis & malignancy.
Primary TB: Radiological features ,
1. Lobar pneumonia, any lobe may be involved .
2. Ipsilateral nodal hailer or mediastinal enlargement which is the most common
manifestation in children with or with out pneumonia
3. Segmental or lobar collapse due to extrinsic nodal compression by enlarged
LN commonly in the anterior segment of the Rt. Upper and middle lobe.
4. Bronchopneumonia, with multifocal involvement.
5. pleural effusion ,unilateral more common in children .
6. Military TB (1-2 ) mm nodules scattered evenly through both lungs due to
hematogenous spread
7. Tuberculoma which result from repeated episodes of disease arrest and
Progression
8. cavitation : less common which suggest progressive primary TB ( primary
TB which progress to the post primary form without a break).
Radiology L1 : د.منى عبالغني
Post primary TB : Radiological features ,
1. Bronchopneumonia : poor marginated nodular opacities arising in the epico-
posterior segment of an upper lobe and \or a superior segment of a lower
lobe.
2. Cavitation.
3. Healing and scar formation .calcifications.
4. Fibrosis and linear opacities
5. Pleural thickening
6. bronchiactasis and bullae due to permanent destruction of the lung tissue and
major bronchi coupled by secondary bacterial infection
7. Military TB
8. Empyema ( infected pleural effusion ).
9. Tuberculoma
Bronchogenic Carcinoma :
one of the most common Ca, that associated with smoking ,
Presenting feature :
1. Pain in shoulder and limitation of movement because of local invasion
2. If affected phrenic nerve will elevate the diaphragm
3. If involve the parasympathetic trunk in either sides of neck will cause Horner syndrome
4. Hilar and medistanial lymph nod enlargement
5. Pleural effusion
6. Invasion of mediastinum
7. Invasion of chest wall
8. Rib metastasis
9. Pulmonary metastasis
Signs of central Tu.:
1. May present as a hilar mass with or without narrowing of adjacent major bronchus
2. Collapse or consolidation of lung beyond the tumor . collapse because the air absorbed
beyond obstructed bronchus and cant replaced , while consolidation is a consequence of
retained secretion and secondary infection
Radiology L1 : د.منى عبالغني
Signs of peripheral Tu.
Usually presented as solitary mass or nodule in chest film or in CT
1. Rounded shadow with irregular border . lobulation , notching and infiltrating edge are the
common attrens
2. Cavitation within the mass , the wall of the cavity are classically thick and irregular , but
thin walled smooth cavities due to ca.
loss of definitive hilar sf Lt. side which is central tu. Also there is a lytic bony lesion in ribs
In Late presentation :
1. Hemoptysis
2. Dyspnea
3. Weight loss
4. Decrease appetite
5. Very high ESR
Radiology L1 : د.منى عبالغني
Pneumonia:
Bacterial pneumonia
The major purpose of chest radiographs in patients with suspected chest
infection is to establish whether or not pneumonia is present. Diagnosing the
responsible infectious agent is rarely possible on radiological grounds as there is
considerable overlap in the appearance of various bacterial pneumonias, and
there is even overlap in the appearance of bacterial or fungal and viral
pneumonias,
The radiological feature
1. One or more areas of consolidation varying from a small ill- defined
shadow to a large shadow involving the whole of one or more lobes
2. Consolidation may be accompanied by loss of volume of the affected lobe,
a feature that particularly common in children.
3. Cavitation is particular feature of infection with staph. & Gram-negative &
anaerobic & T.B. the cavitation may occur in consolidated area
4. The commonest organism in community acquired pneumonia is
streptococcus pneumonia ( pneumococcal pneumonia ) and there is usually
dense consolidation of a considerable portion of one lobe usually without
loss of volume and may be an associated pleural effusion
5. When the consolidation is patchy, involving one or more lobes, it is
commonly referred to as bronchopneumonia. The most frequent causes of
community-acquired bronchopneumonia are Staphylococcus aureus,
various Gram-negative and anaerobic bacteria, and Mycoplasma
pneumoniae.
6. Pneumonia may be secondary to obstruction of a major bronchus,
carcinoma being a common cause of obstruction ,considered in patient
presenting with consolidation of one lobe, or of tm lobes supplied by a
common bronchus (e.g. the right middle and lower lobes), particularly If
there la associated Ion volume.
7. Lobar pneumonia : infection primary involves alveolus , spread through
pores of Kohn and canal of Lambert through out a segment and ultimately
an entire lobe .Bronchi are not primarily affected and remain air filled ;
therefore : Air broncho gram seen and there is no volume loss because
airways are open .Ex S. pneumonia
Viral and mycoplasma pneumonia
Viral pneumonia and pneumonia due to Mycoplasma pneumoniae may
produce widespread ill-defined consolidation and loss of clarity of the
vascular markings, which on occasion may resemble pulmonary oedema.
Alternatively, only a localized area of consolidation may be seen. Pleural
effusions are rare. The radiological abnormality may persist for many
weeks after clinical recovery.
Radiology L1 : د.منى عبالغني
Pulmonary collapse (atelectasis)
The common causes of pulmonary collapse (loss of a lobe or lung) are:
1. bronchial obstruction
2. pneumothorax or pleural effusion
3. linear (discoid) atelectasis.
Collapse caused by bronchial obstruction
Collapse caused by bronchial obstruction occurs because air cannot get into
the lung in sufficient quantities to replace the air absorbed from the alveoli.
The signs of lobar collapse are:
a. Displacement of structures.
b. The shadow of the collapsed lobe - consolidation almost invariably
accompanies lobar collapse, so the resulting shadow is usually obvious.
c. The silhouette sign. The silhouette sign not only helps diagnose lobar
collapse when the resulting shadow is difficult to appreciate, but also
helps to decide which lobe is collapsed. Collapse of the anteriorly
located lobes (upper and middle) obliterates portions of the mediastinal
and heart outlines, whereas collapse of the lower lobes obscures the
outline of the adjacent diaphragm and descending aorta.
The commoner causes of lobar collapse are:
1. Bronchial wall lesions, usually primary carcinoma, but occasionally
other bronchial tumours such as carcinoid tumours.
2. Intraluminal occlusion, usually foreign body or retained mucus plugs,
particularly in postoperative, asthmatic- or unconscious patients, or in
patients on artificial ventilation
3. Invasion or compression by adjacent malignant tumour or, rarely by
enlarged lymph node
When a lobe collapses, the unobstructed lobe(s) on the side of the collapse
undergoes compensatory expansion. The displaced fissure is seen as a well-
defined boundary to an airless lobe in one or other view. The mediastinum and
diaphragm may move towards the collapsed lobe.
As lobar collapse is such an important and often difficult diagnosis to make on
chest radiographs, it is worth devoting time to study the appearance of collapse
of each of the lobes . Computed tomography shows lobar collapse very well , but
is rarely necessary simply to diagnose a collapsed lobe.
With collapse of the whole of one lung, the entire hemi- thorax is opaque and
there is substantial mediastinal and tracheal shift

Radiology L1 : د.منى عبالغني
Collapse in association with pneumothorax or pleural effusion
The presence of air or fluid in the pleural cavity allows the lung to collapse.
In pneumothorax, the diagnosis is obvious but if there is a large pleural
effusion with underlying pulmonary collapse it may be difficult to
diagnose the presence of the collapse on a chest radiograph.
This problem does not arise with CT where it is usually easy to recognize
pulmonary collapse despite the presence of a pleural effusion.
If lobar collapse is identified, it can be difficult to tell whether the collapse
is due to pleural fluid or whether both the collapse and the effusion are due
to the same process, e.g. carcinoma of the bronchus.
Linear (discoid) atelectasis
Linear (discoid) atelectasis is not secondary to bronchial obstruction, it is due to
hypoventilation - the commonest cause of which is postoperative or post-
traumatic pain. The result is a horizontally orientated band or disc of collapse
Pleural effusion
P
leural effusions may lie free within the pleural cavity, in which case the
fluid falls to the most dependent portion of the pleura and assumes a shape
dependent on the thoracic cage and the shape of the underlying lung
or it may become loculated by pleural adhesions.
Although loculation occurs in all types of effusion, it is a particular feature of
empyema.
Such loculations may either be at the periphery of the lung or within the fissures
between the lobes.
A loculated effusion may simulate a lung tumour on chest radiographs.
causes of pleural effusion
1. Infection. Pleural effusions due to pneumonia are, on the whole small, and
the pneumonia is usually the dominant feature on the chest film.
Large loculated effusions in association with pneumonia often indicate
empyema formation .
In some cases of tuberculosis the effusion is the only visible abnormality
and the effusion may be large.
2. Subphrenic abscess, which is nearly always accompanied by a pleural
effusion.
3. Malignant neoplasm. Effusions occur with pleural metastases, but it is
unusual to see the pleural deposits themselves on plain chest radiographs.
Pleural metastases are occasionally seen on CT, MRI or ultrasound as
nodular or mass like pleural thickening. Malignant effusions are frequently

Radiology L1 : د.منى عبالغني
large. If the effusion is due to bronchogenic carcinoma or malignant
mesothelioma, other signs of the primary tumour are usually, but not
always, evident.
4. Cardiac failure. Small bilateral pleural effusions are seen frequently in
acute left ventricular failure. Larger pleural effusions may be present in
longstanding congestive cardiac failure. The effusions are usually bilateral,
often larger on the right than the left. Other signs of cardiac failure, such as
alteration in the size or shape of the heart, pulmonary oedema or the signs
of pulmonary venous hypertension, are usually visible.
5. Pulmonary infarction. Pulmonary emboli which result in pulmonary
infarction may cause pleural effusion. Such effusions are usually small and
accompanied by a lung shadow caused by the pulmonary infarct.
6. Collagen vascular diseases. Pleural effusions, either unilateral or bilateral,
are relatively common in various collagen vascular diseases. They may be
the only abnormal features on chest imaging.
7. Nephrotic syndrome, renal failure and ascites are all associated with
pleural effusion.
Plain Radiological findings
1. The radiographic appearances of fluid in the pleural cavity are the same
regardless of whether the fluid is a transudate, an exudate, pus or blood.
**Free fluid collects in the most dependent portion of the pleural cavity and
always fills in the costophrenic angles.
2. Usually the fluid surrounds the lung and is higher laterally than medially.
3. Very large effusions run over the top of the lung.
4. The smooth edge between the lung and the fluid can be recognized on an
adequately penetrated film, providing the underlying lung is aerated. It is
worth remembering that a large effusion may hide an abnormality in the
underlying lung.
5. Sometimes, even with a large effusion, little or no fluid is seen running up
the chest wall. The fluid is then known as a 'subpulmonary effusion'. The
upper border of the fluid is much the same shape as the normal
diaphragm, and as the true diaphragm shadow is obscured by the fluid it
may be very difficult, or even impossible, to tell from the standard erect
film if any fluid is present at all.
Ultrasound.
Ultrasound is a simple method of determining whether pleural fluid is
present.
Pleural fluid can be recognized as a transonic area between the lung and
diaphragm or between the chest wall and the lung .

Radiology L1 : د.منى عبالغني
It is only rarely possible to determine the nature of the fluid e.g. in
empyema, multiple echoes may be seen due to the pus in the fluid.
Ultrasound is particularly useful in defining the presence, size and shape of
any pleural collection loculated against the chest wall or diaphragm and is
a convenient method of imaging control for pleural fluid aspiration or
drainage.
Computed tomography.
Pleural effusions are usually seen as homogeneous fluid density between
the chest wall and lung
Computed tomography is particularly useful for showing loculated pleural
effusions
If the fluid is due to recent haemorrhage it will show the high density of
blood, otherwise it is not possible to determine the nature of the fluid.
Free pleural fluid moves to the dependent portion of the chest.
Surprisingly, it is sometimes difficult to determine from CT whether fluid
is pleural effusion or ascites.
The distinction is made by noting the relationship of the fluid to the
diaphragm. Pleural fluid collects outside the diaphragmatic dome and can
be seen posterior to the portion of diaphragm that covers the bare area of
the liver.
Computed tomography can be used to distinguish between lung abscess
and empyema ,Like ultrasound, CT can be used to direct the placement of
drainage tubes.
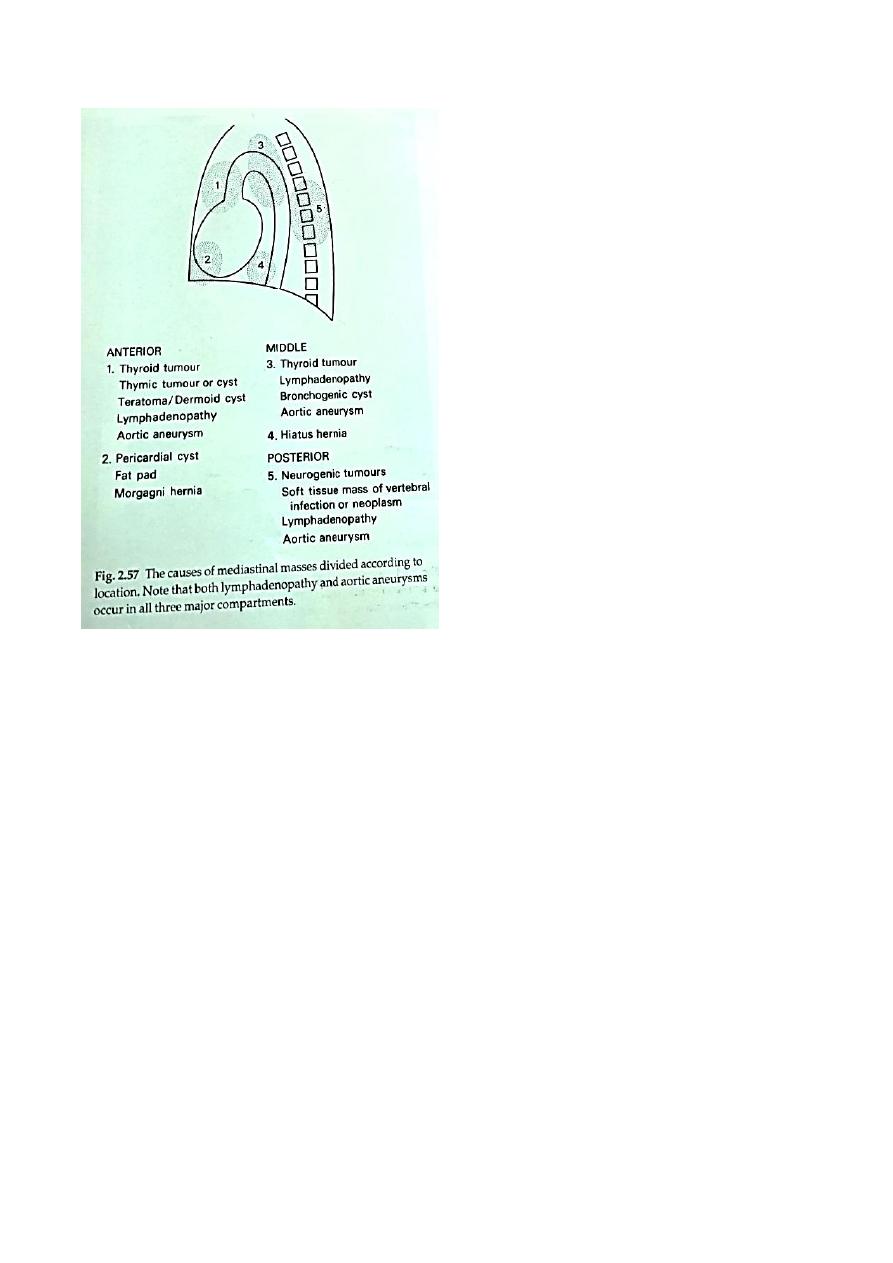
The mediastinum
The mediastinum is divided into anterior, middle and posterior divisions
However, masses often cross from one compartment to the other. Mediastinal
widening can be due to many different pathological processes. These are usually
classified according to their position in the mediastinum; so if a mediastinal mass
is identified on the frontal chest radiograph, the next step should be to attempt to
localize it in the lateral view or on CT
Radiology L1 : د.منى عبالغني
CT and MRI of the normal mediastinum
Computed tomography is the standard method for imaging the mediastinum.
Magnetic resonance imaging is used only occasionally.
The cross-sectional display and the ability to distinguish between fat, various
soft tissues and blood vessels are major advantages of both techniques.
1. The bulk of the mediastinum is due to blood vessels. For CT they are often
enhanced using intravenous contrast medium. At MRI, the larger vessels
are readily seen without contrast agent.
2. The only other normal structures of appreciable size are the thymus,
oesophagus, trachea and bronchi.
3. Normal lymph nodes are small, usually less than 6 mm in diameter
(maximum 10 mm), and many are not visible.
4. The mediastinal structures are surrounded by fat. The sites listed below
normally contain nothing but fat or small lymph nodes. They are, therefore,
areas in which small masses, particularly enlarged lymph nodes, can be
readily recognized:
Between the right tracheal wall and the adjacent lung (the one exception
being the azygos vein which lies in the right tracheobronchial angle).
Radiology L1 : د.منى عبالغني
Between the right wall of the oesophagus and the adjacent lung all the way
down the chest, an anatomical region known as the azygo-oesophageal
recess.
Anterior and to the left of the aorta and main pulmonary artery (other than
the thymus and the left brachiocephalic vein).
Mediastinal masses
Plain chest films in mediastinal masses
1. Intrathoracic thyroid masses (goitres) are the most frequent cause of a
superior mediastinal mass The characteristic feature is that the mass
extends from the superior mediastinum into the neck and almost
invariably compresses or displaces the trachea.
2. Lymphadenopathy is the next most frequent cause of a mediastinal
swelling. Lymphadenopathy may occur in any of the three compartments
and it is often possible to diagnose enlarged lymph nodes from their
tabulated outlines and the multiple locations involved
3. Neurogenic tumours are by far the commonest cause of posterior
mediastinal masses. Pressure deformity of the adjacent ribs and thoracic
spine is often visible.
4. Certain tumours, such as dermoid cysts and thymomas, are, for practical
purposes, confined to the anterior mediastinum.
5. Calcification occurs in many conditions, but almost never in malignant
lymphadenopathy. Occasionally, the calcification is characteristic in
appearance, e.g. in aneurysms of the aorta.
6. A mediastinal mass due to a hiatus hernia is usually easy to diagnose on
plain films because it often contains air and may have a fluid level, best
seen on the lateral view
7. Masses in the right cardiophrenic angle anteriorly are virtually never of
clinical significance. They are nearly all either large fat pads, benign
pericardial cysts or hernias through the foramen of Morgagni
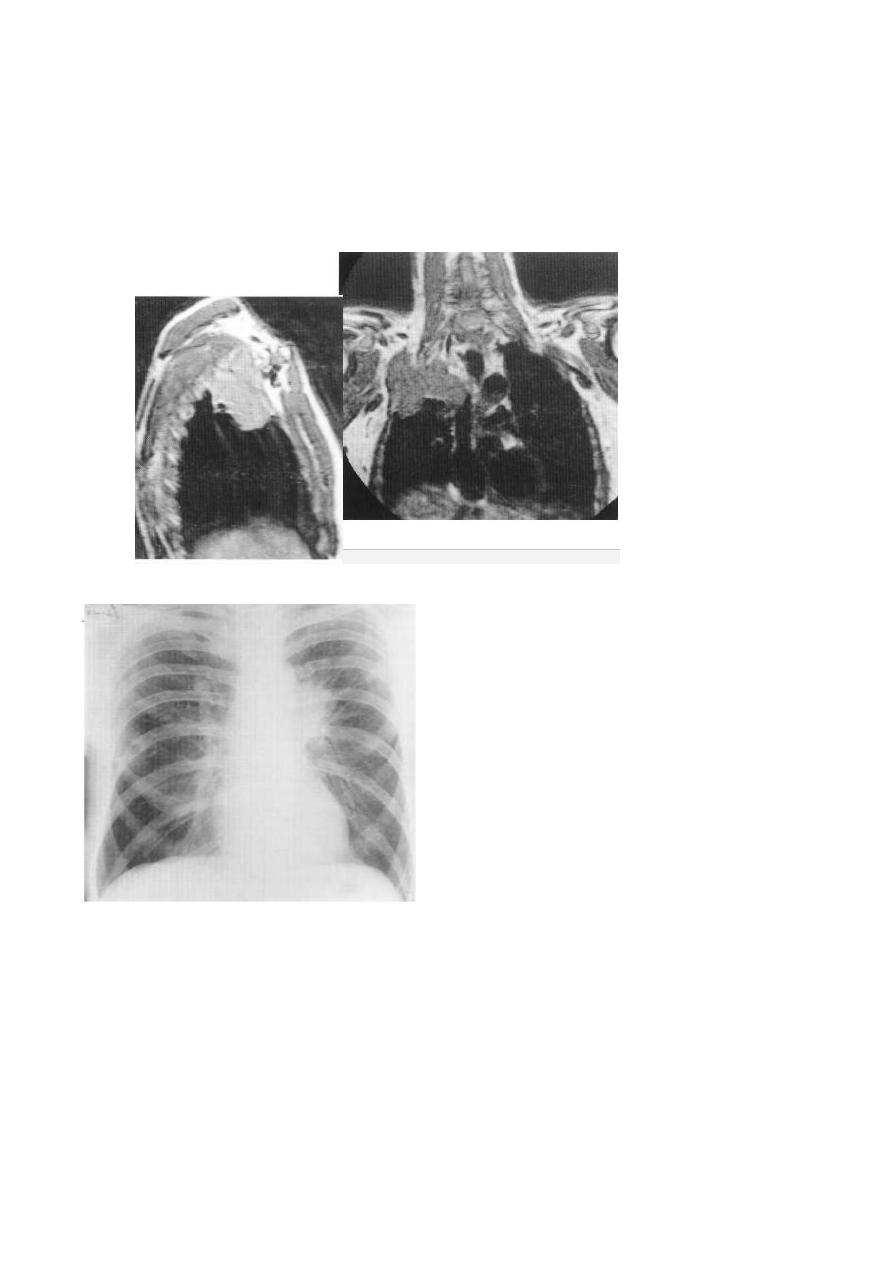
Computed tomography of mediastinal masses
Computed tomography provides much more information than plain chest
radiographs; occasionally, a specific diagnosis can be made. Magnetic resonance
imaging is used only in highly selected cases, e.g. where CT contrast agents are
contraindicated or in demonstrating the relationship of a posterior mass to the
spinal canal .

Radiology L1 : د.منى عبالغني
The advantages of CT are:
1. Abnormalities can be accurately localized. Knowledge of the precise shape,
position and size of a mediastinal mass frequently narrows the differential
diagnosis. For instance, contiguity of the mass with the thyroid in the neck
suggests a goitre and multiple oval-shaped masses suggest
Lymphadenopathy Solid mass anterior mediastinum have a limited
number of possibilities,
2. Occasionally, the density of the abnormality reveals its nature
Fat can be recognized as such, which is useful in distinguishing large
cardiophrenic angle fat pads or unusual mediastinal fat collections from
tumours, e.g, in Cushing’s disease. Cystic teratomas (dermoid cysts) may
contain recognizable fat.
Because of its high iodine content, thyroid tissue is of higher attenuation
than muscle prior to contrast medium administration. After contrast, it
enhances brightly , (A radio-iodlne scan is a highly specific alternative to
CT for confirming that an intrathoracic mass is a goiter
Intravenous contrast enhancement permits ready differentiation of
aneurysms (see below) and anomalous blood vessels from other masses.
Calcification is readily seen, the presence of calcification in a mass
effectively excludes untreated malignant neoplastic adenopathy.
APICAL SHADOWING
The lung apex is a common site for; Apical caps ,TB ,fungal infection ,bullae
,pneumothorax ,tumor of the lung apex (pan coast tumor )
Cavitary lesions
:
A cavity is a gas filled space surrounded by complete wall which is greater than
3mm in thickness, thinner wall cavities are called cysts pneumatoceles ,bulla and
ring shadows . Types :
1. abscesses :necrosis of lung parenchyma with or without bronchial
communication.
2. Fungal ball (air crescent sign ).ex Aspergillus infection with complicated TB
especially in the elderly .
3. Pneumatoceles ; thin wall air filling spaces due to air leak in the pulmonary
interstitium seen with Staph. Aureus infection especially in children
4. cysts: ex hydatid.

Radiology L1 : د.منى عبالغني
Emphysema
is defined pathologically as an increase beyond normal size of air spaces distal to
the terminal bronchiole with destructive changes in their walls.
The radiological signs of emphysema are
1. Increased lung volume. The lungs increase in volume because of the
combined effect of airways obstruction on abnormally compliant lungs.
The diaphragm is pushed down and becomes low and flat The heart is
elongated and narrowed. The ribs are widely spaced and more lung lies in
front of the heart and mediastinum, (Overinflation of the lungs can be said
to be present if the hemidiaphragms at their midpoint are below the
seventh rib anteriorly or the twelfth rib posteriorly)
2. Attenuation of the vessels. The reduction in size and number of the
pulmonary blood vessels can be generalized or localized. If severe, the
involved area is called a bulla. The edge of a bulla is usually sharply
demarcated. In some cases, the normal lung adjacent to the bulla is
compressed and appears opaque.
Bronchiectasis is defined as irreversible dilatation of the bronchi often
accompanied by impairment of drainage of bronchial secretions leading to
persistent infection.
Conditions which cause bronchiectasis include pulmonary Infection in
childhood, cystic fibrosis and longstanding bronchial obstruction.
The radiological features are
1. Visibly dilated bronchi. If they contain air, the thickened walls of the
dilated bronchi may be seen as tubular or ring shadows. If filled with fluid,
the dilated bronchi are either opaque or contain air-fluid levels. As these
fluid levels are very short, they have to be looked for very carefully.
2. Loss of volume of the affected lobe or lobes is almost invariable.
3. A proportion of patients with symptomatic bronchiectasis have normal
plain chest films.
HRCT is very useful both to diagnose bronchiedB to assess its extent
Noor Rahman
