ENDOCRINE DISORDERS
Diabetes MellitusPatient AT your clinic
Healthy personUnderlying systemic problem- undiagnosed
Diagnosed-poorly controlled
Diagnosed- adequately controlled
Of all the endocrine diseases, Diabetes Mellitus is most the commonly encountered for the Oral and Maxillofacial surgeon. Not only can diabetes affect the outcome of surgery (e.g. increased risk of infection), the stress of surgery can affect the control of the disease, especially in the brittle diabetic patient.
Diabetes Mellitus
Diabetes Mellitus
Diabetes mellitus (DM), commonly referred to as diabetes, is a group of chronic metabolic diseases in which there are high blood sugar levels (hyperglycemia) over a prolonged period.Diabetes is due to either:
1. Pancreas not producing enough insulin.2. Cells of the body not responding properly to the insulin produced (resistance).
3. Combination of both
Normal levels
Fasting plasma glucose ( >8hrs)- FPG:
< 100mg / dl (5.6mmol/ l)
Normal
100-125 mg / dl (5.6 – 6.9mmol/ l)
Impaired (risk)• 126 mg / dl ( 7.0 mmol / l )
Provisional diagnosis of DiabetesNormal levels
Oral glucose tolerance test – OGTT(WHO- 75gm anhydrous glucose dissolved in water)
2- hour postload glucose < 140mg/ dl (7.8mmol/l)
Normal glucose tolerance2- hour postload glucose 140- 199 mg/ dl (7.8- 11.1 mmol/l)
Impaired glucose tolerance (risk)
2- hour postload glucose > 200 mg/ dl ( 11.1mmol/ l)
Provisional diagnosis of DiabetesCardinal features of Diabetes:
Frequent urination (Polyuria)Increased thirst ( Polydipsia)
Increased hunger ( Polyphagia)
Weight loss
Fatigue
Frequent and severe infections
Poor wound healing
Family history
Oral Complications
Xerostomia (dry mouth)Burning sensation
Ketone breath (fruity)
Increase gingival inflammatory reaction to plaque
Increased incidence of periodontal abscesses
Increase risk of periodontal disease 2.8 to 3.4 increase
Increase severity and rate of destruction.
Fungal infections
Delayed healing
Thickness of saliva
Vascular, cellular and molecular
REFER TO PHYSCIAN
Occasional
OvereatingLack of exercise
Criteria FOR DIAGNOSIS
Symptoms of diabetes+
Casual PGC > 200mg /dl (11.1 mmol / l)
Criteria FOR DIAGNOSIS
ORFPG > 126mg/dl (7.0mmol/l)
Criteria FOR DIAGNOSIS
OR2-hour postload glucose > 200mg/dl (11.1mmol/l) during an OGTT
High Blood Glucose (Hyperglycemia)
Damage small blood vessels:• Kidney…………… Diabetic Nephropathy
• Heart……………..Heart disease, Stroke
• Eyes………….. Diabetic Retinopathy
• Nervous system:
A. Peripheral Neuropathy (tingling, numbness, foot ulcers, amputations)
B. Autonomous Neuropathy ( GIT,GU,CV)
5. Susceptibility to infection
If left untreated, diabetes can cause many complications:
• Acute complications include diabetic ketoacidosis and nonketotic hyperosmolar coma.
• Serious long-term complications include cardiovascular disease, cerebrovascular (stroke), hypertension, chronic kidney failure, foot ulcers and damage to the eyes.
There are three main types of diabetes mellitus:
Type 1 DM results from the pancreas' failure to produce enough insulin. This form was previously referred to as "insulin-dependent diabetes mellitus" (IDDM) or "juvenile diabetes". It typically occurs in younger patients as a result of genetic predisposition, faulty β cells , autoimmune destruction of the β cells of the pancreas. There is little or absolute deficiency of insulin.TREATMENT
Insulin Injection:Syringe
Pen
Jet Injectors
Insulin Pumps
Exogenous insulins are classified primarily based on their time to onset and length of action:
• Rapid acting (e.g. regular insulin, peak effect 2–4 hours)
• Intermediate acting (e.g. NPH or lente, peak effect 6–12 hours)
• Long acting (e.g. ultralente, peak effect 10–16 hours) and are frequently used in combination.
• Nasally inhaled insulin is also available, but has only about 10% of the activity of subcutaneous insulin, is affected by smoking, and may cause pulmonary changes.
Monitoring
Daily - Continuous glucose monitoring (CGM) systems consist of small sensors inserted subcutaneously, usually on the abdominal wall, that measure glucose in the interstitial fluid and display the value along with trend information, and various alarms on the pump or a monitor.
Periodic : Glycosylated hemoglobin ( Hg A1C ): This test measures the average percentage of glucose levels in the blood over the previous two to three months. Best is 6-8%.
Type 2 DM Is the most commonest (95% of cases).This form was previously referred to as "non insulin-dependent diabetes mellitus" (NIDDM) or "adult-onset diabetes". The primary cause is overweight. It is a milder form than Type 1.
The pancreas produces insulin but:
• Not enough.• Body cells are resistant to it. Insulin resistance happens basically in fat, liver and muscle cells.
Obese or overweight
• More than 20% over their ideal body weight for their height.• Are at risk for Type 2 Diabetes
• Obesity is associated with tissue and muscle resistance to insulin. Pancreas starts to produce large amount of insulin to overcome the resistance and hyperglycaemia. After a few years, the pancreas becomes very exhausted and unable to cope so insulin levels go down and Diabetes happensTreatment
No cureMedications
Insulin (exogenous)
Weight management
Nutrition
Exercise: It increases muscle sensitivity to insulin
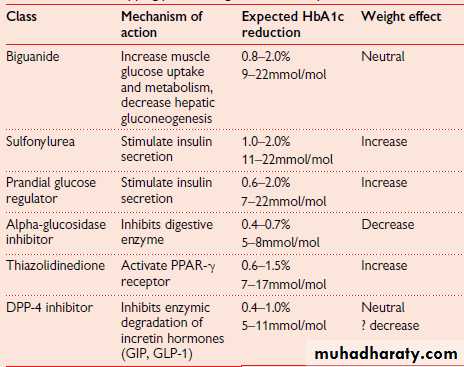
Oral hypoglycaemic agents: summary
Gestational diabetes, is the third main form and occurs when pregnant women without a previous history of diabetes develop a high blood-sugar level (2-10% of pregnancies).Other forms of Diabetes:
• Genetic• Pancreatitis
• Trauma
• Endocrinopathies (Cushing syndrome, Hyperthyroidism)
• Surgery
• Medications (steroids, thiazides)
• Infections (pancreatitis)
• Account for 1-5% of all cases of Diabetes
Dental Management of Diabetic Patient
In the perioperative period, serum glucose levels must be frequently monitored and controlled. This may be difficult in the brittle diabetic patient due to various surgical factors (surgical stress) and so no standard regimen can be used by the Oral and Maxillofacial surgeon that will fit every diabetic patient.Known diabetic patient
Ask about:Medication
Type of Diabetes and severity
Physician
Last visit
Dentist aware of HbA1C (6-8%)
Known diabetic patient
If patient is under adequate medical management without serious complications as coronary atherosclerotic heart disease, hypertension , renal disease. In addition, the blood glucose level is within normal ranges.
Patient can receive any indicated dental T.T.T (After consultation)
Local and general anesthesia is safeKnown diabetic patient
If patient needs urgent dental T.T.T. but glucose levels are high or poorly controlled-Hospital-
Known diabetic patient
Patients with complications need a different T.T.T planMorning appointment (high glucose + low insulin) + short .This reduces hypoglycemia episodes during treatment
Stress free environment to avoid hyperglycemia (sedation + potent anesthesia)
Always follow the sick day rule
Known diabetic patient
• Emotional stresses and painful conditions increase cortisol and epinephrine secretion which induce hyperglycemia• Source of glucose available (e.g. orange juice )
• Prophylactic antibiotic in those on high insulin intake
• Dietary caloric control, while maintaining adequate nutrition for healing (soft or blended food)
• Consult physician for dietary plan
Known diabetic patient
• POST-OPERATIVE INSTRUCTIONS
• Good oral hygiene control
• Tooth brushing
• Dental Floss
• Clean dentures
• Regular visits to the dentist
• Topical fluorides
EMERGENCYHypoglycemia (low blood glucose)
Defined as blood glucose below 3.9 mmol/l, (60mg/dl) resulting from an imbalance between glucose supply, glucose utilization and current insulin levels. This is characterized by typical symptoms.Risk factors
• Impaired awareness of hypoglycemia• Previous exposure to severe hypoglycemia
• Increasing age
• Increasing duration of diabetes
• Strict glycaemic control
• Sleep
• C-peptide negativity
Causes
Insulin doses are excessive, ill timed, or of the wrong type of insulin.
• Inadequate exogenous carbohydrate.
• Endogenous glucose production is decreased (e.g. alcohol ingestion).
• Glucose utilization is increased.
• Insulin clearance is decreased (e.g. renal failure).
• Typical symptoms of hypoglycemia
AutonomicNeuroglycopenic
General
Sweating
Palpitations
Tachycardia (˃110 per min)
Shaking
Hunger
Agitation
Confusion
Drowsiness
• Odd behavior
Speech difficulty
• Incoordination
• Seizures
• Unconsciousness
Headache
Nausea
• Autonomic symptoms are associated with a release of catecholamines, cortisol, glucagon, and growth hormone. They typically occur at a blood glucose level of around 3.8mmol/L.
2. Neuroglycopenic symptoms occur when glucose levels drop below 3mmol/L.
Severe hypoglycaemia• This is defined as an episode that requires assistance from another person, or that requires hospitalization or parenteral glucose administration or treatment with glucagon.
• This occurs when blood glucose drops to a level inadequate to support consciousness, usually below 1.5mmol/L.
• It is thought that, in some cases, this is associated with seizures or cardiac arrhythmias and can be associated with death.
Impaired awareness of hypoglycaemia
Recurrent hypoglycaemia can reduce the hormonal and symptomatic responses to subsequent hypoglycaemia, and, over time, after exposure to multiple episodes, patients can lose the ability to recognize hypoglycaemia.This is termed hypoglycaemia unawareness.
Those with impaired awareness of hypoglycaemia have a 3–5-fold greater risk of severe hypoglycaemia, compared to those with normal awareness.
Often, other people will recognize hypoglycaemia before the patient does.
Gold Score
Ask patient: “How often are you aware of episodes of hypoglycaemia (capillary blood glucose <3.5mmol/L)?”Always 1- 2- 3- 4- 5- 6- 7- Never
A score of 1 or 2 implies good awareness.
A score of 3 denotes borderline awareness,
A score of 4 or above denotes impaired awareness.
Management of Hypoglycemia
Assess the patient
Manage as hypoglycemic (Golden Rule)
Maintain adequate airway, ventilation
Switch on fan, air conditioner
Head-low-feet-up position
Administer 100% oxygen – flow rate 10L/min
• If patient conscious and cooperative:
Fruit juiceJellies
3-4 teaspoons of sugar
Candy
Syrup or honey in the buccal sulcus
Oral glucose (10-20gm); repeat if necessary after 10-15 minutes (children as adults)
• If patient is unconscious or uncooperative:
50 ml dextrose in 50% concentration• or
Glucagon , 1mg,i.m. injection.
For children:
Glucagon , i.m. injection
2-18 years 0.5mg if body weight ˂ 25kg
• 2-18 years 1 mg if body weight > 25kg
and
Oral glucose (10-20g) when regains consciousness ( children as adults)
Signs and symptoms should subside
within
10-15 minutes
Observe patient 30-60 minutes
Measure blood glucose (glucometer)If NO RESPONSE
Call for AmbulanceDiabetic Ketoacidosis (DKA)
Occurs most frequently in persons with type 1 diabetes.Physical signs and symptoms of DKA include:
Hyperglycemia (250 mg/dL or greater)
Dry, parched mouth
Extreme thirst
Frequent urination
General weakness
Fruity breath
Nausea and vomiting
Abdominal pain
Deep, rapid breathing
Hyperosmolar Hyperglycemic Non-ketotic Syndrome
Occurs most frequently in elderly persons with type 2 diabetes, especially residents of long-term care facilities.
Physical signs and symptoms of HHNS include:
Severe hyperglycemia (greater than 600 mg/dL)
Dry, parched mouth
Extreme thirst (which may gradually disappear)
Warm, dry skin that does not sweat
High fever (greater than 101 degrees F)
Sleepiness or confusion
Hallucinations
Weakness on one side of the body