Drugs used in Peptic ulcer
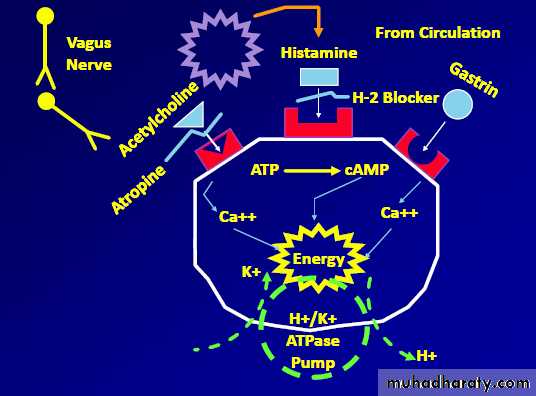
Regulation of gastric acid secretion Gastric acid secretion is under the control of 3 principal agonists: histamine, acetylcholine and gastrine.
The final common pathway is through the proton pump, H+ / K+ ATPase.
Inhibitiors of the activities of the first 2 secretagogues and of the proton pump have been developed
Effects of acetylcholine, histamine, prostaglandin E2, and gastrin on gastric acid secretion by the parietal cells of stomach.
Gs and Gi are membrane proteins that mediate the stimulatory or inhibitory effect of receptor coupling to adenylyl cyclase
Pathogenesis of peptic ulcer disease
Nonsteroidal anti-inflammatory drug (NSAID) use. Infection with gram-negative Helicobacter pylori
Increased hydrochloric acid secretion
Inadequate mucosal defense against gastric acid.
Treatment approaches
1. Eradicating the H. pylori infection
2. Reducing secretion of gastric acid with the use of H2-receptor antagonists or PPIs, and/or
3. protect the gastric mucosa from damage, such as misoprostol and sucralfate.
4. Neutralizing gastric acid with nonabsorbable antacids
5. Surgical treatment in( acute complications )
Antimicrobial agents
Combinations of antimicrobial drugs . Give 90 % or greater eradication rate. Triple therapy consisting of a PPI with either metronidazole or amoxicillin plus clarithromycin
Or
Quadruple therapy of bismuth subsalicylate and metronidazole plus tetracycline plus a PPI
Are administered for a 2-week course.
Note: Bismuth salts inhibit pepsin and increase the secretion of mucus& form a barrier against the diffusion of acid in the ulcer.
Important H2-Antagonists
Cimetidine
Ranitidine
Famotidine
Nizatidine
Roxitidine
H2 Antagonists bind to H2 receptor, preventing histamine from binding to these receptors.
Block the action of histamine on stomach cell thus reducing stomach acid
Indication of use of H2- Antagonists :
1. Peptic ulcer.
2. Gastro esophageal reflux disease (GERD)
3. Erosive esophagitis.
4. Zollinger - Ellison syndrome.
5. Before anesthesia.
Cimetidine: cause gynecomastia, galactorrhea, and reduced sperm count& inhibits metabolism of warfarin, phenytoin.
Ranitidine: Compared to cimetidine, ranitidine is longer acting, and is 5-10 fold more potent.
Famotidine is 3-20 times more potent than ranitidine.
Are metabolized by liver but nizatidine is eliminated principally by kidney.
Pharmacokinetic of H2-Antagonists :
Well absorbed from the gut. Undergo varying degrees of hepatic inactivation before being excreted in the urine.
Half-life is 2-3 hours.
Duration of action is longer.
Administered once or twice daily.
Adverse effects
1. Central nervous system.
2. Cardiovascular reaction.
3. Hepatic reaction.
4. Hematological reaction.
5. Endocrine.
6. Risk to the fetus
Cimetidine inhibits CYP450, slow metabolism &, potentiate the action of warfarin, diazepam, phenytoin
Drug interactions with cimetidine
Inhibitors of the H+/K+-ATPase proton pump (PPIs)
OmeprazoleLansoprazole
Rabeprazole
Pantoprazole
Esomeprazole
The proton pump inhibitors produce quicker healing and provide greater symptomatic relief than H2 - antagonists in patients with peptic ulcer disease and GERD
Omeprazole is the first drug of this class ,it bind to the H+/K+-ATPase enzyme system (proton pump) of the parietal cell, thereby suppressing secretion of hydrogen ions into the gastric lumen.
The proton pump is the final step in the secretion of gastric acid
Actions of PPIs
These agents are prodrugs with an acidresistant enteric coating to protect them from premature degradation by gastric acid.
The coating is removed in the alkaline duodenum, and the prodrug, a weak base, is absorbed and transported to the parietal cell canaliculus.
Omeprazole
Omeprazole in itself is not the active inhibitor of the H+ / K+ - ATPase.It needs transformation in acid media to an intermediate compound, a sulphenamide, that effectively inhibits the H+ / K+ - ATPase
The sulphenamide interacts covalently with the sulphydryl groups of cysteine residues in the extracellular domain of the H+ / K+ - ATPase, thereby inhibiting its activity
Indications of PPIs
1. Peptic ulcer (Duodenal and Gastric ulcers
2. Eradication of Helicobacter pylori in the gut that causes ulcers in combination with antibiotics
3. NSAID - induced gastric ulcers
4. Gastroesophageal reflux disease ulcers
5. Zollinger - Ellison syndrome: proton pump inhibitors are the treatment of choice for zollinger - Ellison syndrome
Pharmacokinetics of PPIs
All these agents are delayed-release formulations and are effective orally.
Some are also available for intravenous injection.
Metabolites of these agents are excreted in urine and feces.
Adverse effects of PPIs
1. GIT: flatulence, diarrhea (by Clostridium difficile colitis ) or constipation, nausea, vomiting or abdominal pain.
2. CNS: paraesthesia, dizziness, somnolence and headache.
3. Skin: rashes, itching
4. Muscle: pain (myalgia).
5. Kidney: Interstitial nephritis.
Prostaglandins
Misoprostol
Prostaglandin E2, produced by the gastric mucosa, inhibits secretion of HCl and stimulates secretion of mucus and bicarbonate (cytoprotective effect).
Misoprostol an analog of prostaglandin E1, as well as some PPIs, are used for prevention of gastric ulcers induced by NSAIDs (in the elderly) & also used in patients with ulcer complications
It is less effective than H2 antagonists and the PPIs
Side effects of Misoprostol
1. Produces uterine contractions
2. Diarrhea and nausea
Antimuscarinic agents (anticholinergic agents)
Muscarinic receptor stimulation increases gastrointestinal motility and secretory activity.
A cholinergic antagonist, such as dicyclomine can be used as an adjunct in the management of peptic ulcer disease and Zollinger-Ellison syndrome, particularly in patients who are refractory to standard therapies.
Its many side effects (for example, cardiac arrhythmias, dry mouth, constipation, and urinary retention) limit its use.
Antacids
Aluminum hydroxide
Magnesium hydroxide
Calcium carbonate
Sodium bicarbonate.
Are weak bases that react with gastric acid to form water and a salt, thereby diminishing gastric acidity.
Because pepsin is inactive at a pH greater than 4, antacids also reduce pepsin activity.
Used for symptomatic relief of peptic ulcer disease and GERD; they may promote healing of duodenal ulcers
Adverse effects
1. Constipating (aluminum hydroxide)
2. Diarrhea (magnesium hydroxide)
3. Preparations that combine these agents aid in normalizing bowel function.
4. Important consideration in patients with hypertension or congestive heart failure (sodium content of antacids)
Mucosal protective agents (cytoprotective compounds) sucralfate
It is complex of aluminum hydroxide and sulfated sucrose
It Binds to positively charged groups in proteins of both normal and necrotic mucosa
Forming complex gels with epithelial cells, &creates a physical barrier that impairs diffusion of HCl and prevents degradation of mucus by pepsin and acid.
It also stimulates prostaglandin release as well as mucus and bicarbonate output, and it inhibits peptic digestion
It is effectively heals duodenal ulcers
Bismuth subsalicylate
This compound effectively heal peptic ulcers. Have antimicrobial actions
Inhibit the activity of pepsin
Increase secretion of mucus, and interact with glycoproteins in necrotic mucosal tissue to coat and protect the ulcer crater.
END