ENTAMOEBA HISTOLYTICA
Morphology (Trophozoite):1- Its size (12-30 µm), Clear ectoplasm.
2- Large finger – like pseudopodia
3- The endoplasm is granular and may contain RBCs.
4- It has one nucleus, contain small central karyosome and fine chromatin granules arranged regularly beneath nuclear membrane.
Morphology (mature cyst):
1- Small (10 – 20 µm) , spherical in shape, smaller than that of E. coli, containing 1 - 4 nuclei is usually found in feces . Each nucleus contain similar nuclear morphology like the trophozoite.
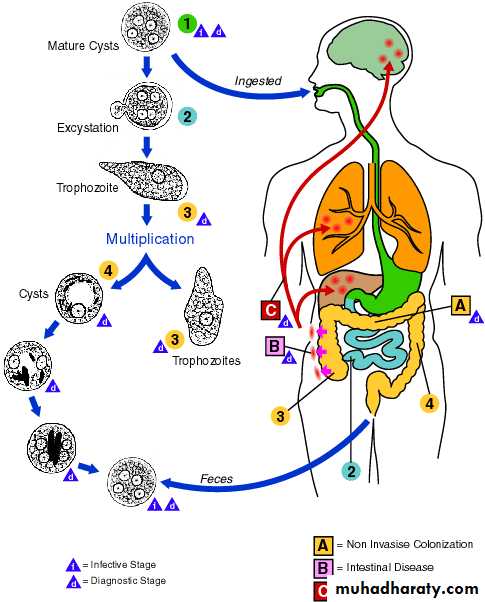
Life cycle of E. histolytica:
Infection by E. histolytica occurs by ingestion of mature cysts in fecally contaminated food, water, or hands. Excystation occurs in the small intestine and trophozoites are released which migrate to the large intestine. The trophozoites multiply by binary fission and produce cysts, which are passed in the feces.
Because of the protection conferred by their walls, the cysts can survive days to-weeks in the external environment and are responsible for transmission of infection. Trophozoites can also be passed in diarrheal stools, but are rapidly destroyed once outside the body, and if ingested rapidly destroyed by gastric juice. In many cases, the trophozoites remain in intestinal lumen as noninvasive infection of individuals who are asymptomatic carriers, passing cysts in their stool only.
In some patients the trophozoites invade the intestinal mucosa and cause intestinal disease or developed perforated ulcer and the trophozoites migrate through the blood stream to invade the extraintestinal organs such as the liver, brain, and lungs and it will cause amoebic infection in these organs.
Life cycle of E. histolytica:
Epidemiology:
* The incidence of Amebiasis is common & high in tropical & subtropical areas especially in areas of lower socioeconomic status due to:(1) Poor sanitation (2) overcrowding & (3) malnutrition
It is estimated that up to 10% of the world`s population may infected withE.histolytica
Transmision of amoebiasis occur through:
1. Mature cyst is the main source of the infection which passing with the feces of chronic patients or asymptomatic carrier .2. Human being acquire the infection via contamination of food, drinks, vegetables or hands with infective cysts especially in restaurant
3. Flies (House fly) play an important roles in transmission of these cysts to the food of human.
Pathogenesis of E.histolytica:
The Pathogenic activity of E. histolytica depend upon:
1- The resistant of the host.
2- The number of the amebas.
3- Presence of pathogenic bacteria.
4. Presence of physical & chemical injury of the mucosa
The lesions produced by E. histolytica are primarily in large intestine and
Secondarily extraintestinal especially the liver, brain or any organ of the body may be affected.
Pathogenesis of Intestinal lesion:
1. The lesion vary from small ulcer to a large typical flask shape ulcer.2. The ulcer has a wide base and narrow opening with irregular elevated edges.
3. The ulcer characterized with large area of tissue necrosis, cell infiltration & rapid lysis of inflammatory cells.
4. The amoebas usually found on the floor of the base of ulcer.
E. histolytica in the large intestine
(Flask shape ulcer)
Clinical features of intestinal lesion:
1- The incubation period range from 2 – 4 weeks.2- The majority of infections with E.histolytica show no symptoms or show symptoms which varies from mild to intense and long lasting.
The typical symptoms include:
1- Diarrhea, The diarrhea frequently alternates with constipation or soft stools may contain mucous but no visible blood.2-Abdominal cramps.
3-Nausia.
4-Anoroxia.
5- Dysentery:
Which is usually starts slowly with abdominal cramps and associated with loose stools and diarrhea with blood, mucus and necrotic tissues.
6- Few patients especially children may show fever, vomiting, abdominal tenderness.
The complications of intestinal amoebiasis:
1- Appendicitis.
2- Intestinal perforation.
3- Hemorrhage.
4- Liver abscess.
5- Ameboma (Granulomas):
a. Are a painful abdominal mass which occur most frequently in the caecum and ascending colon.
b. This lesion may be confused with carcinomas or tumor.
c. Obstructive symptoms or dysentery may also be associated with ameboma.
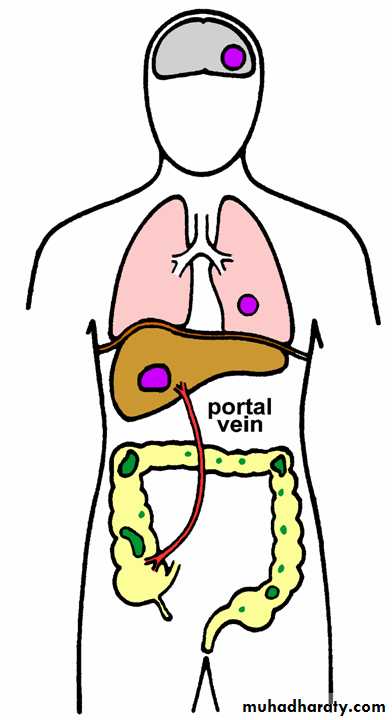
Extraintestinal Amoebiasis :
1. The metastasis of amoeba usually via blood stream or by direct extension after intestinal perforation to the peritoneum. The amoeba may cause local abscess or peritonitis or migrate to the liver which is the most commonly affected than other organs e.g., lungs, perianal skin or brain.
Extraintestinal Amebiasis
2. Amoebic liver abscesses: Are the most common extraintestinal amebiasis and characterized by:
a. Hepatomegaly, Liver tenderness, fever and anorexia.
b. Liver function tests are usually normal or slightly abnormal.
c. Liver abscesses will occasionally rupture into the peritoneum causing peritonitis
3. Pulmonary amoebiasis :
a. This infection due to the direct extension of the liver abscess through the diaphragm, or via blood.
b. The clinical symptoms are: cough, chest pain, dyspnea and fever.
c. The sputum may be purulent or contain blood and trophozoites of E. histolytica.
4. Cutaneous amoebiasis:
It is caused by contact of the skin with amoebic abscess which lead to fistula in the skin.
Diagnosis of Amoebiasis :
1- Stool of patient should be examined microscopically:a- The typical amoebic stool is contain blood, mucous, few WBC & Bacteria.
b- Direct method with saline for motile trophozoite .
C-Stool specimens should be stained usually with iodine and microscopically examined for cysts of E.histolytica .
2- Culture of stool.
3- Sigmoidoscopy may reveal the characteristic flask-shaped ulcers especially in severe cases.4- Biopsy & fluid from large intestine aspirates also be examined microscopically for trophozoites .
5- Serology, is very important for the diagnosis of extraintestinal amoebiasis e.g.: Indirect haemagglutination (IHA) & Polymerase Chain Reaction (PCR test).
6- Ultrasound, CT scan, MRI can be used to detect hepatic abscesses.
Treatment:
1. A symptomatic (source of infection) patients can be treated with Diiodohydroxyquine with tetracycline.Treatment Cont… :
2. Symptomatic patients with diarrhea or dysentery or extraintesinal amebiasis should be treated as follows:
a- Patients should remain in bed and receive a high protein and high vitamin with adequate fluids.
b. Chemotherapy for sever amoebiasis:
1. Metronidazol (Flagel) is the drug of choice:
750 mg three times a day, orally for 5 – 10 day.
2. Tetracycline & diiodohydroxyquine are recommended to be given to the patient since metronidazole may not always cure the intestinal infection.
Prevention & Control:
1- All human infections should be treated
2- A symptomatic carriers should be treated especially those working in restaurants.
3- Effective environmental sanitation is necessary to prevent water, food, and vegetable contamination, e.g. Sewage disposal should be treated with chemical before used as fertilizer in gardens.
4- Chlorination & filtered water supply are important to kill the cyst of E.histolytica.
5- Insects should be controlled by insecticides.
6- Uncooked vegetables should be washed with running water.