Treatment modalities of indirect hyperbilirubinemia
The treatment to decrease indirect bilirubin include different modalities:-Phototherapy
Exchange transfusionMetalloporphyrins
IV immunoglobuline ( IVIG )
1
Indirect bilirubin was reduced by use high intensity light in the visible spectrum
bilirubin absorb light maximally in the blue range from ( 420 – 470 nm ).phototherapy may decrease the need of exchange transfusion but not substitute it .
It act by :
2
Phototherapy :-
Phototherapy
photoisomerization which is conversion of toxic ind. B.unconj ( 4 Z, 15 Z ) to unconj isomer (4 Z , 15 E ) that can be excreted in the bile with out need of conjucation .
Structural isomerisation which convert native B .by irreversible reaction to lumirubin that is excreted in urin & bile with out conjucation .
Photoxidation that convert it to small polar product which can excreted in urin
3
Phototherapy
The therapeutic effect of phototherapy depend onirradiance of light used
distance between infant & light
amount of skin exposed
4
6
Conventional (Standard)Phototherapy
phototherapy is provided at an irradiance of 10 microwatts per square centimeter per nanometer (mW/cm2 per nm).
distance from infant is 45 cm
Usually used for mild elevation of TSB , not rapidly increase and no hemolysis
Intensive Phototherapy
use special blue light that provided an irradiance of 30 mW/cm2 per nm or more .
placed 15 – 20 cm from infant & using fiberoptic phototherapy blanket put under the patient for maximal skin exposure
used when ind bilirubin reach maximal level or rapidly increase or hemolysis
6
Phototherapy need 6–12 hr to produce measurable effect to decrease TSB .
naked all except for eye patch & baby should turn frequently (every 2 hr )for maximal exposurefluid intake increase by 10- 20 % due to over heating & dehydration ) , weigh & temp check daily .
7
Phototherapy
Baby with hemolysis or TSB near toxic level TSB & PCV must be check every 4 – 8 hr while patient with lower level do TSB & PCV every 12 – 24 hr .not rely on color for evaluation while he is on phototherapy .
Monitor TSB continued for 24 hr. after stop of phototherapy especially in patient with hemolytic anemia because of unexpected rise may occur
8
phototherapy
9
Phototherapy side effect
heating & dehydration , increase 10 – 20 % of maintenanceloose stool & diarrhea .
erythematous macular & purpuric rash & transient porphyraemia .
chilling .
eye injury & nasal closure from bandage
Bronze Baby Syndrome ( dark grayish brown ) especially in patient with direct or cholestatic jaundice , so should be avoid in patient with direct hyperbilirubinaemia ,
C/I in patient with porphyria
10
Exchange transfusion
Rx of hyperB.& prevention of B. level from reach to degree that is toxic to brain , byremoval of billirubin from plasma
remove partially hemolysed
remove Ab coated RBC
remove unattached Ab
replaced by donar RBC which should lacking the sensitizing Ag.
11
exchange transfusion
The donor blood fresh (< 5 day old) irradiated whole bloodRh incomp.
befor delivery donor blood O –ve , compatible with mother
After delivery , blood obtained from Rh - ve donar whose cells are compatible with both mother & infant .
usually use type O –ve if mother’s & baby’s ABO group incompatible , but when mother and infant has the same ABO use Rh – ve and this ABO type .
ABO incomp.
use type O Rh –ve or Group O blood of and Rh type of infant should be used crossed match with mother & infant .
12
exchange transfusion
Blood volume to be exchanged is about double the blood volume of infant (2 x 85 mL x Bwt ) .Stomach emptied before exchange to prevent aspiration
body temp. should be maintained & check vital sign ,
under strict aseptic technique & umbilical vein is canulated with catheter to distance not more than 7 cm in full term , some time use peripheral large vessel .
13
exchange transfusion
ET carried out over 45 – 60 min. , alternate aspiration & infusion of 20 ml. Each time & sometimes 5 – 10 ml. Each time in sick patient or premature .
After ET , TSB decrease to ½ the pre exchange level immediately but rebound again 40 – 50 % within hours so we must do TSB at 4 – 8 hr. interval after exchange .
Repeated ET may needed to prevent Kernicterus.
14
exchange transfusion
15
exchange transfusion
16
exchange transfusion
Acute comp. (5- 10 % )Hypoglycaemia ( before , during , after ) .
Hypocalcaemia ( due to anticoagulant ) .
Hypoxia Acidosis ( during ET , check pH & paCO2
Transient bradycardia with or without hypocalcaemia
Cyanosis , Vasospasm , Thrombosis .
Apnea with bradycardia
NEC ( rare ) .
thrombocytopenia, volume overload, arrhythmias
Death 0.3 % .
17
exchange transfusion
Late complicationsCholestasis .
Infection CMV, Hepatitis , HIV
Late anaemia ; hemolytic or hypo regenerative ; Rx by iron , erythropoitin , or blood transfusion .
Mild graft versus host reaction ( diarrhea , rash , hepatitis , eosinophilia
Inspissated bile syndrome ; rare jaundice persist for weeks or months
Portal vein thrombosis & portal hypertension .
18
Metalloporphyrins or TinMesoporphyrin
reduce bilirubin by inhibition of heme-oxygenaseand decrease the need for phototherapy.
A single dose on the 1st day of life may reduce the need for phototherapy. Used when jaundice is anticipated, particularly in patients with ABO incompatibility or G6PD deficiency or when blood products are discouraged .
S/ E : Transient erythema when given with phototherapy
19
IV immunoglobuline ( IVIG )
adjunctive treatment for hyperbilirubinemia due to isoimmune hemolytic disease.when bilirubin approaching exchange levels despite maximal interventions with phototherapy. shown to reduce the need for exchange transfusion in both ABO and Rh hemolytic disease, presumably by reducing hemolysis.
20
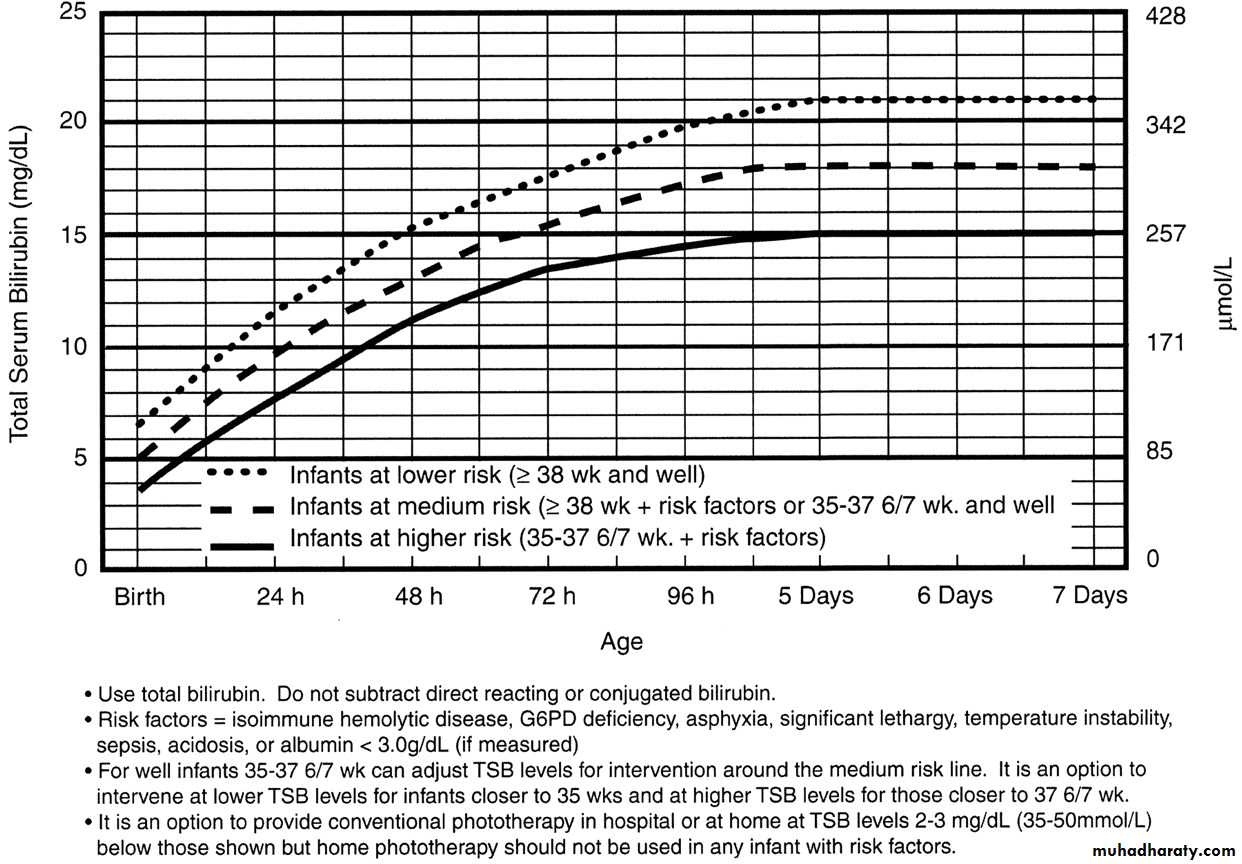
strategies for treatment of indirect hyperbilirubinemia in infants 35 or more weeks
the goal of therapy is to prevent indirect bilirubin related neurotoxicity ( kernicterus ) . Phototherapy and exchange transfusion remain the primary treatmentBecause phototherapy may require 6–12 hr to have a measurable effect, it must be started at bilirubin levels below those for exchange transfusion.
When identified, underlying medical causes of elevated bilirubin and physiologic factors that contribute to neuronal susceptibility should be treated (antibiotics for septicemia and correction of acidosis)
21
use a graph for Guidelines of intensive phototherapy & exchange transfusion level in hospitalized infants 35 or more weeks ’gestation . Which depend on
TSB level ,
age in hours days ,
gestational age ,
Infant condition & presence of risk factors
22
strategies for treatment of indirect hyperbilirubinemia in infants 35 or more weeks
risk factors
that cause kernicterus at lower bilirubin levelisoimmune hemolytic anemia , G6PD deficiency
asphyxia , IVH .
lethargy ,
temperature instability
sepsis , meningitis ,
acidosis ,
hypoalbuminemia
Hypoglycemia .
23
Fig 1. Guidelines for phototherapy in hospitalized infants (already present in hospital since birth ), of 35 or more weeks’ gestation. intensive phototherapy should be used when the TSB reach or exceeds the line indicated for each category.
If TSB is not decreasing and moving to level of exchange transfusion, we must see exchange transfusion graph , and this strongly suggests the presence of hemolysis or sepsis .
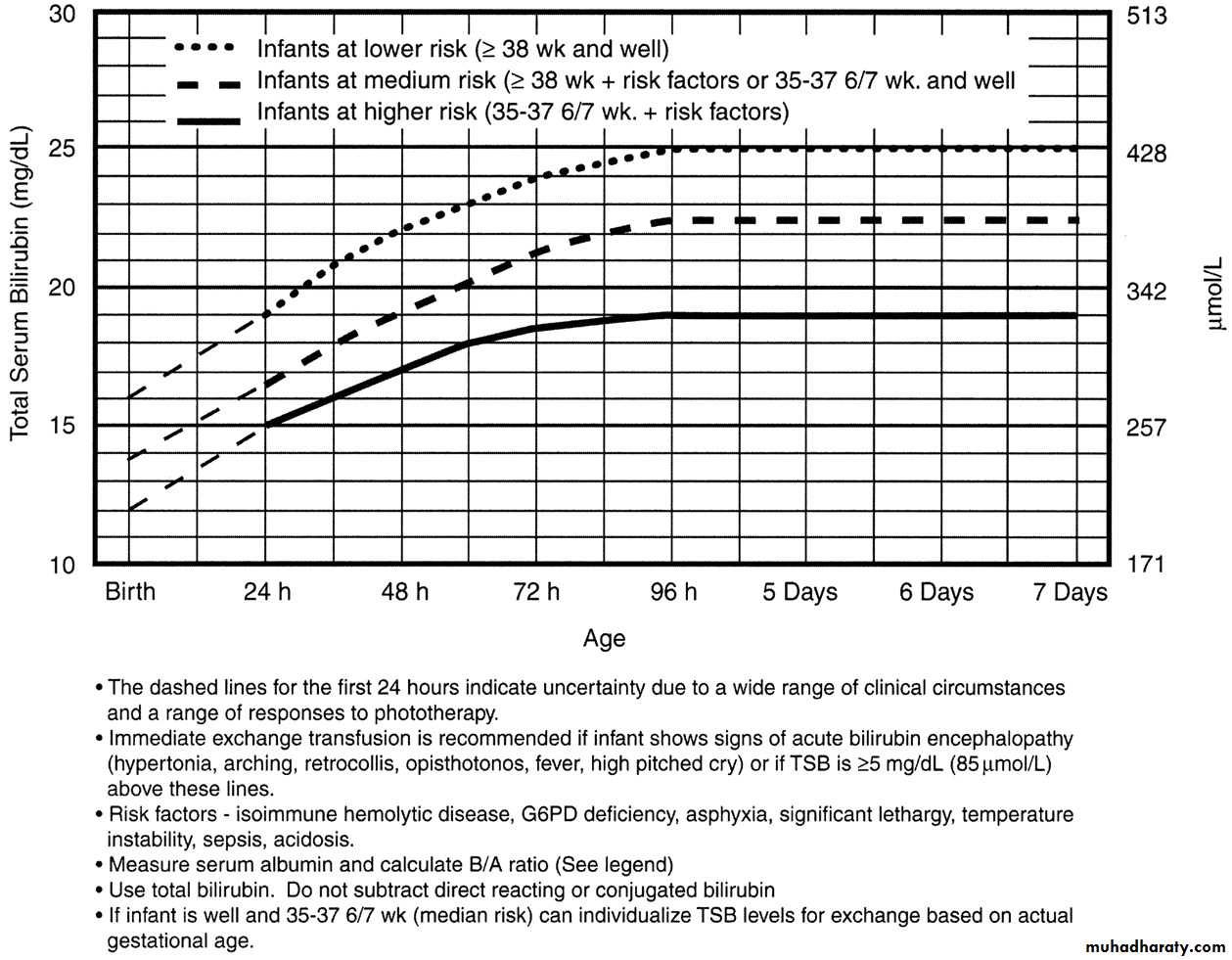
Fig . Guidelines for exchange transfusion in infants 35 or more weeks’ gestation. During birth hospitalization, exchange transfusion is recommended if the total serum bilirubin (TSB) rises to these levels despite intensive phototherapy. determining the need for exchange transfusion
For readmitted infants
if the TSB level is above the exchange level in graph, at any time orIf TSB ≥25 mg/dL in (well , ≥ 38 wk gestation ) after 72hour age or
≥20 mg/dL in a sick infant or infant <38 wk gestation after 72hour age , prepare blood and cross match that in case an exchange transfusion is necessary and put baby on intensive phototherapy repeat TSB measurement every 2–3 hr and consider exchange if the TSB remains above the levels indicated ( in graph ) after intensive phototherapy for 6 hr.
28/2/2005
27For readmitted infants
If TSB ≥25 mg/dL (428 ?mol/L), repeat TSB within 2-3 hr , If TSB 20–25 mg/dL (342–428 μmol/L), repeat within 3–4 hr. If TSB <20 mg/dL (342 μmol/L), repeat in 4–6 hr. If TSB continues to fall, repeat in 8–12 hr
When TSB is <13–14 mg/dL (239 μmol/L), discontinue phototherapy
measure TSB 24 hr after discharge to check for rebound
B : A ( bilirubin \ albumin )ratios can be used together but not instead of TSB level as an additional factor in determining the need for exchange transfusion.
28/2/2005
28If any signs of Kernicterus (bilirubin encephalopathy ). are noted during evaluation or Rx as suggested any where in figure or at any level of B. , emergency ET must be performed .
In infants with isoimmune hemolytic disease and TSB level rising in spite of intensive phototherapy or within 2–3 mg/dL (34–51 μmol/L) of exchange level , administer intravenous immunoglobulin 0.5–1 g/kg over 2 hr and repeat in 12 hr if necessary
28/2/2005
29
Use total bilirubin , do not subtract direct (conjugated) bilirubin
In unusual situations in which the direct bilirubin level is 50% or more of the total bilirubin, there are no good data to provide guidance for therapy, and consultation with an expert pediatric gastroenterologist is recommended ,In patient with isoimmunization
if not need immediate exchange transfusion at birth , we should put him after birth immediately on phototherapy & the decision to do exchange transfusion should be based on judgment that the infant has hight risk of rapid development of dangerous degree of anemia & hyperB. .
cord blood TSB > 5 mg/dL , Hb <10mg suggest sever hemolysis but inconsistently predict the need of ET . Some physician consider Retic. Count > 15 % ,previouse K or erythroblastosis & prematurity to be additional factor support decision of ET .
31
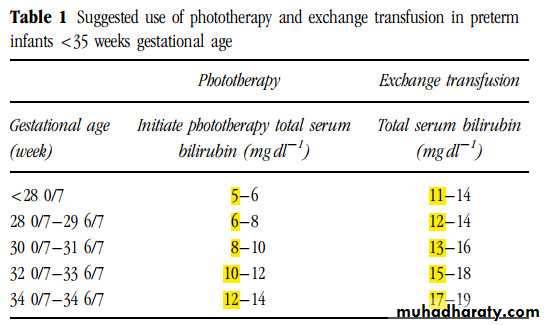
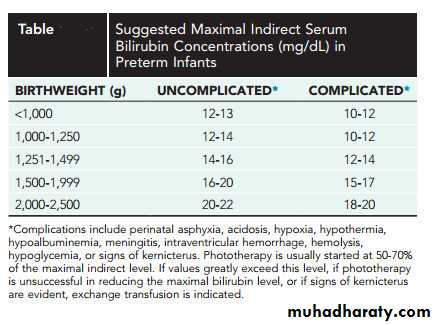
In premature infant less than 35 weeks of gestation
Depend on gestational age and Infant condition & presence of risk factors for development of kernicterus at lower levelUse the lower range of the listed TSB levels for infants at greater risk for more bilirubin toxicity and kernicteruse
32
Also for premature baby
Risk include perinatal asphyxia , acidosis , hypoxia , hypothermia , hypoalbuminaemia , meningitis , intraventricular haemorrhage , haemolysis , hypoglycaemia , or signs of K.33
34