
1
Fifth stage
pediatric
Lec-
.د
اثل
17/11/2015
Hemolytic Uremic Syndrome
• HUS is characterized by the triad of microangiopathic hemolytic anemia,
thrombocytopenia, and renal injury and is an important cause of acute
renal injury in children.
• HUS typically occurs in children <5 years of age but can occur in older
children.
Types of HUS:
Typical HUS (D+HUS):
It is the most common type of HUS. It occurs in children <5 years of age.
It is associated with a prodromal diarrheal illness “D+HUS”, contamination of
meat, fruit, vegetables, or water with verotoxin (VT) producing E. coli ( most
commonly E.coli O157:H7) is responsible for many outbreaks.
Atypical HUS
HUS presenting without a prodrome of diarrhea (D-HUS), may occur at any
age.
The clinical course is usually more severe than that of D+HUS.
D-HUS due to:
o 2ry to infection (Streptococcus pneumoniae, HIV)
o Genetic & acquired defects in complement regulation.
o Medications.
o Malignancy.
o SLE.
o Pregnancy.
CLINICAL MANIFESTATIONS
• Classic D+HUS typically begins as gastroenteritis, often bloody, followed in
7 to 10 days by weakness, lethargy, irritability, and oliguria/anuria.
2
• Physical examination reveals irritability, pallor, edema, petechiae, and
occasionally hepatosplenomegaly. Dehydration is often present; however,
some children have volume overload. Hypertension may be due to volume
overload or renal injury.
• CNS involvement, including seizure occur in up to 25% of the cases.
• Other organs involvement includes: pancreatitis, cardiac dysfunction &
colonic perforation.
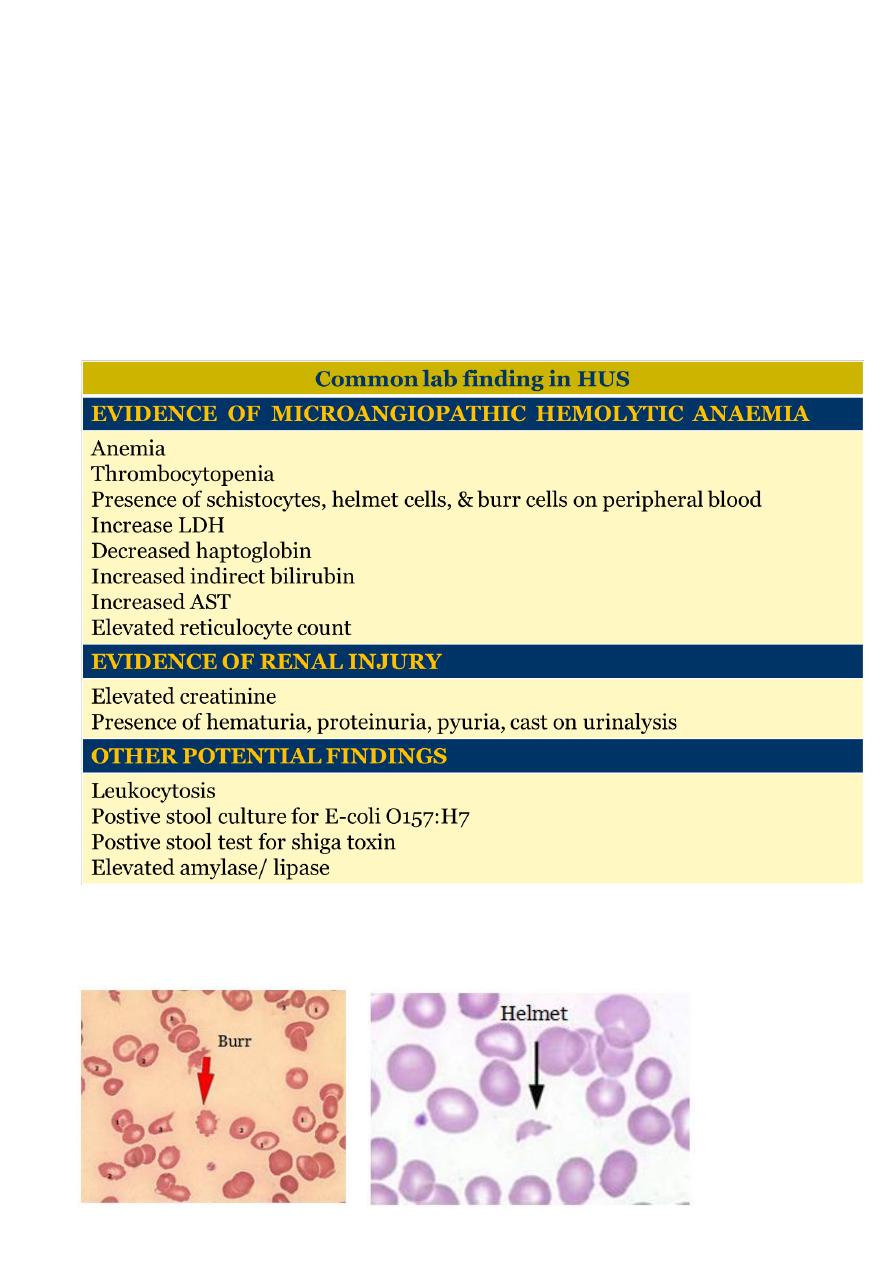
DIAGNOSTIC STUDIES
3
TREATMENT
• Therapy for HUS is supportive and includes volume repletion, control of
hypertension, and managing complications of renal insufficiency, including
dialysis when indicated.
• Early hydration during the diarrheal phase may lessen the severity of renal
insufficiency.
• Red blood cell transfusions are provided as needed.
• platelet transfusions are indicated only during active hemorrhage or
anticipation of a procedure.
• Antibiotics & antidiarrheal agents may increase the risk of developing HUS.
PROGNOSIS
• Most children (>95%) with D+HUS survive the acute phase & recover
normal renal function.
• D-HUS, familial cases, and sporadic HUS have poorer outcomes.
Henoch-Schönlein Purpura
ETIOLOGY
Henoch-Schönlein purpura (HSP) is a vasculitis of unknown etiology
characterized by inflammation of small blood vessels with leukocytic infiltration
of tissue, hemorrhage, and ischemia. The immune complexes associated with
HSP are predominantly composed of IgA.
EPIDEMIOLOGY
• HSP is the most common systemic vasculitis of childhood and cause of
nonthrombocytopenic purpura.
• It occurs primarily in children 3 to 15 years of age, although it has been
described in adults.
• HSP is slightly more common in boys than girls
• Occurs more frequently in the winter than the summer months
4
CLINICAL MANIFESTATIONS
• HSP is characterized by rash, arthritis, and, less frequently, gastrointestinal
or renal vasculitis.
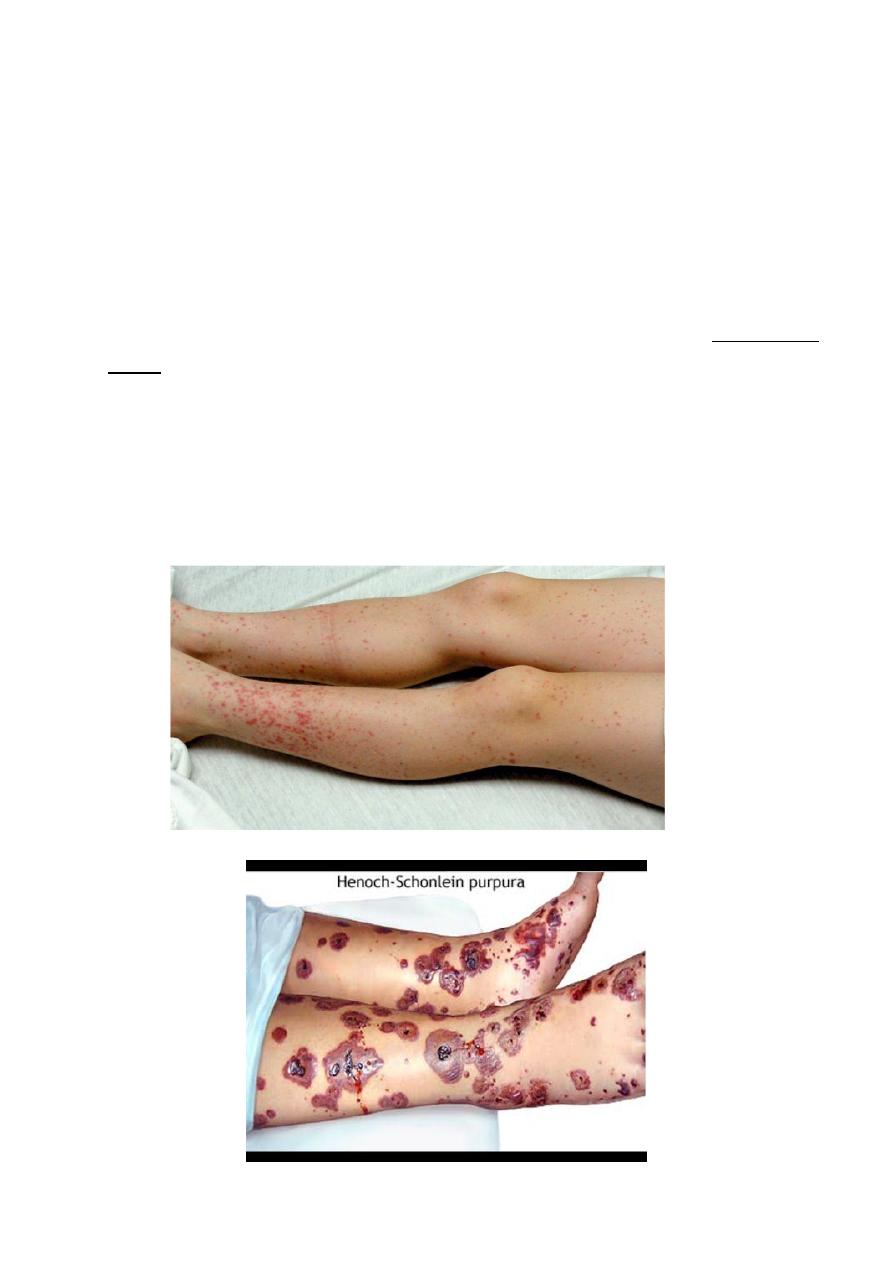
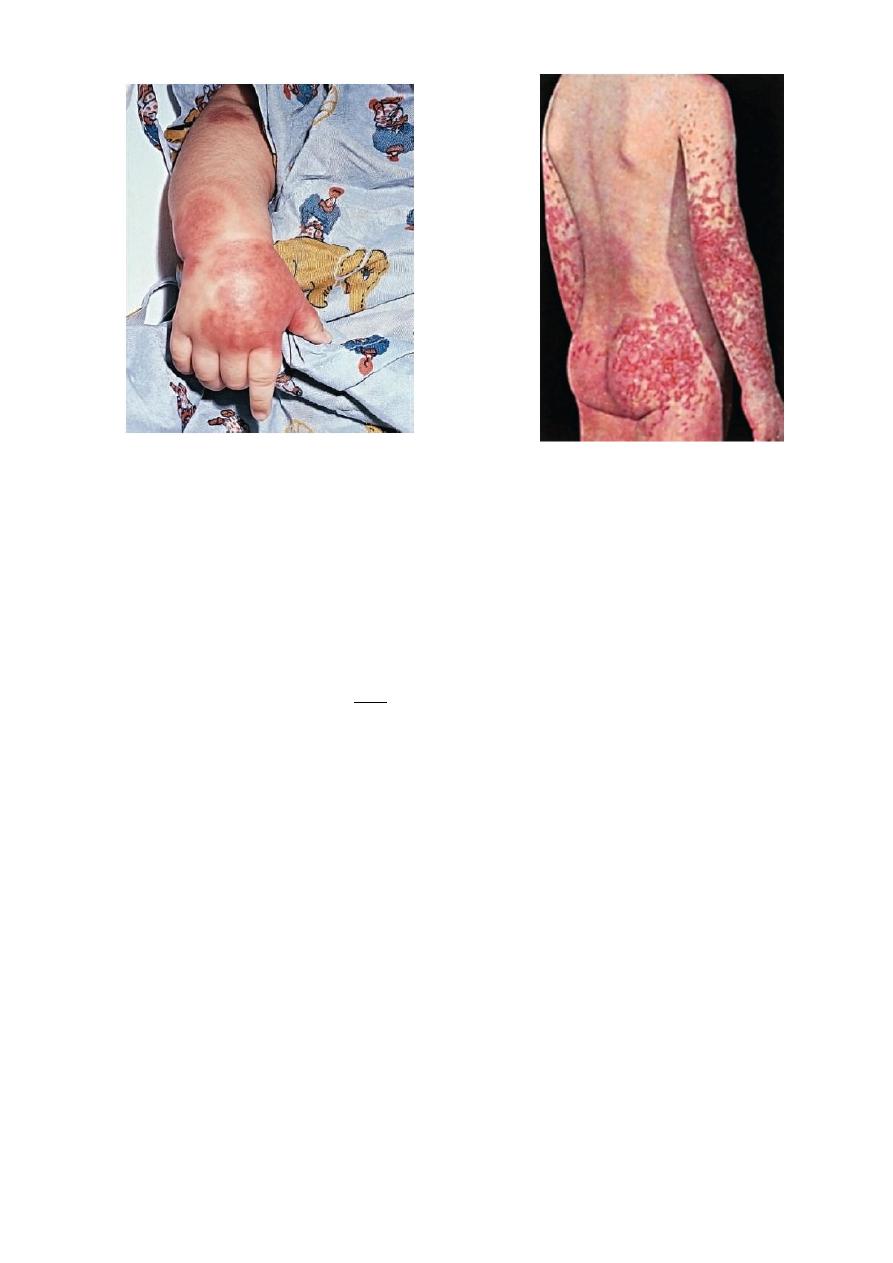
Rash
• The hallmark of HSP is palpable purpura, caused by small vessel
inflammation in the skin leading to extravasation of blood into the
surrounding tissues. IgA often is deposited in the lesions. Although the
rash can occur anywhere on the body, it is classically found in dependent
areas, below the waist on the buttocks and lower extremities.
• The rash can begin as small macules or urticarial lesions but rapidly
progresses to purpura with areas of ecchymosis. The rash also can be
accompanied by edema, particularly of the calves and dorsum of the feet,
scalp, and scrotum or labia.
5
Arthritis
• Arthritis occurs in 80% of patients with HSP; it can occur in any joint but
tends to affect the lower extremities, most commonly the ankles and
knees. The arthritis is acute and can be very painful with refusal to bear
weight.
• The arthritis of HSP does not leave any permanent joint damage; it does
not typically recur.
GIT
• Gastrointestinal involvement occurs in about one half of affected children.
• Typically presents as mild to moderate crampy abdominal pain, thought to
be due to small vessel involvement of the gastrointestinal tract leading to
ischemia.
• Less commonly, significant abdominal distention, bloody diarrhea,
intussusception, or abdominal perforation occurs and requires emergent
intervention.
• Gastrointestinal involvement is typically seen during the acute phase of
the illness. It may precede the onset of rash.

6
Renal
• One third of children with HSP develop renal involvement, which can be
acute or chronic.
• Although renal involvement is mild in most cases, acute
glomerulonephritis manifested by hematuria, hypertension, or acute renal
failure can occur.
• Most cases of glomerulonephritis occur within the first few months of
presentation, but rarely patients develop late renal disease, which
ultimately can lead to chronic renal disease, including renal failure.
CNS
• Neurologic manifestations of HSP, caused by hypertension or CNS
vasculitis, may also occur. They include intracerebral hemorrhage,
seizures, headaches, and behavior changes.
Others
Other less-common potential manifestations of HSP are:
• Orchitis.
• Testicular torsion.
• Pancreatitis
• Carditis.
• Pulmonary hemorrhage.
• Inflammatory eye disease.
LABORATORY AND IMAGING STUDIES
• No laboratory finding is diagnostic of HSP.
• Common but nonspecific findings include ESR, CRP, and WBC count are
elevated in patients with HSP.
• The platelet count is the most important test, because HSP is
characterized by nonthrombocytopenic purpura with a normal, or even
high, platelet count, differentiating HSP from other causes of purpura that

7
are associated with thrombocytopenia such as autoimmune
thrombocytopenia, SLE, or leukemia.
• A serum blood urea nitrogen and creatinine should be obtained to
evaluate renal function.
• Serum albumin levels may be low due to renal or intestinal protein loss.
•
A urinalysis screens for evidence of hematuria. Testing the stool for blood
may identify evidence of gut ischemia. Any question of gut perforation
requires radiologic investigation
• Ultrasound
is often used in the setting of gastrointestinal complaints to
look for bowel wall edema or the rare occurrence of an associated
intussusception
.
• Barium enema
can also be used to both diagnose and treat
intussusception.
• Although often unnecessary in typical HSP, biopsies of skin and kidney can
provide important diagnostic information, particularly in atypical or severe
cases, and characteristically show IgA deposition in affected tissues.
Criteria for Diagnosis of Henoch-Schönlein Purpura
The diagnosis of Henoch-Schönlein purpura is based on the presence of two of
four criteria
.
8
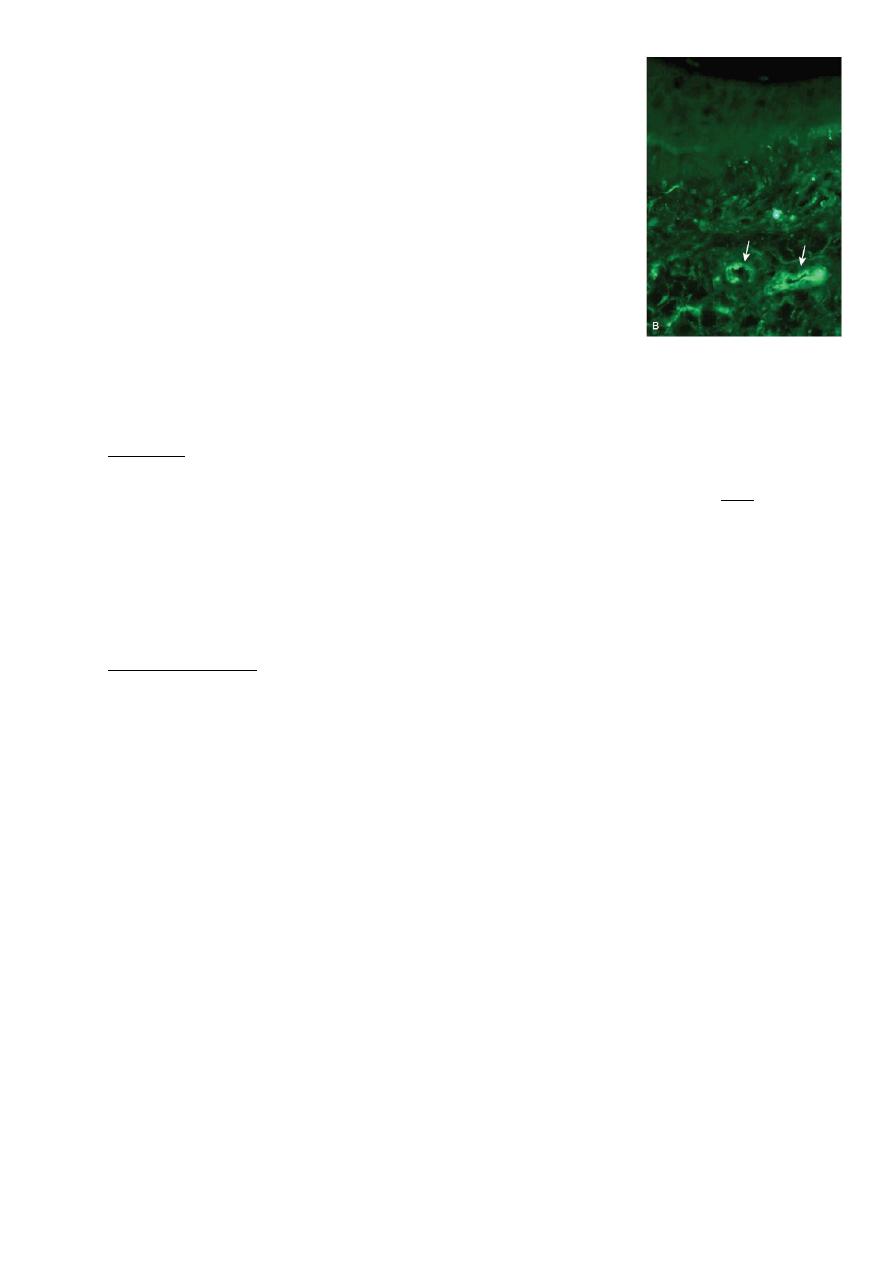
• Skin biopsy of patient with HSP,
showing direct immunofluorescence
of immunoglobulin A within the
walls of dermal capillaries.
TREATMENT
• Therapy for HSP is supportive, an emphasis on
assuring adequate hydration, nutrition, and analgesia.
• A short-term course of NSAI drugs can be administered for the acute
arthritis.
• Systemic corticosteroids usually are reserved for children with GIT disease
and provide significant relief of abdominal pain. A typical dosing regimen is
prednisone, 1 mg/kg/day for 1 to 2 weeks, followed by a taper schedule.
Recurrence of abdominal pain as corticosteroids are weaned may
necessitate a longer course of treatment.
• Acute nephritis typically is treated with corticosteroids but may require
more aggressive immunosuppressive therapy.
• Although few data are available to demonstrate efficacy, IVIG and plasma
exchange are sometimes used in the setting of severe disease.
PROGNOSIS
• The prognosis of HSP is excellent. Most children have complete resolution
of the illness without any significant sequelae.
• Patients with HSP renal disease (elevated blood urea nitrogen, persistent
high-grade proteinuria) are at highest risk for long-term complications,
such as hypertension or renal insufficiency, particularly if the initial course
was marked by significant nephritis.
There is a long-term risk of progression to end-stage renal disease in less than
1% of children with HSP. The rare patients who develop end-stage renal disease
may require renal transplantation. HSP may recur in the transplanted kidney
