
1
Lectures In
Internal medicine
Dr Dhaher Jameel Salih Al-habbo
FRCP London UK
Assistant Professor Department of Medicine.College of Mdicine
University of Mosul
lEC(1,2,3)
4th Stage
MMC&NMC
2015-2016
NAME:________________________________________
College :________________________________________
2
4th stage
باطنية
Lec-1
د.ظاهر
1/11/2015
ASTHMA
Asthma:
Chronic Inflammatory disorder of Bronchi characterized by ,Episodic, reversable Brochospasm resulting
from an exagurated Bronchconsrector response to a various stimuli(allergy).
Affects 10% of children& 5-7% adult
Pathophysiology
G
enetic susceptibilit
y
1
-Childhood asthma occurs in atopic individuals who produce IgE on exposure to small
amounts of common antigen.
2-Asthma in adults is called non-atopic, intrinsic or late-onset asthma.
3-First degree relatives of asthmatics have higher prevalence for asthma

3
Environmental factors
1
-Indoor environment and childhood exposure to allergen is very important in
determining sensitization.
2-House dust mites and pet-derived
allergens are wide spread in house
3-Fungal spores, cockroach antigens and nitrogen dioxide (gas cockers).
Environmental factors ;Out door like ; ozone, sulphur dioxide and air-borne
particles,smoking,Drugs and infection
Asthma Pathogenetic Types:
Extrinsic (Allergic/Immune)
Atopic - IgE
Occupational - IgG
Bronchopulomonary Aspergillosis - IgE
Intrinsic (Non immune)
Aspirin induced
Infections induced
Pathology:
*Inhaled allergen rapidly interacts with mucosal mast cells (IgE-Dependent mechanism).
This will results in histamine and leukotrienes release leading to bronchoconstriction.
*
*Airway edema, increased volume and size of sub mucosal glands.
desquamation of airway epithelial cells.
*
Clinical features:
1-Wheeze, breathlessness, cough, and sensation of chest tightness usually episodic
especially in children and atopic.
2-chronic and persistent wheeze is more common in older non-atopic patients with adult
asthma and it may be difficult to be differentiated from COPD.
4
3-Typically, there is diurnal variation in symptoms and peak expiratory flow
measurement being worse in the early morning. Cough and wheeze usually disturb the
patient sleep (Nocturnal asthma).
(cough variant asthma).
no wheezes
There may be cough with
4-Symptoms may provoked by exercise (exercise-induced asthma).
5-Acute sever asthma: Patient usually extremely distressed, using accessory muscles of
respiration, the chest is inflated and the patient is tachypnoeic.
Pulsus paradoxus (loss of pulse pressure on inspiration due to reduce cardiac return due
to sever hyperinflation) and sweating.
Central cyanosis in sever cases with silent chest and bradycardia.
Investigations:
*Spirometric measurement of FEV1/FVC ratio or PEF before and after bronchodilators
provide reliable indication of the degree of airflow obstruction, relation to exercise &the
reversibility after bronchodilators.
* Radiological.
analysis(ABGA)
Blood Gas
Arterial
*
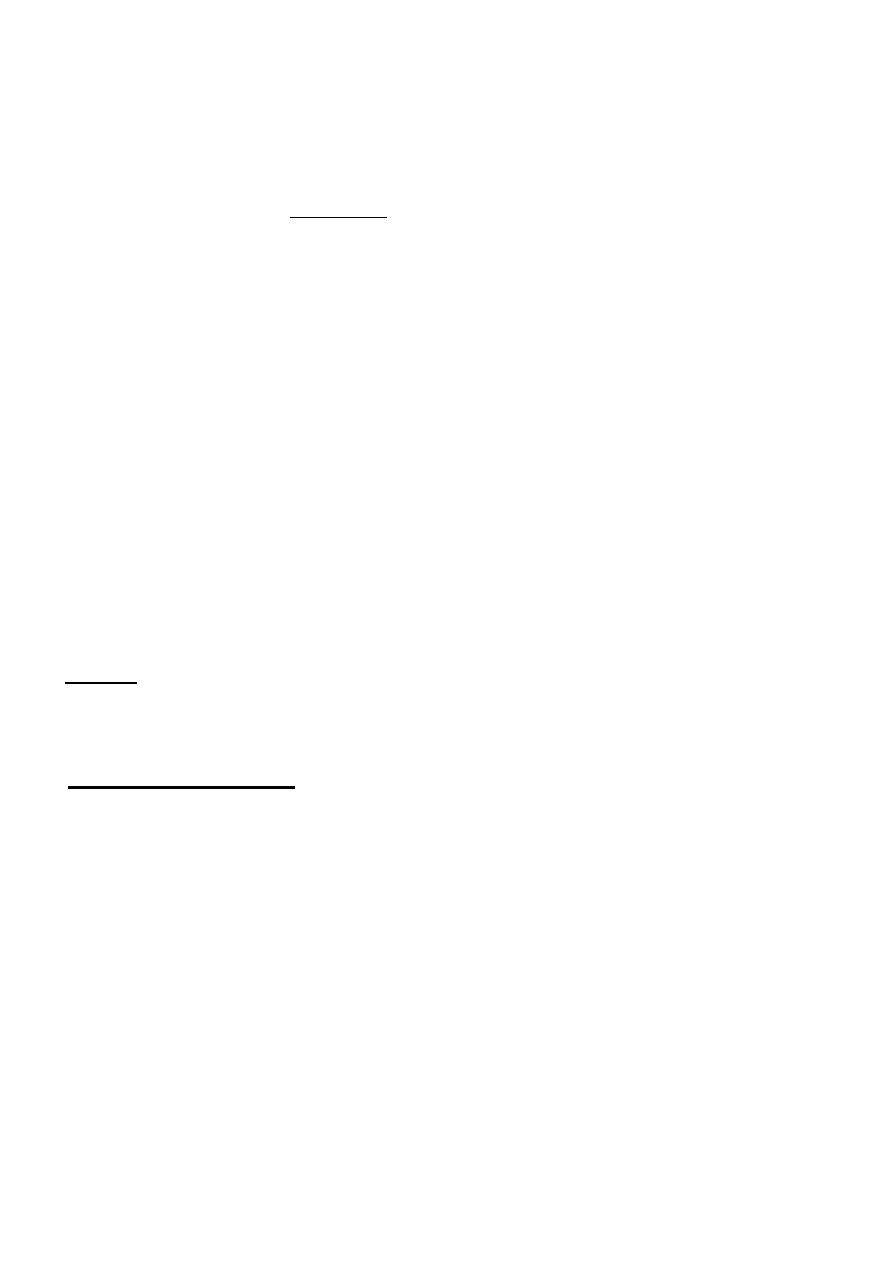
Management:
Patient education:
-
1
A
-The patient should be able to differentiate between reliever (bronchodilators) and
preventer (anti-inflammatory) medications
B-The patient should be fully capable of using the inhaler devices.
C- The patient should be fully capable of using the peak flow meter, to understand the
readings, to determine his personal best measurement and to record all these information
in his personal action plan.
5
Rescue short-course oral corticosteroid treatment:
The rescue course is in the form of
*- 30-60mg prednisolone orally daily
*-Continue as single morning dose until 2days after good control of the symptoms.
*-Tapering the dose to withdraw is required only if we continue treatment
for 3 weeks and more
.
:
of Acute sever Asthma
Immediate treatment
A- Oxygen should be given at the highest concentration.
To maintain a PaO2 of >8.5-9KPa.
B-High dose of inhaled
2-adrenoceptor agonist nebulised using oxygen (salbutamol
2.5-5mgor terbutaline5-10mg) repeated within 30 minutes if necessary. Inhaled
2-
adrenoceptor agonist can be given out side hospital by large volume spacers.
C-Systemic steroids; 30-60mg prednisolone orally or intravenous 200mg hydrocortisone.
6
::
ersist
If the features of severity of asthma p
*-Ipratropium bromide 0.5mg should be added to nebulised
2-adrenoceptor agonist.
*-Continue nebulised
2-adrenoceptor agonist every 15-30 minutes as necessary.
*-Magnesium sulphate (25mg/kg i.v, maximum 2gm)
*-Mechanical ventilation
.

7
4th stage
باطنية
Lec-2
د.ظاهر
1/11/2015
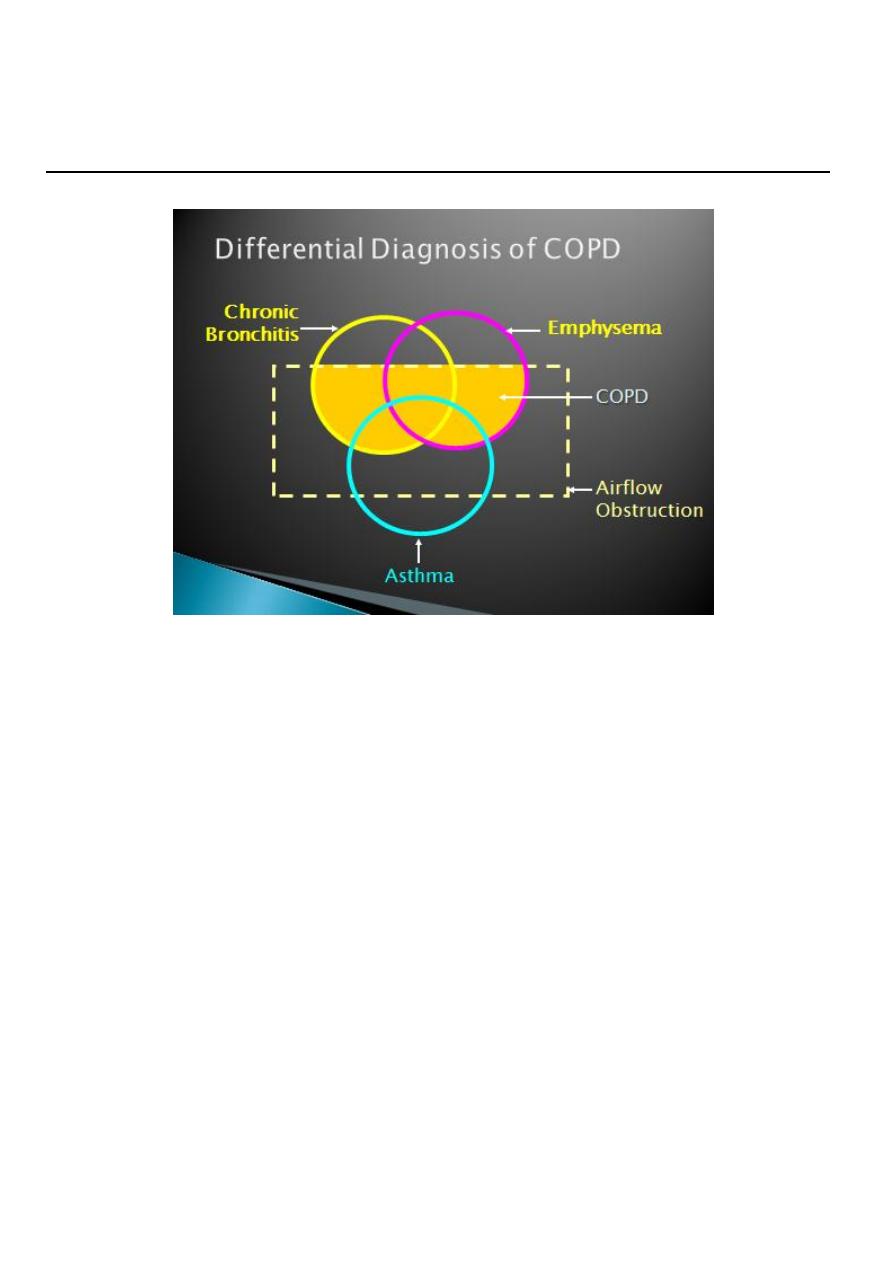
COPD
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COPD preventable and treatable lung disease with some extra pulmonary effects
*
*(muscle weakness, ↑ circulating inflammatory markers, impair water salt and
excretion, altered fat metabolism and ↑prevalence of osteoporosis)
PATHOPHYSIOLOGY OF COPD:
*Collapse of intrathoracic airways during expiration
Increase V/Q mismach↑dead space volume
*
*Flattening of the diaphragm and ↑horizontal alignment of intercostal muscles please
the respiratory muscles at a mechanical disadvantage with ↑ work of breathing..
Emphysema can be divided according to the pattern of enlarged air space
Emphysema is usually centriacinar involving respiratory bronchioles, alveolar ducts
and centrally located alveoli.
Panacinar and paraseptal emphysema with blebs or giant bullae.
smokers
years after starting .
12
-
10
Affects 10-15% of smokers
.
“
, spasm, and swelling
Chronic excessive mucus secretion .
Hypertrophy of mucus-secreting glands .
Smooth muscle hyperplasia.
Bronchial Hyperresponsivenes
Occurs in 50% of COPD patients

8
CLINICAL FEATURES(Chronic bronchitis):
Any patient who coughed up sputum on most days of at least 3 consecutive months
for more than 2 successive years.
This inflammation eventually leads to scarring of the lining of the bronchial tubes.
*Chronic bronchitis affects people of all ages, but is higher in those over 45 years
old.
*Incidence of chronic bronchitis in Females are increased by more than twice in
comparison to males
CLINICAL FEATURES(Emphysema):
pathological process of permanent destructive enlargement of the airspaces distal to
the terminal bronchioles.
Begins with the destruction of air sacs (alveoli) in the lungs where oxygen from the air
is exchanged for carbon dioxide in the blood. Damage to the air sacs is irreversible and
results in permanent "holes" in the tissues of the lower lungs.
Enquiry should be made as about the presence of oedema and morning headaches
which may suggest hypercapnia.
Breath sounds are typically quiet; crackles may accompany infection or bronchiactasis.
Leg oedema usually due to failure of salt and water excretion due to hypoxic and
hypercapnic kidney.
Right heart seldom “fails” in COPD
Clinical examination:
Clinical examination of the chest in mild to moderate disease might be normal.
Variable numbers of inspiratory and expiratory low to medial pitched ronchi are
audible in most patients.
Crackles(cripitations)which may disappear after coughing may be audible over the
lower zones.
9
:
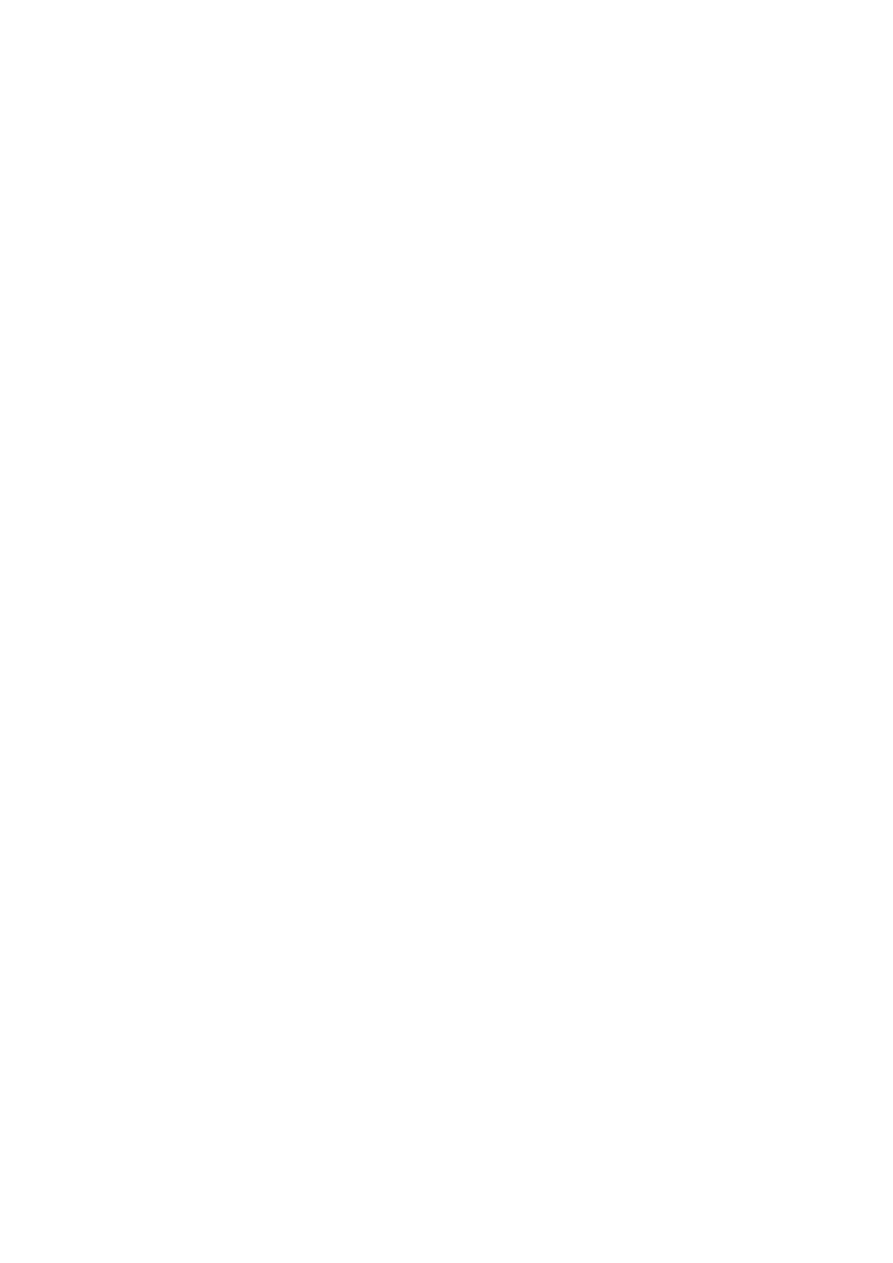
CLINICAL FEATURES
Ronchi, especially on forced expiration.
A reduction in the length of the trachea palpable above the sternal notch.
Trachea descent during inspiration (Tracheal Tug).
Contraction of sternomastoid and scalene muscles on inspiration
Excavation of the suprasternal and supraclavicular fossae during inspiration, together
with indrawing of the costal margins and intercostal spaces.
Increased antero-posterior diameter of the chest relative to the lateral diameter; loss of
cardiac dullness.
Loss of weight common (often stimulates unnecessary investigation).
Pursed lip breathing-physiological response to decrease air trapping.
Flapping tremor and bounding pulse (due to hypercapnia).
Peripheral oedema which may indicate corpulmonale.
Raised JVP, right ventricular heave, loud pulmonary second sound, tricuspid
regurgitation
Pink puffers; Thin and breathless and maintain a normal PaCO2 until the late stage of
disease
Blue bloaters; They tolerate hypercapnia earlier and may develop oedema and
secondarypolycythaemia
11
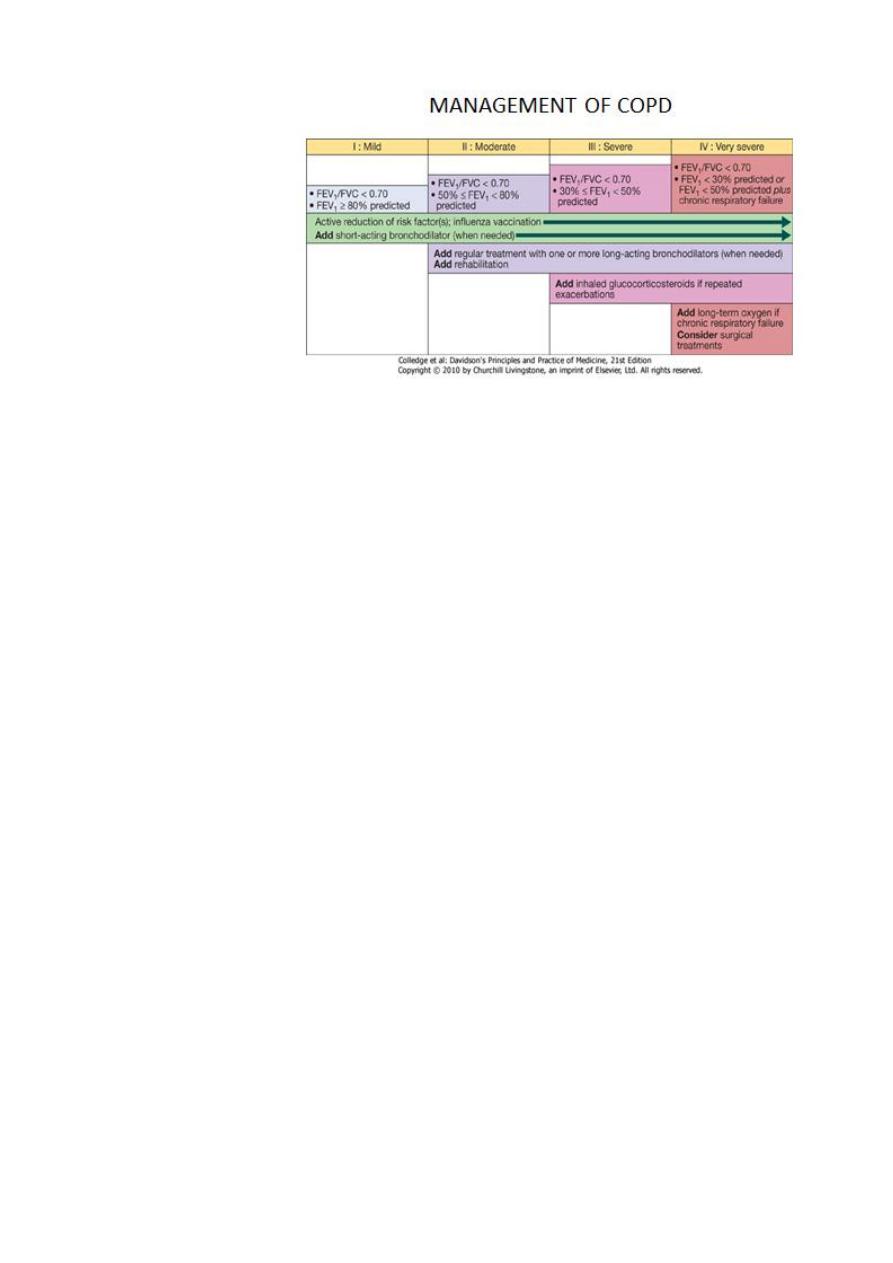
INVESTIGATIONS OF COPD:
Chest x-ray;To Look for lung cancer,bullae.
Complete blood count to document polysthaemia and to exclude
anaemia.
For young with basal emphysema α1-antiproteinaseassay.
Lung function test to document obstructive ventilatory defect with
partial response to bronchdilatores

11
Laboratory study:
• Arterial Blood Gas (ABG):
• 1-Markedly reduced arterial pO2
• 2-Elevated arterial pCO2 (40-50) mmHg
• Residual Volume increased .
• FEV1 decreased ,FEV1/FVC decreased .
• FEF 25-75 (mid-flows) decreased
•
Diffusion capacity (DLCO) near normal
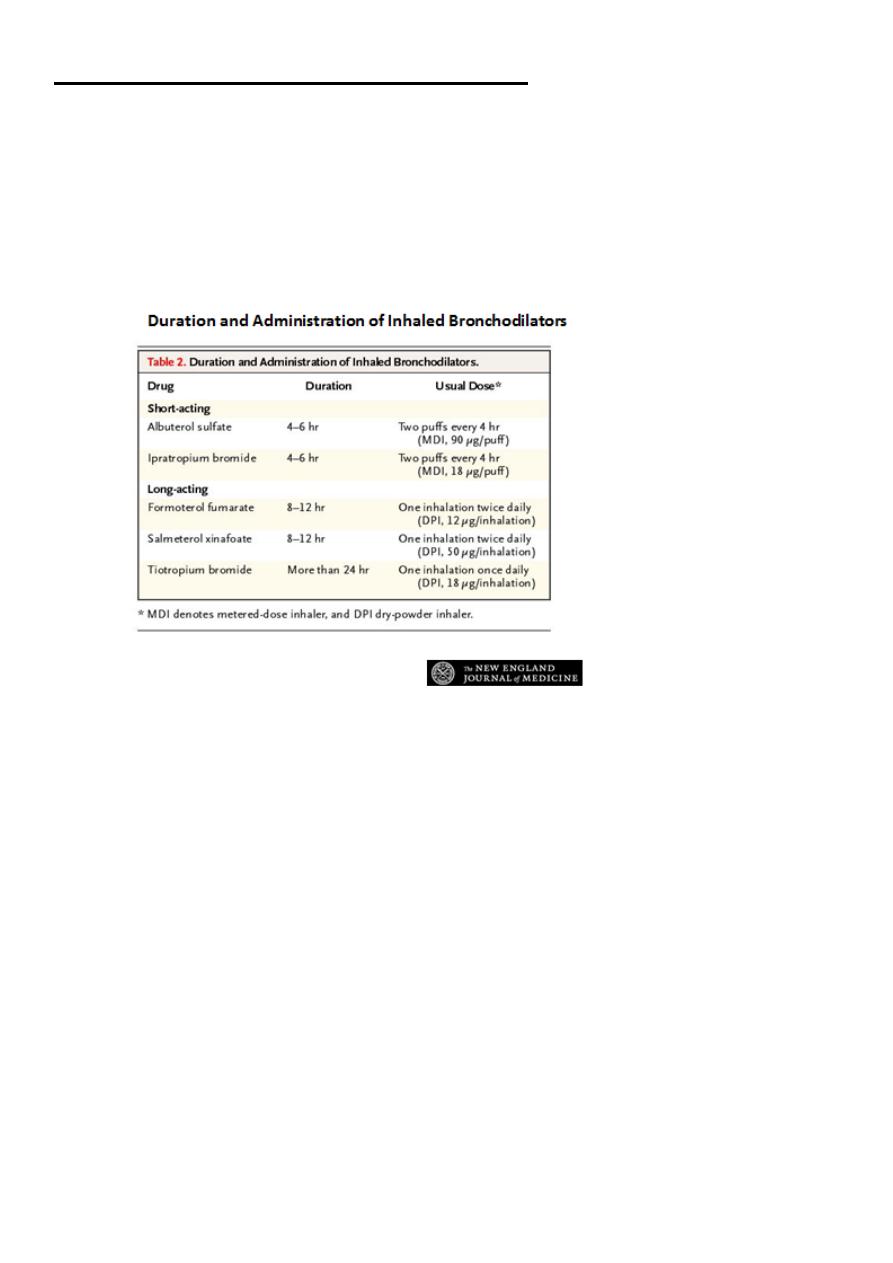
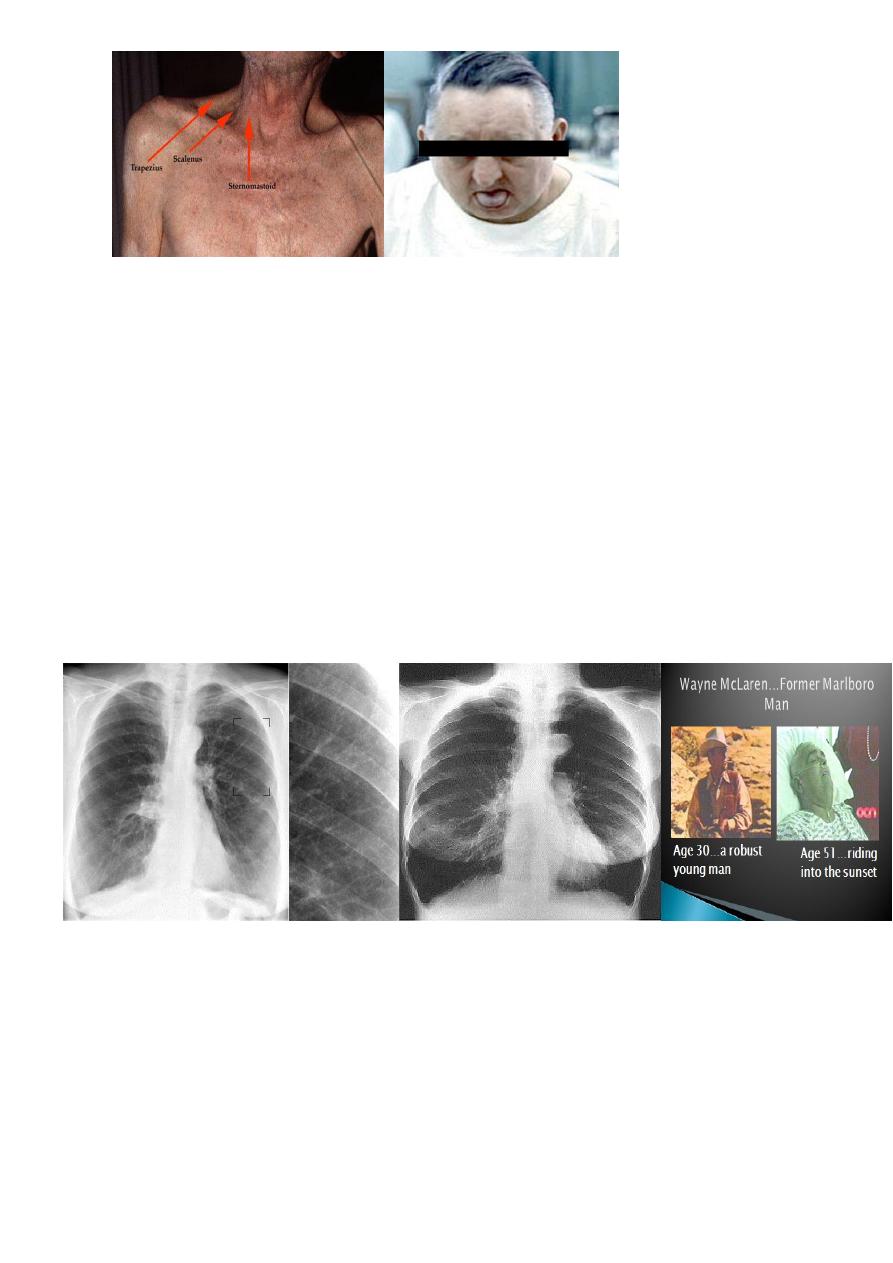
MANAGEMENT OF COPD:
A-Smoking cessation.
B-Bronchodilators.
C-Corticosteroids.
D-Pulmonary rehabilitation.
E-Oxygen therapy.
F-Surgical intervention.
G-Other measures.
H-Palliative care.
12
E-Oxygen therapy
Arterial blood gases in clinically stable patients on optimal medical therapy on at least
two occasion 3 weeks apart:
PaO2<7.3kPa(55mmHg) irrespective of PaCO2 and FEV1<1.5l.
PaO2 7.3-8 kPa(55-60mmHg)plus pulmonary hypertension, peripheral oedema or
nocturnal hypoxaemia.
Patient stopped smoking
Use at least 15hours/day at 2-4L/min to achieve a PaO2>8kPa(60mmHg) with out
unacceptable rise in PaCO
2

13
Treatments for Alpha1 antitrypsin deficiency-related (AAT) emphysema
Treatments for AAT deficiency emphysema including AAT
replacement therapy (a life-long process) and gene therapy are
currently being evaluated.
It is hoped that a clinical trial on gene therapy will take place
within the decade.
Vaccination in COPD:
• Although there is little evidence of a direct benefit of vaccination in patients with
COPD, It is recommend that;
• Pneumococcal vaccination and annual influenza vaccination should be offered to all
patients with COPD in an attempt to reduce both disease-specific mortality and
mortality from all causes.

14
4th stage
باطنية
Lec-3
د.ظاهر
1/11/2015
Pneumonia
Community-acquired pneumonia (CAP)
• UK figures suggest that an estimated 5-11/1000 adults suffer from CAP each year,
accounting for around 5-12% of all lower respiratory tract infections.
• The incidence varies with age, being much higher in the very young and very old, in
whom the mortality rates are also much higher.
• World-wide, CAP continues to kill more children than any other illness.
• Most cases are spread by droplet infection and occur in previously healthy individuals
but several factors may impair the effectiveness of local defences and predispose to
CAP.
• Strep. Pneumoniae remains the most common infecting agent, and thereafter, the
likelihood that other organisms may be involved depends on the age of the patient
and the clinical context.
• Viral infections are an important cause of CAP in children, and their contribution to
adult CAP is increasingly recognised.
Clinical features:
Pneumonia usually presents as an acute illness in which systemic features such as fever,
rigors, shivering and vomiting predominate .
• Pulmonary symptoms breathlessness and cough, painful and dry, but later
accompanied by the expectoration of mucopurulent sputum.
• Proteinaceous fluid and inflammatory cells congest the airspaces, leading to
consolidation of lung tissue.
• This improves the conductivity of sound to the chest wall (bronchial breathing and
whispering pectoriloquy).
• Crackles are often also detected
15
Common clinical features of community-acquired pneumonia (CAP):
• Streptococcus : Rapid onset, high fever and pleuritic chest pain;.
• Mycoplasma pneumoniae: Children and young adults.
• Rare complications include haemolytic anaemia, Stevens-Johnson syndrome,
erythema nodosum, myocarditis, pericarditis, meningoencephalitis, Guillain-Barré
syndrome.
• Legionella pneumophila:Middle to old age. Local epidemics around contaminated
source, e.g. cooling systems in hotels, hospitals. Person-to-person spread unusual.
Chlamydia pneumoniae, Haemophilus influenzae, Staphylococcus aureus.
Investigations:
• The objectives are to exclude other conditions that mimic pneumonia ,assess the
severity, and identify the development of complications.
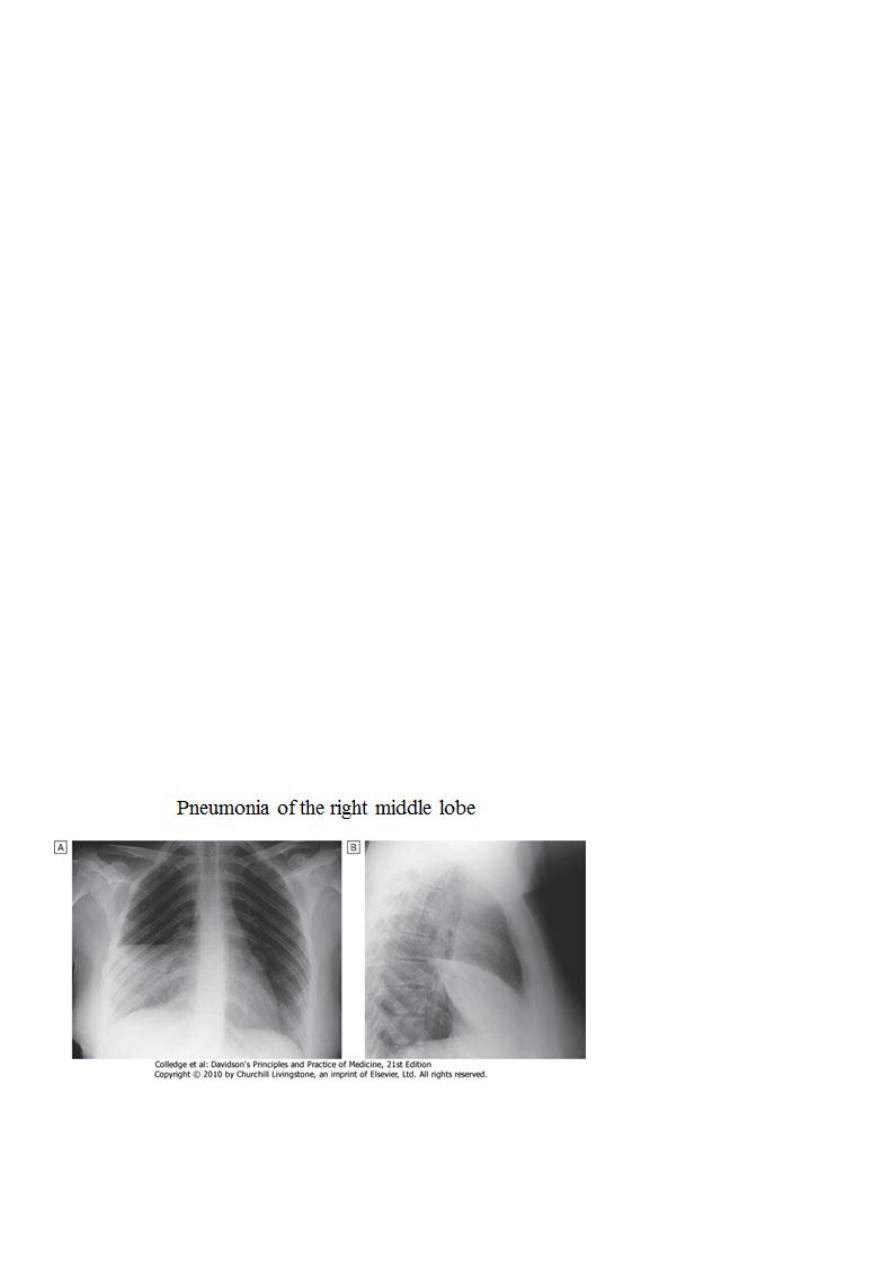
• A chest X-ray usually provides confirmation of the diagnosis. In lobar pneumonia, a
homogeneous opacity localised to the affected lobe or segment usually appears
within 12-18 hours of the onset of the illness .
• Radiological examination is helpful if a complication such as parapneumonic effusion,
intrapulmonary abscess formation or empyema is suspected.

16
• Many cases of CAP can be managed successfully without identification of the
organism, particularly if there are no features indicating severe disease.
• A full range of microbiological tests should be performed on patients with severe CAP
.
• The identification of Legionella pneumophila has important public health implications
and requires notification. In patients who do not respond to initial therapy,
microbiological results may allow its appropriate modification.
• Microbiology also provides useful epidemiological information
• All patients:
• Sputum:direct smear by Gram and Ziehl-Neelsen stains. Culture and antimicrobial
sensitivity testing
• Blood culture: frequently positive in pneumococcal pneumonia
• Serology: acute and convalescent titres for Mycoplasma, Chlamydia, Legionella, and
viral infections. Pneumococcal antigen detection in serum or urine
• PCR: Mycoplasma can be detected from swab of oropharynx
17
• Severe community-acquired pneumonia The previous tests plus consider:
• Tracheal aspirate, induced sputum, bronchoalveolar lavage, protected brush
specimen or percutaneous needle aspiration. Direct fluorescent antibody stain
for Legionella and viruses
• Serology: Legionella antigen in urine.
• Pneumococcal antigen in sputum and blood. Immediate IgM for Mycoplasma
• Cold agglutinins: positive in 50% of patients with Mycoplasma
• Pulse oximetry provides a non-invasive method of measuring arterial oxygen
saturation (SaO
2
) and monitoring response to oxygen therapy.
• Arterial blood gas is important in those with SaO
2
< 93% or with features of severe
pneumonia, to identify ventilatory failure or acidosis.
• The white cell count may be normal or only marginally raised in pneumonia caused
by atypical organisms, whereas a neutrophil leucocytosis of more than 15 × 10
9
/L
favours a bacterial aetiology.
• A very high (> 20 × 10
9
/l) or low (< 4 × 10
9
/l) white cell count may be seen in severe
pneumonia.
• Urea and electrolytes and liver function tests should also be checked.
• The C-reactive protein (CRP) is typically elevated
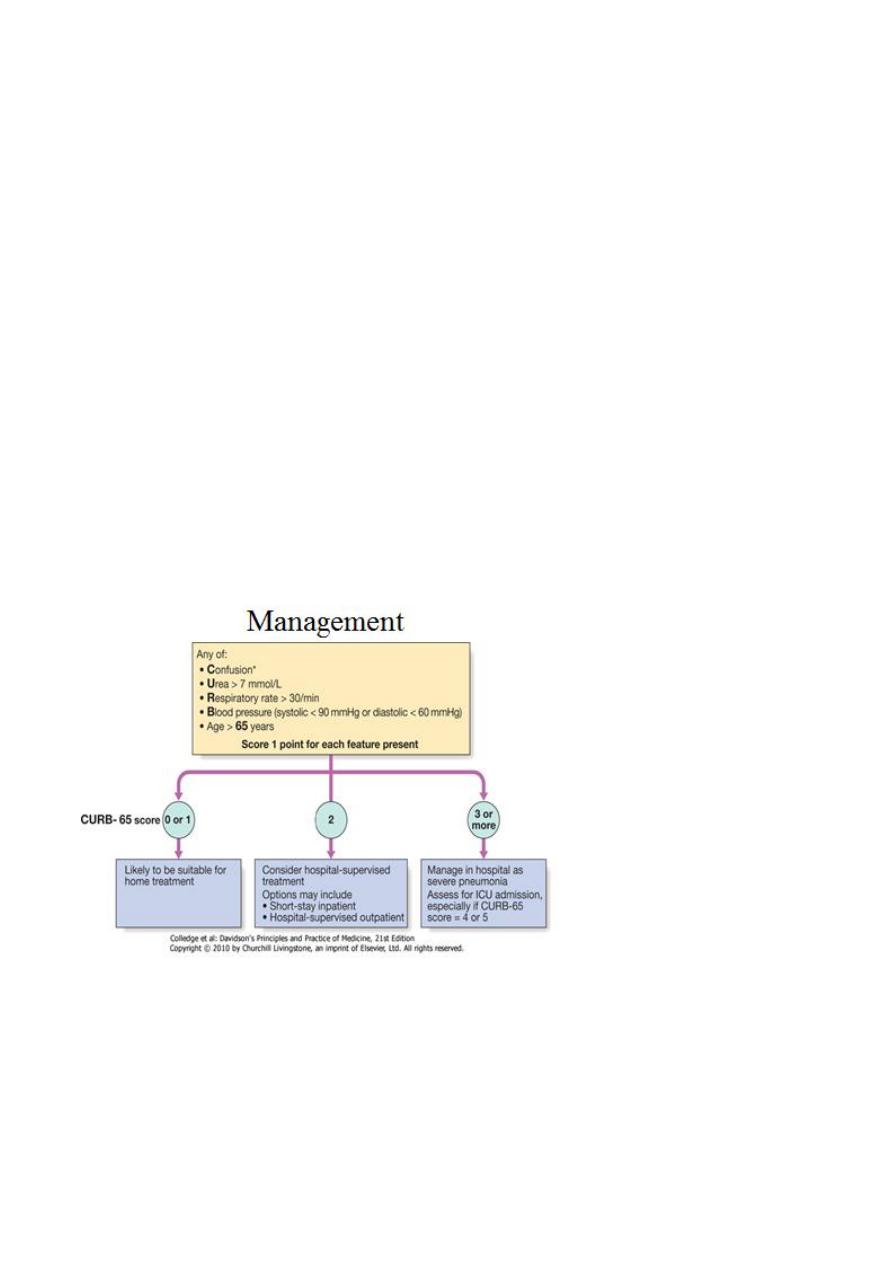
Management:
• Oxygen: should be administered to all patients with tachypnoea, hypoxaemia,
hypotension or acidosis with the aim of maintaining the PaO
2
≥
8 kPa (60 mmHg)
or SaO
2
≥
92%. High concentrations (≥ 35%), preferably humidified, should be used in
all patients who do not have hypercapnia associated with COPD.
• Assisted ventilation should be considered at an early stage in those who remain
hypoxaemic despite adequate oxygen therapy.
• Noninvasive Ventilation (NIV ) may have a limited role but early recourse to
mechanical ventilation is often more appropriate

18
• Fluid balance:
• Intravenous fluids should be considered in those with severe
illness, in older patients and in those with vomiting.
• Otherwise, an adequate oral intake of fluid should be encouraged.
• Inotropic support may be required in patients with circulatory
shock.
Antibiotic treatment:
• Prompt administration of antibiotics improves outcome.
• The initial choice of antibiotic is guided by clinical context, severity assessment, local
knowledge of antibiotic resistance patterns, and at times epidemiological
information, e.g. during a mycoplasma epidemic.
• In most patients with uncomplicated pneumonia a 7-10-day course is adequate,
although treatment is usually required for longer in patients with Legionella,
staphylococcal orKlebsiella pneumonia.
• Oral antibiotics are usually adequate unless the patient has severe illness, impaired
consciousness, loss of swallowing reflex or malabsorption.
Management:
• Most patients respond promptly to antibiotic therapy.
• However, fever may persist for several days and the chest X-ray often takes several
weeks or even months to resolve, especially in old age.
• Delayed recovery suggests either that a complication has occurred or that the
diagnosis is incorrect .
• Alternatively, the pneumonia may be secondary to a proximal bronchial obstruction
or recurrent aspiration.
• The mortality rate in adults managed at home is very low (< 1%); hospital death rates
are typically between 5 and 10%, but may be as high as 50% in severe illness
19
Antibiotic treatment for CAP:
• Uncomplicated CAP :Amoxicillin 500 mg 8-hourly orally.
• If patient is allergic to penicillin: Clarithromycin 500 mg 12-hourly orally or
Erythromycin 500 mg 6-hourly orally.
• If Staphylococcus is cultured or suspected: Flucloxacillin 1-2 g 6-hourly i.v. plus
Clarithromycin 500 mg 12-hourly i.v.
• If Mycoplasma or Legionella is suspected: Clarithromycin 500 mg 12-hourly orally or
i.v. or Erythromycin 500 mg 6-hourly orally or i.v. plus Rifampicin 600 mg 12-hourly
i.v. in severe cases.
• Severe CAP: Clarithromycin 500 mg 12-hourly i.v. or
Erythromycin 500 mg 6-hourly i.v. plus Co-amoxiclav 1.2 g 8-hourly i.v. or Ceftriaxone
1-2 g daily i.v. or Cefuroxime 1.5 g 8-hourly i.v. or
Amoxicillin 1 g 6-hourly i.v. plus flucloxacillin 2 g 6-hourly i.v.

21
Complications of pneumonia:
• Para-pneumonic effusion-common
• Empyema .
• Retention of sputum causing lobar collapse
• DVT and pulmonary embolism
• Pneumothorax, particularly with Staph. aureus
• Suppurative pneumonia/lung abscess
• ARDS, renal failure, multi-organ failure
• Ectopic abscess formation (Staph. aureus)
• Hepatitis, pericarditis, myocarditis, meningoencephalitis
• Pyrexia due to drug hypersensitivity
