
1
4th stage
نسائية
Lec-1
.د
اسماء
16/11/2015
Malposition of fetus
Vertex
The area of the skull between the anterior and posterior fontanelles,
and the parietal eminence Top of the skull
Occiput
Back of the fetal head behind the posterior fontanelle
Sinciput
That part of the fetal head in front of the anterior fontanelle.-forehead
or brow
Malposition:
Position :The relationship of a defined area on the presenting part
(Denominator) to the mother’s pelvis .
2
Occiputoposterior
Position
ed toward the
turn
with its
of the
of the
) or to the
Diagnosis:
Diagnosis during pregnancy is of no
importance, except that OP is a cause
of :
non engagement of the head before the onset of labor.
Early rupture of the membranes because of poorly engaged ,poorly
flexed head during labor.
Abdominal examination:
Slight flattening of the lower abdomen.
limbs are easily felt , anteriorly.
Difficult to define the back or to feel the fetal heart.
Slow descend of the head during labor because of wider diameter of the
poorly flexed head.
Vaginal examination:
High presenting part.
Early rupture of the membranes.
Easy to feel the anterior fontanelle behind the pubis (poorly flexed
head).
Both anterior and posterior fontanelle felt (less poorly flexed head )
Only posterior fontanelle felt posteriorly in well flexed head.
Diagnosis should be made early in labor because it will be difficult later
on because of the formation of caput succedaneum late in labor .This is
frequently happened and present with delay in the second stage.
3
Fingers may be passed above the caput to feel the sutures ,or the free
margin of an ear.
US in labor may be of help.
Course of labor in occipitoposterior positon:
70% spontaneous rotation to OA
10% short rotation to OP delivery as face to pubis.
Remainder assisted rotation will be required.
In the great majority of labors in the OP position is the same as in OT or
OA ,except that the occiput has to rotate through 135 degrees, instead
of 90 and 45 degrees respectively .This occurs if there is :
Effective uterine contraction.
Adequate flexion of the head.
Average size fetus.
Mechanism of labor in OP:
It depends on the head whether well flexed or incompletely flexed.
:occiput in advance meeting the resistance of the
The well flexed head
pelvic floor, slides on the gutter of the levator ani muscule with rotation
through 3/8 of circle, reaching the free space under the pubic arch.
Delivery of the head is by extension (as in ROA)
There is no delay in labor as the head
enter the pelvis with the subocciputo
bregmatic diameter(9.5)
Delivery as OA after spontaneous rotation
ad:
Incompletely flexed he
If there is large head or small pelvis
When the head is pushed during labor the
BPD is hindered if the pelvis is small or the head is large .

4
The forehead descend more easily than the occiput and enter the pelvis
incompletely.
The larger occiputofrontal diameter
(11.5)diameter present to the birth canal.
Neither the occiput nor the sinciput is
sufficiently in advance to influence rotation
spontaneously and alternative mechanism is
used for rotation and delivery.
Difficult and prolonged labor
no progress of labor without intervention
If there is small head or adequate pelvis
The forehead meets the resistance of the pelvic
floor, will rotates (1/8 of circle) to the front of the
subpubic area and the occiput to the hollow of the
sacrum.
delivery is by face to pubis ,the occiput delivered by flexion about the
nose ,followed by delivery of the forehead and the face and chin.
Large occiputofrontal diameter may result into wide perineal tear
Delivered as face to pubis
Incomplete forward rotation from occiputoposterior position with arrest
of the
head in the occiputo transverse position
described as deep transverse arrest of the
head and calls for assistance.
Assisted delivery to OT

5
Management of the first stage of labour
Nothing should be done to affect rotation of the head during the first
stage of labour.
Management is like normal labor with monitoring of the contraction,
dilatation, fetal heart rate.
Continuous epidural pain relief, allow time for spontaneous rotation.
Augmentation of contraction.
C.S. is indicated in case of no progress of first stage for few hours ,or
fetal distress.
Management of the 2nd stage of labor
Careful vaginal examination to diagnose the second stage (rectal
discomfort with desire to bear down)
Finding suggest that spontaneous rotation may not occur like
deflexion .
large caput succedaneum.
moulding .
Indication for interference are:
-failure of descend
-fetal distress
-maternal distress
Assisting delivery in OP:
Assistance is by rotation of the head
to OA to present a smaller more
favorable diameter to the birth canal.
Rotation can be performed :
-manual rotation and forceps delivery.

6
-kjelland’s forceps
-vacuum extractor.
Arrest at the pelvic outlet:
When the fetal scalp is easily visible at the vulval out let. further
progress is prevented by the muscles of the pelvic floor .
Adequate episiotomy.
Careful traction of the head by obstetric forceps in OP,or by vaccum.
Trial of forceps
In case of large head with 2/5 palpable with marked caput &moulding.
Outlet contraction (prominent ischial spines).
Head is not descend with contraction.
Trial of forceps in the operating theater with scrubbed staff and ready
for C.S. if there is :
-difficulty in applying the blades
-to much force needed to deliver the baby
We should resort to C.S. without delay and
Without risk to the mother and the baby.
Occipito transverse position OT
In which the head enter the pelvis in the occipitotransverse position.
Subsequently will rotate to:
ociipito –anterior position in majority of cases.
Occipitoposterior position in minority of cases.
In a small percent of cases,the head fails to rotate and persist in an OT
Rotation occurs because the head flexes as the leading part of vertex
meets the resistance of the pelvic floor and then rotates to adjust to the
shape of the gynaecoid pelvis

7
Causes:
Cephalopelvis disproportion.
Platypelloid or android pelvis.
Relaxed pelvic floor due to multiparity and epidural anasthesia.
Diagnosis:
Easy early labour.
May be difficult when labour is obstructed.(moulding ,caput)
Deep transverse arrest of the head: describe arrest of descend of the
head for a period of 1 hour .
Arrest occurs because of deflexion that accompanies the persistant OT
resulting in the larger occipitofrontal diameter(11cm)becoming the
presenting diameter.
commonly occurs with the vertex at the +1,+2 station.
Management:
During second stage :
Midpelvis is compromised =C.S.
Normal pelvis+ average size pelvis+inadequate uterine contraction
=oxytocine stimulation of labour.
Manual rotation,forceps delivery with kielland’s forceps if normal pelvis
,average size baby and the head at +1,+2 station (head occupy the
hallow of the sacrum.
8
4th stage
نسائية
Lec-2
.د
اسماء
16/11/2015
Malpresentation and malposition of fetus
Malpresentation :any fetal presentation other then vertex including
:breech, shoulder, face ,brow ,and compound presentation.
Cosequences:
Presenting part, ill-fitting
Uterine Contractions, poor
Membranes, rupture early- cord prolapse
Labour, difficult, long, obstructed
Birth trauma
Operative intervention
Increased perinatal and maternal mortality and morbidity
Fetal malformation
Intrauterine fetal death
Cord proplase
Birth trauma,
Birth asphysixa
Infection, fetus, neonate and mother
Uterine rupture
Thromboembolism in the mother.

9
For optimal result:
Early diagnosis,
Planned delivery
Experienced staff
Well equipped hospital
Cross match 2 unit
Adequate hydration
Monitor in Labour
Pain relief
Breech presentation
Breech presentation :
occurs when the fetal buttocks or lower extremities present into the
maternal pelvis.
Breech presentation occurs in 3-4% of all deliveries.
The occurrence of breech presentation decreases with advancing
gestational age. Breech presentation occurs in 25% of births that occur
before 28 weeks’ gestation, in 7% of births that occur at 32 weeks, and
1-3% of births that occur at term.
.
Perinatal mortality is increased 2- to 4-fold with breech presentation,
regardless of the mode of delivery. Deaths most often are associated
with malformations, prematurity, and intrauterine fetal demise.
Predisposing factor
prematurity,is major cause about 20 % are of low birth weight.
uterine abnormalities (malformations, fibroids).
fetal abnormalities (CNS malformations, neck masses, aneuploidy).
multiple gestations.
AF abnormality.
11
Abnormal placentation.
Contracted pelvis.
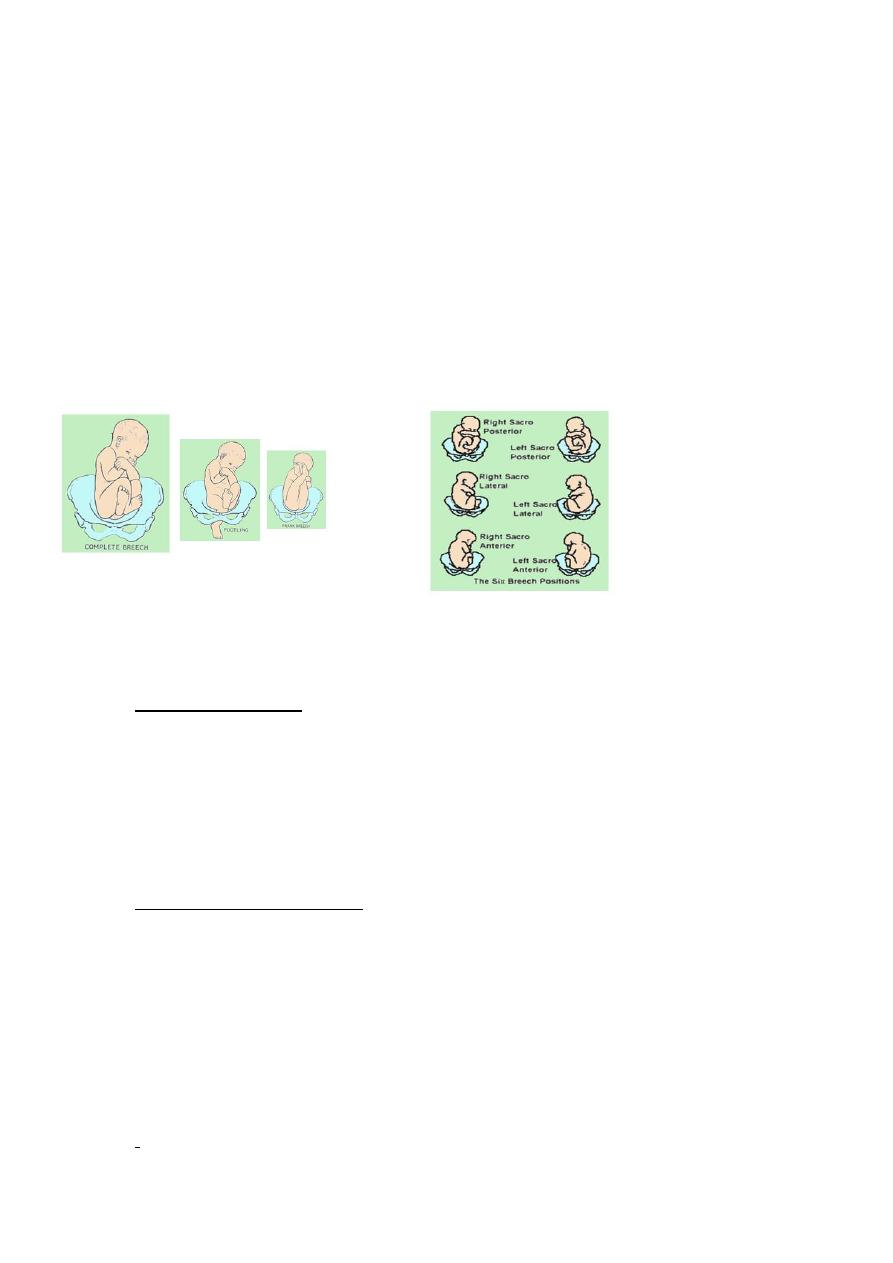
Types of breech presentation
Frank breech (65%) - Hips flexed, knees extended
Complete breech (25%) - Hips flexed, knees flexed
Footling or incomplete (10%) - One or both hips extended, foot
presenting
diagnosis
:
Diagnosis of breech
Palpations and ballottement(leopold man.)
Pelvic exam.
Ultrasound
X-ray studies.
Diagnose underlying cause
.
11
management
38 weeks of gestation
-
until 37
No action
Reason???
Exclude
fetal anomalies
Placenta previae
Multiple pregnancy
Offer external cephalic version (ECV)
Should not be attempted if there are risks
Risks??
Prerequisites??
Drawbacks of ECV
Management of breech presentation
Antepartum management.
Delivery management.
Vaginal breech delivery.

12
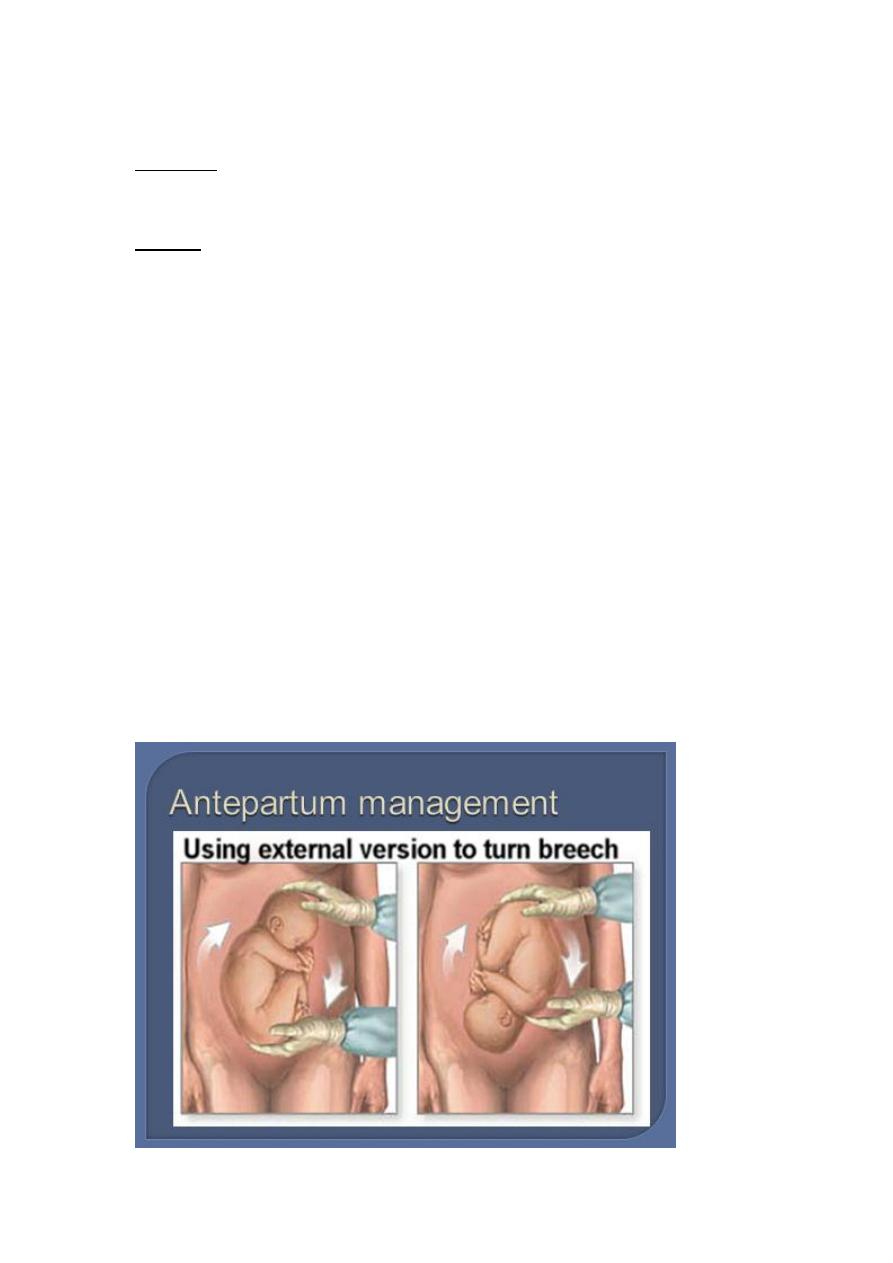
ECV
Is a procedure to turn the breech fetus to a vertex presentation through
external uterine manipulation ,in hospital ,under US guidance.
ECV may be considered at breech presentation at term before the onset
of labour.
Vertion is not carried before 36-37 weeks(tendency for spontaneous
reversion)
Carried in hospital equipped for emergency CS because of the risk of
placental abruption ,or cord compression(fasting patient with I,v line)
Contraindication:
Evidence of uteroplacental insufficiency.
Placenta previa.
Non reassuring fetal monitoring.
Hypertension.
IUGR or oligohyraminos.
History of previous uterine surgery.
Immediate success rate is 35%-76%.
Reversion to breech at term after ECV is2%.
ECV decrease the rate of CS ,but perinatal mortality is not affected.
Mode of delivery:
Assisted Vaginal Breech delivery
Elective Caesarean Section (CS)
Emergency CS
13
Crieteria for VD or CS
VD
Frank
GA>34w
FW=2500-3500gr
Adequate pelvis
Flexed head
If Nonviable fetus
No indication CS
Good progress labor
Willing of the patient
Experienced staff
CS
FW<2500or> 3500gr
Footling
Small pelvis
Deflexed head
Arrest of labor
GA24-34w
Elderly PG
Infertility or poor history
Fetal distress
PIH,PE
APH
Previous CS
Pelvic tumor.

14
Three types of vaginal breech deliveries:
Spontaneous breech delivery
Assisted breech delivery
Total breech extraction
Assisted vaginal breech delivry
As breech delivery can occur in any place when immediate CS is not
available ,practice of deliver skill is important to every practice in OB.
Ensure full dilatation of cervix
Thick meconium passage is common as the breech is squeezed through
the birth canal. This usually is not associated with meconium aspiration
because the meconium passes out of the vagina and does not mix with
the amniotic fluid.
Ritgen maneuver is applied to take pressure off the perineum during
vaginal delivery.
Episiotomies often are cut for assisted vaginal breech deliveries, even in
multiparous women, to prevent soft-tissue dystocia.
No downward or outward traction
is applied to the fetus until the umbilicus has been reached.
With a towel wrapped around the fetal hips, gentle downward and
outward traction is applied in conjunction with maternal expulsive
efforts until the scapula is reached. An assistant should be applying
gentle fundal pressure to keep the fetal head flexed.
After the scapula is reached, the fetus should be rotated 90° in order to
delivery the anterior arm.
The anterior arm is followed to the elbow, and the arm is swept out of
the vagina.
15
The fetus is rotated 180°, and the contralateral arm is delivered in a
similar manner as the first. The infant is then rotated 90° to the back-up
position in preparation for delivery of the head.
The fetal head is maintained in a flexed position by using the Mauriceau-
Smellie-Veit maneuver, which is performed by placing the index and
middle fingers over the maxillary prominence on either side of the nose.
The fetal body is supported in a neutral position with care to not
overextend the neck.
Piper forceps application: Pipers are specialized forceps used only for
the aftercoming head of a breech presentation. They are used to keep
the head flexed during extraction of the fetal head. An assistant is
needed to hold the infant while the operator gets on one knee to apply
the forceps from below.
Assisted vaginal breech delivery: Low 1-minute Apgar scores are not
uncommon after a vaginal breech delivery. A pediatrician should be
present for the delivery in the event that neonatal resuscitation is
needed.
Risk of breech vaginal delivery
Lower Apgar scors
An entrapped head
Nuchal arms
Cervical spine injury
Cord prolapse

16
Face presentation
1:300
Full extension of the head
Presenting part: Face
Denominator: Omentum/Chin
Diameter; Subomento bregmatic 9.5cm
Presentation, Mento anterior– Vaginal delivery
Mento posterior- Ceasaeran
Causes:
Anenecephaly
Prematurity
Multifetal pregnancy
Polyhydramnious
Neck tumours
Sternomastoid spasm
Multiparty
Diagnosis:
Abdominal
Vaginal
Brow presentation
1:800, 1:2000 deliveries
The area between the orbital ridge and the anterior fontenalle
Most unfavourable of all presentation
Transient presentation;
Full flexion—Occiput
Full extension---Face ,Diagnosis is during labour.
17
4th stage
نسائية
Lec-3
.د
اسماء
16/11/2015
Transverse lie and oblique lie
cord presentation and
prolapse
Transverse lie and oblique lie:
The baby lie with it’s long axis transverse or oblique in the uterus.

18
Position :
The fetus may lie in either iliac fossa ,
with the back sloping obliquely across
the pelvic brim, the breech occupies higher level in the opposite
direction of the abdomen.
Two positions are described:
Dorsoanterior
Dorsoposterior
Aetiology:
Multiparity.
Prematurity.
Polyhydramnios.
Multiple pregnancy.
Contracted pelvis,placenta previa ,fibroid.
Uterine malformation.
Diagnosis:
Abdominal examination:
Uterus appears asymmetrical ,broader and lessthan expected for
gestational age.
palpation reveals hard head at one iliac
fossa and softer breech one the other
side. no presenting part is felt over the
brim with the back is felt anteriorely in
dorsoanterior and fetal parts in dorso-
posterior.

19
Vaginal examination:
In early labour the presenting part is high can’t be reached ,membranes
may rupture early.
When the cervix become dilated an arm or a loop of cord may prolapse.
Diagnosis of shoulder presentation
depends on recognition of acromion
process ,scapula and adjacent ribs.
Cource of labour:
There is no true mechanism of labour
Untreated case will ends in obstructed
labour ,rupture of uterus and fetal death.
Delivery not occurs until the fetus is macerated or premature. (doubled
up)
Treatment :
Caesarean section should be performed in persistant transverse lie
presentation.
Internal podalic version in delivery of second twin (transverse lie).
External cephalic version may be tried in selected cases before labour or
in early labour .
In advanced labour or in case of ruptured
membrane C.S. IS SAFER EVEN IN A CASE OF
FETAL DEATH.
Unstable lie
Is a term used when the fetal lie and presentation is repeatedly changed
after 36 weeks of pregnancy .
The lie being variable between longitudinal, transverse and oblique.
By 36 week the fetus usually adopt stable lie and presentation which will
be unchanged until the onset of labour.

21
Incidence is 0.1% -1% .
Risks of unstable lie :
PROM.
Cord presentation and cord prolapse.
Compound presentation.
Uterine rupture.
fetal distress and death.
Causes of unstable lie:
Multiparty.
Polyhydramnios.
Multiple pregnancy .
Fetal anomaly
Placenta previa .
Pelvic tumour as fibroid,ovarian cyst.
Uterine anomaly.
Contracted pelvis or fetal macrosomia.
Management :
Clinical assessment :
History.
Examination :
-abdominal examination to exclude polyhydramnios .
Determine the lie and presentation.
-Pelvic examination : assess the capacity of the Pelvis,
tumour in the pelvis (after excluding placenta
21
previa).
Investigation :
-US : for diagnosis of the lie and presentation and
exclusion of the underlying cause.
-X ray :no place if US is available.
Management options for delivery :
No intervention : the lie will become
longitudinal in >80% of cases before the
onset of labour. (as out patient or
admitted in the hospital till spont.version)
Active:
External cephalic version,then induction
of labour and low amniotomy.
To induce controlled release of liquor use the
Drew-smythe catheter with it’s stylet inside to
puncture the amniotic membrane and allows
controlled release of liquor.
Elective C.S. at 38- 39 weeks gestation
with version to longitudinal lie during laprotomy
if there is contraindication to external cephalic
version or fails or contraindication to vaginal
delivery
.

22
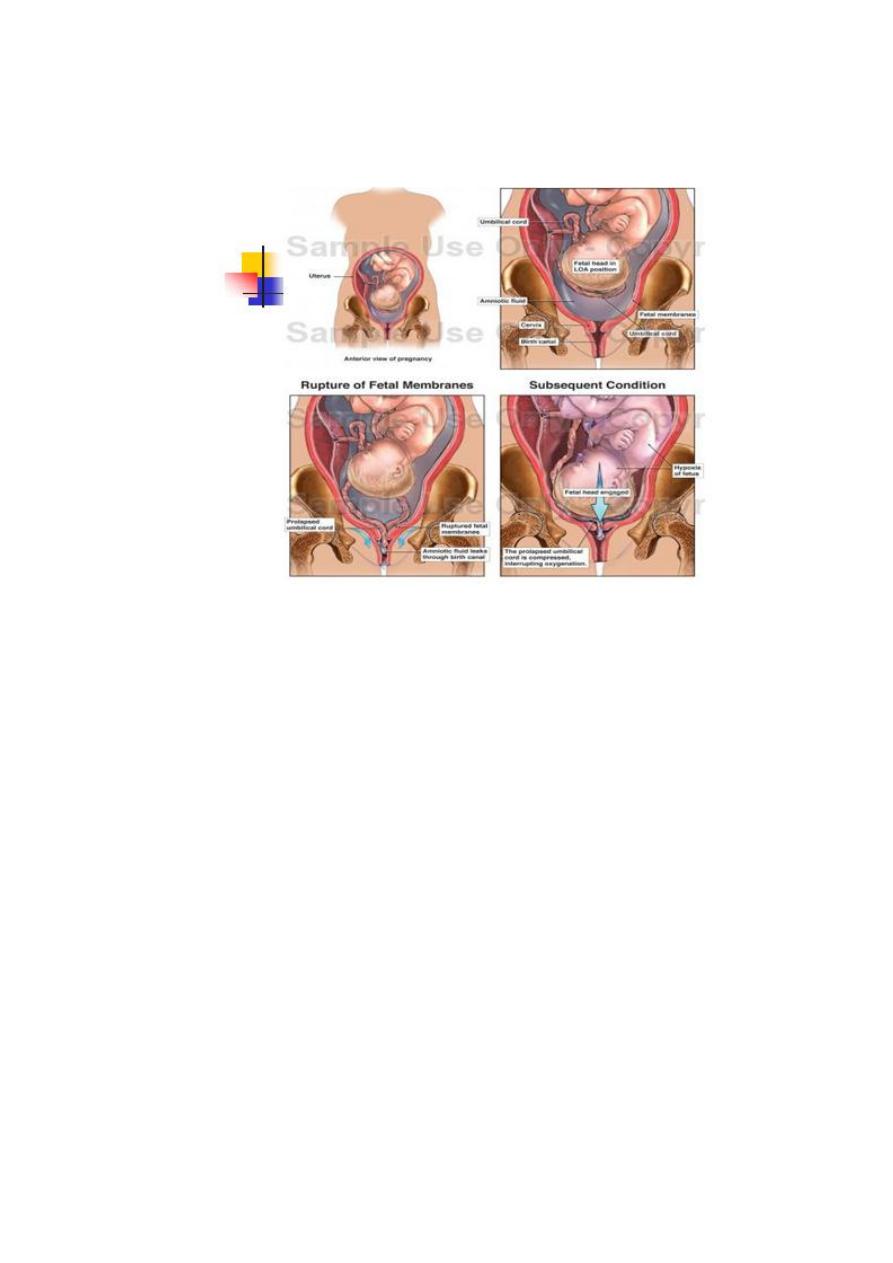
Cord presentation :
Cord prolapse :
Cord presentation : is when the cord
presented in the birth canal over the cervix with intact membrane .
Cord prolapse :when the cord prolapsed out of cervix after the sac is
ruptured.
Incidence once in 200-300 deliveries.
Aetiology:
Presenting part does not fill the lower segment.
Prematurity.
Multiparty.
Operative maneuvers. (amniotomy)
Abnormality of the cord. (long, low placental
insertion)
Fetal hypotension .(cord is not turgid as in
abruptio placentae)
Diagnosis:
Coils of cord may be felt in the fore waters.
If pulsating present distinction is easy .
Cord compression is possible if the liquor is
scanty especially if the head presents.
When the membrane have ruptured the cord prolapse into the vagina
and may protrude out of the vulva.
Absence of the pulsation in the umbilical cord
is unreliable as evidence of fetal death .
23
Anticipation:
All patients should come to the hospital early in labour (in 25% of cases
occurs before admission).
Comes once they notice a leaking liquor even if no contraction.
Those women at risk (hydramnio ,unstable or oblique lie, malposition ,
malpresentation ,CPD ,) should be admitted electively in late pregnancy.
Every patient for amniotomy is a potential
candidate for C.S., look for the level of the
presenting part before surgical induction, if
high then stimulate contraction before
amniotomy and exclude cord prolapse by
pelvic examination .
24
Fetal heart external monitoring may suggest
cord complication even before rupture of the
membranes.
MANAGEMENT :
Fetus a live and sufficiently mature the ideal is immediate delivery by
C.S.
While waiting for C.S. postural treatment involves :
The cord should be replaced within the warm,
moist vagina ,so preventing vasospasm.
Placing fingers in the vagina lifting the
presenting part.
Placing patient in trendelenberg’s position
or Knee elbow position .
Full the bladder with 500-700 ml of saline ,used when the patient
transported for some distance .
Rare exception:
When the cervix is fully dilated.
Multipara.
Longitudinal lie.
Normal fetal heart
Choose between C.S. or rapid delivery by
vacuum or forceps .
Virtually in all cases of cord prolapse C.S. to be
preferred treatment .
In cases of fetal death (absent fetal heart) cord prolapse can be
ignored .

25
Prognosis
Prompt diagnosis at amniotomy and a short
diagnosis to delivery interval result into low fetal
mortality .
Mortality is 5.5% if delivery was effected with in
10 minutes.
C.S. is preferred Because of lower perinatal
mortality even in cases approaching full
dilatation cervix.
26
4th stage
نسائية
Lec-4
.د
اسماء
16/11/2015
Antepartum Haemorrhage
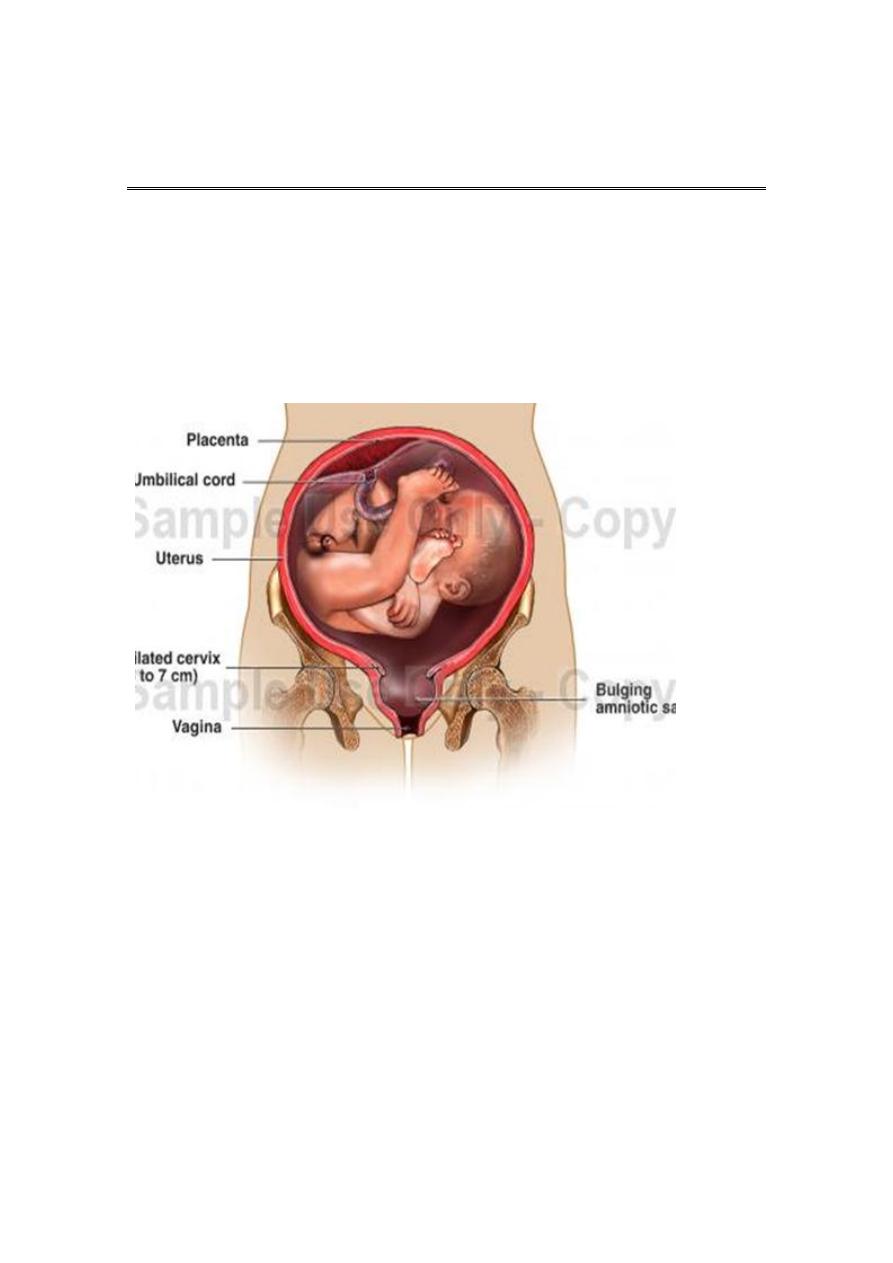
Antepartum haemorrhage: is bleeding from the the placental site from
24 week gesation and before delivery of the fetus.
Bloody show ( Slight vaginal bleeding ) is common during active labor
due to effacement and dilatation of the cervix, with tearing of small
veins.
Causes of antepartum haemorrhage:
Common:
Placenta previa..
Abruptio placentae
Uncommon:
Uterine rupture
Fetal (chorionic) vessels rupture.
Cervical or vaginal laceration.
Cervical or vaginal lesions.
Congenital bleeding disorders.
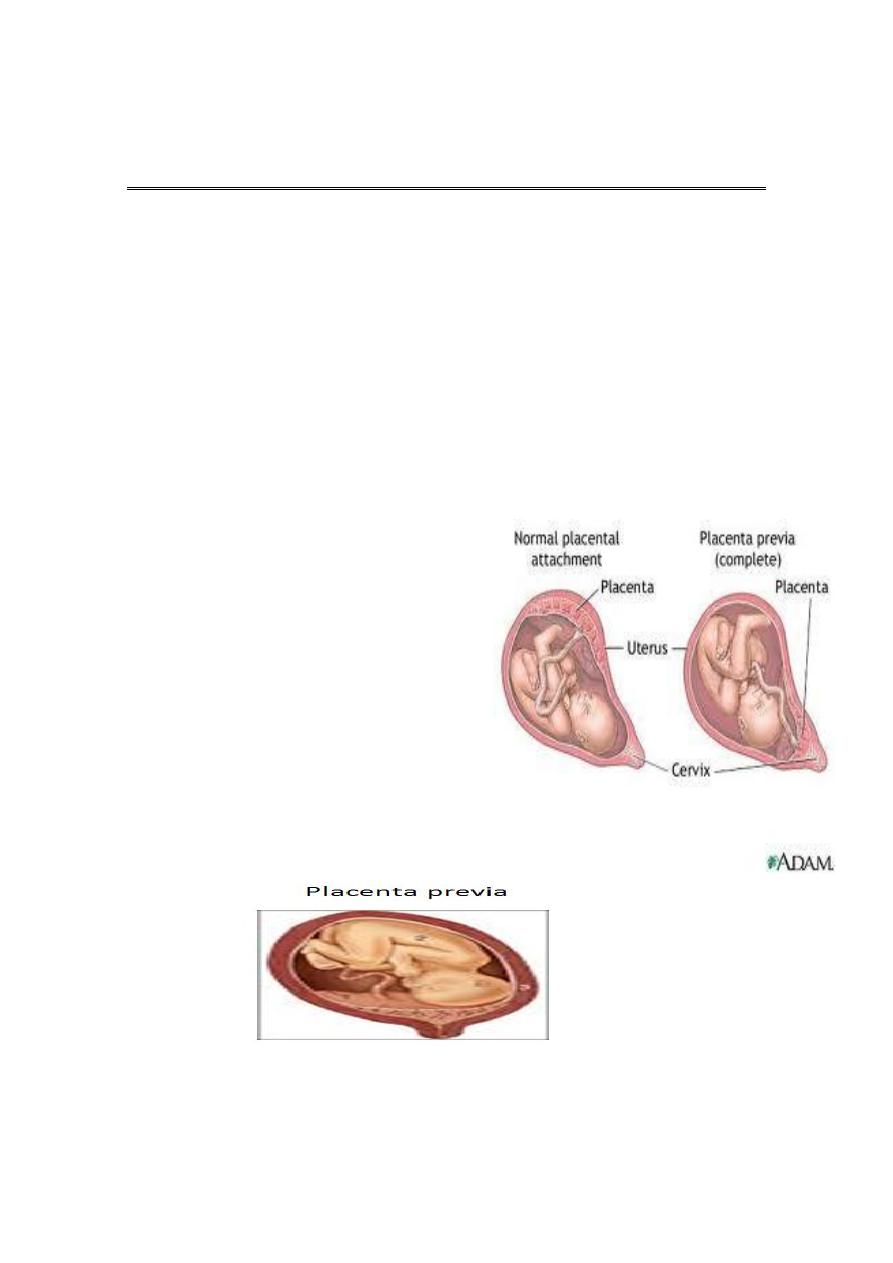
Placenta previa
27
Placenta previa:
Incidence of placenta previa is 0.5% in all pregnancies.
Bleeding from a placenta previa account for about 20% of cases of
antepartum haemorrhage.
:
Presentation
70% present with painless vaginal bleeding in the third trimester.
20 % have uterine contraction.
10% diagnosed incidentally by US.
Predisposing risk factors
Factors associated with higher incidence of
placenta previa:
Multiparity.
Increasing maternal age.
Prior placenta previa have 4-8% risk of placenta previa in subsequent
pregnancy.
Multiple gestation
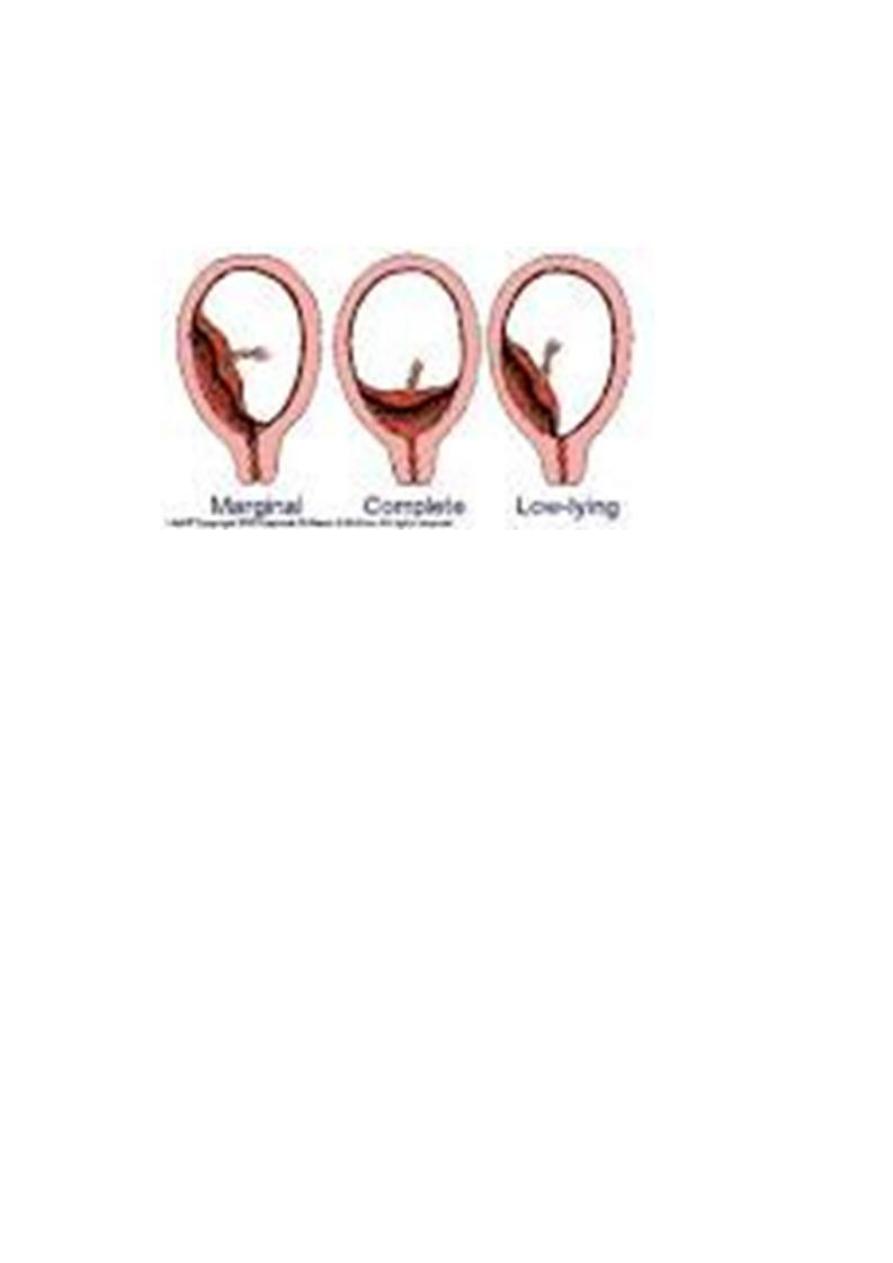
Classification of placenta previa:
Placentra previa is classified according to the relation ship of the
placenta to the internal os into:
Grade I :Marginal placenta previa : the edge of the placenta Is at the
margin of the internal os.
Grade II : the placenta is covering the cervix when it’s closed
Grade III :Major degree :Total placenta previa: internal os is covered
completely by the placenta
Grade IV :Major degree :central placenta previa
Partial placenta previa: internal os is partially covered by the placenta.
Low lying placenta: the placenta is attached to the
lower uterine segment 2 cm from the internal os.
28
Clinical presentation:
The most common characteristics :
Painless vaginal haemorrhage after second trimester or because for
abortion . Bleeding may occur without warning and without pain in a
women who have uneventful prenatal coarse , fortunately the initial
bleeding is rarely so profuse to be fatal , stop spontaneously to recur .In
patient with placenta near the cervix bleeding may not occur until the
onset of labor.
29
The mean gestational age at the onset of labor is 30 weeks.
1/3 present before 30 weeks.
P.p. Most exclusively now diagnosed today by ultrasonography ,4-6% of
patients have some features of placenta previa on US before 20 weeks
,90% are resolved to normal placentation by the third trimester . in case
of complete placenta previa 10% resolved by the third trimester.
Examination finding in placenta previa
During examination the abdomen is soft not tender uterine contraction
may be positive.
Uterus may be larger than date .
there may be malpresentation as breech or transverse lie or non
engaged cephalic presentation .
Fetal heart is positive and usually not affected by the initial blood loss.
Clinical diagnosis can be firmly established by finger examination feeling
the placenta near the internal os which should never be permissible
unless the women is in the operating theater with all preparation for
immediate C.S. and unless delivery is planned and when no facility for
immediate US is not available.
Placental localization by US is the simplest ,precise and safest method
for localization of the placenta .
Trasnabdominal sonography has an accuracy of 95% for placenta previa
detection
false positive result may be due to bladder distention so the scan should
be repeated after emptying of the bladder.

31
False negative in case of the placenta is implanted posteriorly and the
fetal vertex is low and the placenta is low and obscured and the
diagnosis is missed
Transvaginal sonography is accurately diagnose all case of placenta
previa but there is risk of bleeding.
Preterm patient with placenta previa:
No vaginal bleeding require close observation with blood is prepared
and facility for immediate transport to hospital if bleeding occurs.
In properly selected patient there is no difference
between inpatient and outpatient treatment.
If mild to moderate vaginal bleeding conservative
management inform of correction of anemia ,
corticosteroid therapy
If sever and persistent vaginal bleeding and any bleeding after 36 week
emergency delivery is indicated .
Patient with no vaginal bleeding should be delivered at term (38 week).
Mode of delivery
Practically Caesarean section is indicated in all cases of placenta previa
Patient with placenta previa are liable for intraoperative and post
partum haemorrhage because of :
Placental bed at lower segment with poor uterine contraction.
Wide bed of placenta because of less blood supply.
Risk of placenta accreta (anterior placenta previa overlying previous
uterine scar).
DIC.
Measures to control intraoperative bleeding in placenta previa cases:

31
Oxytocic drugs/hot packs/uterine packing.
Oversewing placental bed in placenta accreta.
Ligation of vessels(uterine and internal iliac )
Hysterectomy indicated as life saving and in patients completed their
family.
Abruptio Placentae
Bleeding from a normally situated placenta due to it’s premature
separation ,it could be partial or complete,
Abruptio placentae denotes a sudden accident (clinical characteristics of
this condition) so
referred to as accidental haemorrhage.
Types of abruptio placentae
-Revealed haemorrhage (external )When the blood from the placenta
insinuate itself between the membrane and the uterus then escape
through the cervix.
-concealed haemorrhage (internal) : less often when the blood doesn’t
escapes externally but retained inside in between the detached placenta
and uterus ,this type carries greater hazards because the amount of
bleeding is not properly appreciated and because the possibility of
disseminated intravascular coagulation.
Bleeding in placental abruption is almost always maternal in origin, with
evidence of fetomaternal haemorrhage in 20% of cases.
Incidence :1/200 deliveries .
Risk factors:
.Increased age and parity.
..Preeclampsia.
…Chronic hypertention.
….Preterm rupture of membrane.

32
…..Cigarette smoking.
……Thrombocytopenia.
…….Cocaine use.
……..Prior abruption.
………External trauma.
……….Uterine leiomyoma.
Clinical diagnosis:
Clinical picture vary considerably there might be
Profuse bleeding with mild separation with no fetal
compromise or no external bleeding with complete
separation of placenta and fetal death.
Diagnosis of placental abruption is certain if the patient
presented with painful Vaginal bleeding associated with
uterine tenderness ,hyperactivity and increased tone .
Fetus is cephalic may be in distress or decreased fetal
movement or even fetal death.
Diagnosis of placental abruption is initially clinical US detect 2% of
abruption ,despite initial US examination is required to exclude cases
where placenta previa coexist with abruption.
Complication :
Shock : sometimes shock is out of proportion to the amount of blood
loss.
Fetal distress in 60% and fetal death in 15%
Consumptive coagulopathy .placental abrption is the most common
cause of DIC in occurs in about 20% of cases especially in cases where
abruption is massive or fetal death has occurred.
Renal failure.

33
Couvelaire uterus : extravasation of blood into the uterine musculature ,
diagnosed during laparotomy , rarly it cause sever post partum
haemorrhage by interfering with uterine contraction to indicate
hysterectomy.
Treatment : our aim is resuscitation with blood and crystalloids and
prompt delivery to the mother to control haemorrhage.
And the management will vary depending upon gestational age and the
status of the mother and the fetus.
If the baby is viable:
Expectant management in preterm labor with mild vaginal bleeding:
delaying delivery till term if the bleeding is mild and not in labor ,if sever
vaginal bleeding and in labor delivery is VD if no delay . if sever vaginal
bleeding and not in labor delivery is by C.S. because lack of omnious
deceleration does not guarantee the safety of intrauterine environment
for any period of time , any time placental separation can be caused by
uterine contraction with rapid fetal compromise.
Fetal compromise in placental abruption can be caused by : placental
separation.
maternal haemorrhage
fetal haemorrhage
uterine hypertonus
If the baby is dead: vaginal delivery is preferred unless the haemorrhage
is so brisk that cannot replaced by blood transfusion or there is other
obstetric indication for caesarean delivery . although in patient with DIC
there is risk of brisk bleeding from the uterine and abdominal wound
because of serious coagulation defect ( not placental site bleeding as it’
controlled by uterine contraction).
