1
Fourth stage
obstetrics
Lec 6
Dr. Wildan
3/11/2015
Ectopic pregnancy
extrauterine pregnancy
Objectives:
Students will be able to:
– Define ectopic pregnancy.
– List risk factors.
– List differntial diagnosis of abdominal pain and vaginal bleeding in early pregnancy.
– Evaluate case and confirm diagnosis and justify treatment option.
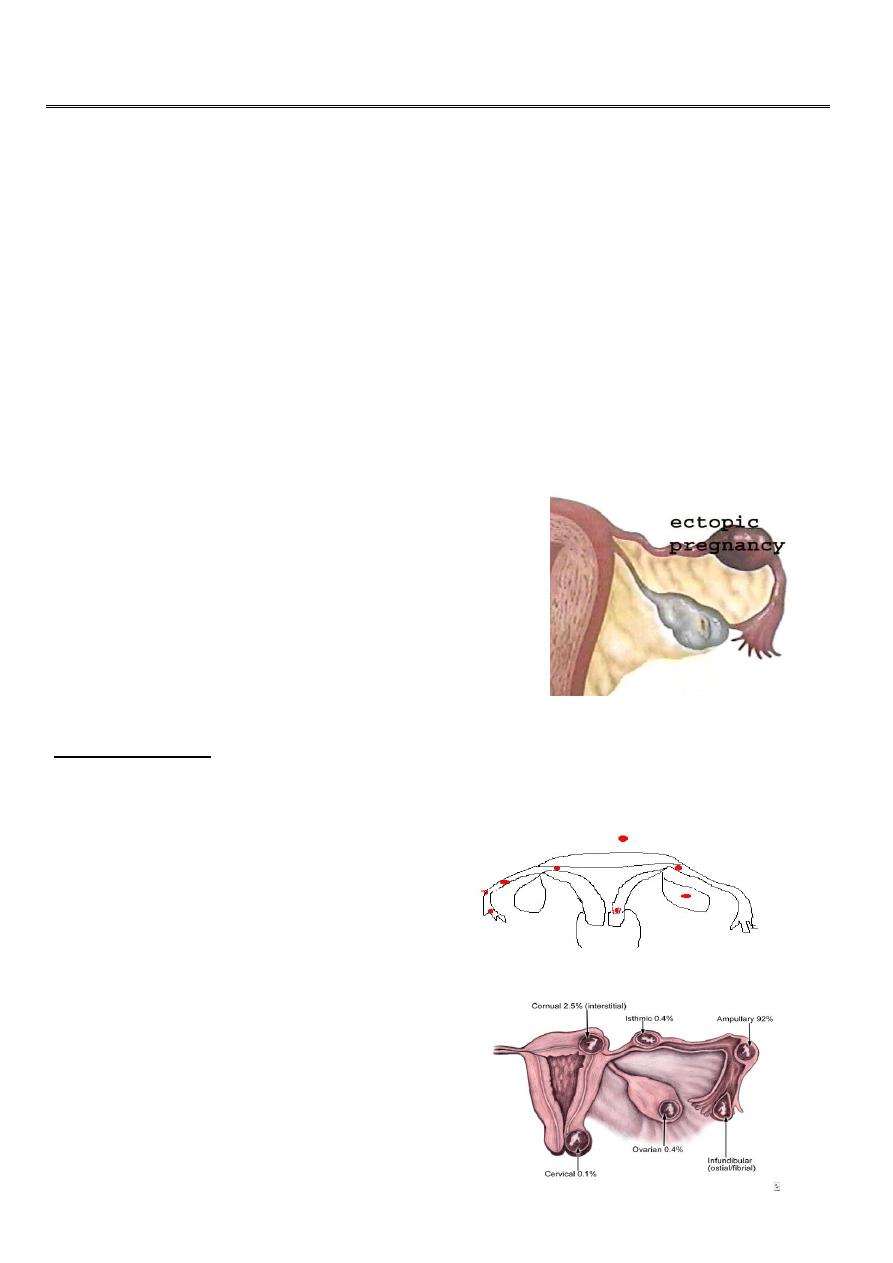
Ectopic pregnancy:
It is an implantation of fertilized ovum on any site
other than the endometrium of uterus.
Ectopic pregnancy remains an important cause of
maternal mortality worldwide.
Sites of ectopic:
Fallopian tube is the most common site ( 98%), the ampulla (80%) is the most common
site of implantation.
Uterus.
Ovary.
Cervix.
Broad ligaments.
Else where in peritoneal cavity.
2
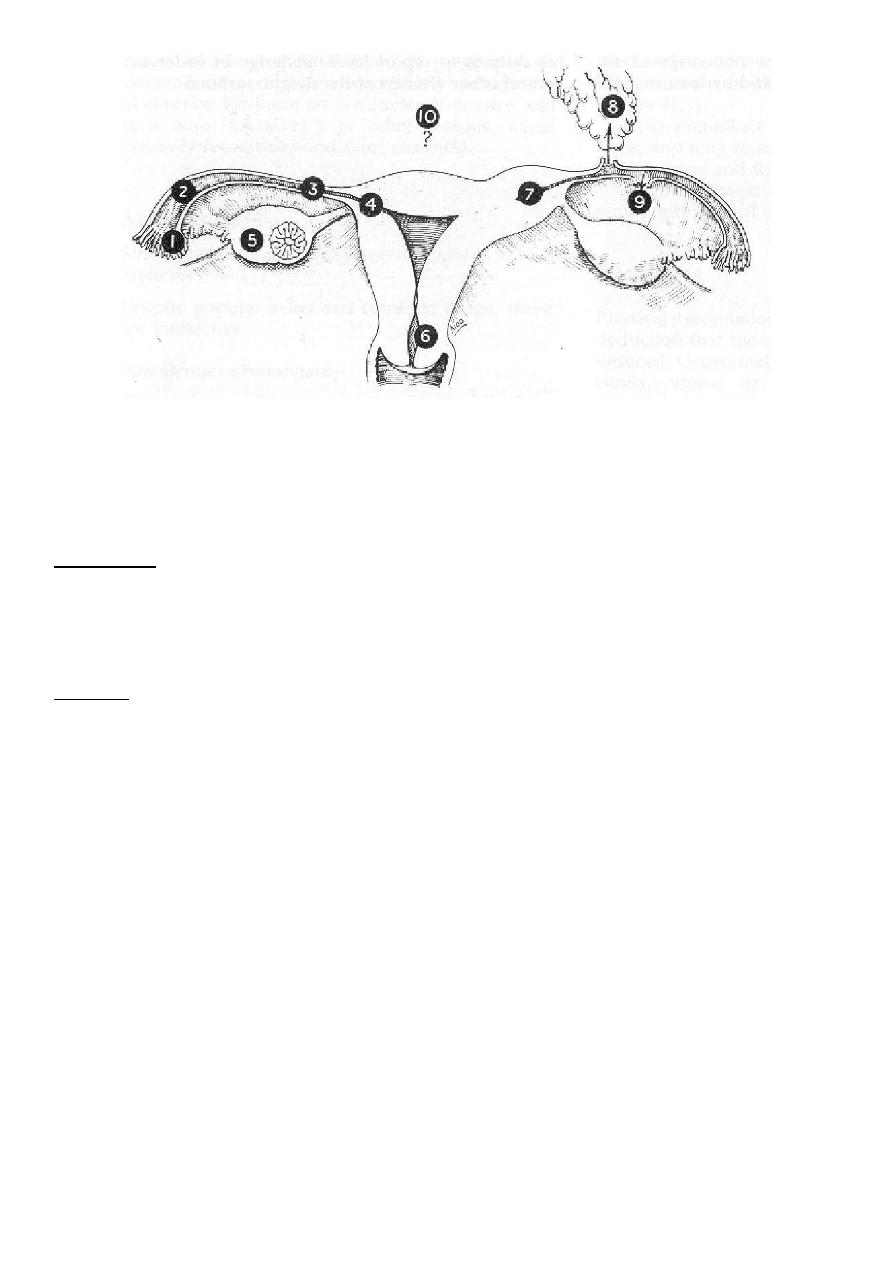
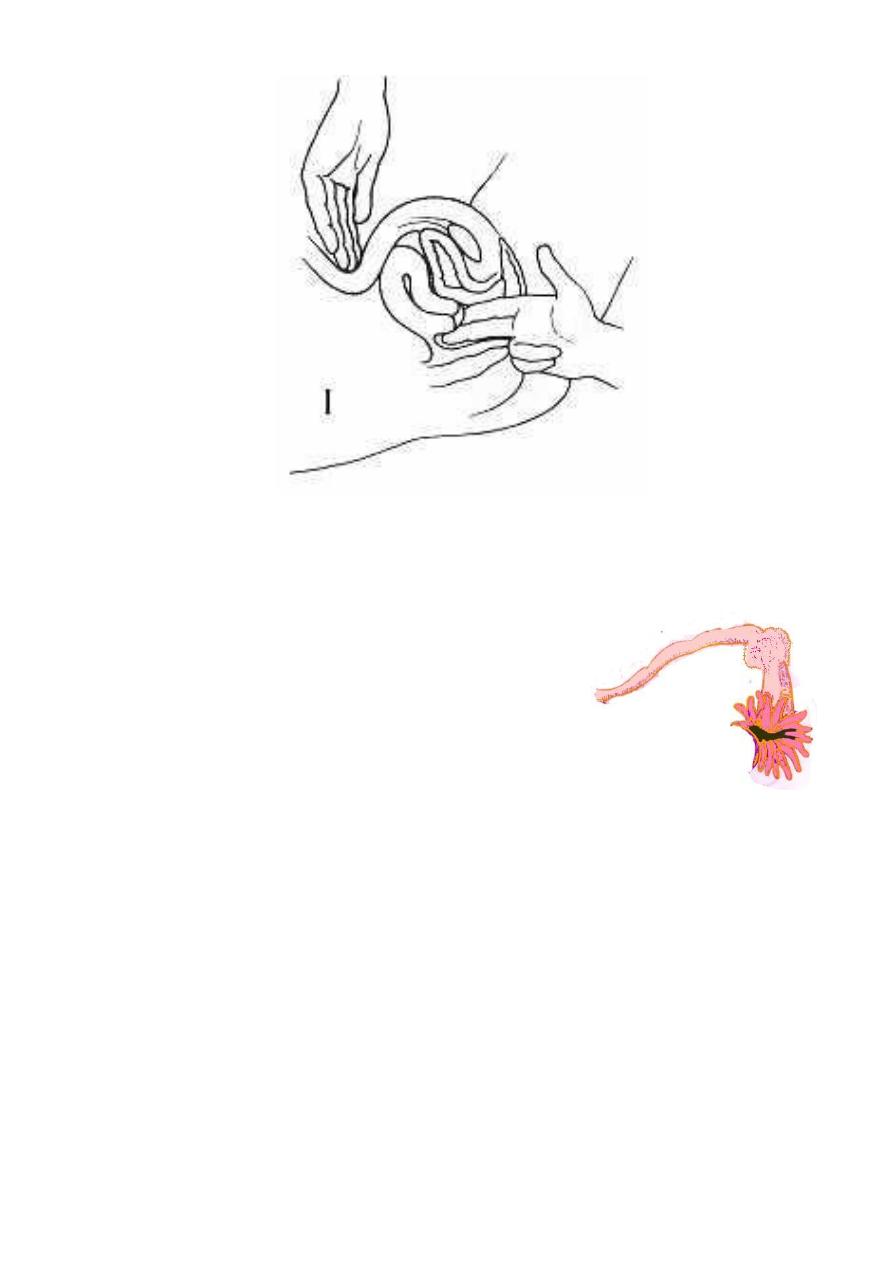
1)Fimbrial 2)Ampullary 3)Isthemic 4)Interstitial 5)Ovarian 6)Cervical
7)Cornual-Rudimentary horn 8)Secondary abdominal 9)Broad ligament
10)Primary abdominal
Incidence:
It's incidence directly related to the prevalence of salpingitis and it is about 1% of all
pregnancy
Causes:
Any mechanical or functional factors that prevent or interfere with passage of
fertilized ovum into uterine cavity and delay it and include the following:
Pelvic inflammatory disease(PID): (Chlamydia, gonococcal, tuberculous).
Tubal surgery: (tubal sterilization, reversal of tubal sterilization).
Congenital abnormalities of fallopian tube: (diverticula, accessory ostia, hypoplasia,
Diethyl stillbesterol (DES) exposure in utero).
Peritubal adhesion: secondary to infection or surgery (appendicectomy).
Gross pelvic pathology (endometrosis).
Uterine fibroid at utero-tubal junction.
Intra uterine device (IUD) in situ (in uterus), 3-4% of pregnancy if occur, is ectopic.
Progesterone only pills.
Assisted reproductive technique (ART) increase risk of hetrotopic pregnancy(as IVF).

3
Risk factors for ectopic pregnancy:
History of previous ectopic pregnancy.(the risk of recurrent ectopic pregnancy is 12–
18%. The future risk increases further with every successive occurrence).
Intrauterine device (IUD) or sterilization failure.
Pelvic inflammatory disease.
Chlamydia infection.
Early age of intercourse and multiple partners.
History of infertility.
Previous pelvic surgery.
Increased maternal age.(35 years and more risk to have ectopic).
Cigarette smoking.
Strenuous physical exercise.
In utero diethylstilbestrol (DES) exposure.
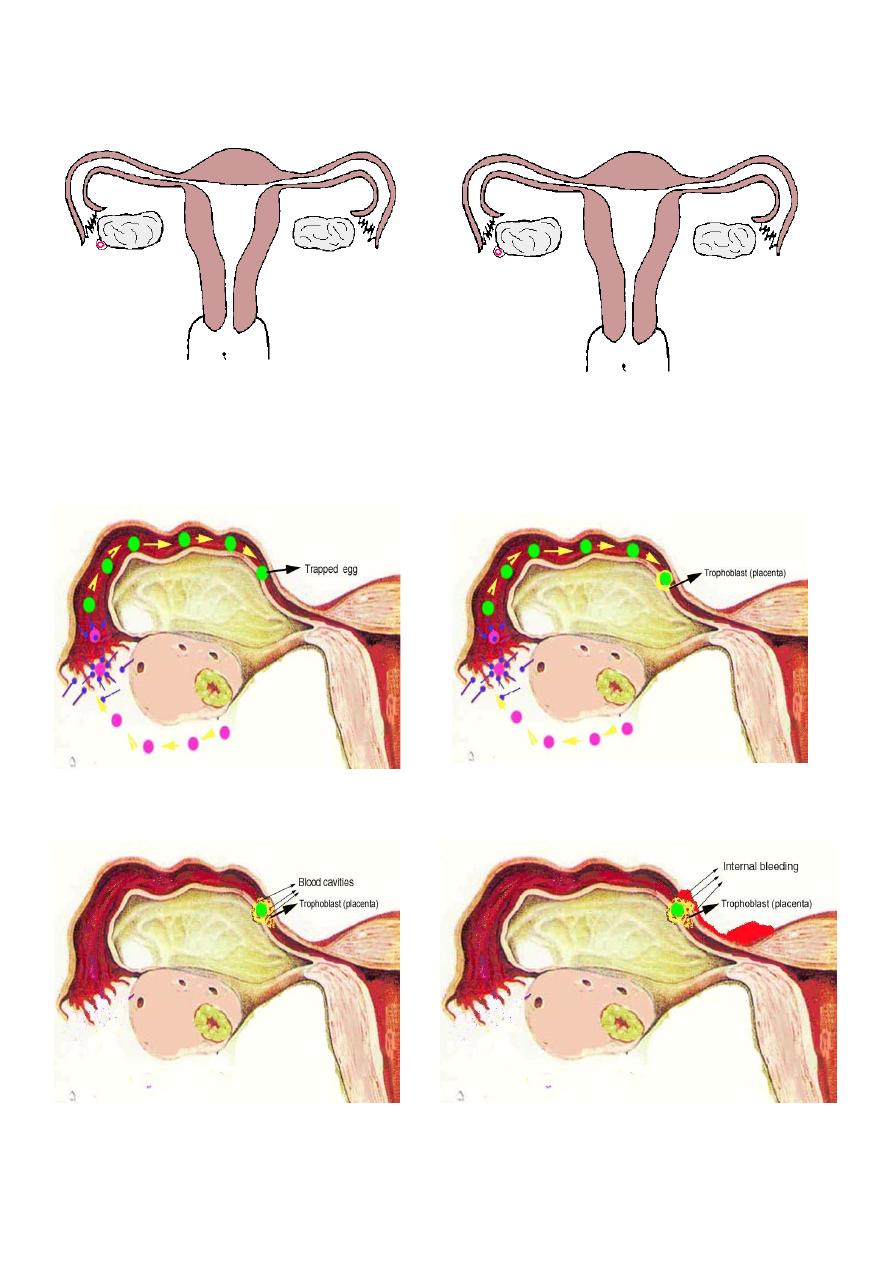
Pathological anatomy:
In normal intrauterine pregnancy:
The ovum is fertilized in the Fallopian tube and then it is transported into the uterus
where there is thick deciduas (between trophoblast and uterine muscle) in which
fertilized ovum can be embeded.
In ectopic pregnancy:
in tube, there is only a very thin layer of connective tissue separating the epithelium
from muscle so it is easy for the trophoblast to erode into muscle of tube (as there is
no decidual formation) and no resistance to invading trophoblast and some of vessels
which meet the trophoblast opened and haemorhage occur around embryo and
embryo die.
Uterus respond to hormonal changes and its enlarged and then endometrium
undergoes decidual changes.
Histologic Characteristics:
Chorionic villi, usually found in the lumen, are pathognomic findings of tubal pregnancy.
Gross or microscopic evidence of an embryo is seen in two thirds of cases.
4
In normal intrauterine pregnancy In ectopic pregnancy
5
The natural progression of tubal pregnancy (Course and outcome)
Tubal pregnancy may terminate in number of ways :
1. Tubal abortion: Part or all of the products of ectopic are expelled from the tube into
peritoneal cavity and collect in rectovaginal pouch.
2. Tubal rupture: Product of conception invade and expand the tube and cause rupture
of tube. If it occur in first few weeks, the pregnancy is situated in isthmic portion of
tube. Later rupture occur in interstial ectopic pregnancy.
3. Tubal mole: Dead embryo surrounded by clot retained in tube which may be
absorbed later on.
4. Secondary abdominal pregnancy (rare): Embryo is expelled from tube and acquires a
secondary attachment in peritoneal cavity and embryo continuo to grow.
Clinical presentation:
The clinical presentation of ectopic pregnancy is very variable.
It is largely determined by the location of pregnancy within the tube.
Asymptomatic:
Discovered when patient attend antenatal clinic for booking and especially for high risk
group.
It is rare for ectopic pregnancy in tube to advance beyond 8 weeks without occurrence of
symptoms. On the other hand one third of interstitial tubal ectopics develop in a similar
way to healthy intrauterine pregnancies with evidence of a live embryo on ultrasound
examination. These pregnancies tend to be clinically silent until sudden rupture occurs.
Symptomatic:
Acute presentation (due to rupture ectopic and abortion).
Subacute presentation (due to non rupture ectopic).
Symptoms of ectopic pregnancy:
There is no pathognomonic symptoms of ectopic pregnancy but the classic triad consist of:
1. Abdominal pain nearly always precedes the bleeding. There is no pathognomonic
pain that is diagnostic of ectopic pregnancy.
2. vaginal bleeding.
3. Amenorrhoea.

6
severe continuous acute sharp abdominal pain typically referred to shoulder due to
diaphragmatic irritation intraperitoneal haemmorrhage occur in rupture ectopic and
in tubal abortion.
Discomfort and dull aching lower abdominal pain mainly on affected side in rupture
ectopic.
Amenorrhoea: most commonly symptom arise after miss period.
Occasionally symptoms arise before miss period.
Sometimes 2-3 miss period in case of interstial ectopic or ectopic in rudemintary horn
of uterus.
Abnormal vaginal bleeding: the amount of bleeding varies
a.Usually bleeding is scanty and dark brown in colour.
b.in some women it can be quite heavy.
c. About 10–20% of ectopic pregnancies present without bleeding
Passage of a decidual cast may sometimes lead to an erroneous diagnosis of
miscarriage.
Examination:
Rupture ectopic pregnancy:
With rupture ectopic pregnancy and intrabdominal hemorrhage, the patient
develops tachycardia followed by hypotension (Shock state).
The abdomen is:
Distended to some degree.
Generalized tenderness and rigidity and rebound tenderness.
Bowel sounds are decreased or absent.
Pelvic examination:
Speculum examination has very little value in the detection of ectopic pregnancy. It
may help to diagnose miscarriage by the visualization of the products of conception
within the cervix or vagina.
Dark brown blood seen from cervix.
Soft cervix.
Cervical excitation (tenderness in movement of cervix) is positive although
cervical excitation is not a specific sign of an ectopic pregnancy.
Uterus slightly enlarged.
Tenderness in ectopic site.
Rarely palpable adnexal mass. Most ectopic pregnancies are very small and
they cannot be felt on palpation.
7
Unpurtured ectopic pregnancy:
Frequently, the findings before rupture and
hemorrhage are nonspecific, and vital signs are
normal.
The abdomen may be not tender or mildly tender,
with or without rebound.
Pelvic examination:
must be performed in an area where facilities for resuscitation are available as
examination may provoke rupture of tube.
Dark brown blood seen from cervix.
Soft cervix.
The uterus may be slightly enlarged, with findings similar to a normal
pregnancy.
Cervical exitation (cervical motion tenderness) may or may not be present.
An adnexal mass may be palpable in up to 50% of cases, but the mass varies
markedly in size, consistency, and tenderness. (remember the palpable mass
may be the corpus luteum and not the ectopic pregnancy).
8
Differential diagnosis:
Gynecological disorder:
1. abortion.
2. ruptured corpus luteum cyst.
3. acute pelvic inflammatory disease (PID).
4. adnexal torsion.
5. degenerating fibroid.
Non gynecological disorder:
1. acute appendicitis.
2. pyelonephritis.
3. pancreatitis.
Investigation:
History and physical examination may or may not provide useful diagnostic
information. The accuracy of the initial clinical evaluation is less than 50% . Additional
tests are frequently required to differentiate early viable intrauterine pregnancy or
suspected ectopic or abnormal intrauterine pregnancy.
Ectopic pregnancy must be suspected when pregnant patient present with abnormal
bleeding and pelvic pain or in patient at risk of ectopic to prevent ruptured ectopic
pregnancy which is life threatening to mother.
1. ultrasound examination
detection of normal intrauterine pregnancy exclude diagnosis of ectopic pregnancy
in most of cases.
The spectrum of sonographic findings in ectopic pregnancy includes the following:
Live embryo (fetal heart positive) in adnexa which is gold slandered to diagnose
ectopic. it confirms ectopic.
Enlarged and empty uterus &/or adnexal mass &/or fluid in pouch of Douglas.
Negative pelvic ultrasound (20-30%) does not exclude ectopic pregnancy.

9
So wait it and repeat ultrasound in 4 days time provided there are no clinical sign
of intraperitoneal bleeding.
Transvaginal scanning provides much clearer images of pelvic structures in
comparison to transabdominal scanning and Intrauterine pregnancy can be
diagnosed one week earlier with transvaginal than with transabdominal
ultrasonography
2. Serum human chorionic gonadotropin (hCG):
Serum B-hCG tests are positive in 100% of ectopic pregnancy.
Serial estimation of B-hCG concentration.
Serial serum hCG assay is particularly useful in the diagnosis of a symptomatic ectopic
pregnancy. It can distinguish between intrauterine and ectopic pregnancy as the level
of hCG doubles every 2 days in normal intrauterine pregnancy. Abnormally slow rise
in serum hCG and prolonged hCG doubling time is an indicator of an abnormal
pregnancy.
B-hCG with ultrasound scanning (Discriminatory zone):
With the use of transabdominal ultrasound, a normal pregnancy could be seen in
most cases when serum hCG exceeded 6500 IU/l .With the transvaginal ultrasound
this threshold can be lowered to 1000 IU/l.
3.
progesterone level :
progesterone level serial measurement may be helpful.
4.
Laparoscopy
It allow for direct visualization of tubes and ovaries and should be considered in
women with hCG above the discriminatory level and absence of intrauterine
gestational sac on ultrasound and if diagnosis is in doubt. Laparoscopy is the gold
standard for the diagnosis of ectopic pregnancy
10
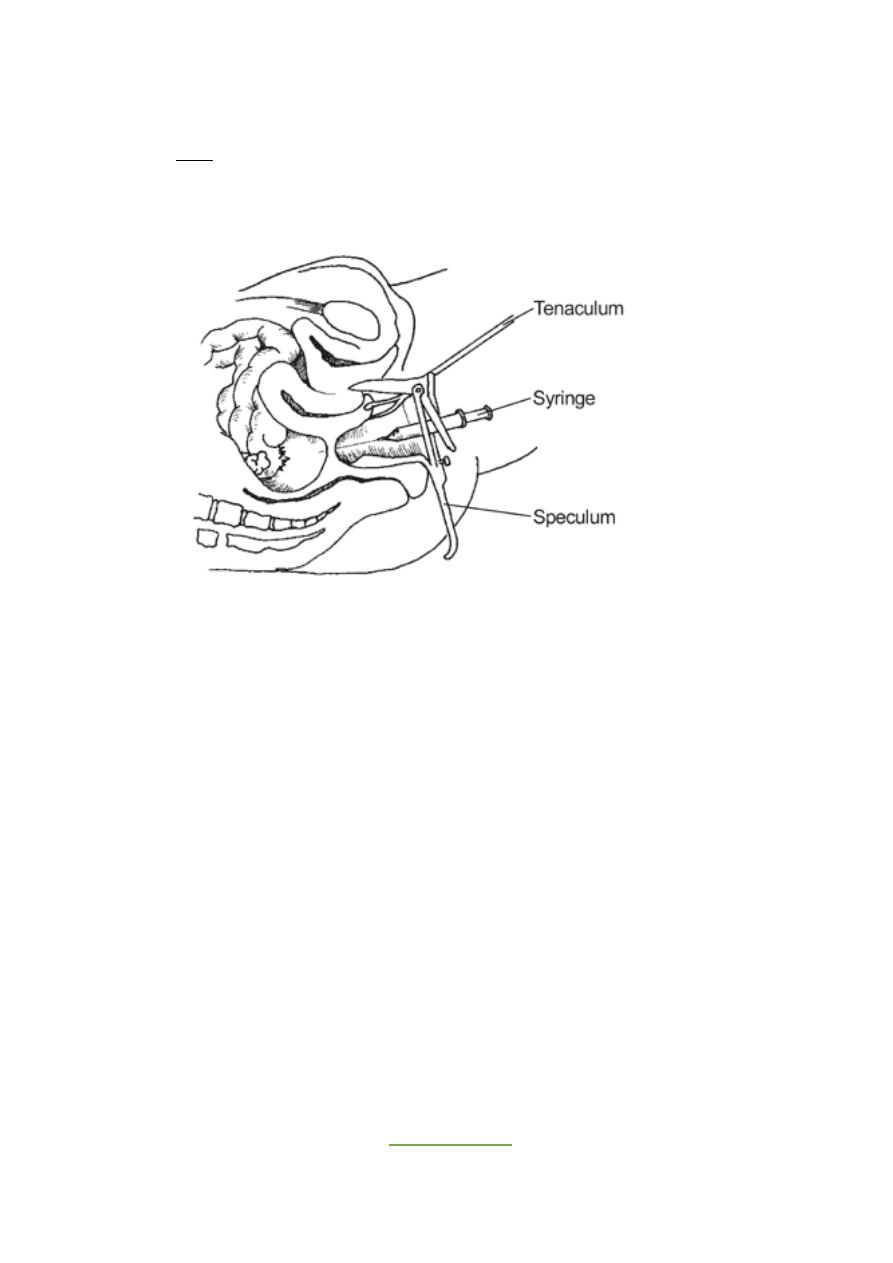
5.
Culdocentesis
• Used in past to diagnose rupture ectopic and not useful for diagnose of early ectopic
pregnancy. Not used nowadays as the results of culdocentesis do not always
correlate with the status of the pregnancy.
6.
uterine curttage :
not advised in routine investigation.
7. Surgery (laprotomy):
For women who present in shock, immediate surgery is both
diagnostic and therapeutic.
Done
“Pregnancy in the fallopian tube is a black cat on a dark night. It
may make its presence felt in subtle ways and leap at you or it may
slip past unobserved. Although it is difficult to distinguish from
cats of other colours in darkness, illumination clearly identifies
it.”
:D
