1
4th stage
Surgery
Lec.7
Dr.mohammed
1/11/2015
Urinary tract infection
Urinary tract infection :
Specific
•
tuberculosis
•
belhareziasis
Non specific
• pyelonephritis
• pyonephrosis
• renal abscess
• perirenal abscess
- UTI
:
is an inflammatory response of the urothelium to bacterial invasion.
:
- Bacteriuria the presence of bacteria in the urine.
:
.
- Pyuria the presence of white blood cells (WBCs) in the urine
•
Uncomplicated UTI :
infection in a healthy patient with a structurally and functionally normal urinary
tract.
•
:
Complicated UTI
infection is associated with factors that increase the chance of acquiring bacteria
and decrease the efficacy of therapy
2
:
Routes of Infection
1. Ascending route.
2.
Hematogenous route.
3.
Lymphatic route.
4.
Direct extension.
Urinary Pathogens :
E. coli is by far the most common cause of UTIs, accounting for 85% of community
acquired and 50% of hospital-acquired infections.
:
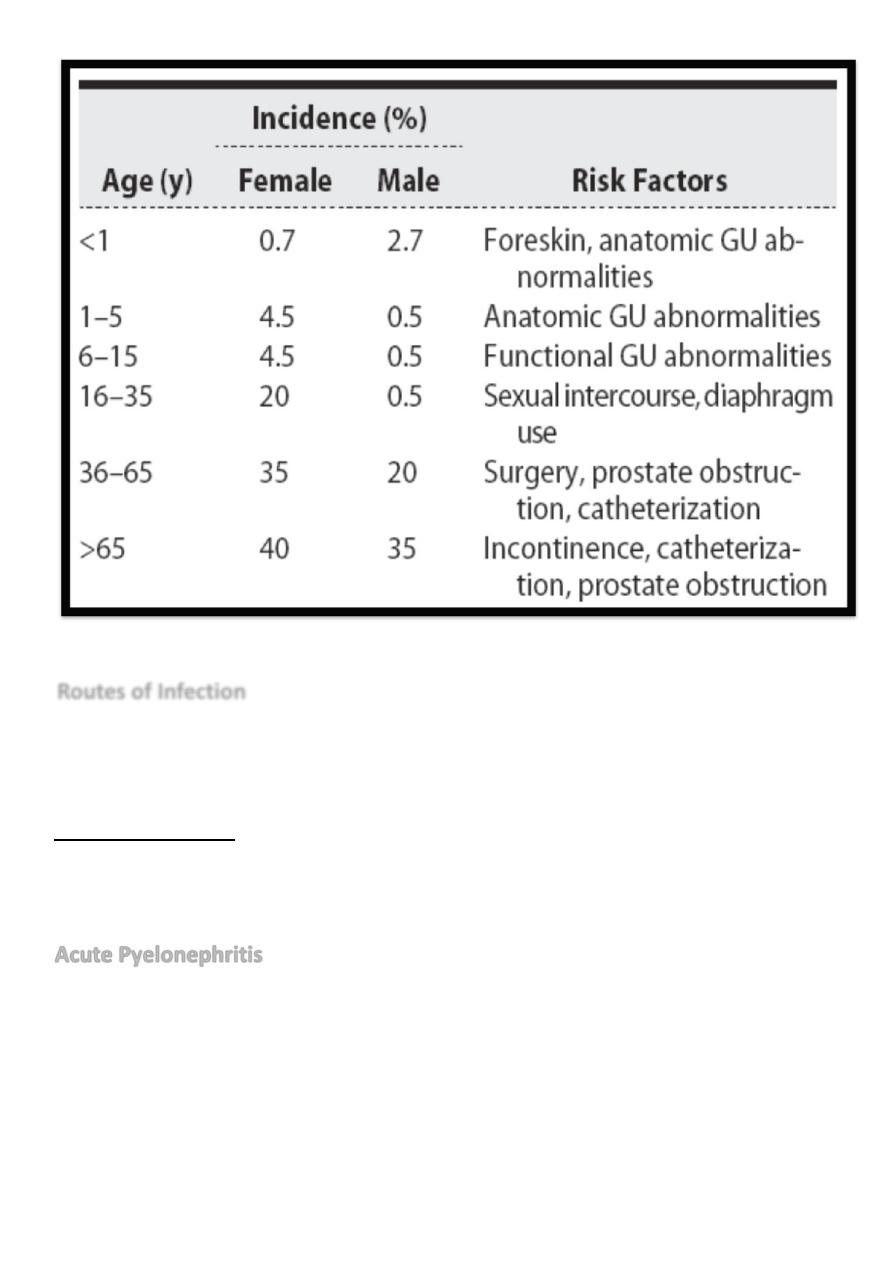
Acute Pyelonephritis
is defined as inflammation of the kidney and renal pelvis, and its diagnosis is usually
made clinically.
clinical picture :
- Patients present with loin pain ,chills, fever, and costovertebral angle pain,
tenderness.
- nausea and vomiting , Sepsis may occur.
3
Investigations :-
1. GUE WBCs and red blood cells,bacteria
:
.
2. blood analysis : Leukocytosis and increased ESR are commonly seen
.
3. Urine for culture and sensitivity .
4. Ultrasound : to detect any complicating factor like obstruction or stone .
5. CT and MRI
:
provide the best anatomic data on the site,cause, and extent of
infection.
:
MANAGEMENT
—
1. depends on the severity of the infection
2. In patients who have toxicity because of associated septicemia, obstruction or
azotemia ,hospitalization is warranted.
—
3. Empiric therapy with intravenous ampicillin and aminoglycosides , or 2
nd
generation cephalosporins is effective against a broad range of uropathogens
Parenteral
therapy should be maintained until the patient become a febrile
—
—
4. If bacteremia is present, parenteral therapy should be continued for an
additional 7–10
days and then the patient should be switched to oral treatment
for 10–14 days
—
5. In patients who are not severely ill, outpatient treatment with oral antibiotics
is appropriate. For adults, treatment with fluoroquinolones or TMP-SMX is well
tolerated and effective. Therapy should continue for 10–14 days.
4
:
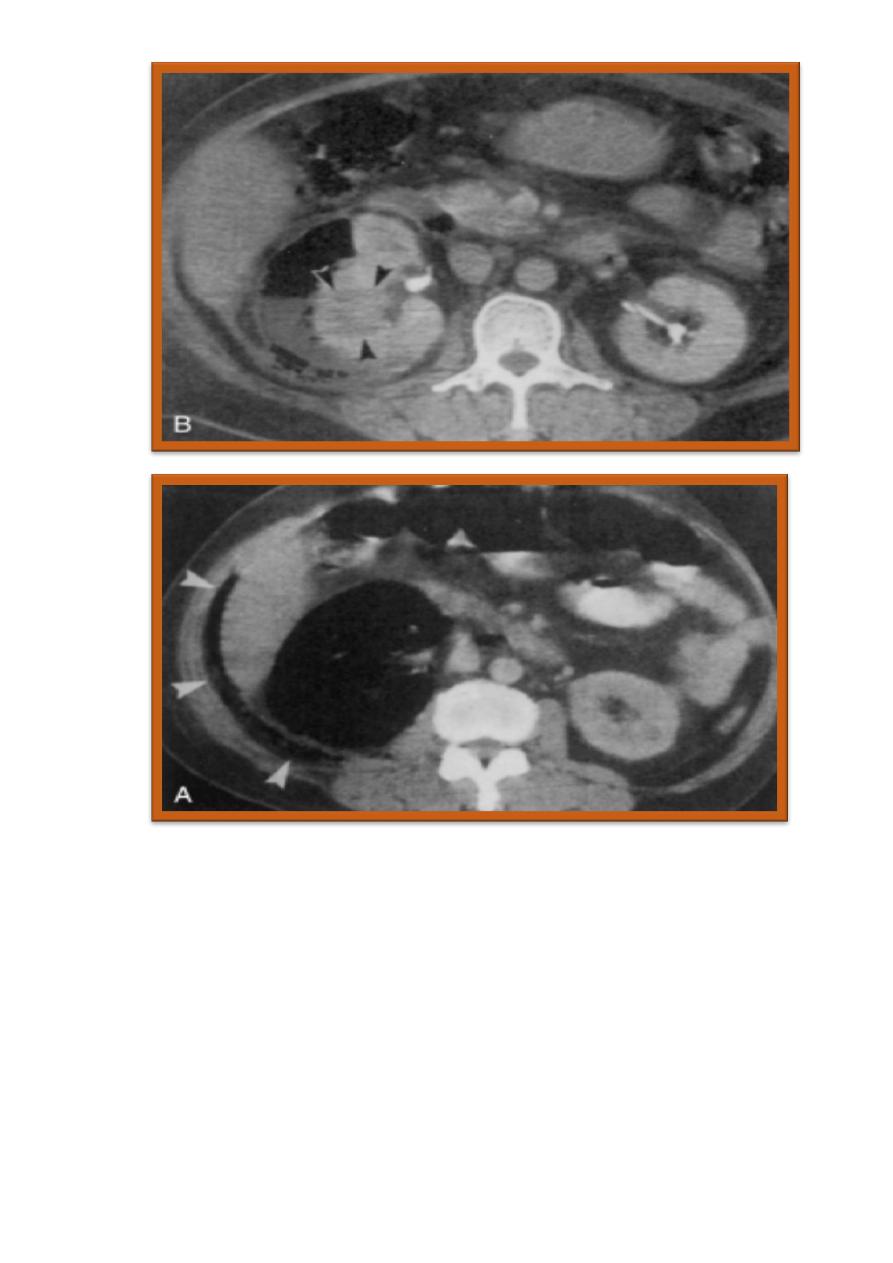
Emphysematous pyelonephritis
is an acute necrotizing parenchymal and perirenal infection caused by gas-forming
uropathogens.
About 80–90% of patients have diabetes; the rest of the cases are associated with
urinary tract obstruction.
Almost all patients display the classic triad of fever, vomiting, and flank pain.
Pneumaturia is absent unless the infection involves the collecting system.
E. coli is most commonly identified. Klebsiella and Proteus are less common.
The overall mortality rate between 20- 43%.
Emphysematous pyelonephritis is a surgical emergency. Most patients are septic,
fluid resuscitation and broad-spectrum antimicrobial therapy are essential
If the kidney is functioning, medical therapy can be considered.
Nephrectomy is recommended for nonfunctioning kidney and for patients who
do not improve after a few days of therapy
.
Xanthogranulomatous Pyelonephritis :
is a rare, severe, chronic renal infection typically resulting in diffuse renal
destruction.
Most cases are unilateral and result in a nonfunctioning, enlarged kidney
usually associated with obstructive uropathy secondary to nephrolithiasis
5
