1
fourth stage
Surgery
Lec-1
Dr.Samer ALsaffar
18/10/2015
The gall bladder and Bile duct
The Gall bladder ( Surgical anatomy and physilogy):
The gall bladder is:
Pear shaped, 7.5 – 12 cm long
30 to 50 mL capacity
Fundus, body, neck, and infundibulum
The cystic duct:
3cm in length
1-3 mm in diameter
Valves of Heister
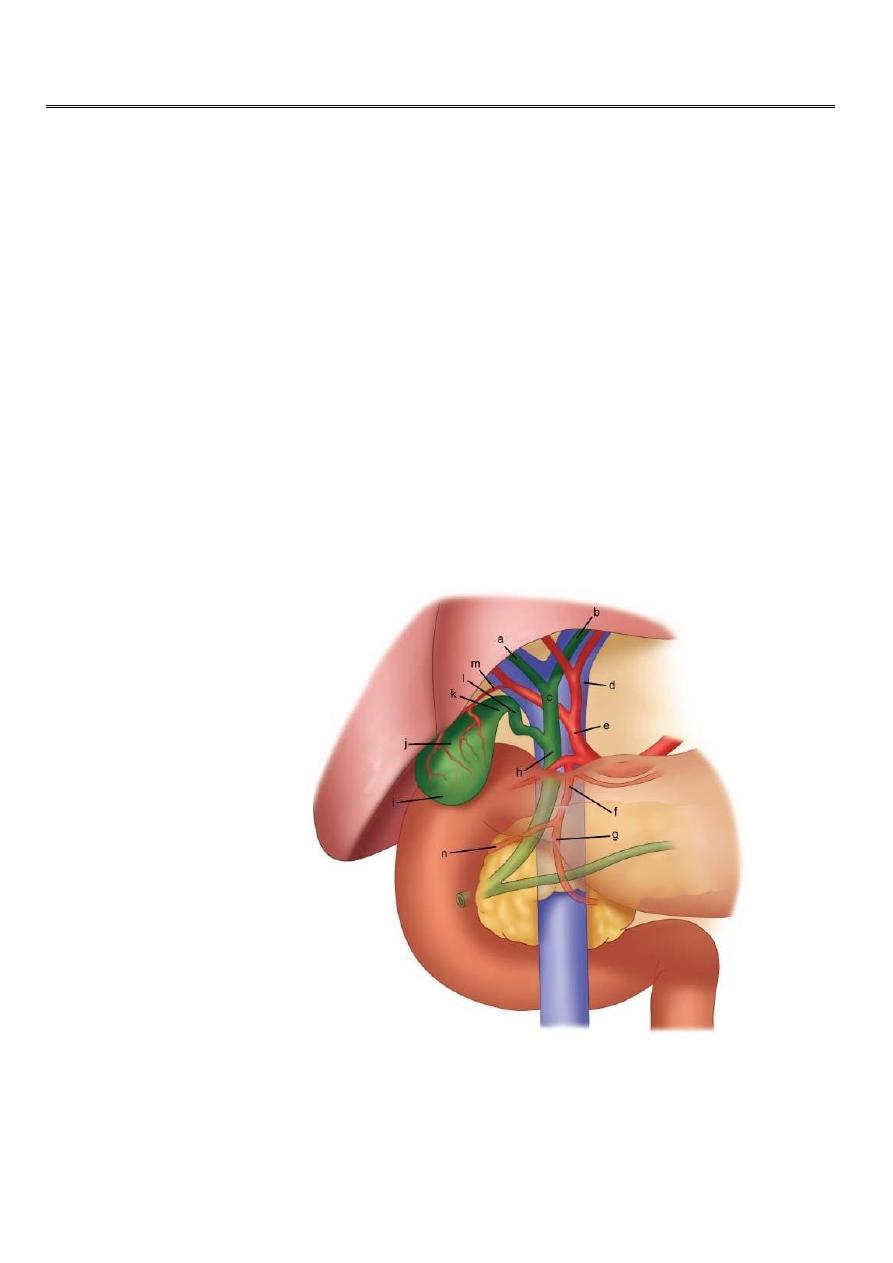
a RHD
b LHD
c CHD
d PV
e HAP
f GDA
h CBD
l CD
k Neck GB
j Body
i fundus
m CA
2
The common hepatic duct:
2.5 cm in length
Union of R & L hepatic ducts
The common bile duct:
7.5cm in length
Union of cystic and CHD
4 parts
Blood supply of gall bladder:
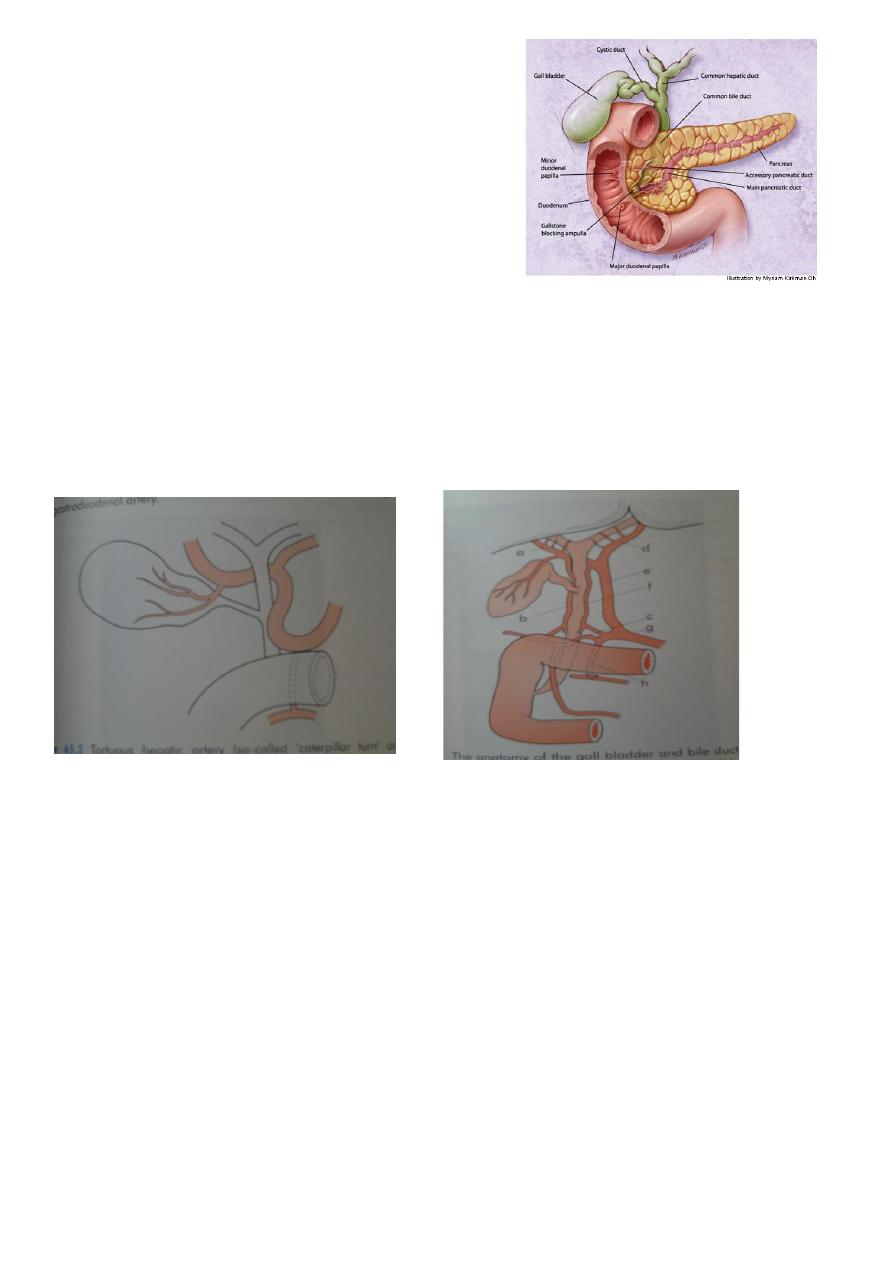
The cystic artery a branch of R hepatic artery
Accessory CA from GD art.
In 15% RHA anterior to CHD
Toutuous RHA and short CA, Caterpillar turn or Moynihan’s hump.
Lymphatics:
Subserosal and submucus lymphatics to the cystic LN of Lund hilum of liver coeliac LN
Subserosal lymphatics to subcapsular lymphatics of liver
Bile:
40ml hour
97% water
Bile salts 1-2%, bile pigments 1%, cholestrol, and fatty acids
Functions of gall bladder:
Reservoir
Concentration of bile, 5 - 10 times
Secretion of mucus– 20ml/day
3
Investigation of the Biliary tract :
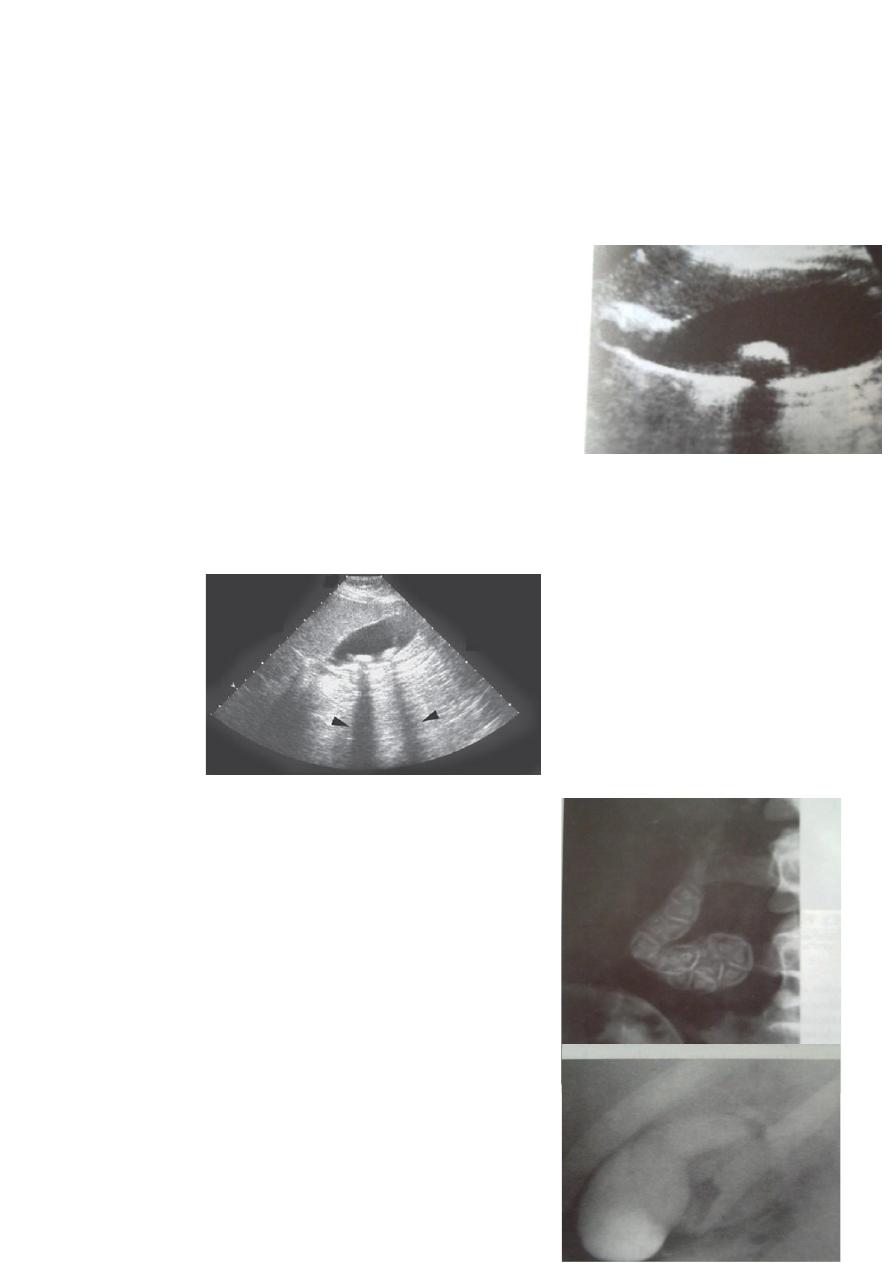
Ultrasound : stones and size
Plain radiograph : calcification
MRCP : anatomy and stones
CT scan : cancer and anatomy
HIDA scan : fucntion
Ultrasonography
:
Non-invasive
Standard initial imaging for patient suspected to have
a gall stone and in
jaundiced patients
Ultrasonography can demonstrate :
Gall stones
GB size, thickness of its wall, presence of inflammation around it, pericystic edema
Size of CBD, occasionally stones in it.
Tumour of pancreas.
Endoscopic ultrasound <<Stone and obstruction of lower CBD
Plain radiography :
Radiopaque gall stones in 10%
Prolactine GB , calcified GB , 25% CA
Limey bile
Gas in the wall , emphysematous cholecystitis
Gas in the biliary tree :
Endoscopic sphincterotomy
Surgical bilio-enteric anastomosis
Internal biliary fistula
Oral cholecystography
Once was of first choice in the dx of gall stones
Intravenous cholangiography
4
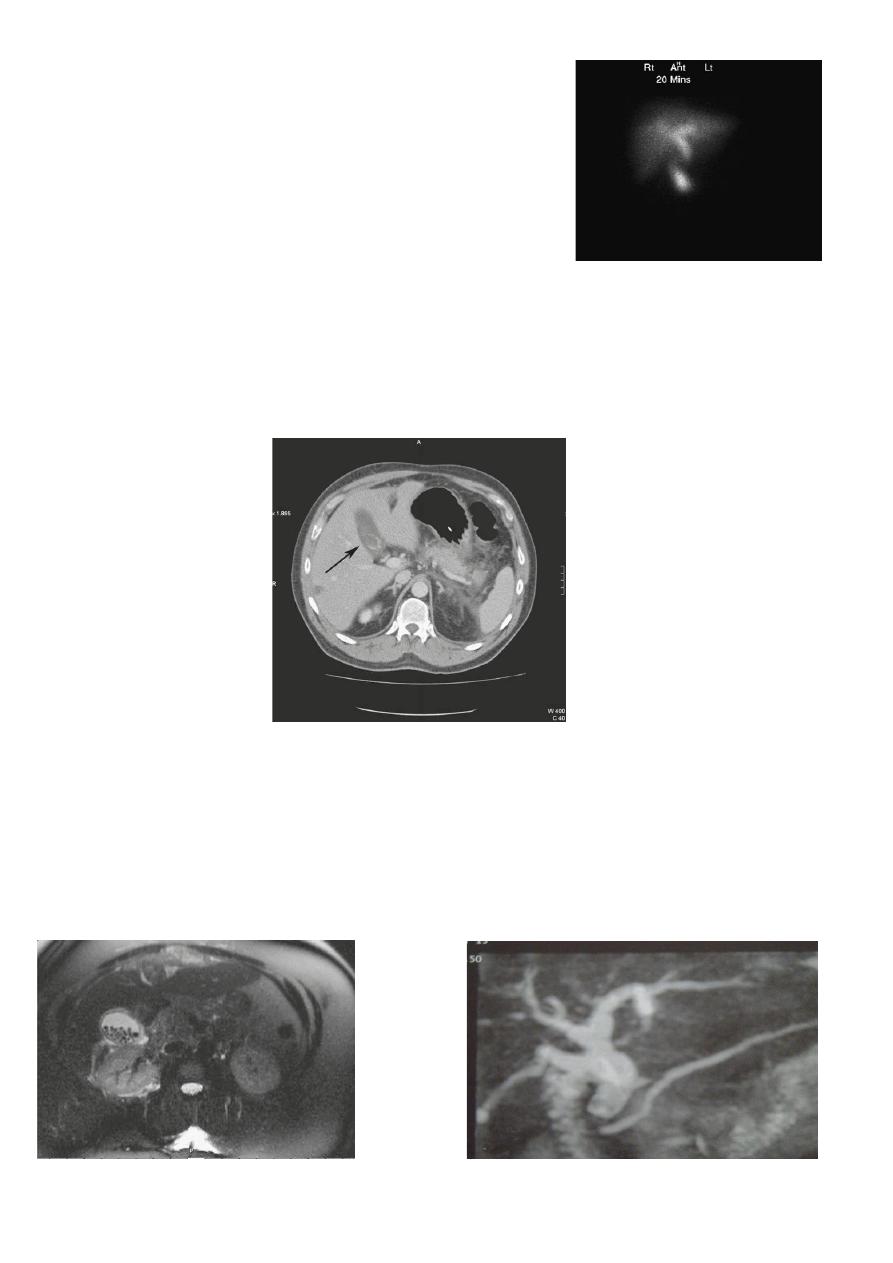
Radioisotope scanning:
Tc 99m labelled with derivatives of iminodiactic acid
(HIDA, PIPIDA), that are excreted in the bile.
Dx of acute cholecystitis GB not visulized
Bile Leakage, assessment
Dimethyl iminodiacetic acid (HIDA) scan.
Computerized Tomography scan :
limited usefulness in investigating the biliary tree
Only when there is a possibility of cancer of gall bladder or bile ducts
Use of CT scan is an integral part of the differential diagnosis of obstructive jaundice
Computed tomography scan demonstrating a gallstone within the gall bladder
(arrowed).
Magnetic Resonance Cholangiopancreatograph: (MRCP)
Standard for biliary tree investigation
Contrast is not
Magnetic resonance cholangio-pancreatography crosssectional image demonstrating a hilar mass
(thick arrow) and gallstones (thin arrow)
5
ENDOSCOPIC RETROGRADE CHOLANGIOPANREATOGRAPHY (ERCP)
Side veiwing endoscopie
Cannulation of ampulla of Vater
Injection of contrast to visualize the bile ducts
Also bile can be taken for cytological and microbiological tests
Brushings from strictures
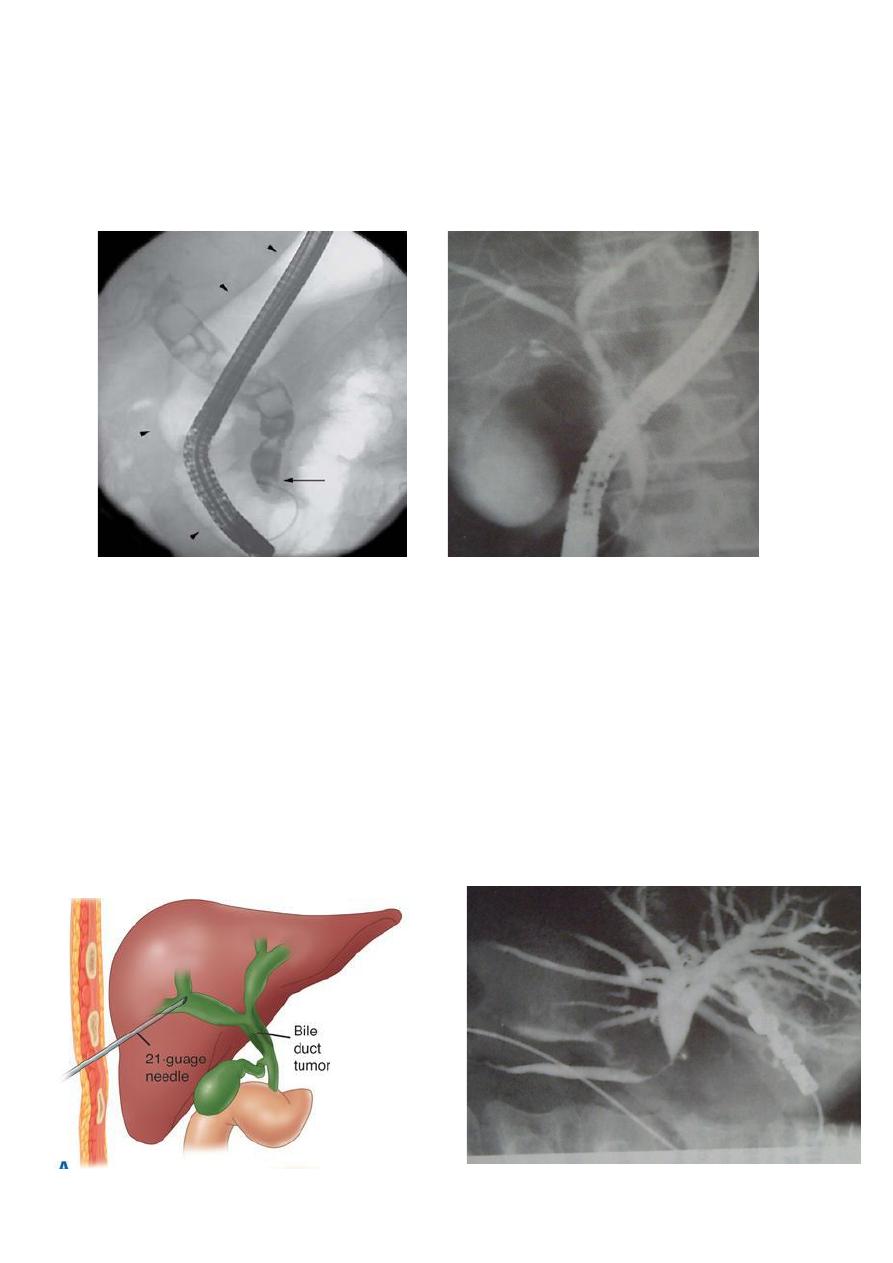
PERCUTANEOUS TRANSHEPATIC CHOLANGOGRAPHY (PTC):
Preparation :
Normal PT
Antibiotics
DX and therapy :
Visulization of biliary tree
Placement of : catheter
Stenting
Choledochoscope
6
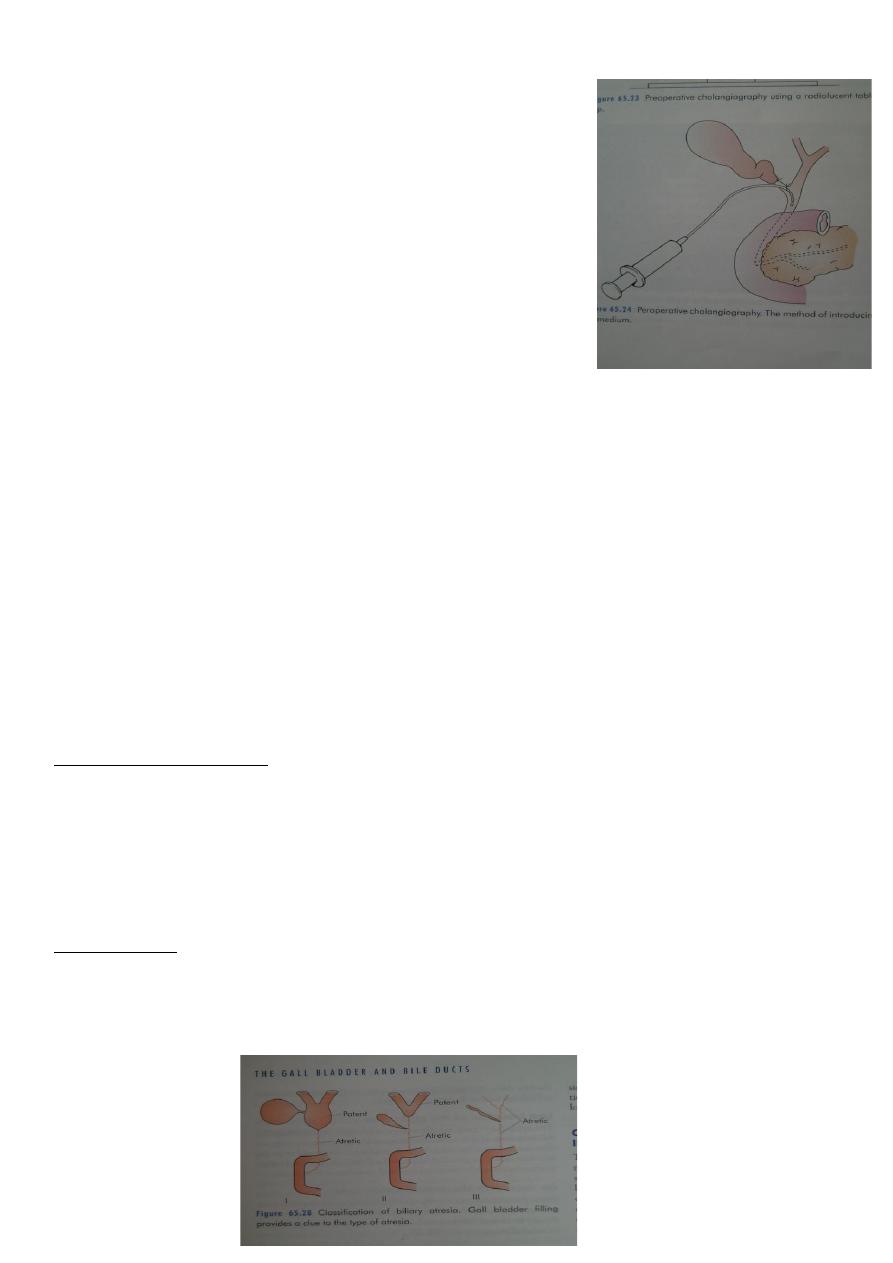
Peroperative cholangiography
Operative biliary endoscopy
(choledochoscopy)
DISEASES OF GALL BLADDER AND BILIARY PASSAGES
Congenital
Acquired
CONGENITAL ABNORMALITIES OF THE GB AND BILIARY TREE
Absence of GB
The phrygian cap
Floating GB
Double GB
Absence of CD
Low insertion of CD
An accessory cholecystohepatic duct ( small ducts of Luschka)
EXTRAHEPATIC BILIARY ATRESIA
Aetiology and pathology:
1 per 14000 live birth
Equal and female
If untreated the child dies before the age of 3 years
20% associated anomalies, cardiac, situs inversus, absent vena cava
Classification:
Type I : atresia restricted to the CBD
Type II :atresia of the CHD
Type III : atresia of the right and left HD

7
Clinical features:
1/3 jaundiced at birth
All jaundiced by the end of the week
Meconium little bile stained
Pale stool and dark urine
Osteomalacia
Pruritis
Clubbing skin xanthoma
Differential Diagnosis
Alpha 1 antitrypsin deficiency
Choledochal cyst
Inspissated bile syndrome
Neonatal hepatitis
Traetment:
Roux-en Y anastomosis
Kasai procedure
CHOLEDOCHAL CYST
Weaknes of part or whole of the wall of the CBD
Anomalous junction of the biliary pancreatic junction:
High amylase
Repeated attacks of panreatitis
Clinical features : premalignant
At any age, Attacks of : jaundice , cholangitis
Swelling in the right hypochondrium
US –abnormal cyst
MRI– clear anatomy
Treatment: Radical excision of the cyst and reconstruction of the biliary tract using Roux en
Y jejunal loop
TRAUMA
Iatrogenic
Accidental, is rare, penetrating or crushing
Presentation of acute abdomen
8
Treatment:
GB—cholecystectomy
Bile ducts:
Drainage using T tube
Roux-en-Y
GALL STONES (CHOLELITHIASIS)
Most common pathology
Affecting about 10–15% of the adult population.
Mostly asymptomatic in >80%
Cholecystectomy is one of the most common operations performed by general
surgeons
AETIOLOGY OF GALLSTONES :
Metabolic
Infective
Stasis
RISK FACTORS ASSOCIATED WITH FORMATION OF GALL STONES
Age > 50 years
Female sex (twice risk in men)
Genetic or ethnic variation
High fat, low fibre diet
Obesity
Pregnancy (risk increases with number of pregnancies)
Hyperlipidaemia
Bile salt loss (ileal disease or resection)
Diabetes mellitus
9
Cystic fibrosis
Antihyperlipidaemic drugs (clofibrate)
Gallbladder dysmotility
Prolonged fasting
Total parenteral nutrition
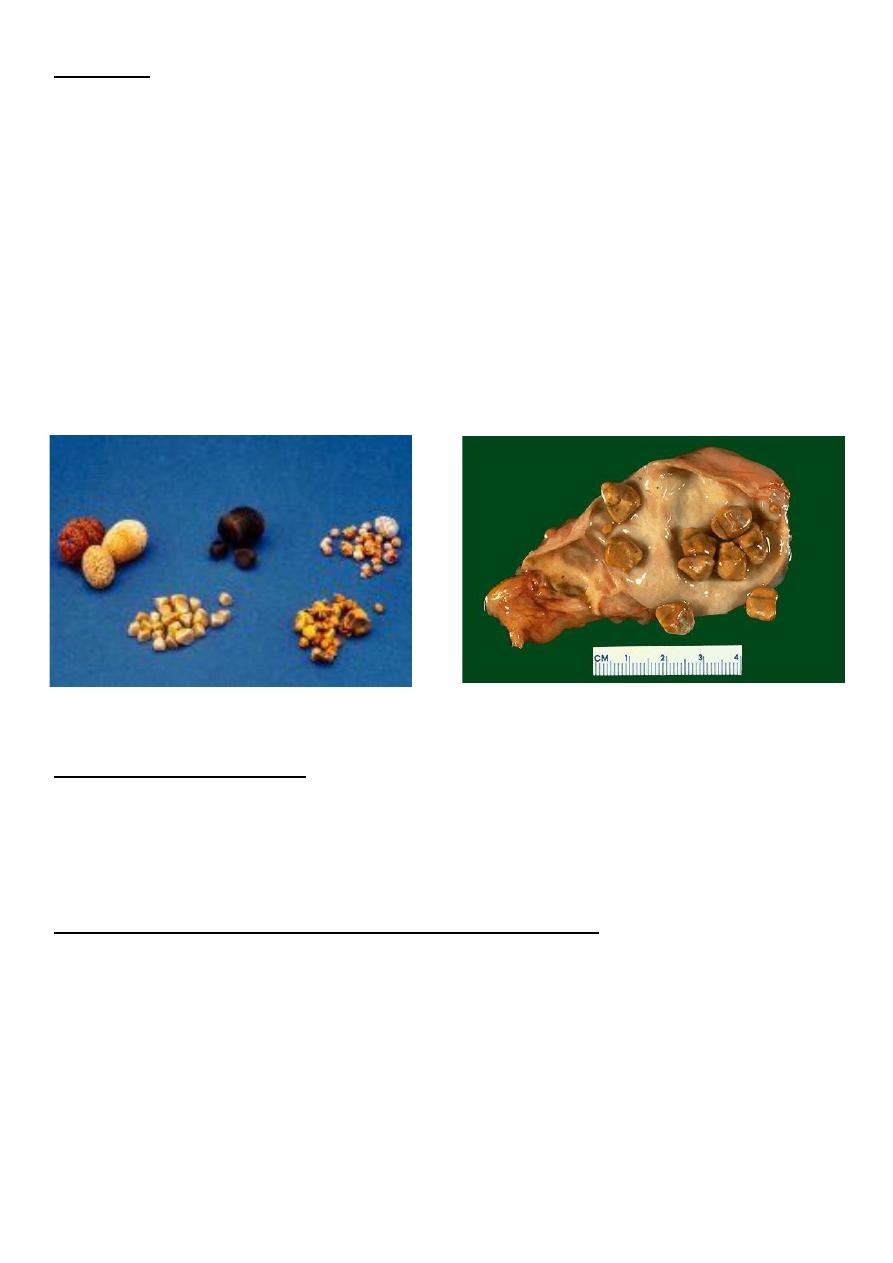
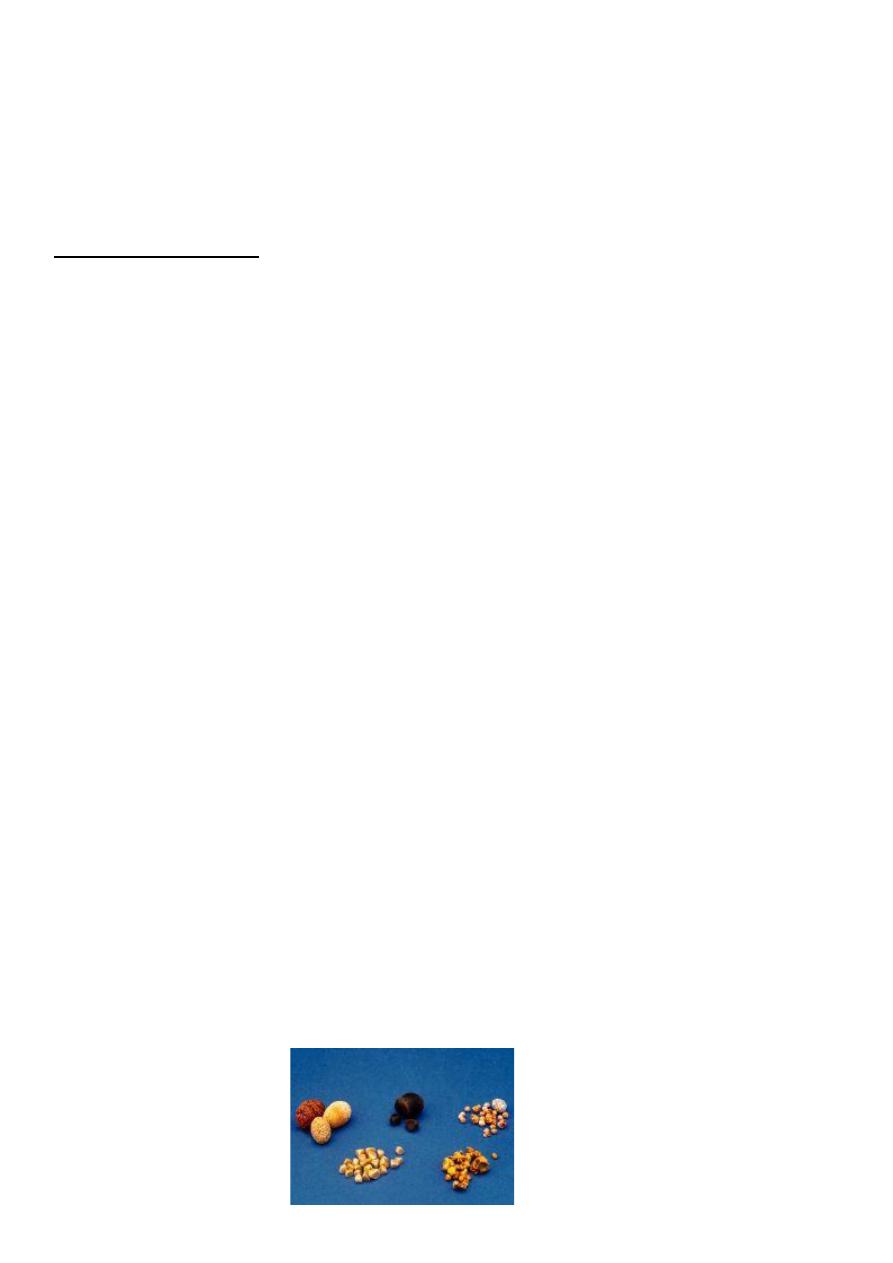
TYPES OF GALL STONES:
Cholesterol
Pigment stones
Mixed stones
CHOLESTEROL STONES
Contain mainly pure cholesterol
•Mostly single ( cholesterol solitaire)
•Obesity,
•high-calorie diets
•certain medications
PIGMENT STONES:
Black stones
Contents: insoluble bilirubin pigment polymer mixed with calcium phosphate
and calcium bicarbonate and < 30% cholesterol
Hemolysis : Hereditary spherocytosis
Sickle cell anaemia
Brown stones:
calcium bilirubinate, calcium palmitate and calcium stearate, as well as
cholesterol
form in the bile duct and are related to bile stasis and infected bile.
MIXED STONES:
Cholesterol major component
Ca bilirubinate, Ca palmitate, Ca carbonate, Ca phosphate, and proteins
Account for 90%
Multiple
Faceted
10
INCIDENCE OF GALL STONES
Female
Fat
Fertile
Fifty
Flatulent
CAUSAL FACTORS IN GALL STONE FORMATION
Metabolic
Infective
Stasis
Metabolic:
Cholesterol
Bile salt
Phospholipid
High cholesterol “Supersaturated” or “lithogenic” bile
Aging
Female contraceptives
Obesity
Clofibrate
Interruption of enterohepatic circulation of bile salts
lead to low bile salts.
Infection:
Unclear
Radiolucent centre of stone mucus plug as nidus for stone formation
B glucuronidase unconjugated insoluble bilirubin.
11
Bile stasis:
Decrease contractility of gall bladder
Estrogen in pregnancy
Parenteral nutrition
Truncal vagatomy
EFFECTS AND COMPLICATIONS OF GALL STONES :
In the GB:
Silent up to 80%
Chronic cholecystitis
Acute cholecystitis
Gangrene
Perforation
Empyema
Mucocele
carcinoma
In the bile ducts:
Obstructive jaundice
Cholangitis
Acute panreatitis
In the intestine:
Acute intestinal obstruction ( gall stone ileus)
12
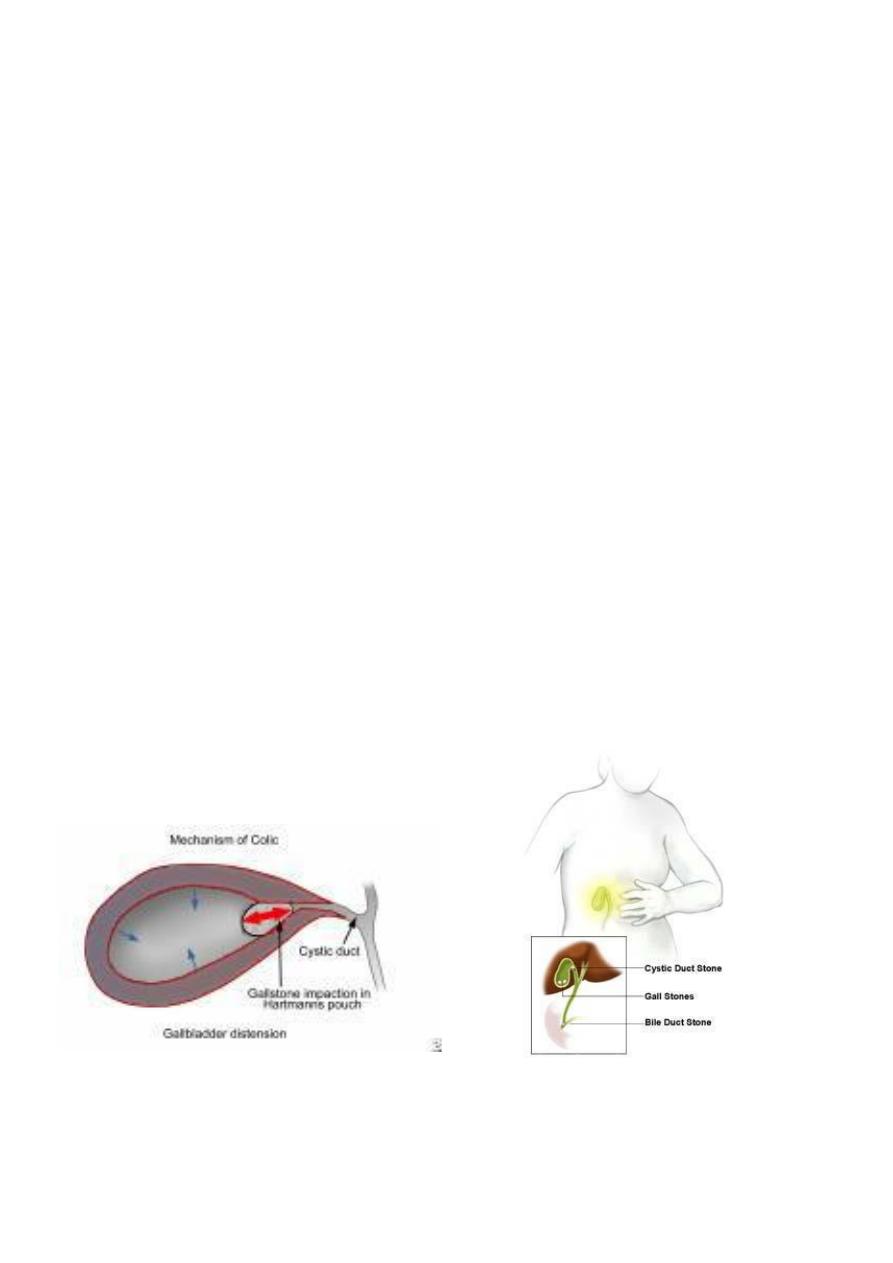
ACUTE CHOLECYSTITIS :
Right hypochondrial pain
Radiate to back, chest
Referred right shoulder pain
Occ. Start at epigastrium or left subcostal
Start at night
Other symptoms : Dyspeptic symptoms , Vomiting , fever
ACUTE CHOLECYSTITIS
BILIARY COLIC
1. Several hours to few days
2. Fever
3. leucocytosis
1. Few minutes to few hours
2. No fever
3. No Leucocytosis
DIFFERENTIAL DX
Common:
Appendicitis
Perforated peptic ulcer
Acute pancreatitis
Uncommon:
Acute pyelonephritis
MI
Pneumonia, right lower lobe
DIAGNOSIS
Physical examination:
Murphy’s sign
Palpable tender gall bladder.
Ultrasound
Liver function test : Bilirubin
WBC
CXR pneumonia ,air under diaphragm
ECG
GUE and urine culture

13
TREATMENT
Conservative
Urgent cholecystectomy
Early cholecystectomy
Elective cholecystectomy
CONSERVATIVE TREATMENT
NPO with IV fluids
NG tube
Analgesia
Antibiotics
Follow up
90% respond to conservative treatment.
Subsequent treatment:
Early cholecystectomy next op. list 5-7 days
Elective cholecystectomy 6 weeks
When to stop conservative treatment : << URGENT
CHOLECYSTECTOMY
- When there is increasing in :
pain and tenderness
pulse and temperature
leucocytosis
Conservative treatment is not advised
<< Uncertinity about the dx
EMPYEMA OF THE GALL BLADDER :
Pus filled gall bladder
A sequel to acute cholecystitis or Mucocele
Treatment:
Cholecystectomy
Disturbed anatomy---- drainage (Cholecystostomy) later cholecystectomy
Acalculous cholecystitis
Acute or chronic
Dx by: Radioisotope in acute cholecystitis
Acute acalculous can occur in patients after major surgery, trauma, burn
CHOLECYSTECTOMY :
Indications
Symptomatic cholelithiasis
Trauma

14
Part of other operation -----Whipple’s procedure
Neoplasia of Gall Bladder
Preparation for operation
Full blood count
Renal profile and liver function tests
Prothrombin time
Chest X-ray and electrocardiogram (if over 45 years or medically indicated)
Antibiotic prophylaxis
Deep vein thrombosis prophylaxis
Informed consent
procedure
Laparoscopic cholecystectomy (Gold standard )
Open colecystectomy
COMPLICATIONS OF CHOLECYSTECTOMY
Inraoperative:
Biliary injuries
Iatrogenic injuries to near by organs
Bleeding.
Early postoperative:
CBD obstruction------------Jaundice
CBD injury --------------Collection , Biliary peritonitis
Bleeding ---------------Local hematoma, Shock
Missed stone in CBD
COMPLICATIONS OF LAPAROSCOPIC CHOLECYSTECTOMY
access complications
bile duct injuries
Biliary injury:
Bile leakage
Local collection or excessive bile drainage if drain is present
Biliary peritonitis
15
PAIN AFTER CHOLECYSTECTOMY
Causes:
Incorrect preoperative diagnosis - for example, irritable bowel syndrome, peptic
ulcer, gastro.oesophageal reflux
Retained stone in the CBD or CD stump
Iatrogenic biliary injury : stricture of common bile duct
Papillary stenosis or dysfunctional sphincter of Oddi
ALTERNATIVE TREATMENT
Criteria for non-surgical treatment of gall stones
Cholesterol stones < 20 mm in diameter
Fewer than 4 stones
Functioning gall bladder
Patent cystic duct
Mild symptoms
SUMMARY POINTS :
Gall stones are the commonest cause for emergency hospital admission with
abdominal pain
Laparoscopic cholecystectomy has become the treatment of choice for gallbladder
stones
Risk of bile duct injury with laparoscopic cholecystectomy is around 0.2%
Asymptomatic gall stones do not require treatment
Cholangitis requires urgent treatment with antibiotics and biliary decompression by
endoscopic retrograde cholangiopancreatography
OBSTRUCTIVE JAUNDICE :
Attributed to CBD obstruction
Stone in CBD
Carcinoma of CBD
Tumor of head of pancreas
FB inside the CBD
Paracitic
MANAGEMENT OF CBD OBSTRUCDTION
Following cholecystectomy
Jaundice ---- immediate action
Ultrasound :
Dilatation
Collection at porta hepatis
16
Biochemical investigations
Immediate MRCP:
If stone detected endoscopic extraction(ERCP)
If CBD obstruction --- surgery
If bile leakage :
Percutaneous drainage
Stenting
STONES IN THE CBD
Several years after cholecystectomy
CBD infestation by Ascaris lumbricoides or clinorchis sinensis
Clinical presentation:
Asymptomatic
Jaundice
Cholangitis ( Charcoat triad )
Fever and rigor
Jaundice
Pain
Signs : Tenderness upper abdomen and RUQ
Management:
Dx
Ultrasound
Liver function test
Liver biopsy
MRCP
ERCP
Resuscitaion
Rehydration
Broad spectrum Antibiotics
Attention to clotting Vit K
Relief of obstruction
Endoscopic sphincterotomy : extraction of stone by Dormia basket or balloon
catheter
Some times stent placement
Percutaneous transhepatic cholangiography:
then drainage
Percutaneous choledochoscopy
Surgery: Choledochotomy

17
Indication for CHOLEDOCHOTOMY
Preoperative:
Stone in CBD
Dilatation of CBD
History of jaundice
Peroperative:
Palpable stone
Dilated CBD
STRICTURE OF CBD :
Benign stricture: 80% postoperative and 20% inflammatory
Malignant stricture
CAUSES OF BENIGN BILIARY STRICTURE
Congenital
Biliary atresia
Bile duct injury at surgery
Cholecystectomy
Choledochotomy
Gastrectomy
Hepatic resection
Transplantation
Inflammatory
Stones
Cholangitis
Parasitic
Pancreatitis
Sclerosing cholangitis
Radiotherapy
Trauma
Idiopathic
POSTOPERATIVE STRICTURE
Technical error during cholecystectomy
Blind control of bleeding in Calot triangle
Failure to identify the anatomy at Calot triangle : acute inflammation
Mirizzi syndrome
Short or absent cystic duct
Anatomical anomalies

18
CBD obstruction
Deeping jaundice
Partial obstruction delayed jaundice
Radiological investigations:
Ultrasound
MRCP
Cholangiography
Through tube
PTC
ERCP
Treatment
Supportive
Relief of obstruction : temporary
ERCP stenting
Transhepatic external drainage and stenting
For strictures of recent onsent:
ERCP --- guide wire---- balloon dilatation---stent placement
Definite relief of obstruction: Choledocho-jejunostomy
Late complications:
CBD stricture
Stone in CBD
Post cholecystectomy pain syndrome
Wrong preoperative diagnosis
Complication of cholecystectomy
PARASITIC INFESTATION OF THE BILIARYBILIARY TRACT
Ascariasis
The round worm, Ascaris lumbricoides, commonly infests the intestine
Complications:
strictures,
suppurative cholangitis,
liver abscesses and empyema of the gall bladder
19
HYDATID DISEASE
Jaundice:
Cyst near porta hepatis
Rupture of cyst into the biliary passages
TUMOURS OF THE BILE DUCT
:
Benign tumours of the bile duct:
Rare
Symptoms not distinguished from common biliary problems
Malignant tumours of the bile duct
Rare, but incidence increasing
Presents with jaundice and weight loss
Diagnosis by ultrasound and CT scanning
Jaundice relieved by stenting
Surgical excision possible in 5%
Prognosis poor – 90% mortality in 1 year
The tumour is usually an adenocarcinoma (cholangiocarcinoma), predominantly in the
extrahepatic biliary
RISK FACTORS
ulcerative colitis, hepatolithiasis, choledochal cyst ,sclerosing cholangitis.
liver fluke infestations in the Far East
CLINICAL FEATURES
Jaundice
Abdominal pain, early satiety
weight loss
palpable gall bladder
INVESTIGATIONS :
Biochemical investigations
tumour marker CA19-9
ultrasound and CT scanning define:
the level of biliary obstruction
the locoregional extent of disease
the presence of metastases
percutaneous transhepatic cholangiography
ERCP
20
TREATMENT : Most patients are inoperable, but 10–15% are suitable for surgical resection
CARCINOMA OF GALL BLADDER :
Risk factors
Comon in india Incidence 9%
Gall stones less than 1%
90% of Ca GB have gall stones
Pathology:
Schirrous adenocarcinoma
Squamous cell
Mixed sq adenocarcinoma
Spread:
Direct invading the liver
Lymphatics
Peritoneal seedlings
Clinical features:
Mostly elderly 70 years
Females more than males 5:1 ratio
Same as cholecystitis
Suspected during cholecystectomy then preoved by histopathology
Jaundice
Mass in liver late sign
INVESTIGATION
non-specific findings such as anaemia, leucocytosis, mild elevation of transaminases
and increased erythrocyte sedimentation
rate (ESR) or C-reactive protein (CRP).
Elevated CA19-9
US and CT scan
percutaneous biopsy
Laparoscopy
Treatment:
Usually discovered after cholecystectomy and so no further surgical treatment
required If tumor confined to mucosa good prognosis
transmural disease, a radical en bloc resection of the gall bladder fossa and
surrounding liver along with the regional lymph nodes
21
PATHOGENESIS OF STONE FORMATION
For cholesterol stones:
Supersturation of bile with cholesterol
Low bile acid concentration
For pigment stones:
Usually accompany haemolysis like in:
Spherocytosis
Sickle cell disease
Prosthetic heart valves
For mixed(brown) stones:
Stasis
Infection—beta glucuronidase insoluble unconjugated bilirubin
Have Fun
:D
