1
4th stage
طب مجتمع
Lec-4
د.ظافر
10/11/2015
Coronary Heart Diseases (Ischemic heart diseases)
Definition:
“impairment of heart function due to inadequate blood flow to the heart
compared to its needs, caused by obstructive changes in the coronary
circulation to the heart”
WHO→ CHD, CAD or IHD is our modern epidemic or the emerging
epidemic.
IHD is first leading cause of
Death in the World.
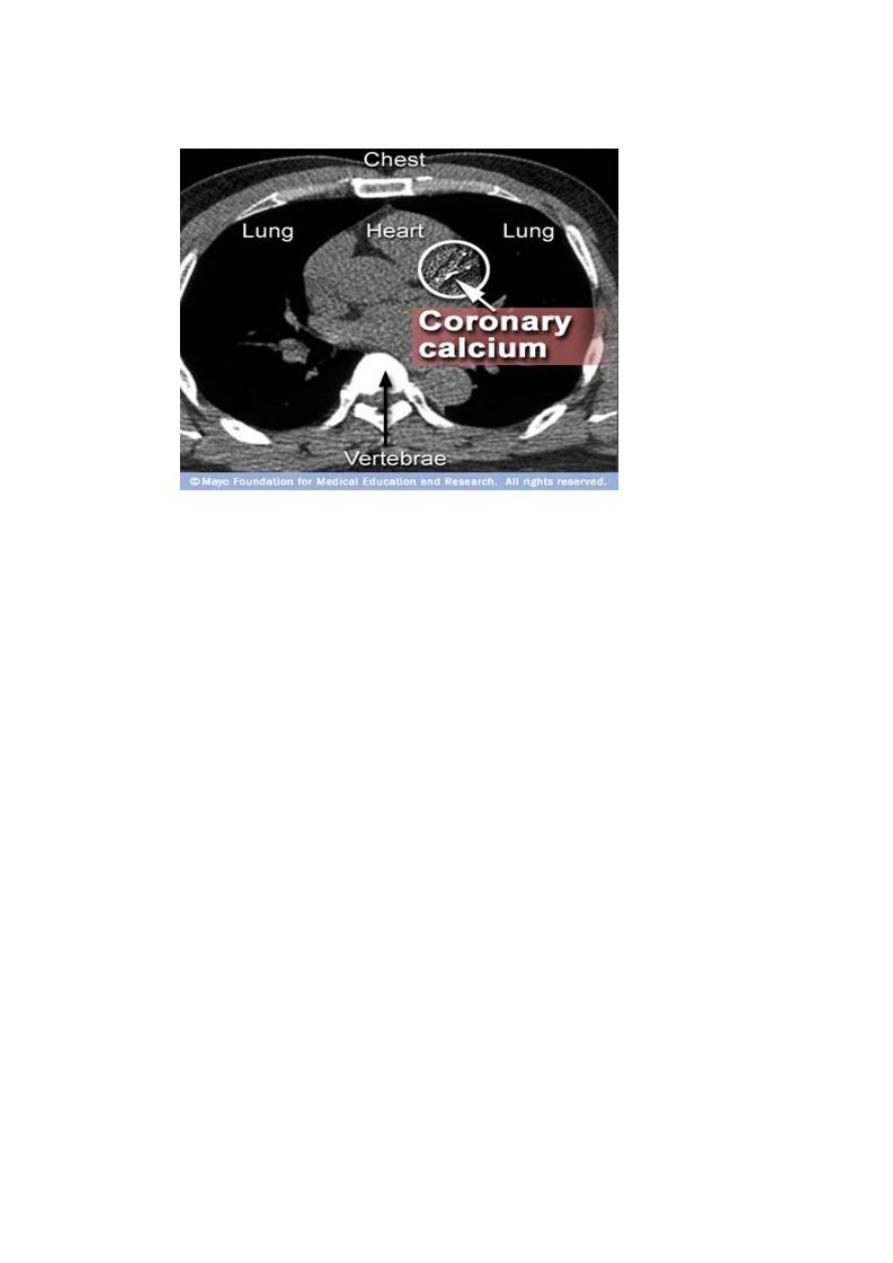
The lumen of a coronary artery can be narrowed when a segment of the
wall thickens (stenosis).
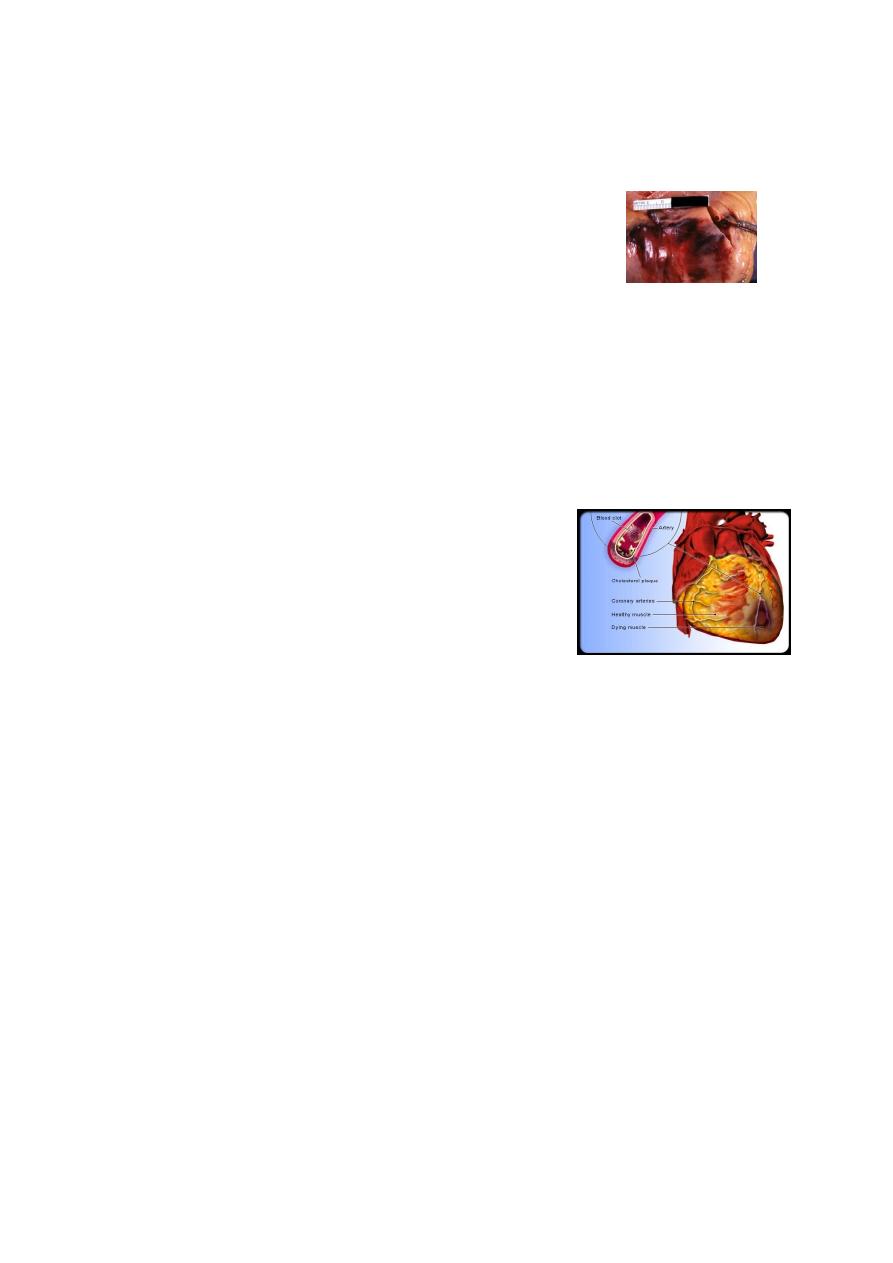
Coronary Atherosclerosis:
This process of arteries thickening and
narrowing is brought about by two linked
processes called atherogenesis and
thrombogenesis
.
Atherogenesis:
Is the formation of atherosclerotic plaque (atheroma) in the internal
layer of the wall of the artery.
Thrombogenesis:
Is the formation of a blood clot (thrombus) in a vessel by
thrombocytes circulating in the blood on atheromatous plaque.

2
Atherogenesis:
Is the formation of atherosclerotic plaque (atheroma) in the internal
layer of the wall of the artery.
Atherogenesis starts with fatty deposits. Fibrous tissue then grows
around a fatty deposit creating an atherosclerotic plaque, which
protrudes into the lumen of the artery narrowing it.
Thrombogenesis:
Is the formation of a blood clot (thrombus) in a vessel by
thrombocytes circulating in the blood on atheromatous plaque.
, it releases
desquamates
or
ulcerates
When a plaque full of cholesterol
the cholesterol content and various fragments of the plaque to the
circulation.
by thrombocytes circulating in
blood clot
This triggers the formation of a
the blood, which leads to varying degrees of obstruction of the lumen.
Clinical manifestations of coronary atherosclerosis
Usually develop when the coronary arteries are narrowed at least by
75%.
1. Chest pain (angina pectoris ”stable or unstable”).
2. Heart attack (myocardial infarction).
3. Arrhythmia of any kinds.
4. Sudden cardiac death.
5. Congestive heart failure.
3
Irreversible damage to the cells may occur in about 40 minutes.
The dead heart muscle cells cannot be replaced by
new muscle cells (specialized).
They are replaced by scar tissue, which is less elastic
and does not contract as the muscle leading to many
complications.
The role of infection:
Certain infectious agents have been implicated based on their isolation
from the atheromatous plaques or on the presence of positive serology
findings for organisms such as
1. C pneumoniae,
2. Helicobacter pylori,
3. Herpes simplex virus,
4. Cytomegalovirus.
Risk factors:
The cause of atherosclerosis is not known.
Risk factors can be divided into those that cannot be changed
(unmodifiable; namely age, sex, race and family history) and those that
can be (modified; or managed (such obesity and alcohol consumption).
Risk factors multiply each other’s effect of increasing the risk of CHD
(multiplicative not additive).

4
Un-modifiable risk factors:
Age:
40-45 for men
50-55 for women.
Sex:
At all age men > women
There is about a decade difference in incidence.
Family history:
Close or primary relatives.
Especially premature atherosclerosis.
Race:
Till now there is no clear data established CHD state.
Modifiable risk factors:
Dyslipedemia:
↑ LDL
↑ VLDL
↑ TG
↑ Cholesterol
↓ HDL
Smoking:
Very strong evidence
Dose-response relationship
2-4 times risk
Passive smokers also at large risk
Multiplicative effects by acting on other risk factors

5
Modifiable risk factors:
Hypertension:
Well established risk factor
Both systolic and diastolic hypertension
Obesity:
Central obesity more harmful than general obesity
BMI > 25 (pre-obese) and > 30 (obese)
WHR > 1 for men and WHR > 0.85 fro women
Waist > 40 inch for men and Waist > 35 inch for women.
Modifiable risk factors:
Diabetes:
Both types IDDM and NIDDM
Risk equivalent to established CHD
It causes and accelerates atherosclerosis
Do not forget “silent MI”.
Sedentary life:
Because physical activity improves lipid profiles, ↓ BP, controls body
weight, controls serum glucose, copes with stress.
At least 30 min exercise (moderate) / day for 4-5 times / week.
Modifiable risk factors:
Metabolic Syndrome:
A cluster of Most established heart attack risk factors including:
- Diabetes or insulin resistant (± glucose intolerance), +
- Raised blood pressure, +
- Atherogenic dyslipidemia, +
- Abdominal obesity, +
- Pro-thrombotic (± pro-inflammatory state)
* Main target for intervention.

6
Personality type A
Alcohol drinking
Dependent / Emerging / Novel Risk Factors:
•↑ Homocysteine.
•↑ Lp (a).
•Abnormalities in blood coagulation:
– ↑ Plasma fibrinogen.
– ↑ Coagulation factors: V, VII, VIII.
– Platelets abnormalities.
– Impaired fibrinolysis.
•Inflammatory markers:
– C-Reactive protein.
– Interlukin.
•Short stature.
•Impaired glucose tolerance.
•Increased oxidative stress.
•Stress.
•Tachycardia.
•Ethnic group.
•S. creatinine.
Ultra-novel risk factors:
• Plasma Myeloperoxidase.
• Red Cell Glutathione Peroxidase 1 activity.
Prevention:
1. Primary: By eliminating or reducing established risk factors (such as
stop smoking and decrease weight)
2. Secondary: Good treatment of established case MI to reduce
complication.
3. Tertiary: Rehabilitation of established case of MI to return to normal
life.

7
4. Primordial: Prevention of risk factor before its development (such as
healthy diets for baby).
Strategies for prevention:
1. Population strategies.
2. High risk strategies.
The assessment of overall cardiovascular (CV) risk is a valuable and
accepted means of identifying patients who are likely to benefit most
from intervention.
Risk elimination is central to the management of CV disease.
Data from large epidemiological cohort studies have provided the raw
data used to evaluate the contribution of individual CV risk factors.
Usually, they use 10 years risk (prediction) of large CV events (such MI)
for certain person, given as %.
Example: Peter has a 5% global risk of CV event, this means, 100
persons, like Peter, 5 of them will get major CV event (like MI) within
subsequent 10 years.
GLOBAL RISK ASSESSMENT SCORING SYSTEMS
• FRAMINGHAM Scoring System (USA).
• PROCAM Scoring System (Germany).
• SCORE Project (European).
• INDIANA Project (Latin Americans).
• Australian Scoring System (Australia).
8
9
11
4th stage
طب مجتمع
Lec-5
د.ظافر
10/11/2015
Rheumatic Heart Disease
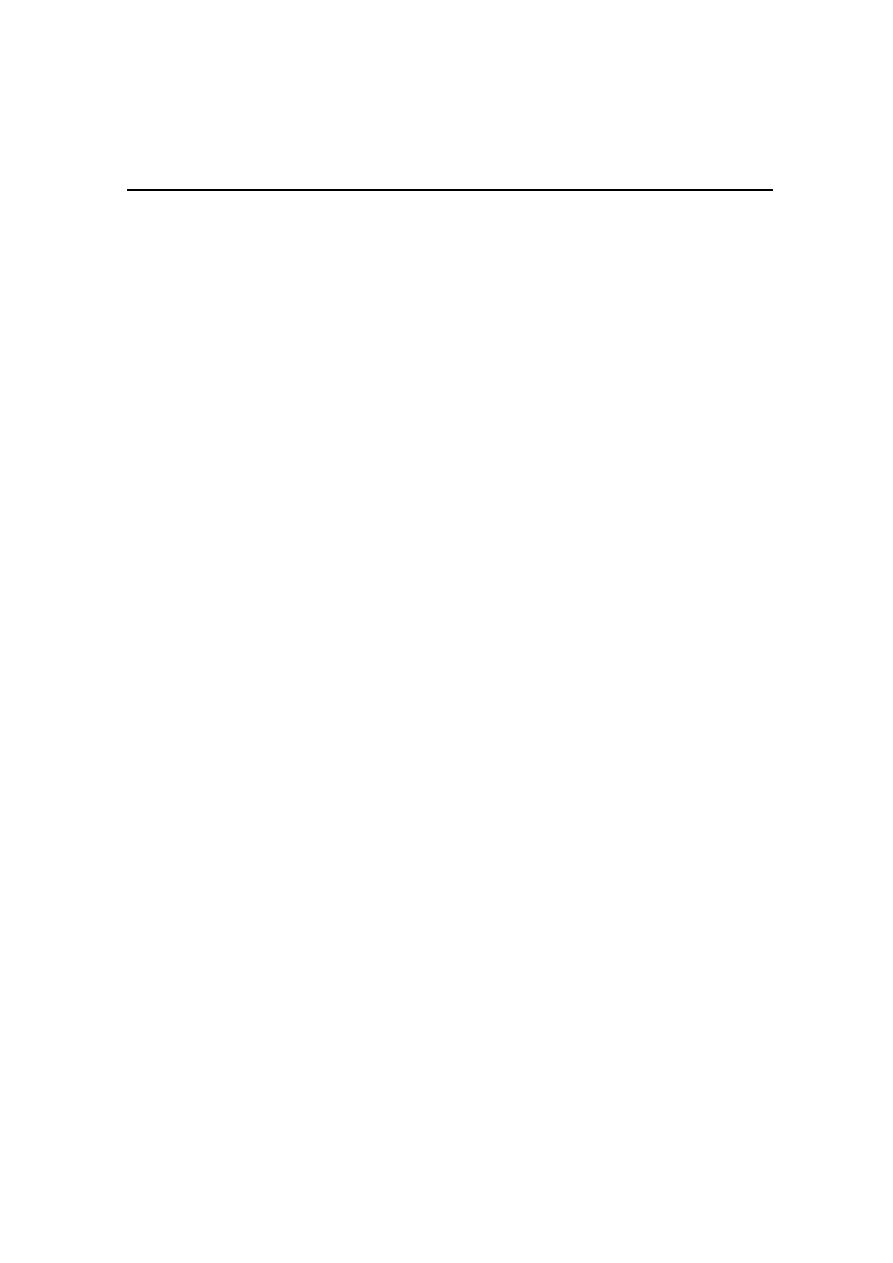
Rheumatic fever (RF) and rheumatic heart disease (RHD) cannot be
separated from an epidemiological point of view.
Rheumatic fever: is a febrile disease affecting connective tissues
particularly in the heart and joints initiated by infection of the throat by
group A beta
hemolytic streptococci.
Although RF is not a communicable disease, it results from
communicable disease (streptococcal pharyngitis).
* RHD is one of the most readily
preventable chronic non-communicable
diseases.
* RF often leads to RHD, which is
a crippling disease with many
consequences such as the following:
- Continuing damage to the heart.
- Increasing disabilities.
- Repeated hospitalization.
- In addition, premature deaths usually around 35 years
Size of the problem:
* RF and RHD present a problem in all parts of the world, especially in
the developing countries.

11
* The reported prevalence rate in school-age children in various parts of
the world ranges from 1 as very low to 33 cases per 1 000\ year.
* Throughout the world, RF is the most common cause of heart diseases
in the age group of 5-30 years,
It causes about one third of deaths from heart diseases.
* The great decrease in incidence of RHD and RF in most developed
countries occurred before the advent of antibiotics. (????)
Epidemiological Factors:
I- Agent factors:
A- Agent:
The onset of RF is usually preceded by a streptococcal sore throat.
Among streptococci, group A, is the causative factor in RF, even not all
group A, but certain "rheumatogenic potential" (serotype is M type 5).
All group A streptococci are sensitive to penicillin. Recently, the virus
(Coxsackie's B-4) has been suggested as a causative factor and
streptococcus acting as a conditioning factor.
Epidemiological Factors:
I- Agent factors:
B- Carriers:
Carriers of group A streptococci are very frequent, including
convalescents, transient and chronic carriers. Theoretically, it is
impossible to eradicate them.
Epidemiological Factors:
II- Host and environmental factors:
A- Age: RF is typically a disease of young 5-15 years.
B- Sex: Both sexes are affected equally.
12
C- Immunity: The toxic-immunological hypothesis (certain products of
group A streptococci act as an antigenic cross-relationship with host
tissues).
D- Socio-economic status: It is a disease of poor, overcrowded people
with poor housing conditions and inadequate health services (social
disease).
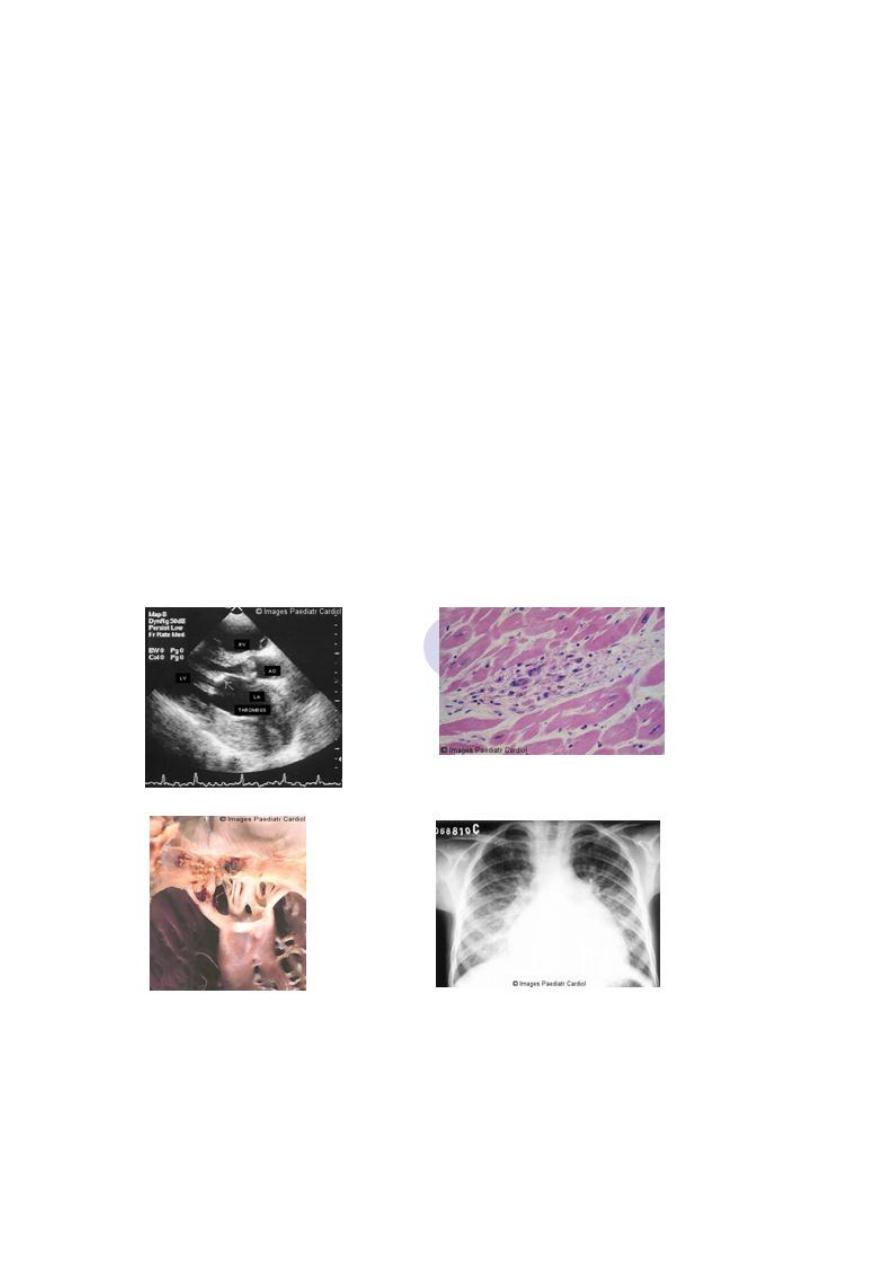
Clinical Features:
Fever: May stays for even 12 weeks or longer with sweating.
Polyarthritis: 90 % of cases, with large joints affection with no residual
damage.
Carditis: 60-70 % and involves all layers of the heart, leading to
tachycardia, cardiac murmurs, cardiac enlargement, pericarditis, and
heart failure (ECG finding is the first-degree AV block).
13
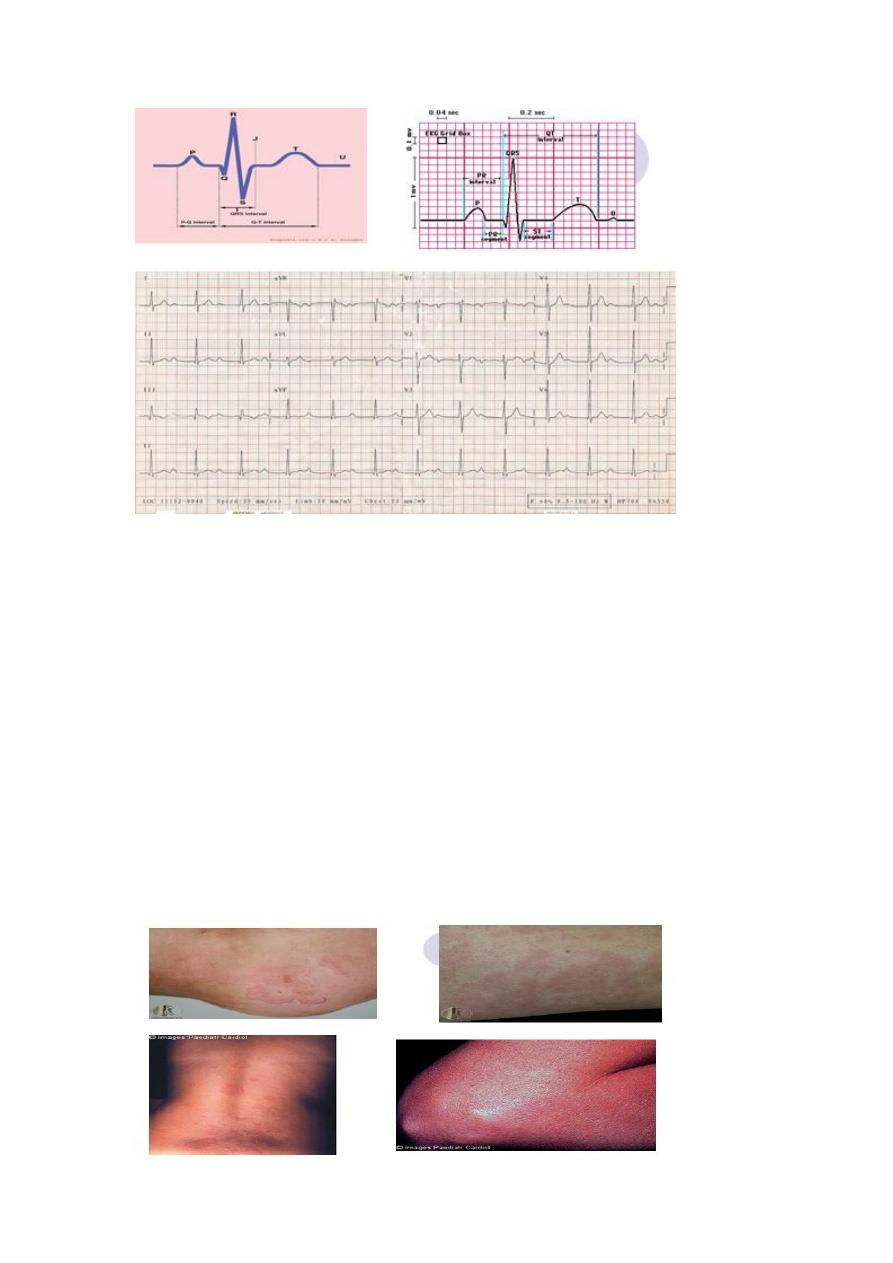
Clinical Features:
Nodules: 4 weeks after the onset of RF, small, non-tender, below skin,
and painless with no residual damage after disappearance.
Brain involvement: As abnormal, jerky, purposeless movements of arms,
legs and body, and disappear without any sequels.
Skin: Different rashes.
* All clinical manifestations disappear without any permanent damage
except carditis.
14
Diagnosis:
The WHO Expert Committee in 1988 has recommended the use of the
"revised" Jones criteria for the diagnosis of RF.
The presence of two major or one major and two minors manifestations
plus evidence of preceding streptococcal infection indicates a high
probability of RF.
Revised Jones criteria:
Major Minor
Fever
Clinical:
Carditis
Polyarthritis Arthralgia
Chorea Previous history RF or RHD
Abnormal ESR
Laboratory:
Erythema marginatum
Subcutaneous nodules C-reactive protein
Leukocytosis
Prolonged P-R
WHO also recommended the following tests as mandatory to over-
diagnose of RF:
Positive throat culture for group A streptococci, and
Demonstration of anti-streptococcal antibodies e.g. antistreptolysin O
(ASO) or other antibodies.
Prevention:
I- Primary prevention:
The aim here is to prevent the first attack of RF, by identifying all patient
with throat streptococcal infection and treating them with penicillin.
II- Secondary prevention:
The aim here is to prevent the recurrence of RF, by identifying those
who have had RF and giving them
600 000 units of benzathine penicillin for child and

15
1 200 000 units for adults at 3 weeks intervals for 5 years or until the
child reaches the age of 18 years.
This secondary prevention is feasible, inexpensive and cost-effective
when implemented through PHC.
III- Non-medical measures:
By improving living conditions.
VI- Evaluation:
6-16 years, periodic surveys, random samples are the best indicators at 5
years intervals; the recommended sample depends on the prevalence.
16
4th stage
طب مجتمع
Lec-6
د.ظافر
10/11/2015
Epidemiology of OA
Osteoarthritis (OA) is the most common form of arthritis.
Evidence of OA is present in the majority of people over age 65 y.
Definition of Osteoarthritis
“Osteoarthritis is a degenerative joint disease.
Characterized by erosion of the articular cartilage, hypertrophy of
bone at the margins (osteophytes), and sub-chondral sclerosis.
And a range of biochemical and morphologic alterations of the
synovial membrane and joint capsule.
“Despite its prevalence, the precise etiology, pathogenesis, and
progression of OA remain beyond our understanding…”
Associated Risk Factors
Age
Female versus Male sex
Obesity
Osteopenia
Occupation
Sports Activities
Prior injury
Muscle weakness
Acromegaly
Calcium crystal deposition disease

17
Clinical Features
Joints Affected: Hand interphalangeal joints, spine,
knees, hips, and first MTP.
Symptoms:joint pain worsens with use and is alleviated
with rest, stiffness, crepitus, functional impairment.
Signs: limp, deformity, alteration in joint shape, muscle
atrophy, weakness, increased effusion, crepitus, restricted
movement, joint line and peri-articular tenderness, bony
swelling, soft tissue swelling.
Radiographic Appearance
Radiographic Criteria:
Loss of joint space
Subchondral sclerosis or cyst formation
Presence of new bone formation or osteophytes

18
Do weight loss improve OA?
For a woman, weight loss of only 5kg reduces the risk of OA by more
than 50%.
Estimated that weight loss could prevent 33% of OA in women and
20% in men.
Obese women had an odds ratio of 8.57 for radiographic and
symptomatic OA of the knee.
Tylenol
Is acetaminophen effective for Osteoarthritis?
Is acetaminophen the drug of choice?
Is it safe?
Acetaminophen has clearly been demonstrated to be effective in the
treatment of the pain of OA when c/w placebo, with a NNT of 3.6 for
50% pain reduction when using 1000mg.
Acetaminophen is the drug of choice in both the ACR and EULAR
guidelines.
Acetaminophen has been demonstrated to be safe in doses up to
4gm/day.
19
Traditional NSAIDs
Are NSAIDs more effective than acetaminophen?
Are some NSAIDs more efficacious than others?
Do NSAIDs destroy cartilage in the long term?
There is no reliable evidence in human models by clinical trials that
NSAIDs are either chondroprotective or chondrodestructive.
Cochrane Review 1997: no evidence to assess clinical differences
among the various NSAIDs. Decisions should be made upon safety,
acceptability and cost.
Consensus expert opinion and clinical data appear to state that in the
treatment of mild No…as OA is principally non-inflammatory NSAIDs
should clearly be titrated for clinical effect.
to moderate osteoarthritis acetaminophen and NSAIDs have
comparable efficacy.
New FDA Recommendations
News
The three COX2 agents are associated with an increased risk of
adverse CV events c/w placebo.
Data from large clinical trials,CV risk of the COX2 equal to the
non-selective NSAIDs.
The COX2 agents reduce the incidence of GI ulcers visualized at
endoscopy.
Issues With Aspirin Use

21
Evidence (from CLASS) suggests that aspirin use, even in low doses, is
a more important risk factor for the occurrence of upper GI events
than was anticipated
Opioids
Is there a role for opioid analgesia in osteoarhtritis?
Is there a role for chronic therapy with opioid analgesics?
Steroid Injections – The Evidence
Pain and inflammation decreases
for only 2-4 weeks.
Very little comlication 1:15 000 - 1: 50 000
No evidence for cartilage destruction,
even upon repeativie injections
Patients should be informed about the above evidence
Can be done at the start, while waiting NSAIDs for action.
Braces and Heel Wedges
Principal purpose is to reduce pain, assist function, and prevent
disease progression.
Action by alterations of biomechanical force loads.
Heel Wedges
Wedges are thought to assist patients with medial compartment
osteoarthritis by mechanically decreasing the varus torque.
Braces
Valgus or unloader braces are thought to assist patients with medial
compartment osteoarthritis with a significant varus deformity.
EBM 2010
Glucosamine and chondroitin have individually and collectively
shown inconsistent efficacy, even in meta-analyses, in decreasing
knee pain and improving joint function associated with OA.

21
The literature consistently demonstrates an excellent safety profile of
these agents.
These agents may be safely tried as an initial therapy in selected OA
patients prior to initiating therapy with other
modalities of treatment.
They are not proved yet by FDA.
Hyalgan
Using Hyalgan:
Indications: indicated for the treatment of osteoarthritis not
responsive to non-pharmacologic measures and to simple
analgesics.
Requires sterile technique, remove joint effusion if present
prior to injection.
Three to five weekly injections recommended.
Is it safe?
No concern of inhibition of prostaglandins.
Post-injection synovitis is described, and can last up to three
weeks.
Exercises in Management of Osteoarthritis?
Cochrane Data Base:
High intensity and
low intensity
aerobic exercise
appear to be
effective in:
Improving functional status,
Improve gait,
Decrease pain.
Quadriceps strengthening exercises can:
22
Increase strength and;
Decrease dependency
Improve function
Decrease pain.
23
4th stage
طب مجتمع
Lec-7
د.ظافر
10/11/2015
Cancer
Different Kinds of Cancer
Carcinomas, arise from the cells that cover external and internal body
surfaces such as lung, breast, and colon.
Sarcomas, arise from cells found in the supporting tissues of the body
such as bone, cartilage, fat, connective tissue, and muscle.
Lymphomas, arise in the lymph nodes and tissues of the body's immune
system.
Leukemias are cancers of the immature white blood cells.
Loss of Normal Growth Control:
Cancer arises from a loss of normal growth control.
In normal tissues, the rates of new cell growth and old cell death are
kept in balance. In cancer, this balance is disrupted. This disruption can
result from uncontrolled cell growth or loss of a cell's ability to undergo
"apoptosis."
Apoptosis, or "cell suicide," is the mechanism by which old or damaged
cells normally self-destruct.

24
Carcinoma in Situ:
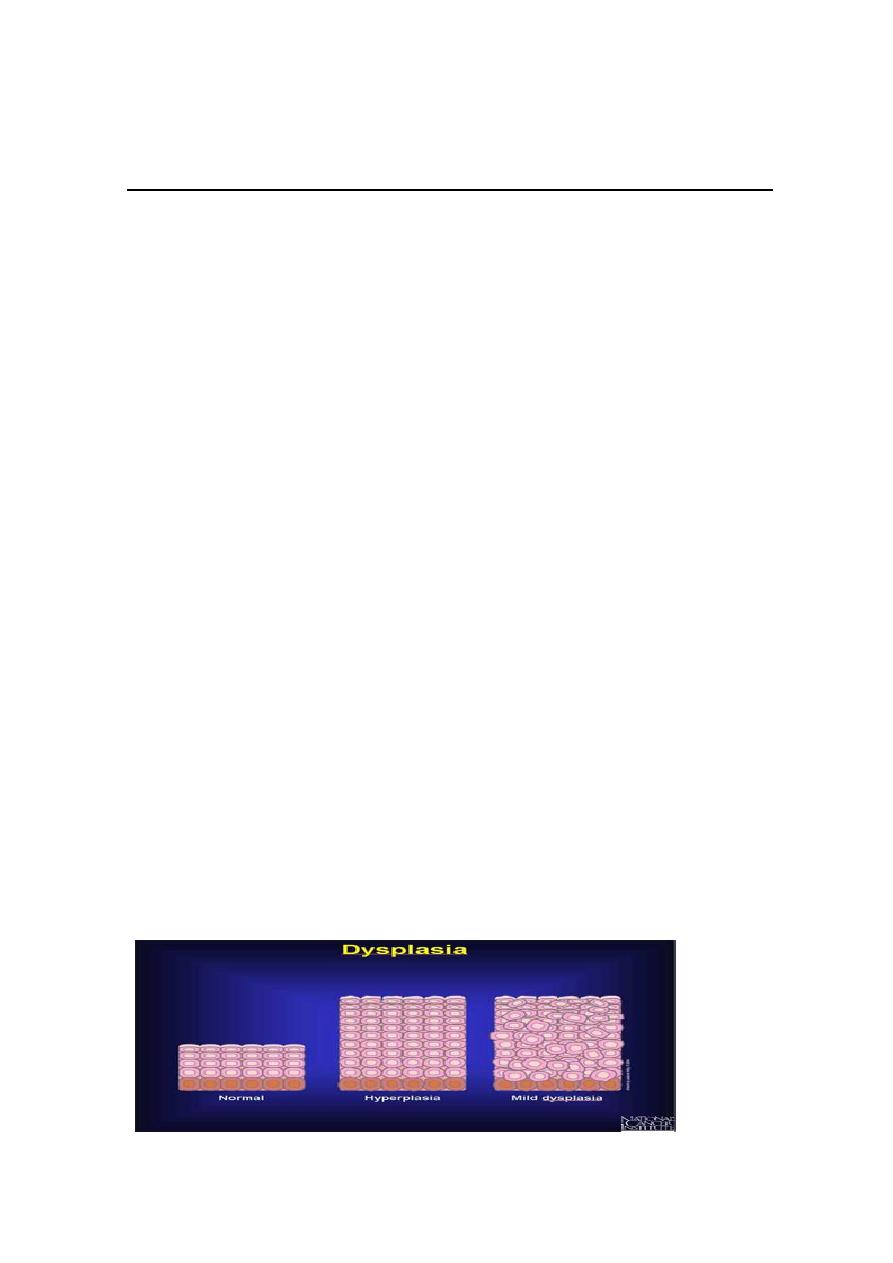
The most severe cases of dysplasia are sometimes referred to as
"carcinoma in situ."
In Latin, the term "in situ" means "in place“, so carcinoma in situ refers
to an uncontrolled growth of cells (tumor) that remains in the original
location.
Invasion and Metastasis (spread of cancer):
Cancers are capable of spreading throughout the body by two
mechanisms:
1. Invasion, refers to the direct migration and penetration by cancer
cells into neighboring tissues.
2. Metastasis, refers to the ability of cancer cells to penetrate into
lymphatic and blood vessels, circulate through the blood or lymphatic
stream, and then invade normal tissues elsewhere in the body.
25
Malignant versus Benign Tumors:
Benign tumors are tumors that cannot spread by invasion or metastasis;
hence, they only grow locally.
Malignant tumors are tumors that are capable of spreading by invasion
and metastasis. By definition, the term "cancer" applies only to
malignant tumors.
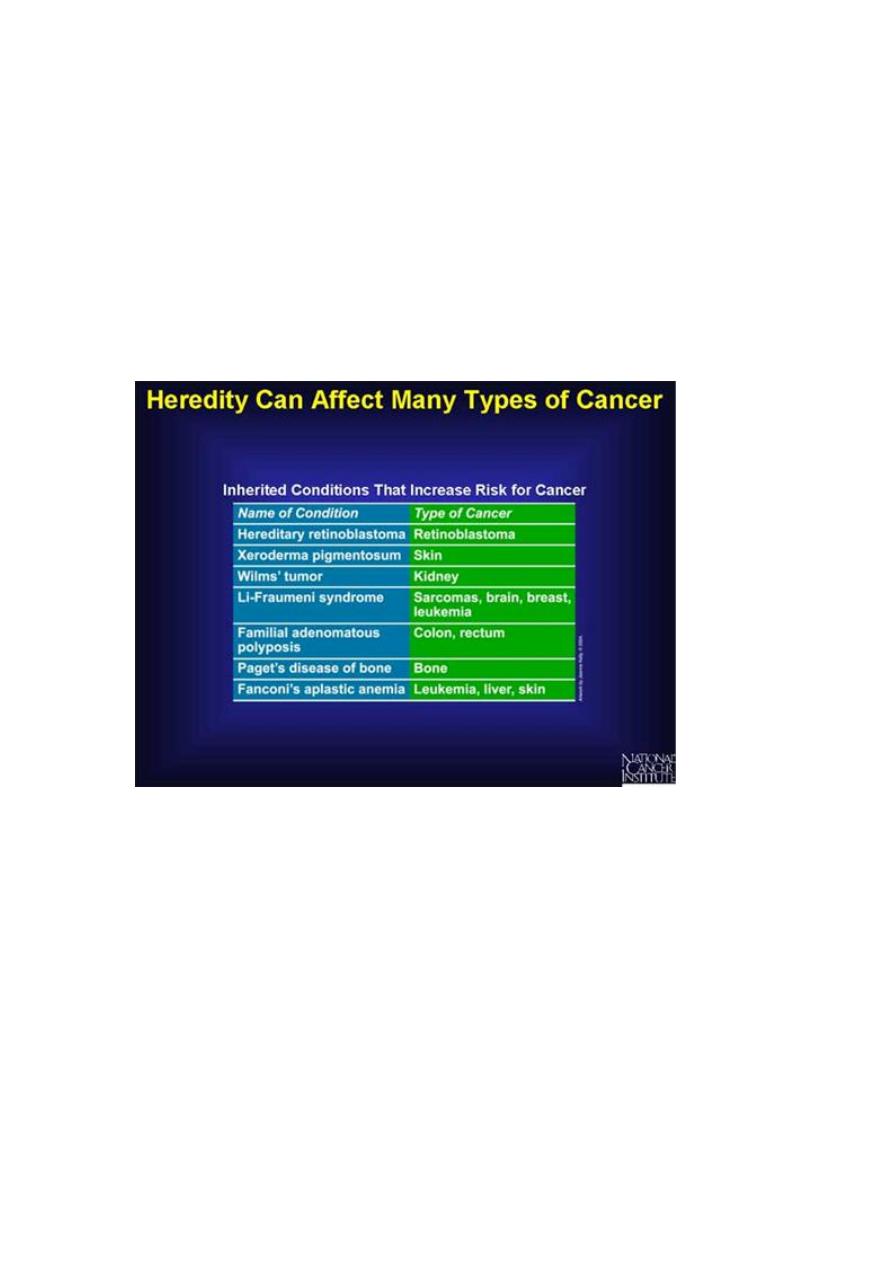
What Causes Cancer?
1. Intrinsic factors: such as heredity, diet, and hormones, behaviors,
lifestyle.
2. Extrinsic factors: such as chemicals, radiation, and biological.
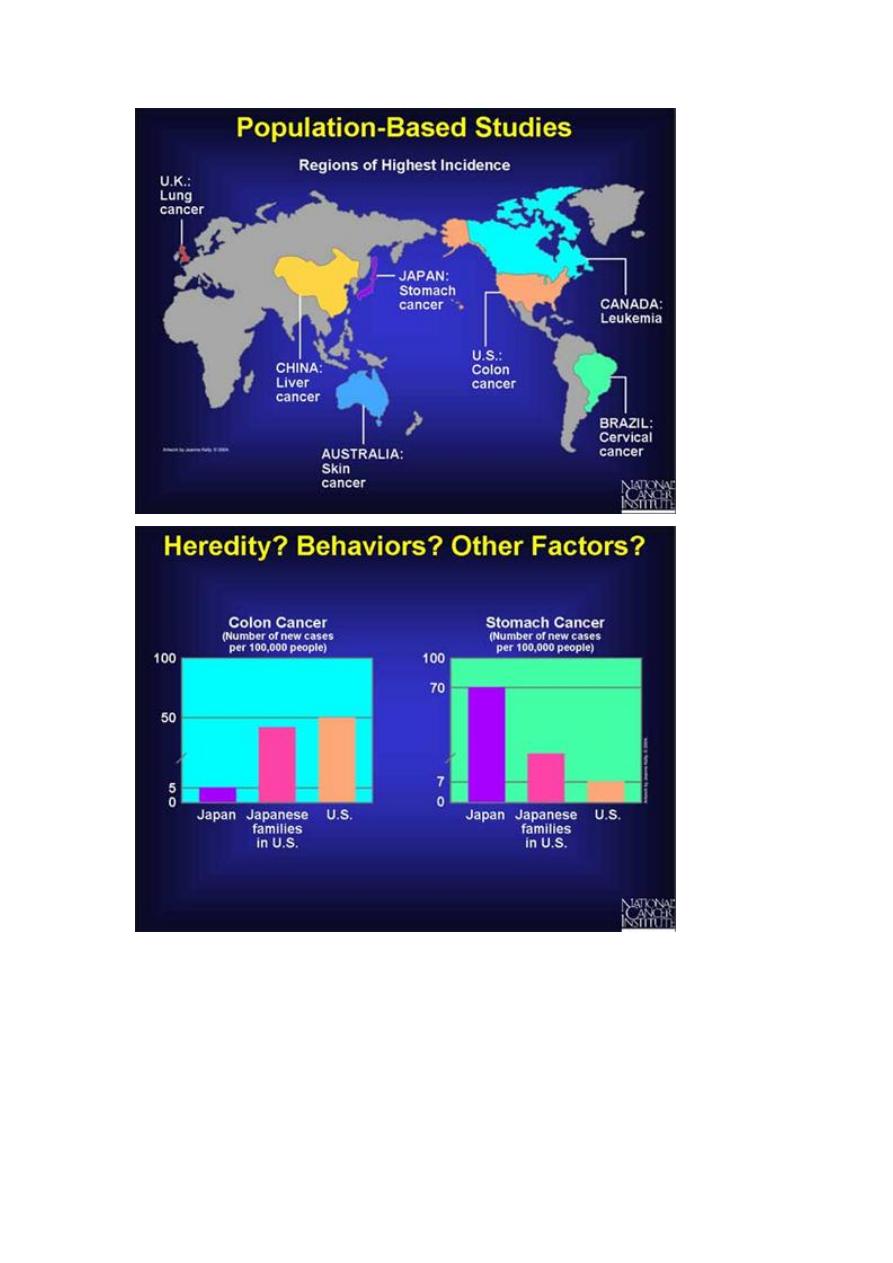
3. Multifactorial: in Japan, the rate of stomach cancer is higher, than in
the United States. But this difference has been found to gradually
disappear in Japanese families that have moved to the United States.
This suggests that the risk of developing cancer is not determined
primarily by heredity. The change in risk for cancer for Japanese families
could involve cultural, behavioral, or environmental factors.
26

27
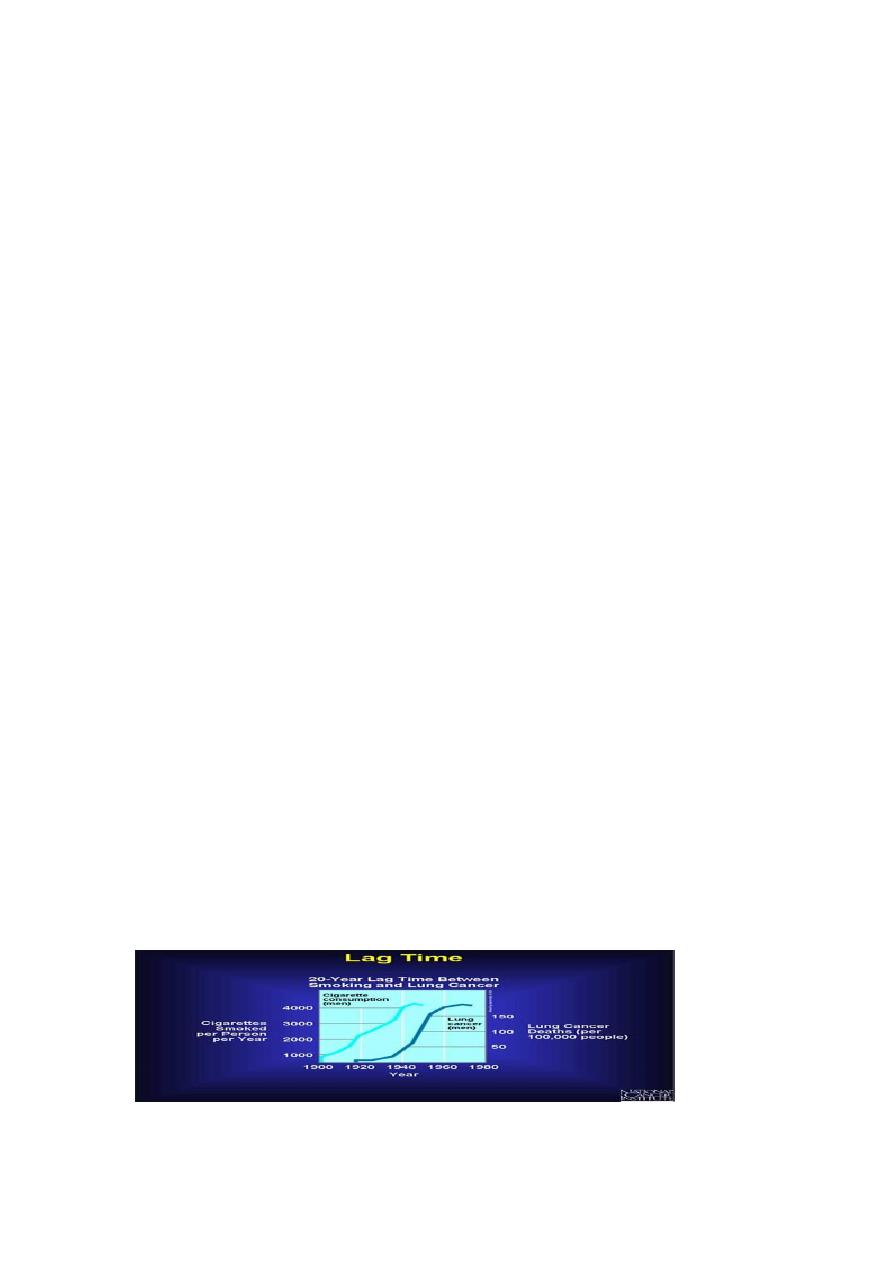
Tobacco Use and Cancer:
Tobacco smoking is the greatest public health hazard. Cigarette smoke
contains more than 24 different carcinogens.
Cigarette smoking is the main cause of lung cancer and contributes to
many other kinds of cancer as well, including cancer of the mouth,
larynx, esophagus, stomach, pancreas, kidney, and bladder.
Current estimates suggest that smoking cigarettes is responsible for at
least one out of every three cancer deaths, making it the largest single
cause of death from cancer.
Radiation:
Low-Strength Radiation (non-ionizing):
Prolonged or repeated exposure to ultraviolet radiation from sunlight is
a low-strength type of radiation that can cause cancer.
High-Strength Radiation (ionizing):
Such as X-rays or radiation emitted from unstable atoms called
radioisotopes. These two types of radiation are stronger than ultraviolet
radiation, they can penetrate through clothing and skin into the body..
Infection:
1. Viruses:
Few viruses that infect human cells actually cause cancer. viruses
implicated in cervical cancer (HPV), liver cancer (HBV), and certain
lymphomas (EBV), leukemias (HTLV), and sarcomas (KSAHV).
2. Bacteria:
The bacterium Helicobacter pylori, which can cause stomach ulcers.
3. Parasites.
28
Cancer Risk and Aging:
Because a number of mutations usually must occur for cancer to arise,
the chances of developing cancer increase as a person gets older (aging)
because more time has been available for mutations to accumulate.
Living more, means exposed more
For example, a 75-year-old person is a hundred times more likely to
develop colon cancer than a 25-year-old.
7 Warning signals (cancer societies education)
Change in bowel or bladder habits
A sore that does not heal
Unusual bleeding or discharge
Thickening or lump in the breast or elsewhere
Indigestion or difficulty in swallowing
Obvious change in a wart or mole
Nagging cough or hoarseness
CAUTION

29
Diagnosis of cancer:
1. Diagnosis of cancer is histopathological.
2. The importance of biological markers (BRCA1&BRCA2).
3. The importance of screening.
4. Early finding of cancer may decrease a person's risk of dying from the
cancer.
31
4th stage
طب مجتمع
Lec-8
د.ظافر
10/11/2015
Diabetes Mellitus
Introduction to Diabetes Epidemiology
Definition:
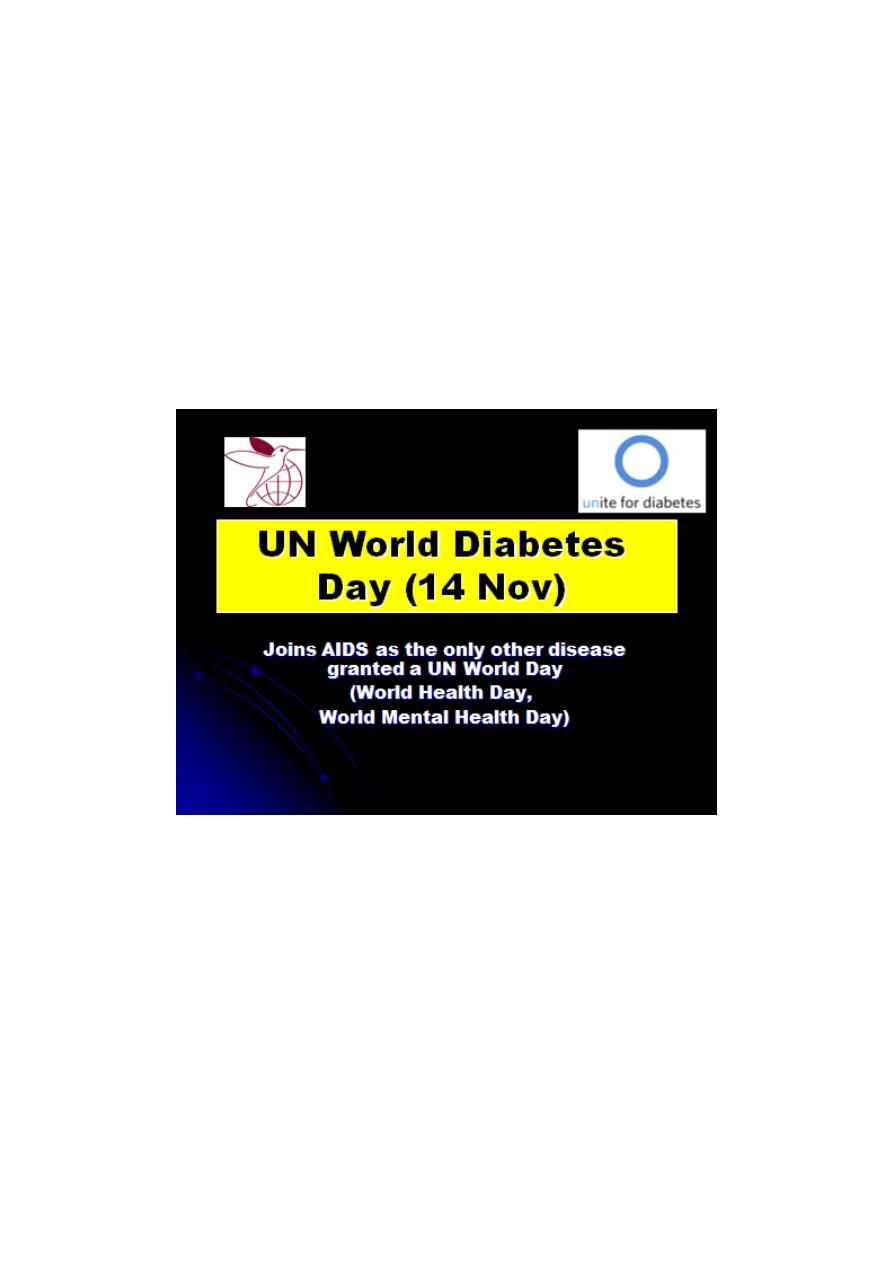
A metabolic disorder of multiple aetiology characterized by chronic
hyperglycaemia with disturbances of carbohydrate, fat and protein
metabolism resulting from one or more of the following:
1. Defects in insulin secretion (lack or absence).
2. Defects in insulin formation (structure or action).
3. Defects in insulin receptors (lack or abnormal).

31
Diabetes mellitus
Diabetes mellitus was well known in ancient times, long before scientists
and doctor began to investigate it
The main features of the disease were recognized at that time, and may
still be listed as:
1. Severe thirst
2. Excessive drinking
3. Frequent urination
4. Bodily wasting
Classification:
1. Diabetes Mellitus (DM):
i-Insulin dependant diabetes Mellitus (IDDM, Type 1)
ii- Non - insulin dependant diabetes Mellitus (NIDDM, Type 2)
iii- Malnutrition – related diabetes mellitus (MRDM)
iv- Other types (secondary to pancreatic, hormonal , drug induced,
genetics and other abnormalities)
2. Impaired glucose tolerance (IGT)
3. Gestational diabetes mellitus (GDM)
4. Metabolic syndrome.
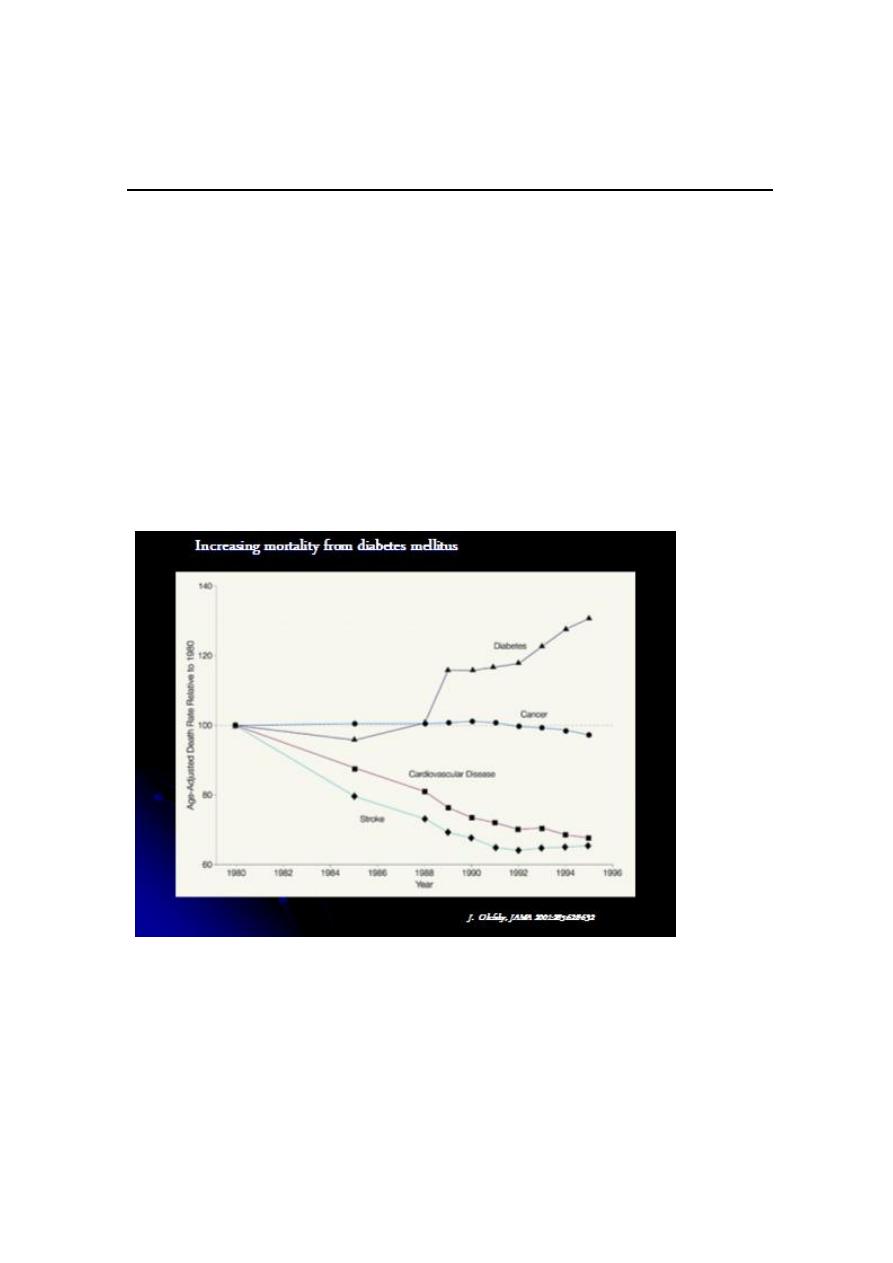
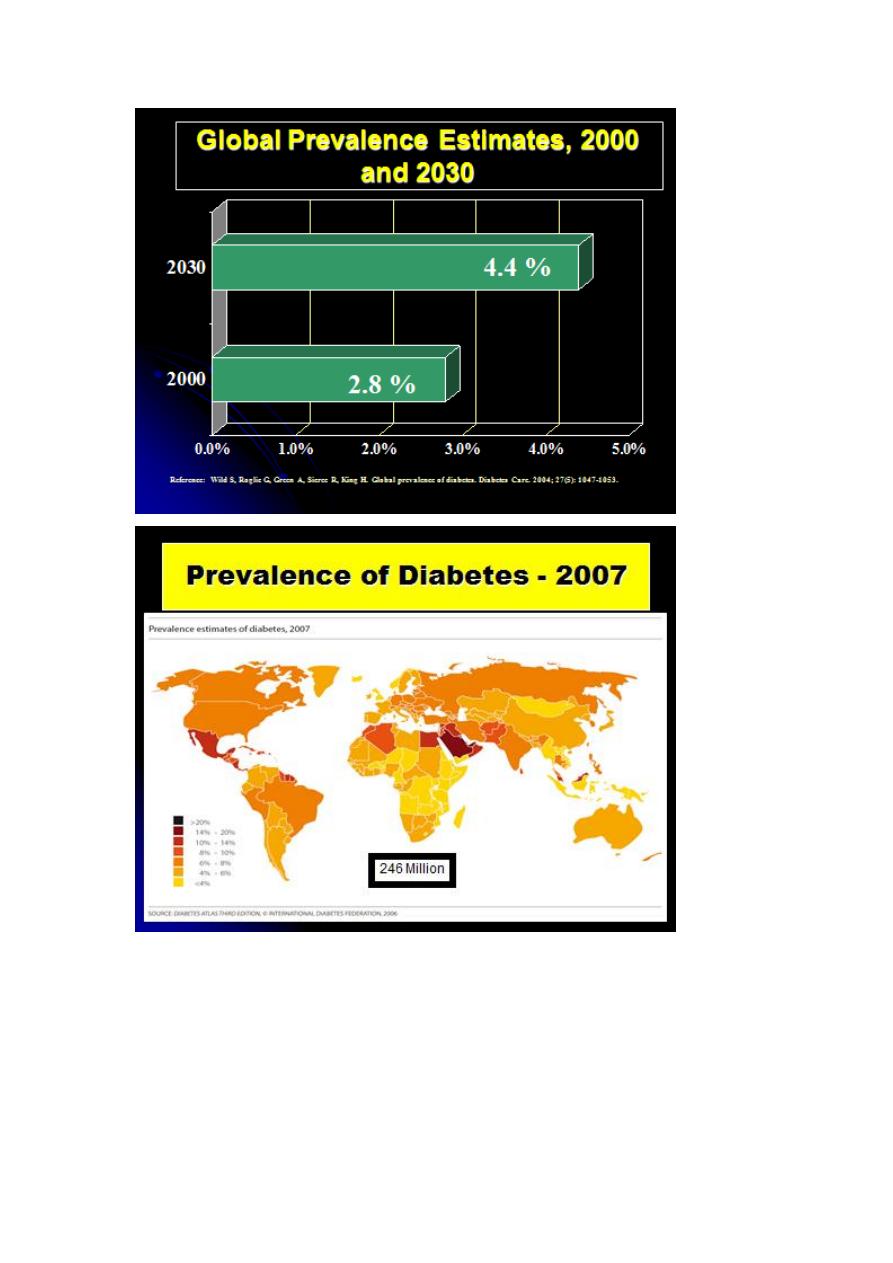
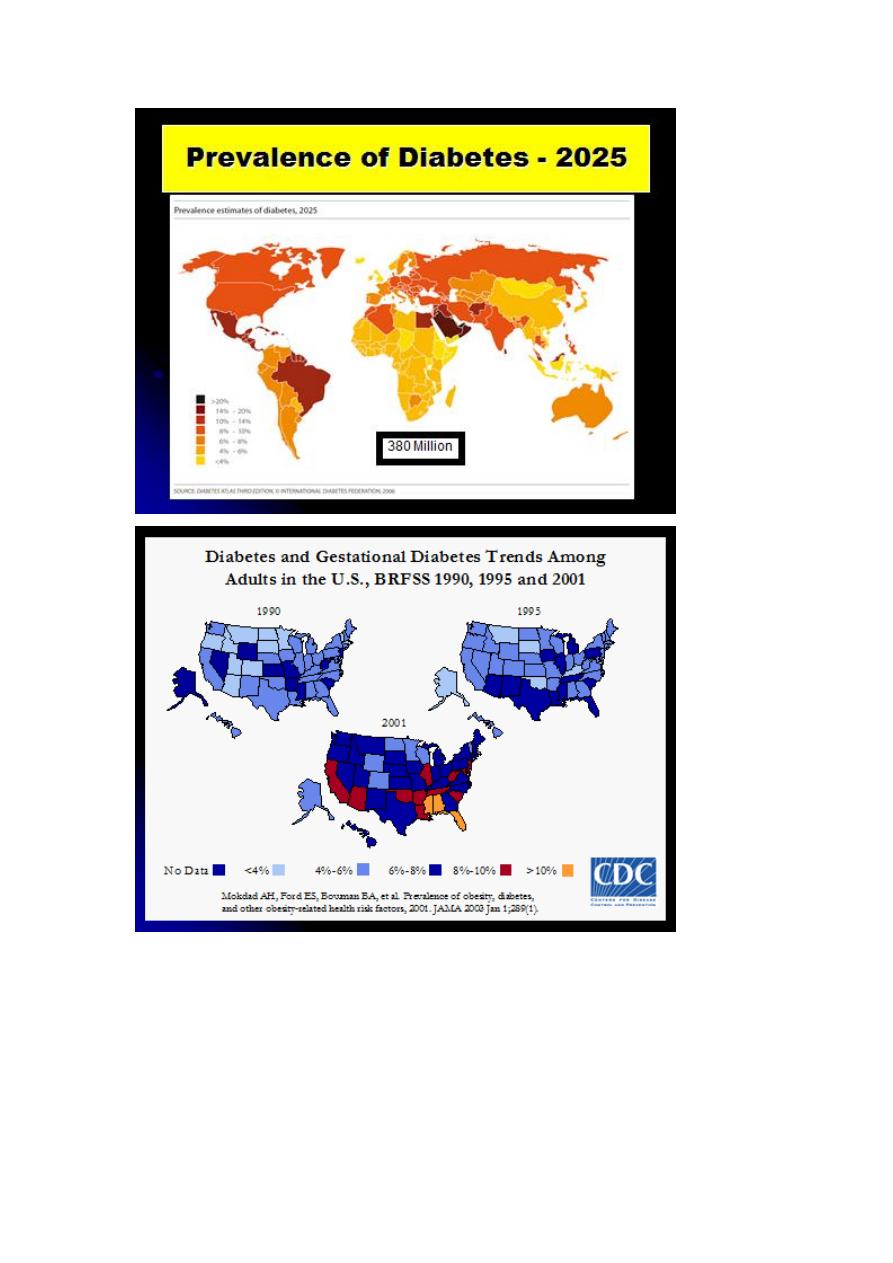
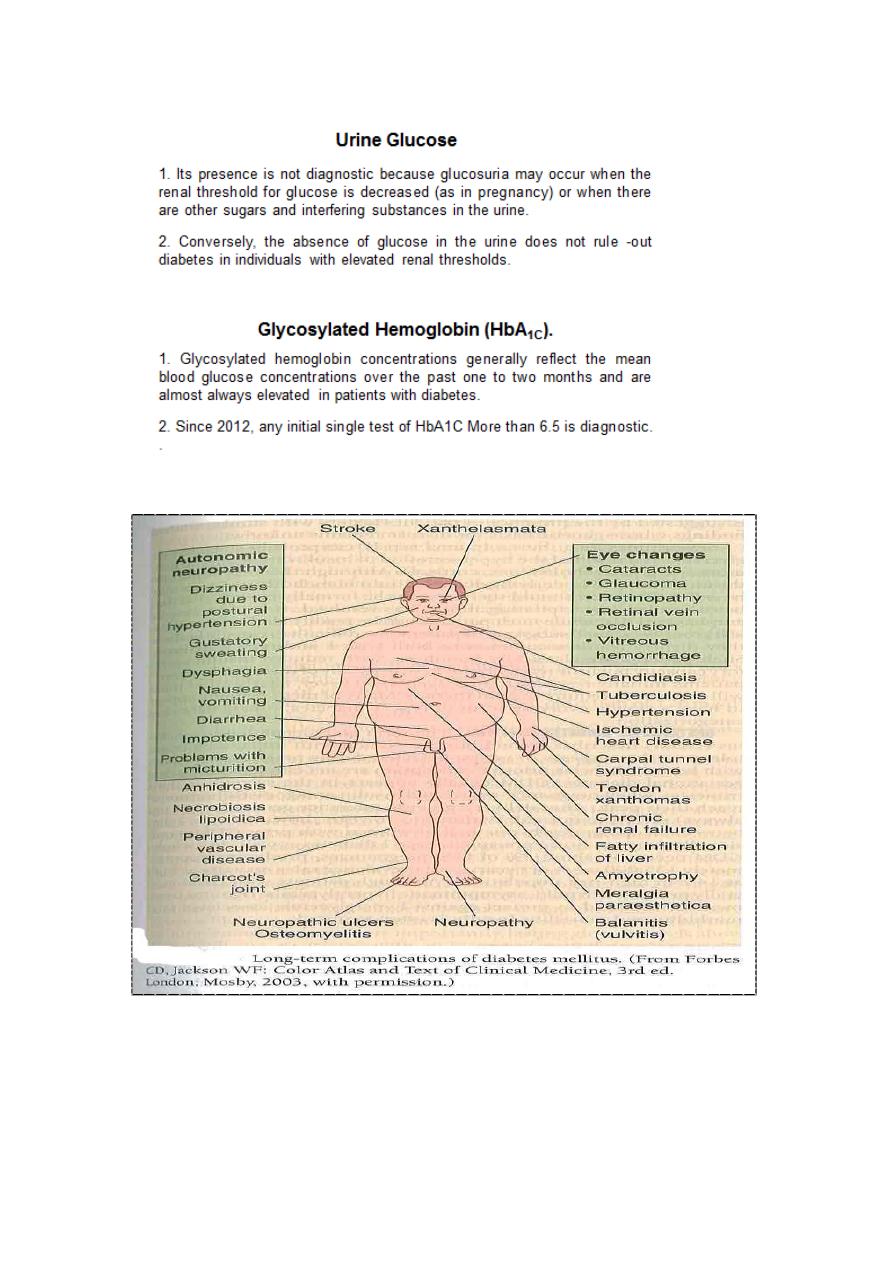
Epidemiology of diabetes
Prevalence worldwide is increasing*
2.8% in 2000; 4.4% in 2030 worldwide
171 million in 2000; 366 million in 2030
Greatest rise in developing world
32
33

34
35

36
Screening of diabetes:
1. Urine examination.
2. Blood sugar testing.
Target population (high-risk population):
1. > 40 years.
2. +ve family history.
3. Obese.
4. Women who have had a baby > 4.5 Kg.
5. Women who show excess weight gain during pregnancy.
6. Premature atherosclerosis.
Management of Diabetes:
1. Maintain blood glucose as close as possible to normal values (drug
therapy).
2. To maintain ideal body weight:
A- Diets.
B- Exercise.
3. Self care.
4. Blood glucose monitoring:
A- Glycosylated hemoglobin.
B- Home blood glucose monitoring.
C- Routine lab.
6. Having a pocket card.
37
By managing the ABCs of diabetes, people with diabetes can reduce
their risk for heart disease and stroke.
A stands for A1C
B stands for Blood pressure
C stands for Cholesterol
D stands for diet and lifestyle change
E stands for exercise
38
4th stage
طب مجتمع
Lec-9
د.ظافر
10/11/2015
Obesity
Definition: An abnormal growth of the adipose tissue due to an
enlargement of fat cell size (hyper-trophic obesity) or an increase in fat
cell number (hyper-plastic obesity) or a combination of both.
BMI > 30 for males and > 28.6 for females.
Prevalence: 20 -40 percent in adults and 10-20 percent in children in
developed countries.
Risk factors:
1. Age: Incidence increase with age, obese child usually → obese
adult,1/3 of obese adults were obese Childs.
2. Sex: Optimal age for obesity is 29-35 year in male and 45-49 in
female.
3. Genetic factor: Important.
4. Physical inactivity: Vicious circle, decrease expenditure of energy
more important than overeating.
5. Socio-economic status: Inverse relation now.
6. Eating habits: Between meals, more sugar, carbohydrates and fats
with low fibers.

39
7. Psychological factors: Depression, anxiety, loneliness and
frustration (vicious circle). (Secret eaters).
8. Familial tendency.
9. Endocrine factor: Cushing's syndrome, hypothyroidism and GH
deficiency.
Assessment of Obesity:
1. Body weight:
a. > 2 SD from median weight for height as a cut-off point for
obesity.
b. BMI = weight in kg / (height in meter)
2
.
2. Skin fold thickness: (Harpenden skin calipers) mid triceps, biceps,
scapular and supra-iliac skin. The sum of measurement should be
< 40 mm in males and < 50 mm in females.
3. Others.
4. WHR.

41
Hazards of Obesity:
1. An established risk factor in hypertension, IHD, accidents,
gallbladder diseases and diabetes. Nonetheless, even in cancers.
2. Varicose veins, abdominal hernias and OA of knee, hips, spine in
addition to flat feet.
3. Psychological abnormalities.
4. Increased risk from surgery.
5. Sleep apnea.
6. Lowered fertility.
7. Lowered life expectancy.
8. Establiehed risk factors in breast cancer.
Prevention:
1. Dietary changes.
2. Physical activity.
3. Others: surgery plus medicine.
41
Accidents
Definition:
"An unexpected, unplanned occurrence which may involve injury".
WHO definition:
unplanned event resulting in recognizable damage.
Important facts about accidents:
* Accidents represent a major epidemic of non-communicable disease.
They are no longer considered accidental and they are part of the price
we pay for technological progress.
* Accidents have their own natural history and follow the same
epidemiological pattern as any other disease (Interaction between host,
agent and environment).
* Accidents occur more frequently in certain age groups, at certain
times, and at certain localities.
* Certain people are more prone to accidents; alcohol, drugs,
physiological and psychological states increase their susceptibility.
* The majority of accidents are preventable.
* Accidents allover the world, they rank the fourth among the ten
leading causes of deaths, leading to 7.5 per cent of deaths in both

42
developed and developing countries. About 4 million of deaths allover
the world is due to accidents (only one million is due to intentional
injuries).
Types of accidents:
1. Road traffic accidents: Accounts for about 1 million of deaths
allover the world annually, and for each death, there will be 30-40
minor injuries, and 10-15 serious injuries (disabilities). Mean ages
affected are 15-24 years.
2. Domestic accidents: Affects both extreme of ages and the most
common causes are;
-
Drowning.
-
Burns.
-
Poisoning.
-
Falls.
-
Injuries from sharp and pointed instruments.
-
Bites and other injuries from animals.
3. Industrial accidents: Thousands workers are died and many
others are injured and crippled.
4. Passenger's accidents: Railways, airplanes, ships etc.
5. Burns: 10 per cent of all accidental deaths are due to burns.
6. Wars and Terrorist actions.
Causation of accidents: Multiple
1. Human 90 per cent.
2. Environmental 10 per cent.

43
Prevention of accidents:
1. Data collection.
2. Safety education.
3. Promotion of safety measures: Such as safety belts, safety
helmets, leather clothing and boots, Children protection and
others.
4. Alcohol and other drugs.
5. Primary cares.
6. Elimination of causative agents.
7. Enforcement of laws.
8. Rehabilitation of services: Such as medical, social and
occupational.
9. Accidents researches (accidentology).
THE ELDERLY (Geriatrics):
Aging is a natural process.
Actually, the modern physician cannot heal an old age, but can protect,
promote and extend it.
Thus, old age should be regarded as a normal, inevitable biological
phenomenon.
Size of the problem:
Worldwide, the population aged 60 or over is expected to be more than
double from 500 million in 1990 to about 1.2 billion by the year 2035
and 72 per cent will be living in developing countries.
Most of this growth is expected to be in Africa, Asia

44
Throughout the world, the "oldest old" (aged 85 or older) are the most
rapidly increasing age group among the older population.
The oldest elderly require a lot of proper health and social services. The
majority will be women, and many are living alone.
CULTURAL VIEWS FOR THE ELDERLY:
The Western society, with its emphasis on youth, productivity,
individualism, autonomy and self-control, is often quite intolerant of old
people. Those societies that have entered the information age of
computers, global telecommunications and artificial intelligence give an
increased cultural importance to the brain.
In non-Western cultures, the elders are considered the living store of
oral history and ancient traditions; of cultural mores, beliefs, myths, and
ritual expertise.
In addition to that, certain religious guides are seriously intended for the
care of elderly and regarded that as one of the priorities of moral and
religious values.
HEALTH PROBLEMS OF THE AGED:
I- Problems due to the Aging Process:
Senile cataract, glaucoma, nerve deafness, bony changes affecting
mobility (such osteoarthritis), emphysema, failure of special senses, and
changes in mental outlook.

45
II- Problems Associated with Long-Term Illness:
1. Degenerative diseases of heart and blood vessels.
2. Cancer.
3. Accidents.
4. Diabetes.
5. Diseases of locomotor system: articular and non-articular diseases
such as fibrositis, myositis, neuritis, gout, rheumatoid arthritis,
osteoarthritis, spondylitis of spine, etc.
6. Respiratory illnesses: such as chronic bronchitis, asthma, and
emphysema.
7. Genitourinary problems: Enlargement of prostate, dysuria, nocturia,
frequent and urgency of micturition are common complaints among
elderly.
III- Psychological Problems:
1. Mental changes: Such as impaired memory, rigidity of outlook, and
dislike of changes.
2. Sexual adjustment:
3. Emotional disorders: "bitterness", inner "withdrawal", "depression“
and even "suicide".
