RadioLoGY
lecture
7
+8
جامعة بغداد
–
كلية الطب
PLAIN ABDOMEN + ESOPHAGUS
STOMACH AND DUODENUM
ؤيد
م بتكم
MUSTAFA laith
Dr Laith
1
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
GIT RADIOLOGY
Plain abdomen
Plain means without contrast.
The standard films are supine & erect AP views (alternative to erect, lateral
decubitus film is used in ill patients).
The stomach can be readily identified by its location, gastric rugae in supine
patient & by the air-fluid level beneath the left hemidiaphragm in erect patient.
The duodenum contains air usually & show air-fluid level. In the small bowel,
gas is rarely sufficient to outline the whole of a loop. Short fluid levels in the small
& large bowel are normal.
Short fluid levels in the small & large bowel are normal.
STANDARD VIEWS:
1. Erect abdomen.
2. Supine anteroposterior position.
3. Lateral decubitus (in ill patients).
How to look at plain abdominal film:
Look for any dilated loops of bowel & try to decide the dilated portion.
Look for any gas outside the bowel.
Locate any calcifications (if any).
Look for ascites or soft tissue masses.
Assess the size of the liver & spleen.
2
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Dilatation of bowel
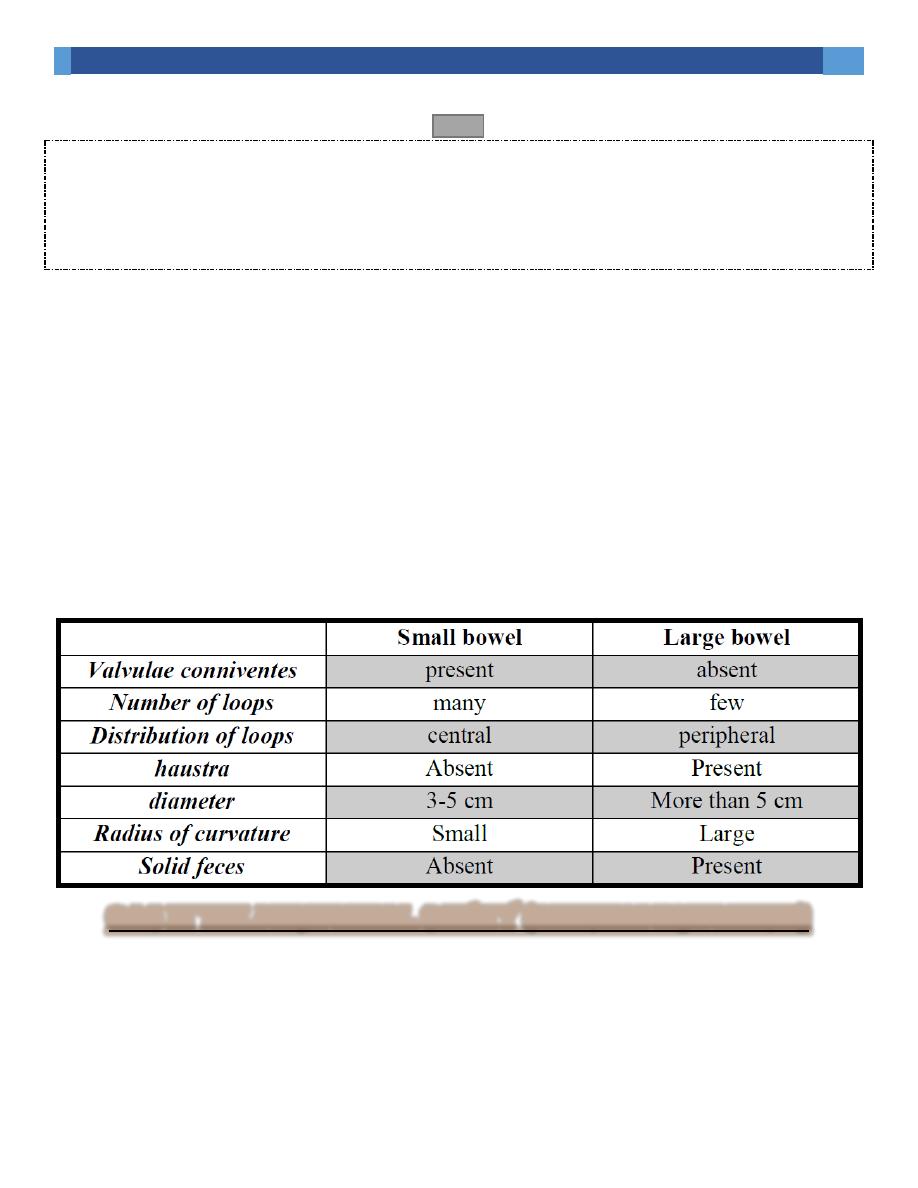
Colonic haustra (usually seen in the transverse & ascending colon) form
incomplete bands across colonic gas shadows.
Small bowel (SB) valvulae conniventes (noted in dilated jejunum) are closer than
haustra & cross the width of bowel (stack of coins). Remember that the sigmoid
& ileum are smooth & may be similar.
The radius of curvature; when tighter, it suggests a dilated small bowel loop.
The presence of fecal material is reliable indicator of the position of the colon.
The small bowel usually lies centrally while the large bowel lie peripherally
(remember that the transverse & sigmoid colon may lie centrally when dilated).
Numerous layered loops are often seen in small bowel dilatation, but not present
in large bowel (LB) dilatation.
Causes of dilatation:
1. Mechanical SB obstruction: small bowel dilatation with normal or reduced caliber
of colon.
2. LB obstruction: dilated colon to the point of obstruction +/- SB dilatation (if the
ileocecal valve is incompetent).
3. Paralytic ileus: SB & LB dilatation (gas may be present in the rectum).
4. Local peritonitis: dilatation of loops adjacent to inflammation.
5. Toxic dilatation of the colon (in ulcerative colitis & rarely in Crohn's disease):
distended LB especially the transverse colon (diameter > 6 cm) with grossly
abnormal haustra or absence of haustration.
3
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
6. SB infarction may mimic both SB & LB obstruction.
7. Closed loop obstruction (if contains air), it is seen in a characteristic shape e.g.
cecal or sigmoid volvulus.
NB: Patients with gastroenteritis may have normal film, or show excessive fluid
levels with or without dilatation (mimicking paralytic ileus or SB obstruction)
In summarization:
Diameter
Loop of curvature
Number of loops
Valvulae conniventes/haustra
Location
Fecal material Small bowel Large bowel Valvulae conniventes present absent
Gas in the peritoneal cavity (pneumoperitoneum)
Is almost always due to GIT perforation or follows surgical intervention in the
abdomen.
The most common cause of spontaneous pneumoperitoneum is a perforated peptic
ulcer & 2/3 of such cases are recognizable radiologically.
4
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Largest pneumoperitoneum occurs in colonic perforation & smallest in SB
perforation & very rare in perforated appendicitis.
Pneumoperitoneum is seen as air under the right hemidiaphragm on an erect
abdominal film or CXR, but air under the left hemidiaphragm is more difficult to
identify because of overlying gastric & splenic flexure gas.
CXR is preferable to erect plain abdominal film & sometimes lateral decubitus
film is required to confirm the presence of pneumoperitoneum (collected beneath
the flank).
Post-operatively, pneumoperitoneum is normal finding (even after laparoscopy).
In adults, it will absorb with 7 days & in children within 1 day. An increase in
amount of air on successive films indicates leakage.
Gas in an abscess
May form either small bubbles or larger collections of air (both can be confused
with bowel gas). Fluid levels may be seen on a horizontal ray film. Abscesses may
displace adjacent structures (e.g. elevation of a hemidiaphragm in subphrenic
abscess & bowel displacement in pericolic & pancreatic abscesses).
Pleural effusion or pulmonary collapse/consolidation occur in subphrenic abscess.
US, radionuclide examination & CT are used in evaluating abdominal abscesses.
Gas in the bowel wall
Oval gas bubbles in bowel wall are seen in pneumatosis coli,
Linear streaks of intramural gas usually indicate bowel infarction.
If noted in the neonatal period is diagnostic of necrotizing enterocolitis.

5
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Gas in biliary tree
Following sphincterotomy
Anastomosis of CBD to bowel
Also seen in fistula from erosion of GB stone into duodenum or colon or following
penetration of DU into CBD.
Occasionally, gas may be seen in the wall or lumen of GB in acute cholecystitis
from gas-forming organisms.
Ascites
X-ray cannot detect small amount, while large amount will separate bowel loops
& displace the ascending & descending colon from fat stripes. SB loops float to
the center of abdomen.
Ascites is more readily recognized with ultrasound or CT.
Abdominal calcifications
Localize the calcifications using a lateral or oblique view.
Assess the pattern & shape of calcification to limit the diagnosis.
Causes:
1. Pelvic vein phleboliths may be mistaken for urinary stones & faecoliths.
2. Calcified mesenteric LN: as in TB causing irregular calcification & very dense
& are often mobile.
3. Vascular calcification e.g. aortic aneurysm (easier to be assessed on lateral film).

6
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
4. Uterine fibroids: spherical outline & contain numerous irregularly shaped well
defined calcifications.
5. Soft tissue calcification in buttocks e.g. after injection of certain medicines.
6. Malignant ovarian tumors occasionally contain visible calcification. Dermoid
cyst may contain teeth.
7. Adrenal calcification: e.g. after hemorrhage, TB, adrenal tumors. Minority of
patients with Addison disease show adrenal calcifications.
8. Liver calcification: hepatomas, hydatid cyst, abscess, TB.
9. GB stones.
10. Splenic calcifications: in cysts, infarcts, old hematomas, & TB.
11. Pancreatic calcifications: in chronic pancreatitis & diagnosed from its
position.
12. faecolith: in colonic diverticulae or in the appendix (indicating the presence of
acute appendicitis)
13. Urinary stones & other renal calcifications.
Role of plain abdominal x-ray:
1- Baseline for surgical preparation.
2- For detection of air under the diaphragm.
3- For patient with chest condition that may present with abdominal complaint.
4- For patient with acute abdomen.

7
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Plain films of liver & spleen
As the liver enlarges, it will displace the hepatic flexure, transverse colon & right
kidney downwards & the stomach to the left & the diaphragm may be elevated.
As the spleen enlarges , the tip may be visible in the left upper quadrant below the
lower ribs, eventually may fill the left abdomen & may extends to the right lower
quadrant displacing the splenic flexure , left kidney & stomach.
OTHER IMAGING MODALITIES
Contrast studies.
Ultrasound.
CT scan (with and without contrast).
MRI (with and without contrast).
Advantages of CT scan
1- Show the whole width of bowel wall.
2- Easier than either endoscopy or BA enema.
3- Very rapid.
4- Multiplanar (With modern scanners).
5- Lumen evaluation with contrast (gastrograffin or air).
6- Virtual colonoscopy possible.
Role of CT scan
1- Diagnosing and staging tumor.
2- Assessing the complications of GI disease and surgery.
3- Confirm or exclude appendicitis and intestinal obstruction.
4- Bowel trauma.
Role of Ultrasound
1- US can assess bowel wall.
2- Ascites
3- Infantile pyloric stenosis
4- Intussusception

8
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
5- Suspected appendicitis
5- Endoscopic ultrasound to assess the depth of invasion of tumors in bowel wall
and in diagnosing tumors of pancreas.
Role of MRI
1- MRI has a limited role in GIT disease.
2- Currently its major use for:
a. Assessing local spread of rectal cancer.
b. Assessing perianal fistula and abscess.
Abdominal & pelvic masses
US, CT or MRI are the appropriate imaging modalities.
The site, displacement of adjacent structures& calcifications are the radiographic
signs of a mass, but it can not differentiate between solid & cystic masses.
Examples: enlarged bladder, uterine, ovarian enlargement can be seen as a pelvic
mass displacing the bowel.
Retroperitoneal tumors & LN may become visible on plain films & may mask the
psoas outlines.
Renal masses & hydronephrosis can appear as masses in the flank.

9
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Contrast
Imaging techniques-General principles:
Contrast examinations
Endoscopy is often the first investigation, because it shows mucosal lesions
directly and also allows biopsy material to be obtained.
Barium sulphate is the best contrast for GIT (with good mucosal coating &
excellent opacification & being inert); its disadvantage is that it may impact
proximal to colonic or rectal stricture.
Water-soluble contrast media (e.g. gastrograffin) are the other available agents.
Gastrograffin is hypertonic (soon become diluted), less radio-opaque & irritant if
enter the lungs. Its major uses are GIT perforation, immediate post-operative
examinations, in specific conditions in pediatric patients & for GIT opacification
prior to CT of the abdomen.
Contrast examinations are carried out under fluoroscopic control (so that only
constant narrowing is filmed while peristaltic waves are transitory & not filmed).
Double contrast are the standard techniques used in contrast studies, where the
mucosa is coated with barium & the lumen is distended by air , often in
combination with an injection of smooth muscle relaxant.
NOTEs: the barium study of Esophagus is called (Barium Swallow), of stomach
(Barium Meal), of small intestine (Barium Follow-through), of large intestine
(Barium Enema)
Air + barium = double contrast

11
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
We don’t give barium in solid obstruction (if partial obstruction, it will go
complete) and in perforation (it will cause peritonitis)
In anastomosis leak we give water-soluble media.
In CT scan, double contrast means (oral + IV).
CT scan (also ultrasound) is very sensitive to uric acid stones, calcium and
appendicitis.
PET (positron emission tomography): Very sensitive to metastases. Also can
differentiate between Lymph node enlargements whether benign or malignant.
ALGOARITHM IN GIT INVESTIAGTIONS
Barium swallow Endoscope (with or without biopsy), Endoscopic
Ultrasound EUS CT Scan PET
In EUS we can see all the layers of the tract (mucosa, submucosa, muscularis
propria and serosa or adventitia in esophagus)
Terms used in reporting contrast examinations:
Mucosal pattern is the appearance of the inner surface of bowel. Abnormalities
of mucosal pattern can be categorized as abnormal smoothing (of the mucosal
folds) or abnormal irregularity.
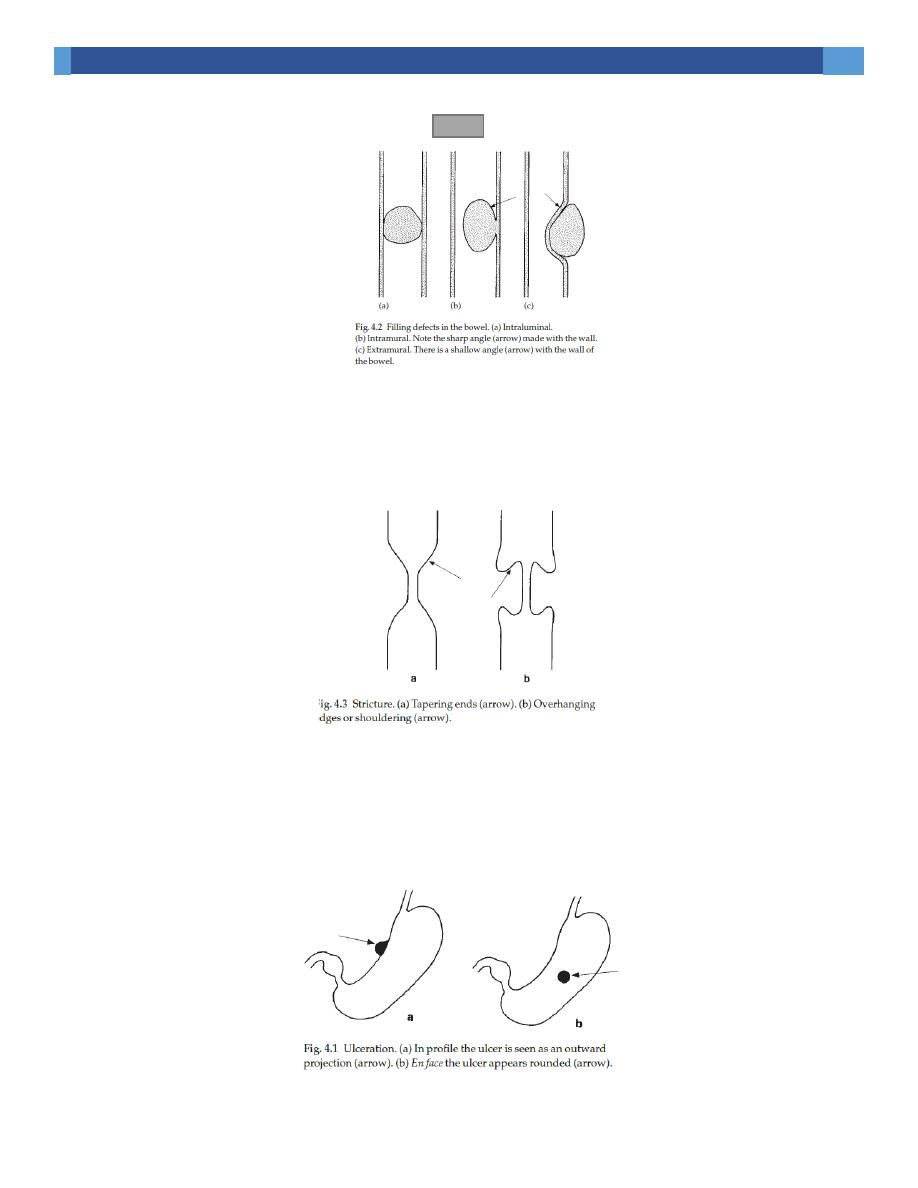
Filling defect is used to describe any process occupying space within the bowel
resulting in an area of total or relative radiolucency within the barium column.
1. An intraluminal filling defects has barium all round it e.g. food.
2. an intramural filling defects cause indentation from one side only forming a
sharp angle with the bowel wall & is not completely surrounded by barium e.g.
Ca colon.
3. Extramural filling defects causes narrowing from one side only forming a
shallow angle with the bowel wall, the mucosa is preserved but stretched over
the filling defect e.g. enlarged pancreas or LAP.
11
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Stricture is circumferential or annular narrowing (it must be differentiated from
peristaltic waves); it may have tapered ends or abrupt end (or shouldering).
Shouldering is an important radiological sign of malignancy.
Ulceration becomes visible when the crater is filled with barium. En profile, it
appears as an outward projection from the lumen & en face, the ulcer appears as a
rounded collection of barium.

12
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
CT, MRI & US examinations
CT show the whole width of bowel wall & used for diagnosing (especially in
elderly where Ba enema & endoscopy may be unpleasant) & staging tumors & for
assessing the complications of GI disease & surgery. It can be used to confirm or
exclude appendicitis, intestinal obstruction & in bowel trauma.
MRI has a limited role in GIT disease, its major use is for assessing the local
spread of rectal cancer & assessing perianal fistula & abscess formation.
Ultrasound can assess bowel wall & detect ascites (not the mucosa), can also be
used for the diagnosis of infantile pyloric stenosis, intussusception & suspected
appendicitis. Endoscopic US is used to assess the depth of invasion of tumors in
bowel wall & in diagnosing tumors of pancreas.
Oesophagus
Plain films may show dilated oesophagus in achalasia & may show opaque
foreign bodies
On Ba swallow, the barium-filled oesophagus has a smooth outline but when
empty, the barium lies in between mucosal folds (3-4 folds).
The aorta impresses the left side of oesophagus (more prominent in elderly).
Below the aortic impression, the left main bronchus makes a small impression.
The lower oesophagus is closely applied to the back of the left atrium & left
ventricle.
13
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Peristaltic waves are observed during fluoroscopic control. Sometimes the
contraction waves may not occur in an orderly fashion but are more pronounced
& prolonged so that the oesophagus has an undulated appearance (tertiary
contraction).
Indications of Ba swallow
1. Swallowing disorders
2. Oesophageal strictures
3. Assessing reflux.
Strictures:
When faced with a stricture, try to answer the following:
Where is the stricture?
What is its shape?
How long is it?
Is there a soft tissue mass?
Carcinoma may form an irregular stricture with shouldered edges of several
centimeters. A soft tissue mass may be visible.
CT may show thickening of wall, mediastinal invasion, LAP, liver &
pulmonary metastases.
Endoscopic US to assess the depth of invasion & assist Endoscopic biopsy &
can be used to assess involvement of paraoesophagal LAP.
14
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Peptic strictures found at the lower oesophagus +- hiatus hernia & reflux &
are characteristically short & have smooth outline with tapered ends. There may
be an ulcer close to stricture.
Achalasia produces a smooth, tapered narrowing at the lower end of
oesophagus +/- oesophageal dilatation & absent peristaltic waves with food
residue. The lungs may show consolidation & bronchiectasis (due to
aspiration). The stomach bubble is usually absent.
Corrosive strictures are long strictures begin at the level of aortic arch. It is
usually smooth with tapered ends but may be irregular.
Filling defects
1. Intramural filling defects
1. Lieomyoma cause a smooth, rounded indentation & a soft tissue mass
may be seen indicating extraluminal extension.
2. Carcinoma may cause irregular filling defect, but usually causes stricture.
2. Extramural filling defects
E.g. Ca bronchus, mediastinal LAP & aortic aneurysm.
An anomalous right subclavian artery (arising from aortic arch) give rise
to a characteristic short smooth narrowing as it crosses behind the oesophagus.
3. Intraluminal filling defects e.g. food impaction behind a stricture.
15
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Dilatation
obstruction & visible stricture e.g. achalasia.
Disease of smooth muscle e.g. scleroderma.
Varices
Appears as lucent, tortuous, wormlike filling defects on barium swallow
which distorts the mucosal pattern.
Web
Thin shelf like projection arising from the anterior wall of cervical
oesophagus. The oesophagus must be filled with barium to be demonstrated
It can be isolated finding or as part Plummer-Vinson syndrome (anemia,
web, dysphagia & iron deficiency anaemia).
Diverticulae
Are saccular outpouchings
Zenker's diverticulum arises through a congenital weakness in inferior
pharyngeal constrictor & lie behind the oesophagus & can displace or compress
the oesophagus.
Oesophageal atresia
A plain abdominal film will show air in the bowel (if there is a fistula between
the trachea & oesophagus)
16
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
The diagnosis is made by passing a tube that holds up or coils in a blind ending
pouch. Contrast examination may be dangerous in cases of spillage to the
trachea.
Candidiasis
Causes mucosal ulceration seen as fine irregularities projecting from the lumen.
Further Reading: ADOPTED FROM ARMSTRONG
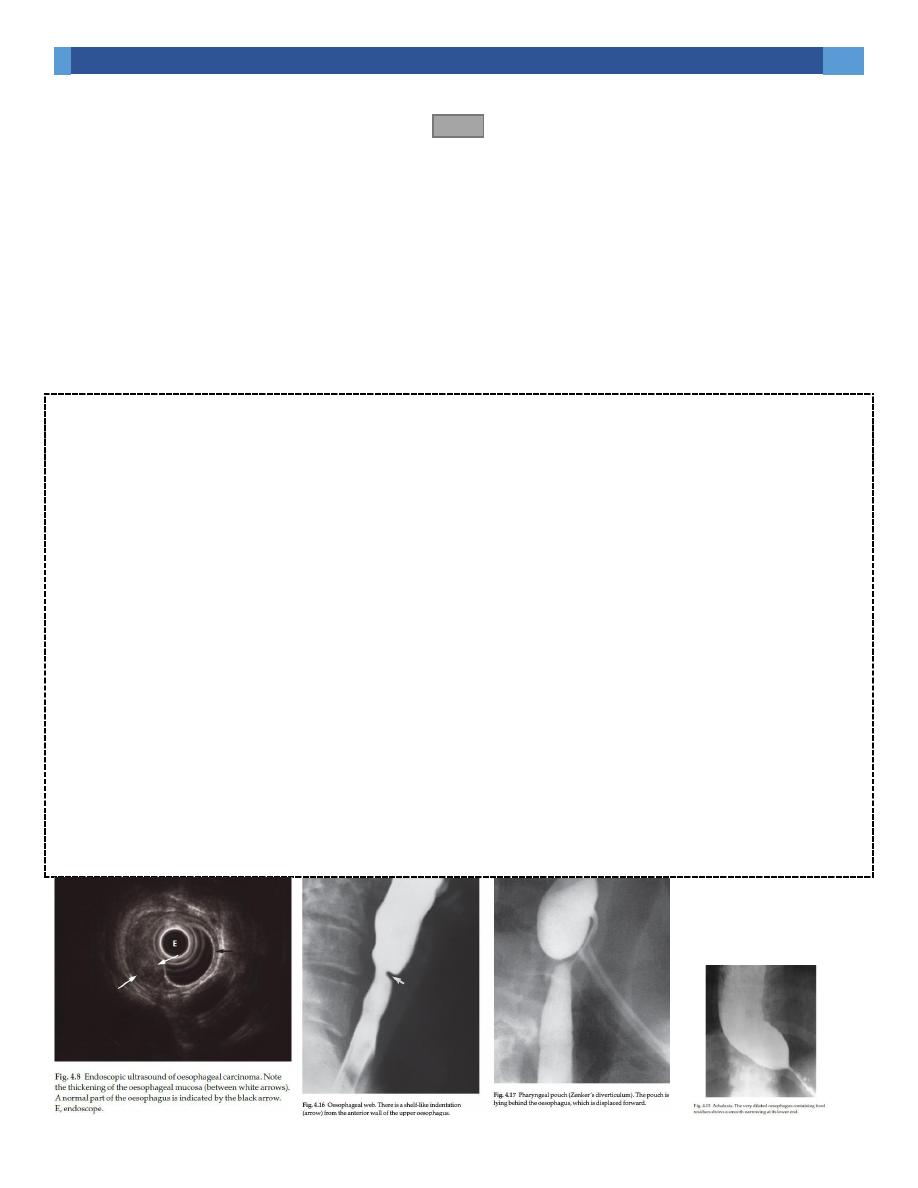
Oesophageal carcinoma is usually first diagnosed at upper GI endoscopy or barium swallow and the
diagnosis is confirmed by biopsy at endoscopy. Carcinomas usually involve the full circumference of
the oesophagus to form a stricture, which can be readily demonstrated at barium swallow
examination. It may occur anywhere in the oesophagus, shows an irregular lumen with shouldered
edges and is often several centimetres in length (Fig. 4.7). A soft tissue mass may be visible.
Assessing the extent of the tumour is carried out by endoscopic ultrasound and CT examination.
Endoscopic ultrasound (EUS) is able to demonstrate the layers of the oesophageal wall and the
surrounding lymph nodes.
Oesophageal cancer is seen as a hypoechoic mass and the depth of invasion of the tumour into the
oesophageal wall may be assessed (Fig. 4.8). Endoscopic ultrasound may also be used to assess
involvement of regional lymph nodes; EUS is highly
accurate in the local staging of early cancers but is limited when the endoscope does not fit into the
lumen of a narrow tumour stenosis. CT is performed following an intravenous smooth muscle
relaxant while swallowing water. The tumour is seen as a thickening of the oesophageal wall and the
length of the tumour can usually be assessed (Fig. 4.9). CT may also show invasion of the
mediastinum or adjacent structures, evidence of metastatic spread to lymph nodes, liver or lungs
(Fig. 4.10). The role of MRI in staging oesophageal carcinoma is under investigation. Assessment of
response to treatment and follow-up of patients with carcinoma of the oesophagus is usually done
with CT.
FDG-PET or FDG-PET/CT is used to determine the presence of metastatic disease in selected cases
and has a higher accuracy than CT in the detection of distant metastases (Fig. 4.11).
17
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
The stomach & duodenum
In centers with expert endoscopy, indications for Ba meal are:
1- Failed gastroscopy.
2- Duodenal strictures.
3- Assessment
of
functional
patency/gastric
emptying
following
gasteroenterostomy.
4- Suspected anastomotic leak following surgery (use water soluble & not barium).
Barium meal
Fasting for at least 6 hours is important. 200 ml of barium is required. Each part
of the stomach & duodenum should be checked to ensure that there is no
abnormal narrowing. The outline of lesser curvature is smooth, while the greater
curvature is irregular. The gastric mucosa has smooth folds.
The duodenal cap is triangular & may be difficult to recognize in chronic ulcers
with deformity. Diverticula of the duodenal loop are common & without
significance.
Filling defects:
May arise from the wall or indent the wall from outside. CA is the commonest cause
of filling defect in adult.
Carcinoma produce irregular filling defect with alteration of mucosal pattern.
Overhanging edges or shouldering may be seen at the junction of the tumor & the
stomach. CA near fundus may obstruct the oesophagus, while that near the antrum
18
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
can lead to gastric outlet obstruction. When the whole stomach is involved, it may
appear narrowed & lacking peristalsis with obliteration of folds.
Early gastric cancer may appear as effacement of folds or shallow ulcer.
Diffuse infiltration of the stomach with lymphoma can produce fold
thickening.
CT is useful in assessing the extent of tumor & metastases to LN & liver.
Leiomyoma produce a smooth, round filling defect. It may have a large extra-
luminal extension (easily seen on CT). It may have ulcer on its surface.
Polyps may be single or multiple, sessile or with stalk. Imaging can not
differentiate between malignant & benign.
Intraluminal filling defects e.g. food or blood following hematemesis or bezoar.
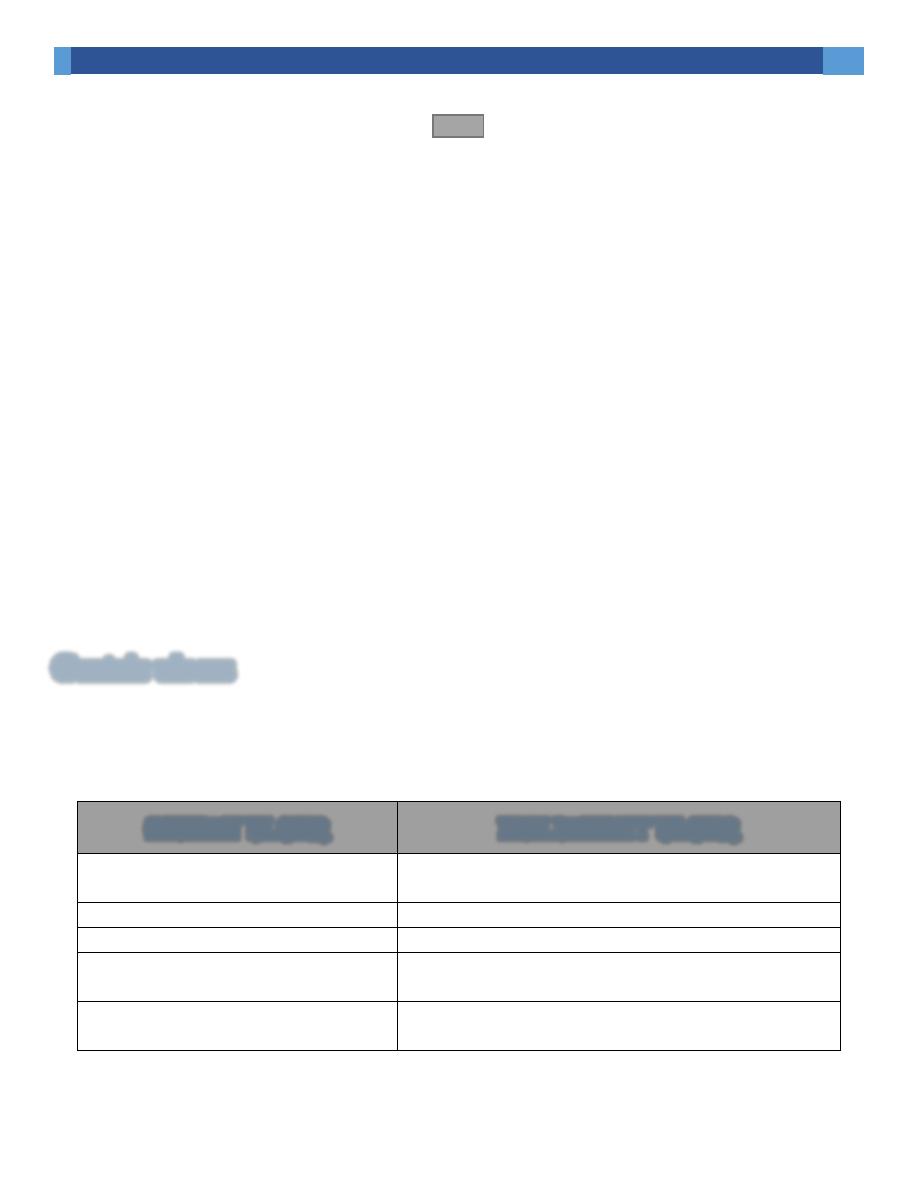
Gastric ulcers
May be benign or malignant. Once a gastric ulcer is diagnosed, its nature is
determined at gastroscopy.
Benign ulcer
Malignant ulcer
1. Projects beyond the lumen of
stomach.
1. Irregular filling defect not projecting.
2. Regular edge.
2. Irregular edge.
3. On antrum & grater curvature.
3. On fundus & the lesser curve.
4. Radiating mucosal folds reach the
edge of crater or near the edge.
4. Does not reach.
5. Reduce in size after medical
treatment.
5. Little change with medical treatment.
19
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Gastric outlet obstruction
Ba normally leaves the stomach within minutes. Prolonged delay with a dilated
stomach needs explanation.
Chronic DU with deformed, stenosed duodenal cap.
Antral carcinoma with irregular filling defect in the antrum.
Duodenal, ampullary, pancreatic carcinoma.
Acute or chronic pancreatitis +- pseudocyst.
Poor functional patency of a gastroenterostomy.
Pyloric stenosis in infants (confirmed with US).
Gastritis
Erosive gastritis (when severe) seen as small shallow Ba collections surrounded by
a lucent halo.
Hiatus hernia
Either sliding or rolling type.
In sliding type, the GE junction & portion of stomach are situated above
diaphragm. Reflux through incompetent cardiac sphincter may occur & result
in oesophagitis, ulceration or stricture.
In rolling type, the fundus herniates through the diaphragm but the GE junction
remains competent below the diaphragm.

21
Plain Abdomen
Lectures 7+8 Oesophagus + Stomach + Duodenum Dr. Laith
Sometimes hiatal hernia may be seen on CXR.
Duodenal ulcer
Mostly occur in the duodenal cap, few are postbulbar in location. The ulcer
crater may have surrounding lucent zone with radiating mucosal folds. When
chronic, DU causes deformity of the duodenal cap from scarring (it is
impossible to be sure about the presence of ulcer).
