Hyperbilirubinemia in the Newborn
• Dr.Ban Adil• MBCHB,FICSM,MRCPCh
JAUNDICE (ICTERUS).
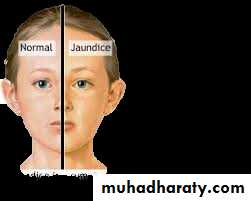
• Def.:Yellow discoloration of the sclera, skin, and mucous membranes• Clinically apparent jaundice in children and adults occurs when the serum concentration of bilirubin reaches 2–3 mg/dL (34–51 μmol/L);
• the neonate may not appear icteric until the bilirubin level is >5 mg/dL (85 μmol/L).
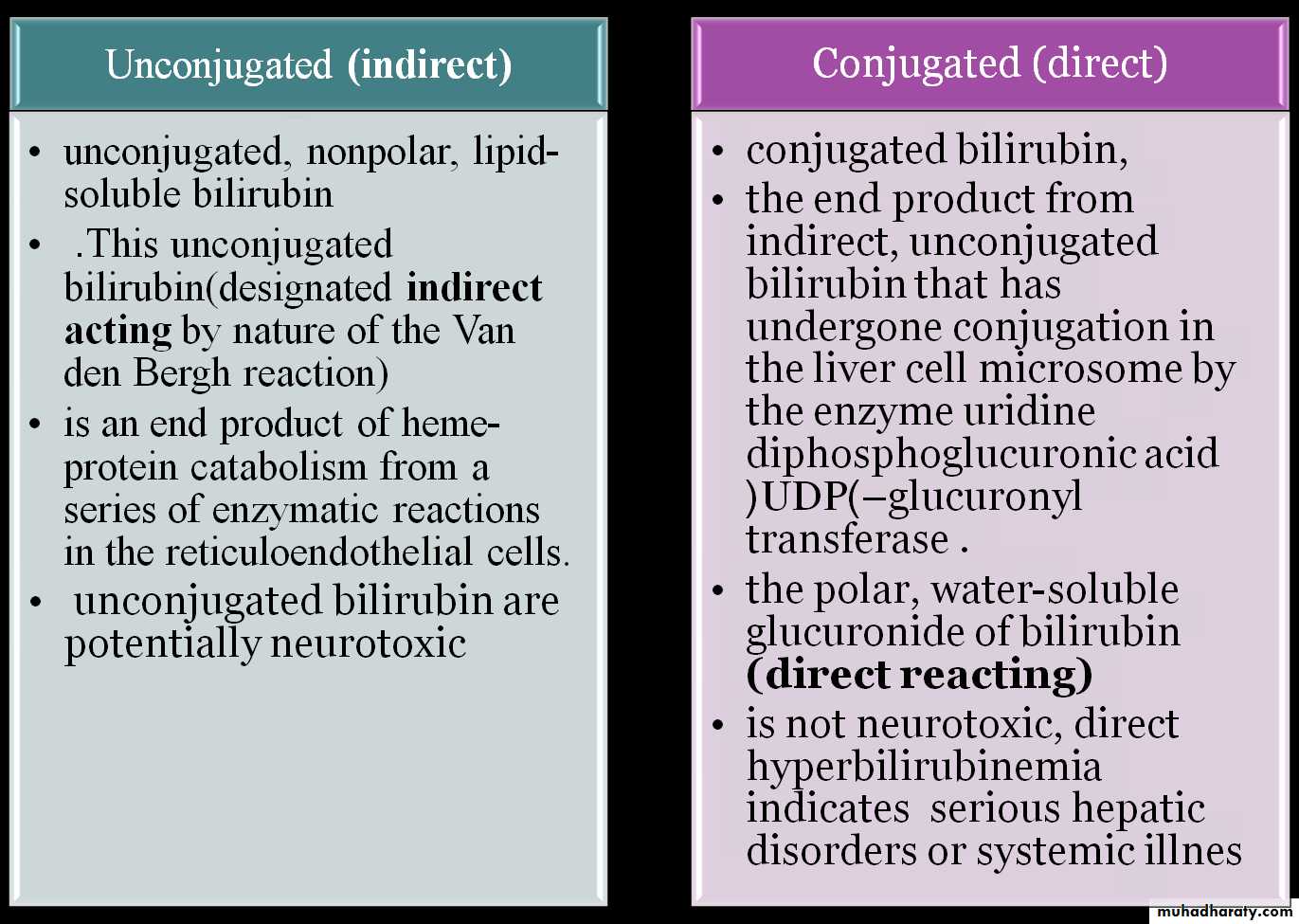
Types of jaundice
Types of jaundice
• unconjugated, nonpolar, lipid-soluble bilirubin pigment in the skin. This unconjugated bilirubin (designated indirect acting by nature of the Van den Bergh reaction) is an end product of heme-protein catabolism from a series of enzymatic reactions in the reticuloendothelial cells. unconjugated bilirubin are potentially neurotoxic• conjugated bilirubin, the end product from indirect, unconjugated bilirubin that has undergone conjugation in the liver cell microsome by the enzyme uridine diphosphoglucuronic acid (UDP)–glucuronyl transferase to form the polar, water-soluble glucuronide of bilirubin (direct reacting) Even though the conjugated form is not neurotoxic, direct hyperbilirubinemia indicates potentially serious hepatic disorders or systemic illnesses.
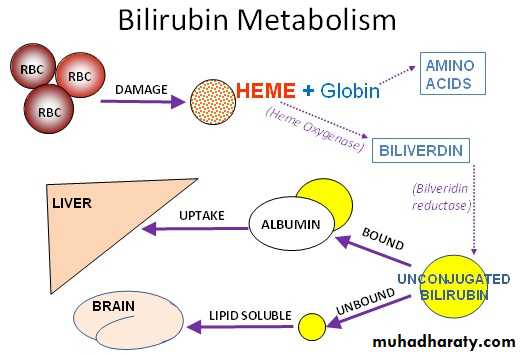
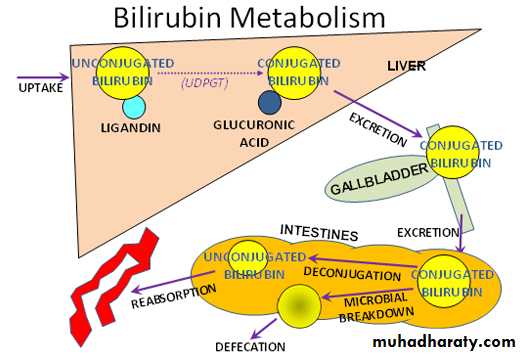
Metabolism of bilirubin
• Bilirubin is produced by the catabolism of hemoglobin in the reticuloendothelial system.• ring of heme is cleaved by heme oxygenase to form biliverdin
• Biliverdin is converted to bilirubin by biliverdin reductase.
• One gram of hemoglobin produces 35 mg of bilirubin
• Compared with adults, newborns have a twofold to threefold greater rate of bilirubin production (6 to 10 mg/kg/24 hr versus 3 mg/kg/24 hr). This increased production is caused in part by an increased RBC mass (higher hema-tocrit) and a shortened erythrocyte life span of 70 to 90 days compared with the 120-day erythrocyte life span in adults.
• Bilirubin produced after hemoglobin catabolism is lipid soluble and unconjugated and reacts as an indirect reagent in the van den Bergh test. Indirect-reacting, unconjugated bilirubin is toxic to the CNS and is insoluble in water, limiting its excretion
• Unconjugated bilirubin binds to albumin on specific bilirubin binding sites; 1 g of albumin binds 8.5 mg of bilirubin in a newborn. If the binding sites become saturated or if a competitive compound binds at the site, displacing bound bilirubin, free bilirubin becomes available to enter the CNS. Organic acids such as free fatty acids and drugs such as sulfisoxazole can displace bilirubin from its binding site on albumin.
• Hepatic conjugation results in the production of bilirubin diglucuronide, which is water soluble and capable of biliary and renal excretion. The enzyme glucuronosyltransferase represents the rate-limiting step of bilirubin conjugation
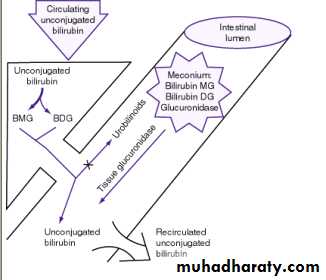
• Most conjugated bilirubin is excreted through the bile into the small intestine and eliminated in the stool. Some bilirubin may undergo hydrolysis back to the unconjugated fraction by intestinal glucuronidase, however, and may be reabsorbed (enterohepatic recirculation). In addition, bacteria in the neonatal intestine convert bilirubin to urobilinogen and stercobilinogen, which are excreted in urine and stool and usually limit bilirubin reabsorption. Delayed passage of meconium, which contains bilirubin, also may contribute to the enterohepatic recirculation of bilirubin.
HB
globin
hemebiliverdin
iron
Unconjugated bilirubin
albumin
2 Glocoronic acid
UDPGTBilirubin diglocoronide
urobilinogen
stercobilinReabsorbed to blood
Absorbed back to liver by
E.H circulation
Jaundice and Hyperbilirubinemia in the Newborn
Hyperbilirubinemia is a common and, in most cases, benign problem in neonates. Jaundice is observed during the 1st wk of life in approximately 60% of term infants and 80% of preterm infants.
ETIOLOGY.
• Unconjugated hyperbilirubinemia may be caused or increased by any factor that:• increases the load of bilirubin to be metabolized by the liver (hemolytic anemias, polycythemia, shortened red cell life as a result of immaturity or transfused cells, increased enterohepatic circulation, infection);
• damages or reduces the activity of the transferase enzyme or other related enzymes (genetic deficiency, hypoxia, infection, thyroid deficiency);
• competes for or blocks the transferase enzyme drugs and other substances requiring glucuronic acid conjugation.
• leads to an absence or decreased amounts of the enzyme or to reduction of bilirubin uptake by liver cells (genetic defect, and prematurity).
increases the load of bilirubin to be metabolized by the liver (
damages or reduces the activity of the transferase enzyme or other related enzymes
HB
globin
hemebiliverdin
iron
Unconjugated bilirubin
albumin
2 Glocoronic acid
UDPGTBilirubin diglocoronide
urobilinogen
stercobilinReabsorbed to blood
Absorbed back to liver by
E.H circulation
genetic deficiency, hypoxia, infection, thyroid deficiency
leads to an absence or decreased amounts of the enzymecompetes for or blocks the transferase enzyme
genetic defect, and prematurity
• hemolytic anemias
• polycythemia,• shortened red cell life as a result of immaturity or transfused cells,
• increased enterohepatic circulation,
• infection
5.The toxic effects of elevated serum levels of unconjugated bilirubin are increased by factors that reduce the retention of bilirubin in the circulation hypoproteinemia,
6.displacement of bilirubin from its binding sites on albumin by competitive binding of drugs such as sulfisoxazole and moxalactam, acidosis, and
increased free fatty acid concentration secondary to hypoglycemia, starvation, or hypothermia
displacement of bilirubin from its binding sites on albumin binding of drugs such as sulfisoxazole and moxalactam, acidosis, and increased free fatty acid concentration secondary to hypoglycemia, starvation, or hypothermia
HB
globin
hemebiliverdin
iron
Unconjugated bilirubin
albumin
2 Glocoronic acidUDPGT
Bilirubin diglocoronide
urobilinogen
stercobilin
Reabsorbed to blood
Absorbed back to liver by
E.H circulation
factors that reduce the retention of bilirubin in the circulation
5. Factors that increase the toxic effects of elevated serum levels of unconjugated bilirubin• the permeability of the blood-brain barrier neuronal susceptibility to injury, all of which are adversely influenced by asphyxia, prematurity, hyperosmolality, and infection.
• Early and frequent feeding decreases whereas breast-feeding and dehydration increase serum levels of bilirubin
• The neonatal production rate of bilirubin is 6–8 mg/kg/24 hr (in contrast to 3–4 mg/kg/24 hr in adults
• Delay in passage of meconium, which contains 1 mg bilirubin /dL, may contribute to jaundice by enterohepatic circulation after deconjugation by intestinal glucuronidase (
• Drugs such as oxytocin and chemicals used in the nursery such as phenolic detergents may also produce unconjugated hyperbilirubinemia
. Delay in passage of meconium, which contains 1 mg bilirubin/dL, may contribute to jaundice by enterohepatic circulation after deconjugation by intestinal glucuronidase
HB
globin
hemebiliverdin
iron
Unconjugated bilirubin
albumin
2 Glocoronic acid
UDPGTBilirubin diglocoronide
urobilinogen
stercobilinReabsorbed to blood
Absorbed back to liver by
E.H circulation
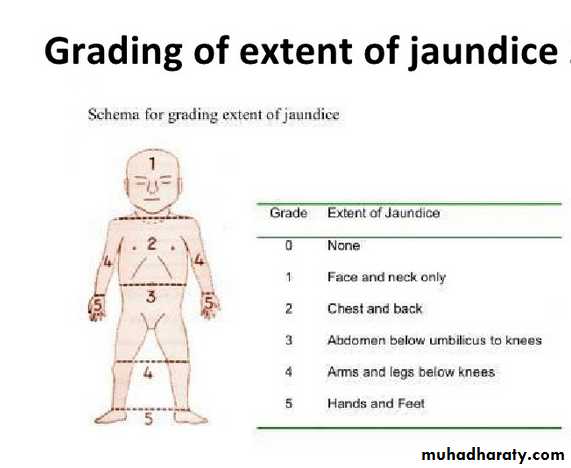
CLINICAL MANIFESTATIONS
• Jaundice usually becomes apparent in a cephalocaudal progression starting on the face and progressing to the abdomen and then feet, as serum levels increaseDermal pressure may reveal the anatomic progression of jaundice face, = 5 mg/dL; mid-abdomen, = 15 mg/dL; soles, = 20 mg/dL , but clinical examination cannot be depended on to estimate serum levels.
•
•
•
•
• 11/4/2014 6:37 PM - Screen Clipping
•
•
]). Noninvasive techniques for transcutaneous measurement of bilirubin (TcB) that correlate with serum levels may be used to screen infants, but determina tion of serum bilirubin level is indicated in patients with elevated age-specific transcutaneous measurement, progressing jaundice, or risk for either hemolysis or sepsis.
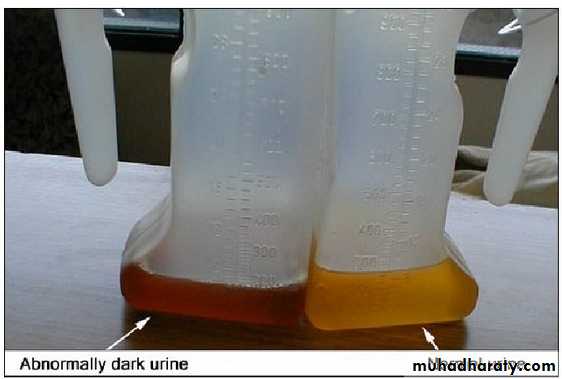
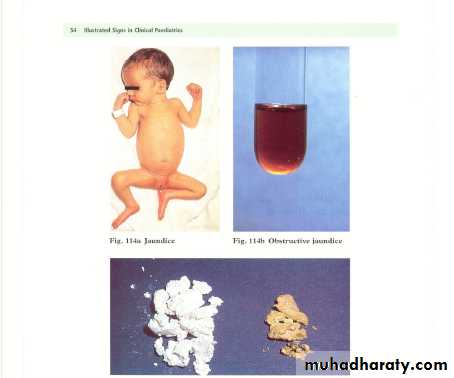
jaundice from deposition of indirect bilirubin in the skin tends to appear bright yellow or orange,
jaundice of the obstructive type (direct bilirubin) has a greenish or muddy yellow cast.
Although signs of kernicterus rarely appear on the 1st day, affected infants may present with lethargy and poor feeding and, without treatment, can progress to acute bilirubin encephalopathy
•
•
•
•
• 11/4/2014 6:37 PM - Screen Clipping
•
•
DIFFERENTIAL DIAGNOSIS. Jaundice that is present at birth or appears within the 1st 24 hr of life
• erythroblastosis fetalis,
• concealed hemorrhage,• sepsis,
• congenital infections, including syphilis, cytomegalovirus, rubella, and toxoplasmosis
Jaundice that 1st appears on the 2nd or 3rd day
isusually physiologic but may represent a more severe form.
Familial non-hemolytic icterus (Crigler-Najjar syndrome)
early-onset breast-feeding jaundice.
. Jaundice appearing after the 3rd day and within the 1st wk:
bacterial sepsis
urinary tract infection;
it may also be due to other infections, notably syphilis, toxoplasmosis, cytomegalovirus, (TORCH)or enterovirus
1st recognized after the 1st wk of life
There is a long differential diagnosis for jaundice :Including
• breast-milk jaundice,
• septicemia,
• congenital atresia or paucity of the bile ducts, hepatitis,
• galactosemia,
• hypothyroidism,
• CF,
• congenital hemolytic anemia crises related to red cell morphology and enzyme deficiencies spherocytosis,G6PD,pyruvate kinase def.(
DIAGNOSIS
Investigations for early jaundiceSerum bilirubin level
FBC and film
Blood group
Maternal blood group
Direct coombs test
Consider G6PD level
The differential diagnosis for persistent jaundice during the 1st mo of life:
• cholestasis,
• hepatitis
• , cytomegalic inclusion disease, syphilis, toxoplasmosis,
• familial non-hemolytic icterus,
• congenital atresia of the bile ducts,
• galactosemia, or
• inspissated bile syndrome following hemolytic disease of the newborn.
• Rarely, physiologic jaundice may be prolonged for several wk, as in infants with hypothyroidism or pyloric stenosis.
Serum bilirubin level
Conjugated fraction of bilirubinLiver function test (GGT, ALT, AST, Albumin)
Coagulation profile (PT, PTT, INR)Abdominal ultrasound (gallbladder)
HIDA scan (with follow through)
Thyroid function test (TSH, free T4)
Metabolic screen (urine for reducing substance)
Hepatitis screen (TORCH)
Liver biopsy (bile duct proliferation)
FBC and film
Blood group
Maternal blood group
Direct coombs test
Investigations for prolonged jaundice
• Full-term, low-risk, asymptomatic infants may be evaluated by monitoring total serum bilirubin (TSB) levels. Regardless of gestation or time of appearance of jaundice, patients with significant hyperbilirubinemia and those with symptoms or signs require a complete diagnostic evaluation, which includes determination of direct and indirect bilirubin fractions, hemoglobin, reticulocyte count, blood type, Coombs test, and examination of a peripheral blood smear. Indirect hyperbilirubinemia, reticulocytosis, and a smear with evidence of red blood cell destruction suggest hemolysis (
• ). In the absence of blood group incompatibility, non–immunologically induced hemolysis should be considered.
• If direct hyperbilirubinemia is present, hepatitis, congenital bile duct disorders (atresia, paucity, Byler disease), cholestasis, inborn errors of metabolism, CF, and sepsis are diagnostic possibilities. If the reticulocyte count, Coombs test, and direct bilirubin are normal, physiologic or pathologic indirect hyperbilirubinemia may be present (
PHYSIOLOGIC JAUNDICE (ICTERUS NEONATORUM)
• Under normal circumstances, the level of indirect-reacting bilirubin in umbilical cord serum is 1–3 mg/dL• rises at a rate of <5 mg/dL/24 hr;
• thus, jaundice becomes visible on the 2nd–3rd day,
• usually peaking between the 2nd and 4th days at 5–6 mg/dL
• and decreasing to below 2 mg/dL between the 5th and 7th days of life
increased bilirubin production resulting from
increased RBC mass,shortened RBC life span,
hepatic immaturity of glucuronosyltransferase.
Cause of physiological jaundice
Risk factors for elevated indirect hyperbilirubinemia include:
• maternal age, race (Chinese, Japanese, Korean, and Native American),• maternal diabetes,
• oxytocin induction,
• prematurity,
• drugs vitamin K3
• polycythemia,
• male sex,
• trisomy 21,
• cutaneous bruising, blood extravasation (cephalohematoma),
• breast-feeding,
• weight loss (dehydration or caloric deprivation),
• delayed bowel movement, and
• a family history/sibling who had physiologic jaundice (
Prediction of which neonates are at risk for exaggerated physiologic jaundice can be based on hour-specific bilirubin levels in the 1st 24–72 hr of life ( Fig )
Indirect bilirubin levels in full-term infants decline to adult levels (1 mg/dl) by 10–14 days of life.
In premature infants, the rise in serum bilirubin tends to be the same or somewhat slower but of longer duration than in term infants.
Peak levels of 8–12 mg/dL are not usually reached until the 4th–7th day,
and jaundice is infrequently observed after the 10th day, corresponding to the maturation of mechanisms for bilirubin metabolism and excretion.
• Pathological jaundice is suspected if :
• it appears in the 1st 24–36 hr of life.• serum bilirubin is rising at a rate faster than 5 mg/dL/24 hr, (
• serum bilirubin is >12 mg/dL in full-term infants (especially in the absence of risk factors) or 10–14 mg/dL in preterm infants,
• jaundice persists after 10–14 days of life,
• direct-reacting bilirubin is >2 mg/dL at any time.
• Other factors suggesting a nonphysiologic cause of jaundice are family history of hemolytic disease, pallor, hepatomegaly, splenomegaly, failure of phototherapy to lower bilirubin, vomiting, lethargy, poor feeding, excessive weight loss, apnea, bradycardia, abnormal vital signs (including hypothermia), light-colored stools, dark urine positive for bilirubin, and signs of kernicterus
breast-feeding jaundice
• occurs in the 1st week of life, in breast-fed infants who normally have higher bilirubin levels than formula-fed infants .• Hyperbilirubinemia (>12 mg/dL) develops in 13% of breast-fed infants in the 1st wk of life
• may be due to decreased milk intake with dehydration
• and/or reduced caloric intake.
• More in primi- mother,C/S
• JAUNDICE ASSOCIATED WITH BREAST-FEEDING
• Giving supplements of glucose water to breast-fed infants is associated with higher bilirubin levels,
• in part because of reduced intake of the higher caloric density of breast milk.
• Frequent breast-feeding(>10/24 hr),
• rooming-in with night feeding,• discouraging 5% dextrose or water supplementation,
• and ongoing lactation support may reduce the incidence of early breast-feeding jaundice
JAUNDICE ASSOCIATED WITH BREAST-FEEDING.
Significant elevation in unconjugated bilirubin (breast-milk jaundice) develops in an estimated 2% of breast-fed term infantsafter the 7th day of life,
with maximal concentrations as high as 10–30 mg/dL reached during the 2nd–3rd week
If breast-feeding is continued, the bilirubin gradually decreases but may persist for 3–10 wk at lower levels.
breast-milk jaundice
If nursing is discontinued, the serum bilirubin level falls rapidly, reaching normal levels within a few days.
With resumption of breast-feeding, bilirubin levels seldom return to previously high levels.
Phototherapy may be of benefit .
Although uncommon, kernicterus can occur in patients with breast-milk jaundice.
The etiology of breast-milk jaundice is not entirely clear, but may be attributed to the presence of glucuronidase in some breast milk.
Kernicterus
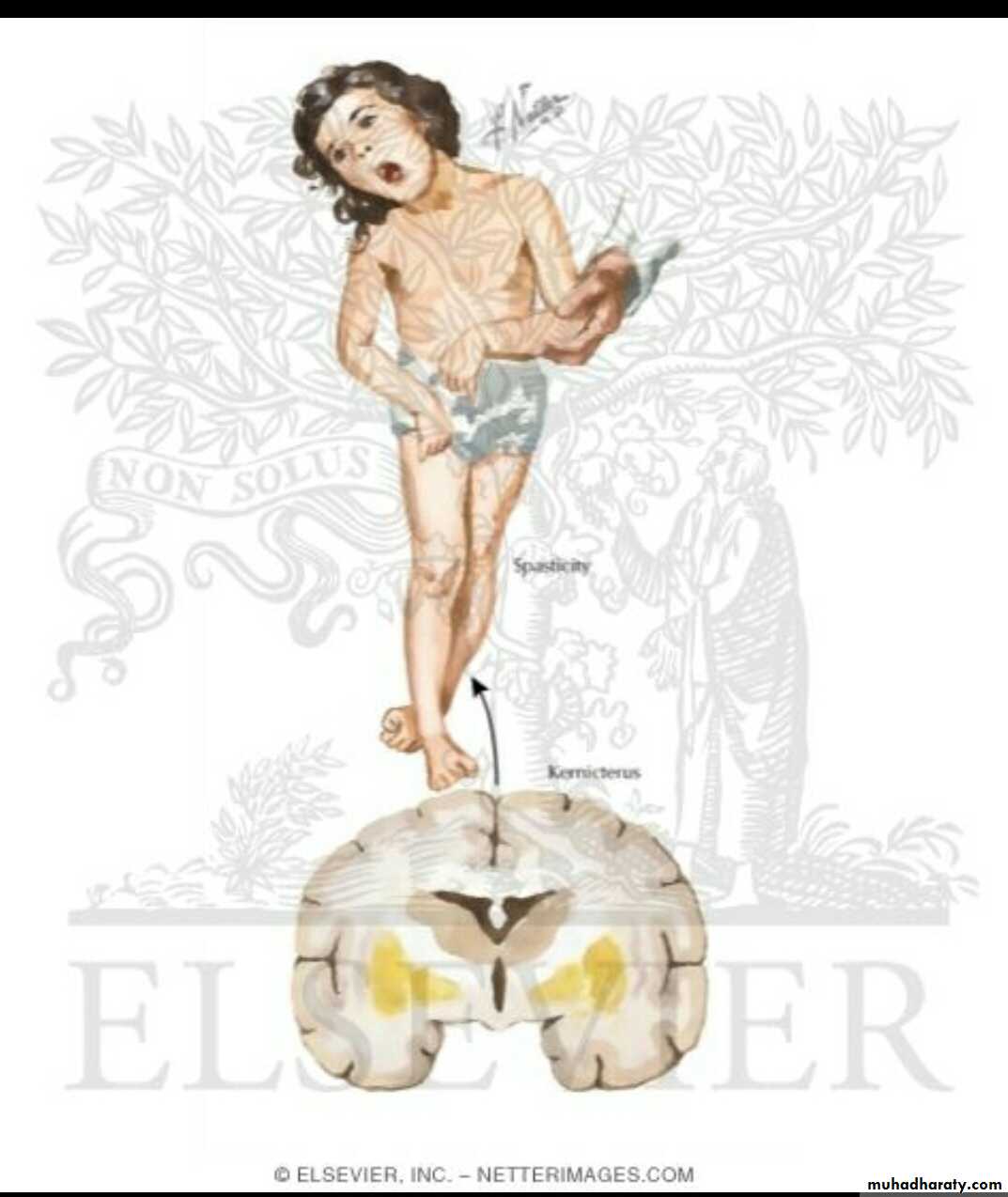
• Kernicterus: or bilirubin encephalopathy, is a neurologic syndrome resulting from the deposition of unconjugated (indirect) bilirubin in the basal ganglia and brainstem nuclei.
• The precise blood level above which indirect-reacting bilirubin or free bilirubin will be toxic for an individual infant is unpredictable.
• Kernicterus usually does not develop in term infants when bilirubin levels are less than 20 to 25 mg/dL.
• The incidence of kernicterus increases as serum bilirubin levels increase to greater than 25 mg/dL.
• Kernicterus may be noted at bilirubin levels less than 20 mg/dL in the presence of sepsis, meningitis, hemolysis, asphyxia, hypoxia, hypothermia, hypoglycemia, bilirubin-displacing drugs (sulfa drugs), and prematurity.
• Other risks for kernicterus in term infants are hemolysis, jaundice noted within 24 hours of birth, and delayed diagnosis of hyperbilirubinemia.
• .
• In previously healthy, predominantly breast-fed term infants, kernicterus has developed when bilirubin levels exceed 30 mg/dL.
• Onset is usually in the 1st wk of life, but may be delayed to the 2nd–3rd wk
Kernicterus has developed in extremely immature infants weighing less than 1000 g when bilirubin levels are less than 10 mg/dL because of a more permeable blood-brain barrier associated with prematurity.
CLINICAL MANIFESTATIONS
• Signs and symptoms of kernicterus usually appear 2–5 days after birth in term infants• and as late as the 7th day in premature infants,
• but hyperbilirubinemia may lead to encephalopathy at any time during the neonatal period.
• .
The early signs may be subtle and indistinguishable from those of sepsis, asphyxia, hypoglycemia, intracranial hemorrhage, and other acute systemic illnesses in a neonate.
Lethargy, poor feeding, and loss of the Moro reflex are common initial signs.
Subsequently, the infant may appear gravely ill and prostrated, with diminished tendon reflexes and respiratory distress.
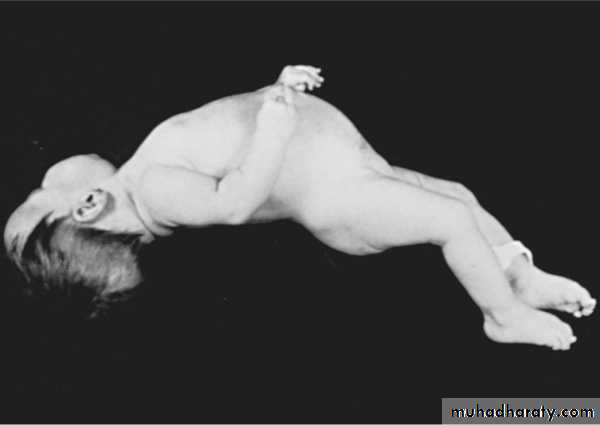
Opisthotonos with a bulging fontanel, twitching of the face or limbs, and a shrill high-pitched cry may follow.
Opisthotonos
• In advanced cases, convulsions and spasm occur,• with affected infants stiffly extending their arms in an inward rotation with the fists clenched . Rigidity is rare at this late stage.
• Infants with severe cases of kernicterus die in the neonatal period.
• Spasticity resolves in surviving infants, who may manifest later nerve deafness, choreoathetoid cerebral palsy, mental retardation, enamel dysplasia, and discoloration of teeth as permanent sequelae.
ACUTE FORM
Phase 1 (1st 1–2 days): poor sucking, stupor, hypotonia, seizures
Phase 2 (middle of 1st wk): hypertonia of extensor muscles, opisthotonos, retrocollis, feverPhase 3 (after the 1st wk): hypertonia
CHRONIC FORMFirst year: hypotonia, active deep tendon reflexes, obligatory tonic neck reflexes, delayed motor skills
After 1st yr: movement disorders (choreoathetosis, ballismus, tremor), upward gaze, sensorineural hearing
• Clinical Features of Kernicterus
ACUTE FORM
Phase 1 (1st 1–2 days): poor sucking, stupor, hypotonia, seizuresPhase 2 (middle of 1st wk): hypertonia of extensor muscles, opisthotonos, retrocollis, fever
Phase 3 (after the 1st wk): hypertonia
CHRONIC FORMFirst year: hypotonia, active deep tendon reflexes, obligatory tonic neck reflexes, delayed motor skills
After 1st yr: movement disorders (choreoathetosis, ballismus, tremor), upward gaze, sensorineural hearing loss
• Clinical Features of Kernicterus
Many infants who progress to these severe neurologic signs die; the survivors are usually seriously damaged, but may appear to recover and for 2–3 mo show few abnormalities. Later in the 1st yr of life, opisthotonos, muscle rigidity, irregular movements, and convulsions tend to recur
• In the 2nd yr, the opisthotonos and seizures abate, but irregular, involuntary movements, muscle rigidity, or, in some infants, hypotonia increase steadily.
• By 3 yr of age, the complete neurologic syndrome is often apparent and consists of bilateral choreoathetosis with involuntary muscle spasms, extrapyramidal signs, seizures, mental deficiency, dysarthric speech, high frequency hearing loss, squinting, and defective upward eye movements. Pyramidal signs, hypotonia, and ataxia occur in a few infants. In mildly affected infants, the syndrome may be characterized only by mild to moderate neuromuscular incoordination, partial deafness, or “minimal brain dysfunction,” occurring singly or in combination; these problems may be inapparent until the child enters school (
is an effective and safe method for reducing indirect bilirubin levels.
Bilirubin absorbs light maximally in the blue range (420–470 nm).Broad-spectrum white, blue, and special narrow-spectrum (super) blue lights have been effective in reducing bilirubin levels
Therapy of Indirect Hyperbilirubinemia
Phototherapyphotochemical reaction producing configurational isomer
• the reversible, more water-soluble• bypassing the liver's conjugation system
• excreted in bile without conjugation.
• a more water-soluble structural isomer which does not spontaneously revert to unconjugated native bilirubin (irreversible)
• can be excreted in urine.
Mode of action of phototherapy
Conventional phototherapy
is applied continuously, and the infant is turned frequently for maximal skin surface area exposure
. It should be discontinued as soon as the indirect bilirubin concentration has reduced to levels considered safe with respect to the infant's age and condition.
Maximal intensive phototherapy
Such therapy includes “special blue” fluorescent tubes,placing the lamps within 15–20 cm of the infant,
and placing a fiberoptic phototherapy blanket under the infant's back to increase the exposed surface area.
Because phototherapy may require 6–12 hr to have a measurable effect,
it must be started at bilirubin levels below those indicated for exchange transfusion.In term infants, phototherapy is begun when indirect bilirubin levels are between 16 and 18 mg/dL.
Phototherapy is initiated in premature infants when bilirubin is at lower levels
Bilirubin in the skin absorbs light energy, causing several photochemical reactions.
One major product from phototherapy is a result of a reversible photo-isomerization reaction converting the toxic native unconjugated 4Z, 15Z-bilirubin into an unconjugated configurational isomer 4Z,15E-bilirubin,which can then be excreted in bile without conjugation.).
The other major product from phototherapy is lumirubin, which is an irreversible structural isomer converted from native bilirubin and can be excreted by the kidneys in the unconjugated state. Bilirubin absorbs light maximally in the blue range (420–470 nm
BIRTHWEIGHT (g)
UNCOMPLICATEDCOMPLICATED[*]
<1,000
12–13
10–12
1,000–1,250
12–14
10–12
1,251–1,499
14–16
12–14
1,500–1,999
16–20
15–17
2,000–2,500
20–22
18–20
• Suggested Maximal Indirect Serum Bilirubin Concentrations (mg/dL) in Preterm Infants
Phototherapy is usually started at 50–70% of the maximal indirect level.
If values greatly exceed this level, if phototherapy is unsuccessful in reducing the maximal bilirubin level, or if signs of kernicterus are evident, exchange transfusion is indicated.
Serum bilirubin levels and hematocrit should be monitored every 4–8 hr in infants with hemolytic disease or those with bilirubin levels near toxic range for the individual infant.
Others, particularly older infants, may be monitored less frequently.
Serum bilirubin monitoring should continue for at least 24 hr after cessation of phototherapy in patients with hemolytic disease because unexpected rises in bilirubin may occur and require further treatment.
Skin color cannot be relied on for evaluating the effectiveness of phototherapy;
• the skin of babies exposed to light may appear to be almost without jaundice in the presence of marked hyperbilirubinemia.
Although not necessary for all affected infants, intravenous fluid supplementation added to oral feedings may be beneficial in dehydrated patients or those with high bilirubin levels nearing exchange transfusion.
Dark skin does not reduce the efficacy of phototherapy.
NOTES
Complications of phototherapy
• increased insensible water loss
• diarrhea
• dehydration
• macular-papular red skin rash
• lethargy
• masking of cyanosis
• nasal obstruction by eye pads
• potential for retinal damage
• Skin bronzing may be noted in infants with direct-reacting hyperbilirubinemia
Exchange transfusion
usually is reserved for infants with dangerously high indirect bilirubin levels who are at risk for kernicterus.As a rule of thumb, a level of 20 mg/dL for indirect-reacting bilirubin is the "exchange number" for infants with hemolysis who weigh more than 2000 g.
Asymptomatic infants with physiologic or breast milk jaundice may not require exchange transfusion, unless the indirect bilirubin level exceeds 25 mg/dL.
The exchangeable level of indirect bilirubin for other infants may be estimated by calculating
10% of the birth weight in grams
the level in an infant weighing 1500 g would be 15 mg/dL. Infants weighing less than 1000 g usually do not require an exchange transfusion until the bilirubin level exceeds 10 mg/dL.Small infusions of fresh whole blood crossmatched with that of the mother and infant
are alternated with withdrawals of an equivalent quantity of the infant's blood, which is discarded.
Depending on the size of the infant, aliquots of 5 to 20 mL per cycle are withdrawn and infused,
with the total procedure lasting 45 to 60 minutes.
The total amount of blood exchanged is equal to twice the infant's blood volume, calculated as:
Weight (kg) X 85 ml/kg X 2
This volume should remove 85% of the infant's RBCs (the source of bilirubin), maternal antibodies.The exchange transfusion usually is performed through an umbilical venous
The level of serum bilirubin immediately after the exchange transfusion declines to levels that are about half of those before the exchange;levels rebound 6 to 8 hours later as a result of continued hemolysis and redistribution of bilirubin from tissue stores.
Complications of exchange transfusion
Graft versus reactionRelated to the blood
• Hepatitis B,C ,HIV,CMV..)
infection
Hypoglycemia
Hypocalcemia
Hypomagnesemia
hyperkalemia
Metabolic
Anemia/polycythemia
PerforationRelated to the catheter
Haemorrhage
vasospasmHypo-or hyperthermia
Related to the procedureVolume overload
Necrotizing entrerocolitisarrythmia
Late anemia
Late complicationspersistent icterus with significant elevations in direct and indirect bilirubin in infants with hemolytic disease. The cause is unclear, but the jaundice clears spontaneously within a few weeks or months.
Inspissated bile syndrome
Portal vein thrombosis and portal hypertension
Late Complications.Late anemia
may be hemolytic or hyporegenerative. Treatment with supplemental iron, erythropoietin, or blood transfusion may be indicated.
A mild graft vs host reaction may be manifested as diarrhea, rash, hepatitis, or eosinophilia.
Inspissated bile syndrome refers to the rare occurrence of persistent icterus in association with significant elevations in direct and indirect bilirubin in infants with hemolytic disease. The cause is unclear, but the jaundice clears spontaneously within a few weeks or months.
Portal vein thrombosis and portal hypertension