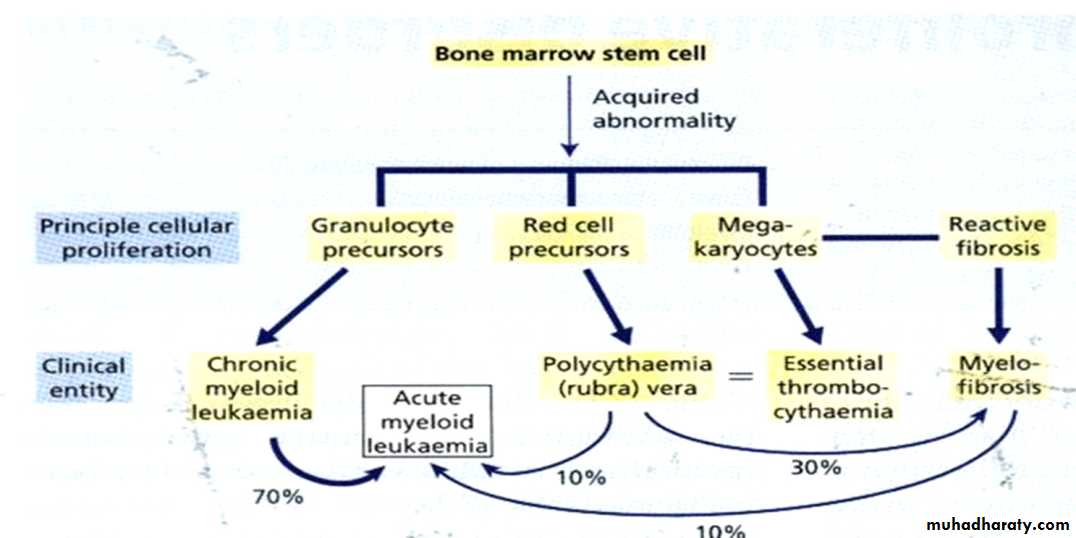
باطنيه د.خالد نافع CML Myeloproliferative disorderClonal evolutionClonal evolution & stepwise progression to fibrosis, marrow failure or acute blast phase
Chronic myelogenous leukemia(CML(
Description : CML is a myeloproliferative disorder characterized by increased proliferation of granulocyte, and evidence of myeloproliferation involve liver and spleen.
CML accounts for 20% of all leukemia affecting pts. between 30-80 years, with a peak incidence at 55years.
CML. Historical vs. Modern Perspective
ParameterHistorical
Modern
Course
Fatal
Indolent
Prognosis
Poor
Excellent
7-yr survival
40%
90%
Frontline Rx
Allogeneic SCT;
IFN-
Imatinib
Second line Rx
?
New Tyrosine Kinase Inhibitors; allo SCT
ETIOLOGY
Not clear
Little evidence of genetic factors linked to the disease
Increased incidence
Survivors of the atomic disasters at Nagasaki & Hiroshima
Post radiation therapy
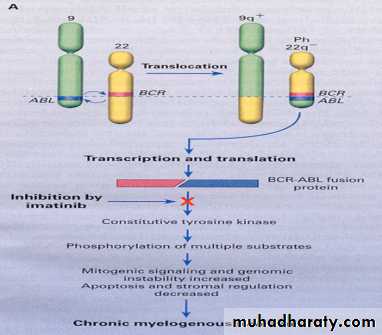
CML is an acquired abnormality that involves the stem cells and is characterized by specific chromosomal abnormality (translocation) between the long arm of chromosome 22 and 9 which is called philadelphia chromosome (ph). Approximately 95 % of patients with CML have this abnormality.
The chromosome has been found in all myeloid and lymphoid cell indicating the involvement of the pluripotential stem cell.
Leukaemogenesis
Molecular consequence of the t(9;22) is the fusion protein BCR–ABL, which has increased in tyrosine kinase activityBCR-ABL protein transform hematopoietic cells so that their growth and survival become independent of cytokines
It protects hematopoietic cells from programmed cell death (apoptosis)
Phases of chronic myeloid leukemia
Chronic phase accelerated phase blast phaseCLINICAL FEATURES
25 % asymptomatic at time of diagnosis
Chronic Phase :
Splenomegaly in 90% of patients . In about 10% the enlargement is massive. Afriction rub may be heard in cases of splenic infarction.
Hepatomegaly 50%. Lymhadenopathy is unusual.
Symptoms related to hypermetabolism
Weight loss
Anorexia
Lassitude
Night sweats
Stable disease, no cancer out side bone marrow or spleen, Median duration 3 years, range several months to > 20 years
Features of anaemia
Pallor, dyspnoea, tachycardia
Abnormal platelet function
Bruising, epistaxis, menorrhagiaHyperleukocytosis
thrombosisIncreased purine breakdown : gout
Visual disturbances
Priapism
Phases- Cont.
Accelerated phase
Median duration is 3.5 – 5 yrs before evolving to more aggressive phases
Clinical features
Increasing splenomegaly refractory to chemotherapy
Increasing chemotherapy requirement
Lab features
Blasts>15% in blood
Blast & promyelocyte > 30% in blood
Basophil 20% in blood
Thrombocytopenia
Cytogenetic: clonal evolution
.
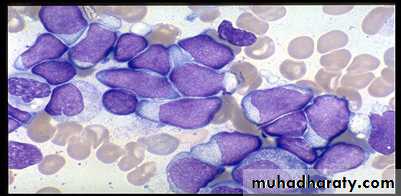
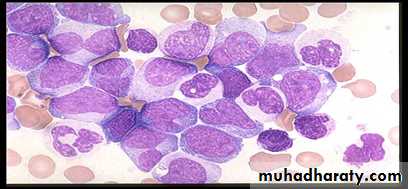
Blastic phase
Resembles acute leukaemia
Diagnosis requires > 20% blast in marrow
2/3 transform to myeloid blastic phase and 1/3 to lymphoid blastic phase
Survival : 9 mos vs 3 mos (lym vs myeloid(
CML-ALL CML-AML
LAB FINDINGa.Complete Blood Count(CBC): 1.N/N anaemia. 2.WBC count range 9.5-600 x 109/L(mean 220x 109/L) .3. Platelet count 162-2000 x109/L(mean 445x109/L) 4. In the blood film all stages of maturation are present from myeloblast to neutrophil, myeloblast less than 10%. Basophilia &oesonophils may increase as the disease progresses.
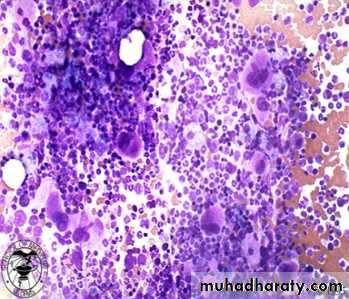
b. Bone marrow
Hypercellular (reduced fat spaces)Myeloid:erythroid ratio – 10:1 to 30:1 (N : 2:1)Myelocyte predominant , blasts less 10%Megakaryocytes increased & dysplasticIncrease reticulin fibrosis in 30-40%.*For chromosomal analysis(Ph chromosome),
*RNA analysis for BCR-ABL.
c. other laboratory findings : Serum B12 and transcobalamin increasedSerum uric acid increasedLactate dehydrogenase increased
CML - principles of treatment
Relieve symptoms of hyperleukocytosis, splenomegaly and thrombocytosis
Hydration
Chemotherapy (busulphan, Hydoxyurea)
Control and prolong chronic phase
alpha interferon+chemotherapy
imatinib mesylate
chemotherapy (hydroxyurea)
Eradicate malignant clone (curative)
allogeneic transplantation
alpha interferon ?
imatinib mesylate/STI 571 ?(Tyrosine kinase inhibitor(
Chemotherapy ;
Hydoxcarbamide 1000-1500 mg/day orally the effects should be monitered every 2-6 weeks. Fewer side effect
Acts by inhibiting the enzyme ribonucleotide reductase
Haematological remissions obtain in 80%.
However disease progression not altered and persistence of Ph chromosome . containing clone
1.HSCT
Intensive chemotherapy and total body irradiation (TBI) are followed by the transplantation of HLA matched allogeneic stem cell.
.Tyrosine kinase activity inhibitor
- IMATINIB mesylate/ (STI 571, GLIVEC)400 mg single dose orally. Acts specifically by blocking the binding site for ATP in the Abl kinase. -NILOTINIB (TASIGNA)600-800 mg daily(300-400 mg x2) -DASATINIB (SPRYCEL)50-70 mg once or twice daily
-Ponatinib
Variants of CML
*Ph-negative CML BCR-ABL negative;
About 5% of patients with haematologically acceptable CML lack the Ph chromosome.
older patient mostly male with lower platelet count and higher absolute monocyte count.
Respond poorly to treatment.
Median survival less than 1 year.
*Juvenile CML
Rare.Affecting children <12 year-old.
C/F – anaemia, or lymphadenopathy with hepatosplenomegaly, skin rashes.
Lab findings – leucocytosis with variable numbers of blast in the peripheral blood.
Marrow is hypercellular but lacks chromosomal abnormalities.
Responds poorly to standard cytotoxic drugs.