Page1
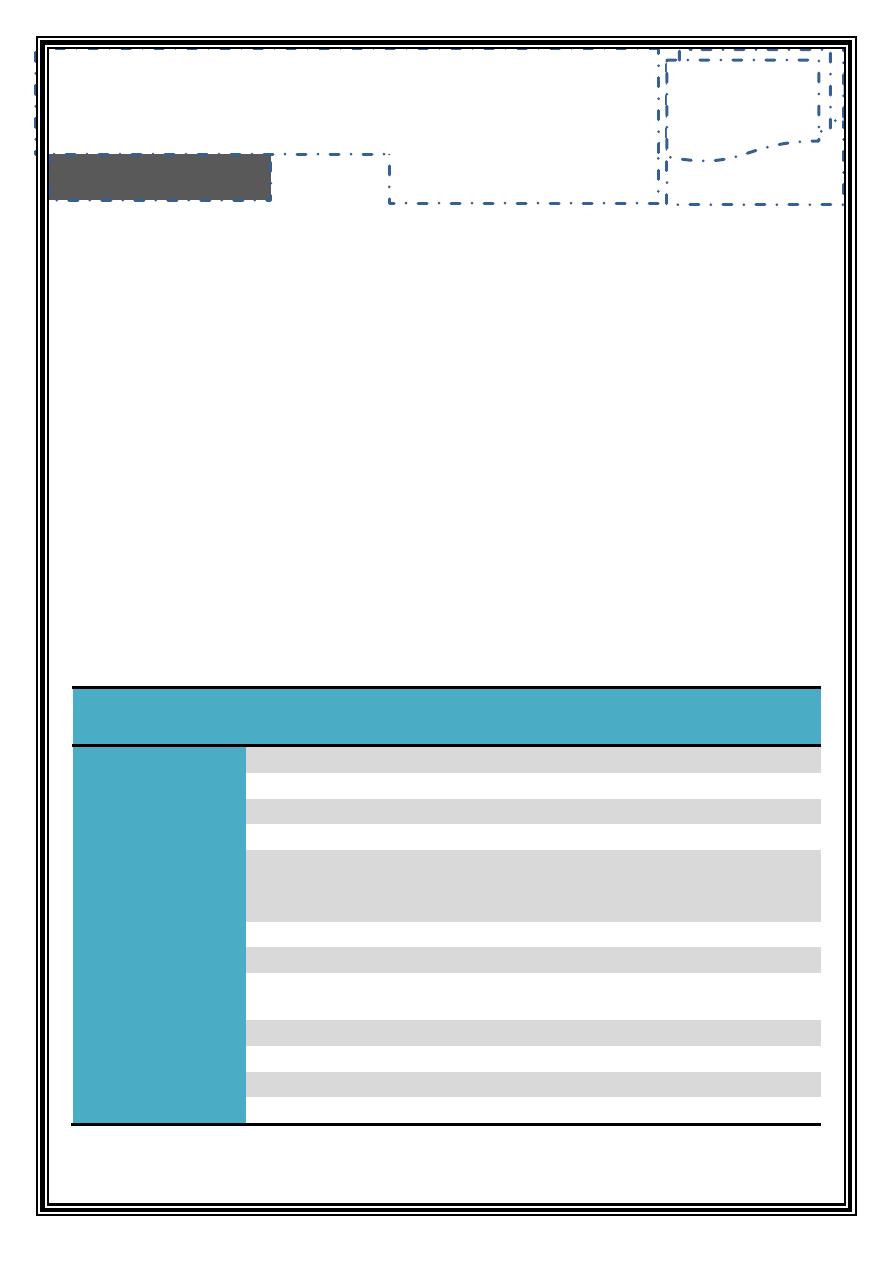
Introduction
Cranial nerves are 12 pairs of nerves, arise from the brain and distribute in
head and neck region and may reach abdomen as in case of vagus nerve
•
CNI, CNII, CNIII, CNIV arise from midbrain
•
CNV, CNVI, CNVII, CNVIII arise from pons
•
CNIX, CNX, XNXI, CNXII arise from medulla oblongata
As a dental student, you should be well oriented with the basic
information as well as clinical examination of each nerve
ﻳﻌﻧﻲ ﺍﺣﻔﻅ ﻫﺫﺍ ﺍﻟﺟﺩﻭﻝ ﻭﺍﺣﻔﻅ ﻓﺣﻭﺻﺎﺕ ﻛﻝ ﻋﺻﺏ
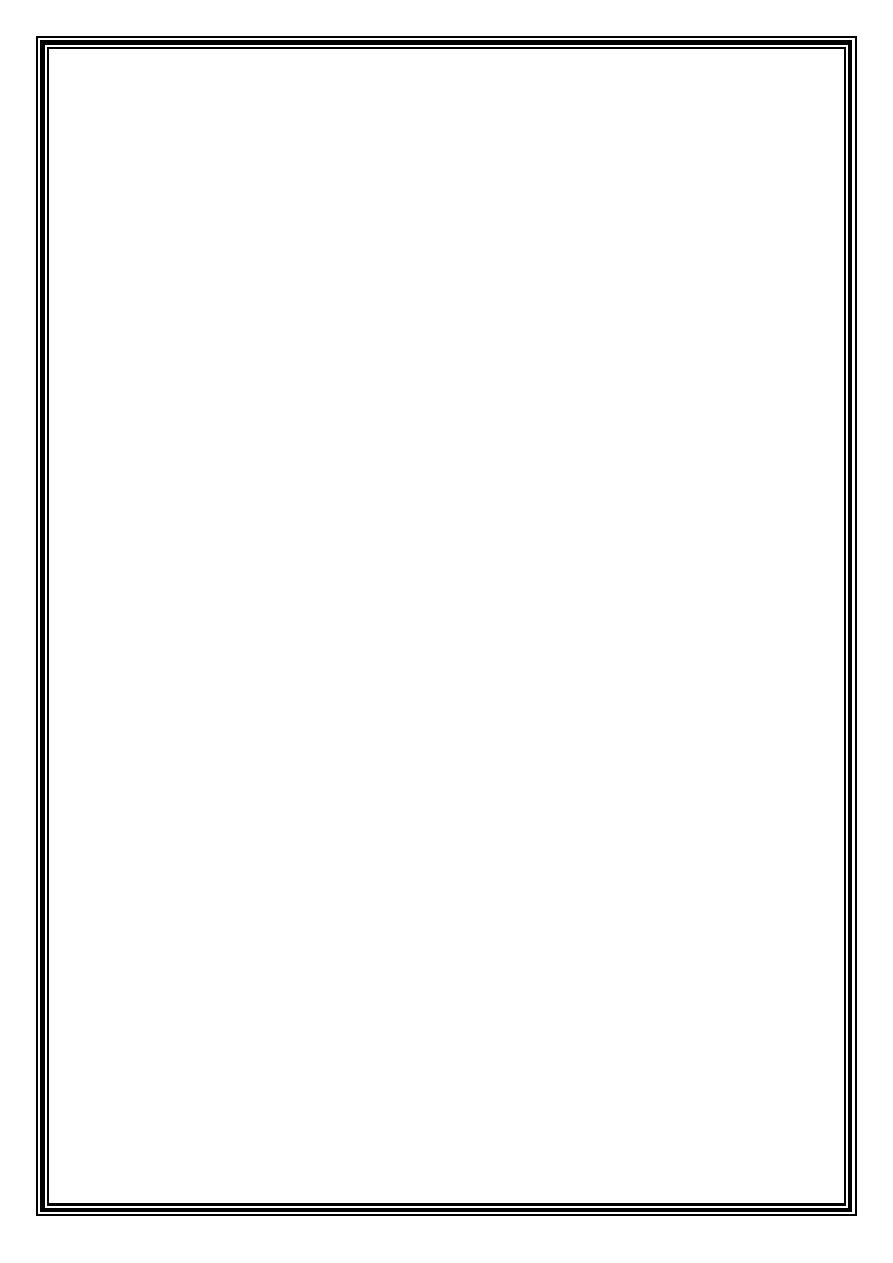
Cranial
nerve
Symbol Motor Sensory
Para-
sympathetic
Foramen
Olfactory
CNI
√
Cribriform plate
Optic
CNII
√
Optic canal
Oculomotor
CNIII
√
√
SO fissure
Trochlear
CNIV
√
SO fissure
Trigeminal
CNV
√
√
1.
Ophthalmic: SO fissure
2.
Maxillary: rotundum
3.
Mandibular: ovale
Abducent
CNVI
√
SO fissure
Facial
CNVII
√
√
Stylomastoid
Vestibulocochlear
CNVIII
√
Internal acoustic canal
(dose not exit cranium)
Glossopharyngeal
CNIX
√
√
√
Jugular
Vagus
CNX
√
√
√
Jugular
Accessory
CNXI
√
Jugular
Hypoglossal
CNXII
√
Hypoglossal canal
.د
ﺑﺼﻴﺮ
6 Sheets / 300 I.D.
ﻃﺐ ﻓﻢ
-
ﺳﻤﻨﺎر
3
Cranial Nerves
seminar 3, 4, 5, and 6
Page2
CNI Olfactory nerve
Arises from olfactory epithelium passing through the cribriform plate to the olfactory bulb
the to the primary olfactory cortex
Examination
: holding aromatic compounds (coffee, soap, onion) near each nostril
Abnormality
: Anosmia: patient cannot detect smell due to:
1.
Transient loss of smell , flu or sinusitis
2.
Tumor near frontal lobe of brain (meningioma, carcinoma of paranasal sinuses)
3.
Fracture of anterior cranial fossa near area 43 or injury to CNI or cribriform plate
Aromatic compound causes CNS stimulation, used to regain patient's consciousness
CNII Optic nerve
Arises from retina passing through optic canal crossing optic chiasm (medial fibers cross to
other sides in optic chiasm)
Examination
1.
Visual acuity: by Snellen chart, placed 6m from the subject
2.
Visual field: lateral field loss called (hemianopia) due to damage in optica chiasm as
in Paget disease (Prognathism, visual disturbance, hemianopia, ↑ALP)
Normal ALP 1.5-4 Bodansky, 3-11 King Armstrong
3.
Pupillary reflex : direct or consensual, afferent=optic, efferent=oculomotor
4.
Color reflex : ishihara plate detects color blindness
5.
Ophthalmoscopy or funduscopy
Abnormalities
•
Section of on optic nerve causes blindness of the affected eye
•
Destruction of fibers in optic chiasm leads to blindness of nasal retina=temporal
field loss (bitemporal hemianopia)
•
Destruction occur in Right optic tract, it will cause: Right temporal retinal blindness
(loss of right nasal field) and Left nasal retina blindness (loss of left temporal field)
•
Myopia: object is in front of retina (cannot detect letters)
•
Hyperopia: object image is behind retina
•
Astigmatism: disorientation in different form in vertical and horizontal plane
•
Multiple sclerosis: demyelination of white mater, occur in 2
P
nd
P
3
P
rd
P
decade, associated
with HH6 infection, manifested by: CharcoAid triad (ataxia, nystagmus, scanning
speech), facial pain, perioral parasthesia, visual disturbance
•
Glaucoma↑IOP
ﻣﺎء
ﺍﺳﻭﺩ
Cataract
ﻣﺎء
ﺍﺑﻳﺽ↑corneal opacity
•
Myosis: caused by morphine, neostigmine (used for dx of myasthaenia gravis)
•
Mydriasis: caused by atropine, amphetamine
•
Scotoma: patient sees black spots
Page3
CNIII Oculomotor nerve
Arises from mid brain, enters to orbit through superior orbital fissure, supplies all
extraocular (except two) and intraocular muscles
Examination
1.
Accomodation test: by focusing on near object (bilateral pupillary constriction
(myosis), convergence of eye balls, increased thickness of retina)
Note: pupillary constrictor= circular fibers, Pupillary dilator= radial fibres
2.
Eyeball movement: each eye examined alone
Abnormalities
:
•
Ptosis: dropping of eyelid
•
Proptosis (exophthalmus): seen in
o
Elevated thyroid hormones
o
Histiocytosis (Hans Schüller)
o
Diabetes insipidus
o
Cavernous sinus thrombosis
•
Squint (strabismus) : uncoordinated muscular tension
•
Horner syndrome: tumor of apex of lung causes destruction to upper cervical
sympathetic or stellate ganglia, leading to the cut of sympathetic supply to head and
neck, manifested by: ptosis, enophthalmos, myosis and no response to pupillary reflex
CNIV Trochlear nerve
Exits through superior orbital fissure, supplies superior oblique muscle
CNV Trigeminal nerve (
)ﻣﻬﻡ ﺟﺩﺍ
Function: sensory to face, scalp, teeth, oral cavity, nasal cavity. Motor to oral and
masticatory muscles
Trigeminal neuralgia: severe facial pain involving one or more of the three divisions causes:
1.
Most common: compression on the nerve by tortuous artery or vein or tumor
2.
Multiple sclerosis
3.
Arteriosclerosis
If alcohol injected to TG ganglion>>necrolysis>>temporary relief (anaesthesia dolorosa)
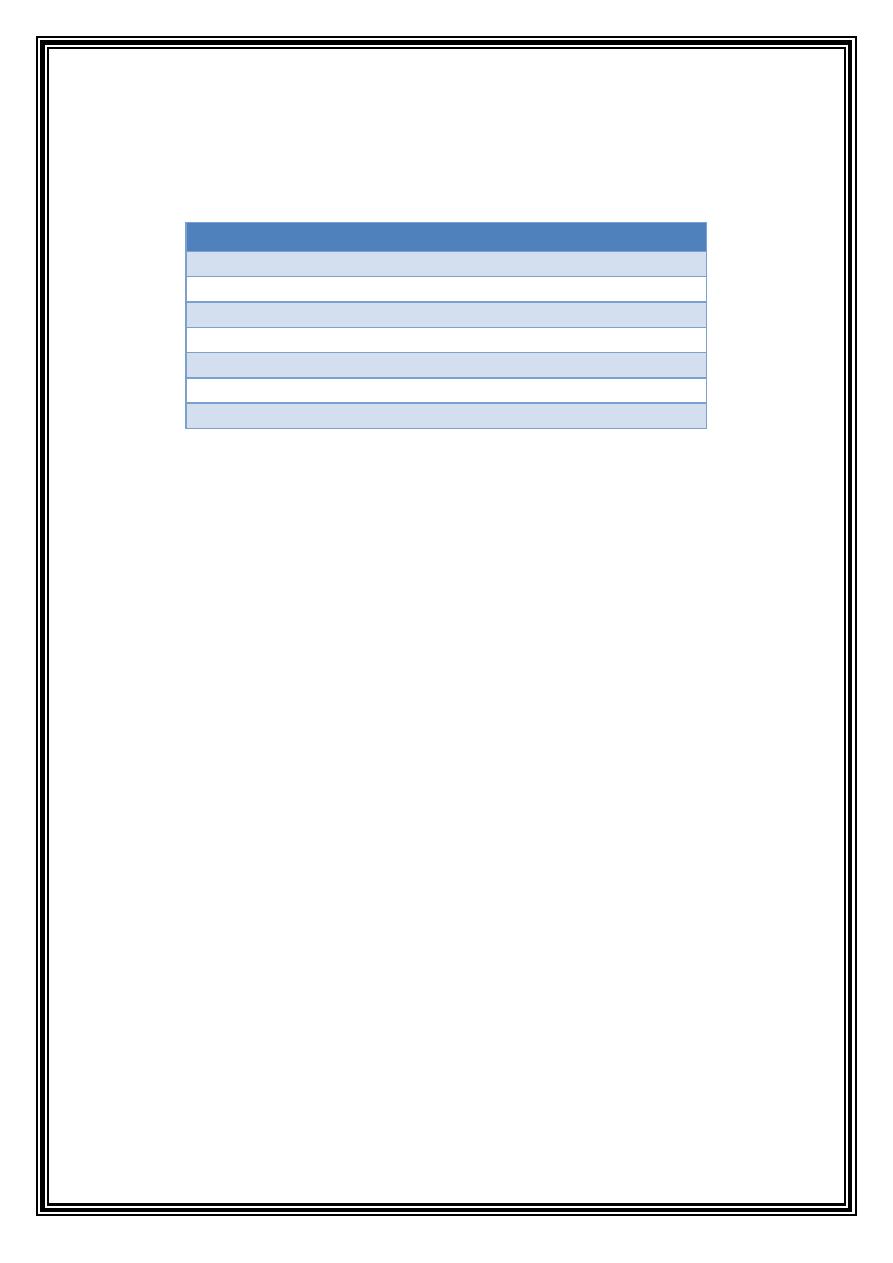
Extraocular muscle
Function
Nerve
Levator palpebrae
Opens palpebral fissure CNIII
Superior rectus
↑↑
Upward
CNIII
Inferior rectus
↓↓
Downward
CNIII
Medial rectus
→← Medially (adduction)
CNIII
Inferior oblique
↗↖
Upward medially
CNIII
Superior oblique
↘↙
Downward medially
CNIV
Lateral rectus
←→ Laterally (abduction)
CNVI
Page4
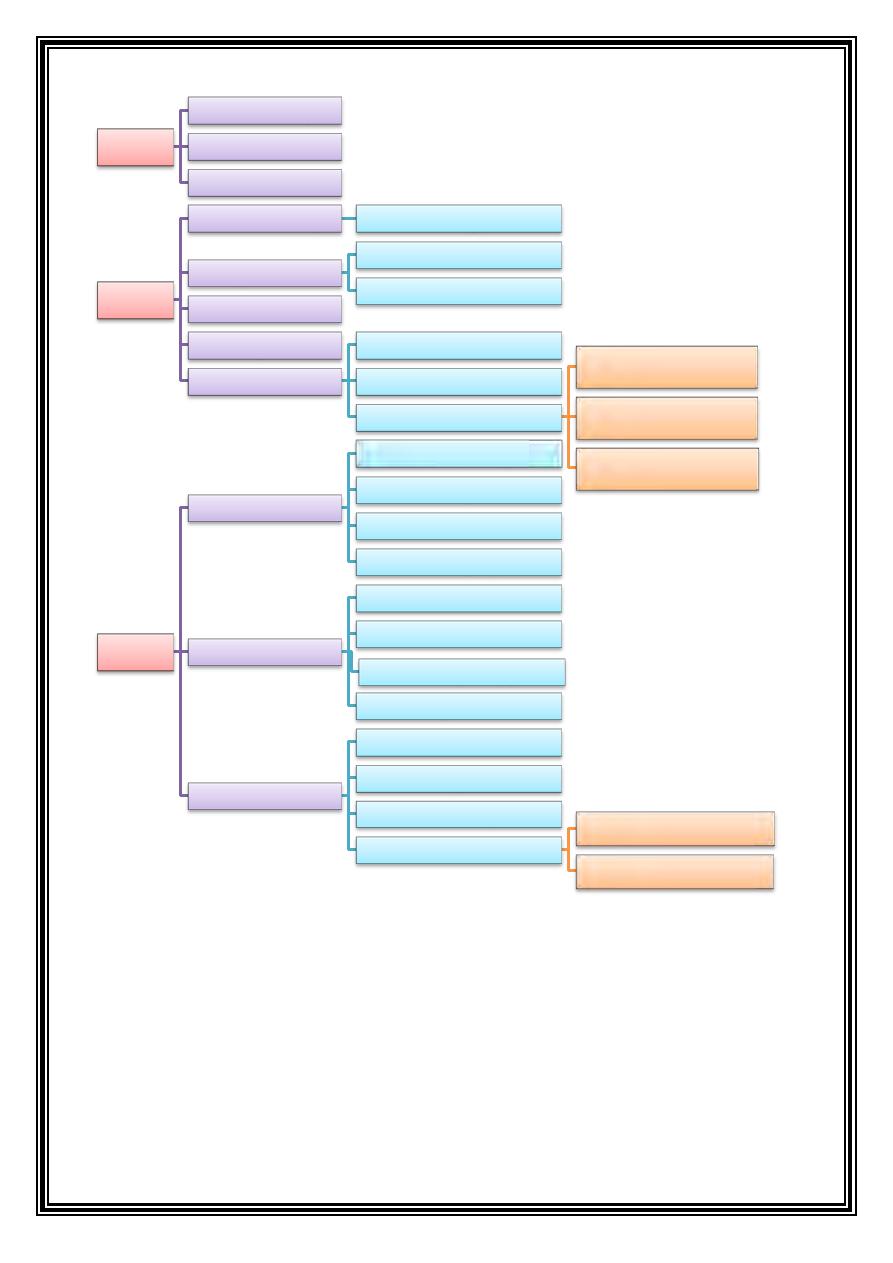
Has 3 branches
: Ophthalmic (Exits through superior orbital fissure), Maxillary (Exits through
foramen rotundum), Mandibular (Exits through foramen ovale)
Examination
1.
Jaw jerk: positive in 50% of patients
2.
Pin prick test
3.
Corneal reflex (blinking): afferent CNV1(ophthalmic), efferent: facial
CNVI Abducent nerve
Originate from pons, exits through superior orbital fissure, supplies lateral rectus, damage
to the nerve causes squint (strabismus) and diplopia
CNV1
Nasociliary
Lacrimal
Frontal
CNV2
Befor exiting
Meningeal
zygomatic
Temporal
Orbital
PSAN
Ganglionic
infraorbital canal
MSAN
ASAN
Infraorbital nerve
Superior labial
lateral nasal
inferior pulpebral
CNV3
Trunk
To medial pterygoid*
Nervus spinosus
To tensor palatini*
To tensor tympani*
Anterior
Massetric*
Temporal*
To Lateral pterygoid*
Long buccal
Posterior
IAN
Lingual
Auriculotemporal
To mylohyoid
mylohyoid*
anterior digastric*
Page5
ﻓﺎﺻﻝ
ﺍﻋﻼﻧﻲ
Meninges
: dura mater, arachnoid, pia mater
Meningitis
: neck stiffness, convulsions, brain abscess
Pituitary
gland
: called master gland because it controls the function of other glands
Anterior lobe
1.
Thyroid stimulating hormone TSH: controls T3(triiodothyronine) and T4(thyroxin)
2.
Growth hormone GH: ↑gigantism, ↓cretinism
3.
Adrenocorticotropic hormone ACTH
4.
Follicular stimulating hormone FSH
5.
Luteinizing hormone LH
6.
Prolactin
Intermediate lobe:
secretes melanocyte stimulating hormone MSH
Posterior lobe
1.
Antidiuretic hormone (vasopressin) used for:
a.
Child nocturnal neurosis
b.
Bleeding disorder for hemophilia and von Wilbrand disease
c.
As vasoconstrictor for dental practice for hypertensive patients, called citapressin
Should be avoided for pregnant women (causes abortion)
2.
Oxytocin: for induction of labor, also ↓ postpartum bleeding after delivery
Pituitary gland tumor:
↑ICP, continuous headache
•
Maxillary sinus>
also called antrum of highmore
Root lodged inside is removed by Caldwell Luc approach (causes devitalization of canine)
•
Function of paranasal sinuses:
1-Decrease weight of skull
2-Resonance of the sound
3-Humidication if inspired air
•
Signs and Symptoms of sinusitis:
1-
morning headache>> continuous pain
exaggerated by position> bending position
2-
In the radiograph show as hazy
radiopacity(water and air)
3-
allergic rhinitis & nasal blockage
4-
Upper teeth sensitivity
5-
tenderness
6-
blurred vision
7-
bradycardia
8-
coma
•
Fiberoptics used for diagnosis of:
1-
interproximal caries
2-
tooth crack
3-
acute sinusitis> more red than normal
4-
cystic hygroma , nasolabial cyst
•
Treatment of sinusitis
1-
nasal decongestant: Nasophrine drop
0T
2-
antihistamine: Alermine 10 mg(causes sedation), Loratadine 10 mg
3-
Massive IV antibiotics ,surgery
•
Chronic sinusitis
>>appears as radiopacity in the wall.
Treated by > Caldwell Luc, Disadvantage> devitalization of canine
•
Sinusitis is life threatening
it causes septicemia and ↑ICP (loss of consciousness)
Page6
Connection
between Pterygoid venous plexus & cavernous sinus by >> Emissary vein
Cranial nerves
pass through cavernous sinus> III, IV, V (branches V1 and V2) and VI
Dexamethasone
>> used to decrease intracranial pressure>>Treatment of coma.
Cranial nerve
pass through superior orbital fissure>>
0T
0T
CNIII, CNIV, CNV1 (ophthalmic), CNVI
Carbamazepine (Tegretol)
0T
:
0T
Drug of choice in palsy
0T
,
0T
CNV neuralgia: 500 mg, Max= 1200mg
Side effect: Blood dyscrasias: Potentially fatal blood cell abnormalities. (eg, agranulocytosis,
aplastic anemia, neutropenia, leukopenia, thrombocytopenia, pancytopenia, and anemias);
Parasympathetic ganglia of head and neck:
A-Ciliary ganglion: A small parasympathetic ganglion lying in the orbit between the optic
nerve and the lateral rectus muscle; it receives preganglionic innervation from the Edinger-
Westphal nucleus by way of the oculomotor nerve, and in turn gives rise to postganglionic
fibers that innervate the ciliary muscle and the sphincter of the iris (sphincter pupillae)
B-Otic ganglion: An autonomic ganglion situated below the foramen ovale medial to the
mandibular nerve; parasympathetic fibers (lesser petrosal) distributed to the parotid gland.
C-Pterygopalatine ganglion: A small parasympathetic ganglion (greater petrosal) in the
upper part of the pterygopalatine fossa, supplying the lacrimal and minor salivary glands.
D-submandibular ganglion: A small parasympathetic ganglion suspended from the>> lingual
nerve; its branches go to the submandibular and sublingual glands; its preganglionic fibers
come from the superior salivatory nucleus by way of the chorda tympani.
ﻧﻬﺎﻳﺔ
ﺍﻟﻔﺎﺻﻝ
ﺍﻹﻋﻼﻧﻲ
ﻋﻭﺩﺓ
ﻟﻸﻋﺻﺎﺏ
ﺕّﺳﻟﺍ
ﺍﻟﺑﺎﻗﻳﺔ
Page7
CNVII Facial nerve
Arises from pons, enters internal acoustic meatus, exits from stylomastoid foramen
•
Gives parasympathetic innervation to lacrimal gland (through greater petrosal) and to
submandibular and sublingual salivary glands (through chorda tympani)
•
Innervate anterior 2/3 of tongue by special sensation (taste)
•
Supplies stapedius muscle (smallest muscle in human body)
•
Supplies muscles of facial expression+ posterior belly of digastric+ posterior auricular m.
MUSCLES OF FACIAL EXPRESSION
1-
Occipitofrontalis:
Elevates eyebrows, wrinkles forehead
2-
Corrugator supercilii:
Eyebrows down and medial
3-
Orbicularis oculi:
Closes eyelids
4-
Procerus:
Wrinkles skin over nose
5-
Nasalis:
Draws ala of nose downward
6-
Depressor septi:
Constricts nares
7-
Orbicularis oris:
Closes lips
8-
Levator anguli oris:
Elevates angle of mouth medially
9-
Levator labii superioris:
Elevates upper lip, dilates nares
10-
Levator labii superioris alaeque nasi:
Elevates upper lip, elevates ala of nose
11-
Zygomaticus major:
Draws angle of mouth up and back (smile)
12-
Zygomaticus minor:
Elevates upper lip
13-
Depressor labii inferioris:
Depresses lower lip
14-
Depressor anguli oris:
Depresses angle of mouth
15-
Risorius:
Retracts angle of mouth
16-
Buccinator:
Holds cheeks tight toward teeth
17-
Mentalis:
Elevates and protrudes lower lip
18-
Auricularis:
Retracts and elevates ear
Branches of facial nerve after exiting through stylomastoid foramen
1.
Posterior auricular muscle
2.
Nerve to posterior belly of digastric
Branches of facial nerve after entering parotid gland
1.
Temporal (muscles near orbit and forehead)
2.
Zygomatic (muscles of orbital and infraorbital area)
3.
Buccal (muscles of cheek)
4.
Marginal mandibular (muscles of chin and lower lip)
5.
Cervical (platysma)
Sensory branch of facial nerve called>>
nervous intermedius
>> supply geniculate ganglion
(which innervates the tongue, palate, pharynx, external auditory meatus)
Page8
Examination:
1.
Inspection: symmetry of the face at rest, smiling and blinking (to dx paralysis)
2.
Motor function: eyebrows elevation, forehead wrinkling, teeth showing, air blowing
against closed mouth, air blowing through nose
3.
Taste sensation: by sweet, salty or bitter compounds (Ageusia= loss of taste)
4.
Schirmer test: place blotting paper beneath lower eye led to cause provoked
secretion, remove after 5 minutes, 10mm of it should be wet, if less >xerophthalmia
Facial paralysis, types
It is either upper or lower motor neuron lesion.
Upper motor neuron lesion (UMNL) leads to paralysis in lower part of the face on one side,
this is because upper part of the face has bilateral innervation centrally
Lower motor neuron lesion (LMNL) leads to paralysis of upper and lower parts of the face
Explanation
Upper face>>take innervation from the 2 hemisphere
Lower face>>contralateral innervation (like speech center>> aphasia: inability to speech)
If central facial palsy (facial root in the brain)>>> patient can still wrinkle his forehead
But if peripheral facial palsy>> can wrinkle>> in contralateral side of damage, but cannot
wrinkle in the same side
Intracranial causes of facial palsy
1.
Trauma , temporal bone fracture
2.
Tumor of pituitary gland
3.
Ramsay hunt syndrome
4.
CVA (most common)
5.
Multiple sclerosis
6.
Lyme disease
7.
HIV infection
Extracranial causes of facial palsy
1.
Tumor of parotid gland or surgery
2.
Melkersson Rosenthal syndrome
3.
Misplaced local anaesthesia
4.
Heerfordt syndrome
5.
Bell's palsy
Post herpetic neuralgia:
pain remains after a month after the mucocutaneous lesion of
shingles have healed; occur due to inflammation and fibrosis around the nerve.
Responds well to Tegretol. It can be prevented by: corticosteroids, and acyclovir
Ramsay Hunt syndrome
(herpes zoster oticus) occurs when a shingles infection affects the
facial nerve near one of the ears. In addition to the painful shingles rash, Ramsay Hunt
syndrome can cause facial paralysis and hearing loss in the affected ear.
High doses of antiviral medications and corticosteroids are used to treat it
Heerfordt's syndrome
a triad of symptoms (rare symptom) including bilateral parotid
swelling (sarcoidosis), uveitis, and facial nerve involvement that is usually manifested as a
transient facial nerve paralysis.
Page9
Melkersson–Rosenthal syndrome
is a rare neurological disorder characterized by:
1-
Recurring facial paralysis,
2-
Swelling of the face and lips (usually the upper lip),
0T
3-
Fissured tongue.
The cause of Melkersson–Rosenthal syndrome is unknown, but there may be a genetic
predisposition. It can be symptomatic of Crohn's disease or sarcoidosis.
Bell's palsy
>> transient hemifacial paralysis of up & lower affected sides, patient complaint:
1-
cannot wrinkle, cannot close eye
2-
dropped eye lid and mouth corner
3-
drooling of saliva
4-
accumulation of food
5-
loss of taste sensation
6-
dry eye and mouth
Cause is unknown but could be a complication of HSV infection, affects age 20-50
How to differentiate between Bell's palsy and CVA
Bell's palsy: (LMNL) upper and lower part affected, cannot close eyes or wrinkle forehead
CVA: (UMNL) only lower part is affected, can close eye and wrinkle forehead
Why there is a difference between manifestation of facial and hypoglossal paralysis
Facial nerve: face deviated to unaffected side due to pulling action of unaffected muscles
Hypoglossal: tongue deviated to affected side due to pushing action of unaffected muscles
Does CVA affect emotional expressions?
No it doesn’t, because emotions are supplied by limbic system
Stapedius muscle:
smallest muscle in human body, originate from stapes insert in oval
window of the ear. Paralysis to this muscle will cause loudness of the voice (hyperacusis)
CNVIII Vestibulocochlear nerve
Name: vestibular (balance), cochlear (hearing). It is also called auditory or acoustic nerve.
It is the only cranial nerve that remains inside the skull, it enters IAM with CNVII
Examination:
1.
Weber test
:
a tuning fork of a frequency of 256-512Hz is used to differentiate
conductive from sensorineural deafness. It is placed at the vortex of the skull. The
patient is asked to determine whether the sound is more audible on one side
compared to the other. In conductive hearing loss, the sound is lateralized to the
deaf ear whereas in sensorineural hearing loss the sound is lateralized to the better-
hearing ear.
2.
Rinne test: the base of the vibrating fork is placed over the mastoid. The patient is
asked to indicate when the sound is no longer perceived, and at that time, the fork is
immediately moved so that the vibrating ends are directly in front of the external
auditory meatus. The sound should be audible; if not, this is an indication of
conductive hearing loss
Page10
Conductive deafness: wax, perforation of tympanic membrane, accumulation of fluid
around tympanic membrane, otosclerosis of ear bone
Sensorineural deafness: damaged organ of corti, acoustic neuroma, fractured petrous bone
3.
Oculocephalic reflex (Hallpike test or doll's eye maneuver)
When the head is suddenly tilted to one side, the eyeballs tilt to the other side
4.
Oculovestibular reflex (caloric test)
•
Hot water 37+7=44
P
o,
P
and cold water 37-7=30
P
0
•
When hot water is applied, the head tilts to the same aside
•
When cold water is applied, the head tilts to the opposite side
•
When hot and cold water are applied the head tilts upward, this is to check for
the vitality of brain stem (if negative>brain stem death)
5.
Auriscope (otoscope): direct visualization of tympanic membrane and EA canal
CNIX Glossopharyngeal nerve
From medulla oblongata, passes jugular foramen, forming superior, inferior, otic ganglia.
Function:
1.
Supplies stylopharyngeus muscle
2.
Innervates posterior 1/3 of the tongue
3.
Innervates posterior 1/3 of auditory canal
4.
Innervates palatine tonsils
Examination
by gag reflex: afferent: CNIX, efferent CNX
CNX Vagus nerve
From medulla oblongata, passes jugular foramen. It is the largest cranial nerve
Descends to abdomen to innervate GIT, heart, lungs
Function
Motor to heart, lungs and visceral organs, muscles of soft palate (except tensor palatini)
Sensory: taste, cutaneous fibres from tympanic membrane and posterior part of EAC
Rubbing the external acoustic meatus causes nausea due to CNX stimulation
Examination
1.
Observe movements of the palate and uvula by asking the patient to say 'aah .'
2.
Assess tonsillar, palatal and upper pharyngeal tactile sensation using a dampened swab
stick and tongue depressor .
3.
The gag reflex may be elicited by touching either the tonsil or pharynx. Test each side
separately. Testing for the gag reflex is unpleasant. It should be performed only if there
is other evidence of nerve paresis.
4.
Assess the volume and quality of the patient's speech, noting if the voice is hoarse or has
a nasal quality.
5.
Ask the patient to cough to determine whether this is more nasal or bovine than normal.
6.
Ask the patient to puff out the cheeks, to test palatal closure of the nasopharynx.
Page11
The CNIX and CNX are involved in several reflexes:
•
The gag reflex involves constriction and elevation of the pharynx and palate in
response to tactile stimulation of the upper pharynx and tonsils.
•
The oculocardiac reflex (slowing of the heart rate after orbital compression )
•
The carotid sinus reflex (carotid body tumor is also called potato tumor)
Muscles of soft palate (all supplied by CNX except tensor palatini)
1.
Palatoglossus
2.
Palatopharyngeus
3.
Levator palatini
4.
Uvula muscle
5.
Tensor palatini
(supplied by CNV)
Damage to CNX causes:
dysphonia, deviation and defective mobility of soft palate
Trotter's syndrome:
nasopharyngeal or retropharyngeal carcinoma, caused by Epstein Barr
virus, manifested by deviation of soft palate, unilateral deafness, cervical
lymphadenopathy, unilateral headache. Diagnosed by C.T. and biopsy. This tumor is
radiosensitive, so the use of radiograph is to diagnose and treat it.
CNXI Accessory nerve
From medulla oblongata, passes jugular foramen. Supplies palate, pharynx, tonsils,
trapezius and sternocleidomastoid muscles
Examination:
head rotation, shoulder shrug and elevation against force
CNXII Hypoglossal nerve
From medulla oblongata, passes hypoglossal canal. Supplies all intrinsic and extrinsic
muscles of the tongue (except palatoglossus by vagus)
Examination
1.
Asses speech by saying (Laa) to see upward movement of the tongue
2.
Assess movement of the tongue from side to side
3.
Ask patient to protrude tongue to see asymmetry
Abnormality
: bulbar or pseudobulbar lesions cause deviation to the side of the lesion
