Lec7 DERMATOLOGY dr.Omar
Bacterial skin infections Viral skin infections Fungal skin infectionsBacterial skin infections
Why does skin get infected? There are multiple types of bacteria which are normally present on the skin. For example: Staphylococcus epidermidis and yeasts The presence of bacteria does not automaticallylead to a skin infection
What is the difference between colonisation andinfections??? Colonisation: Bacteria are present, but causing no harm Infection: Bacteria are present and causing harm.A break in the epidermal integrity can alloworganisms to enter and becomepathogenic. This can occur as a result oftrauma, ulceration, fungal infection, skindisease such as eczema
Impetigo A highly infectious skin disease, which commonly occurs in children. The causative organism is usually Staphylococcus Aureus (>90% cases1), but less often can be strep pyogenes. Begins as a vesicle, which may enlarge into a bulla. Weeping, exudative area with characteristic honey coloured or golden, gummy crusts, which leave denuded red areas when removed. May present as macules, vesicles, bullae or pustules Bullae are more prominent in staphylococcal infection and in infantsImpetigo
Treatment: Mild localised cases - use topical antibioticPolyfax Widespread or more severe infections –use systemic antibiotics, such asflucloxacillin (or erythromycin if penicillinallergic)
Folliculitis Inflammation of the hair follicle. Presents as itchy or tender papules and pustules at the follicular openings. Complications include abscess formation and cavernous sinusthrombosis if upper lip, nose or eye affected. Most common cause is Staph Aureus. Other organisms to consider include: Gram negative bacteria – usually inpatients with acne who are on broad specantibiotics Pseudomonas (“Hot tub folliculitis”) Yeasts (candida and pityrosporum)Folliculitis treatment Topical antiseptics such as Chlorhexidine Topical antibiotics, such as Fusidic acid or Mupirocin More resistant cases may need oral antibioics such as Flucloxacillin Hot tub folliculitis – ciprofloxacin2 Gram negative – trimethoprim
Cellulitis Infection of the deep subcutaneous layer of the skin Presents as a hot, tender area of confluent erythema of the skin Can cause systemic infection with fever, headache and vomiting. Erysipelas is more superficial and has a more well demarcated border
Erysipelas
Cellulitis
Streptococcus – Group A Strep Pyogenes. Others include Group B, C, D strep, Staphylococcus Aureus, haemophilus influenzae (children) and anaerobic bacteria (e.g Pasteurella spp. After animal bites)
Treatment of cellulitis Oral Flucloxacillin or erythromycin if allergic Co-amoxiclav in facial cellulitis If severe systemic upset, may require admission for IV antibiotics. After the acute attack has settled, especially in recurrent episodes – consider the underlying cause
Orbital cellulitis – refer urgently
Staphylococcal Scalded Skin Syndrome A superficial blistering condition caused by exfoliative toxins ofcertain strains of Staph Aureus Usually in children less than 5 yrs old Characterised by blistering and desquamation of the skin andNikolsky's sign (shearing of the epidermis with gentle pressure),even in areas that are not obviously affected begins with a prodrome of pyrexia and malaise, oftenwith signs and symptoms of an upper respiratory tract infection discrete erythematous areas then develop and rapidlyenlarge and coalesce, leading to generalized erythema - often worse inthe flexures with sparing of the mucous membranes large, fragile bullae form in the erythematous areas andthen rupture Complications include hypothermia, dehydration and secondary infection. Treatment: ABC, refer urgently for IV antibiotics and fluids, may needreferral to tertiary burns centre
What is the diagnosis?Painful red nodule
Furunculosis (boils) and carbuncles Deeper Staphylococcal abscess of the hair follicle Coalescence of boils leads to the formation of a carbuncle Treatment is with systemic antibiotics and may need incision and drainage. Consider looking for underlying causes, such as diabetes
Erythrasma Colonisation of axillae or groin with Corynebacterium Minutissimum. Presents as a fine, reddish brown rash in the flexures, which is sharply marginated. Often misdiagnosed as a fungal infection Woods light illumination produces acharacteristic coral-pink fluorescence. Treatment is with topical fusidin cream
.
When you use the Wood’s light, the skin lesionshows a dramatic coral pink fluorescence.
Viral Skin InfectionsViral warts and verrucas Caused by human papilloma virus Main types, common, plane and plantar Very common Disappear spontaneously eventually If treatment is needed, options include: Salicylic acid topically – needs daily treatment and cantake months Cryotherapy Imiquimod cream
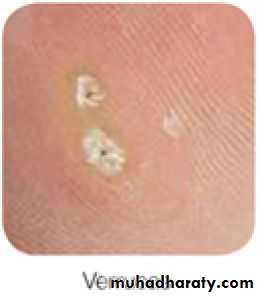
Molluscum contagiosum Caused by MC virus Common in children, but can occur at any age Spread by direct contact Presents as multiple small, pearly, dome-shaped papuleswith central umbilication Can occur at any site Usually resolve spontaneously in 6-18 months Resolution is heralded by the development of erythemaaround the lesions. Treatment is not usually necessary – simple reassuranceand advice about reducing transmission. If treatment is necessary, options include: Piercing the lesion with an orange stick tipped with iodine Curretage imiquimod cream
Herpes Zoster (Shingles ) Caused by reactivation of the chickenpox viruswhich has lain dormant in the dorsal root orcranial nerve ganglia Rash is preceded by a prodromal phase of upto 5 days of tingling or pain Then develop painful groupedvesicles/pustules on a red base in adermatomal distribution. Most common in thoracic and trigeminal areas Lesions become purulent, then crusted Healing takes place in 3-4 weeks
Shingles treatment Aciclovir 800mg 5 times daily, for 7 days Rest, analgesia usually gabapentine.Complications include: Post herpetic neuralgia Secondary infection Guillain Barre Syndrome Occular diseasePost-herpetic NeuralgiaPain lasting longer than 3 months after therash.The followings are risk factors fordeveloping post-herpetic neuralgia?A: Older ageB: More severe pain during the eruptionC: Severely inflamed rashD: Prodromal pain in dermatome
Herpes Simplex Virus A highly contagious infection spread by directcontact HSV 1 : also commonly called “coldsore” HSV 2 usually presents on the genitalia Primary infection is usually asymptomatic. Recuurent infection presents as acute, painfulgingivo-stomatitis with multiple small intra/perioral ulcers (but any site could be affected).Associated with fever, malaise andlymphadenopathy. Clinically: Grouped umbilicatedvesicles/pustules on erythematous base.
Treatment: Topical aciclovir can be used: 5 times dailyfor 5 days. Reduces duration of attack andduration of viral shedding. The correct dose of aciclovir for HSV is200mg 5 times daily for 5 days
Genital herpesHerpetic WhitlowHerpes Simplex Keratitis