1
Fifth stage
Dermatology
Lec 6
د.عمر
22/11/2015
Atopic Dermatitis
Atopic dermatitis (AD) is a chronic, highly pruritic, eczematous skin disease
that follows patients from early childhood into puberty and sometimes
adulthood.
Also referred to as eczematous dermatitis, the disease often has a
remitting/flaring course, which may be exacerbated by social,
environmental, and biological triggers.
Prevalence
• Approximately 15% in the US and Europe
• This represents a profound increase in recent years (from as low as 3% in
1960)
Natural History of Atopic Dermatitis
• 60% of pts develop AD by 1 year of age.
• 85% of pts develop AD by age 5.
• Earlier onset often indicates a more severe course.
• Many cases resolve by age 2, improvement by puberty is common.
• 50%-60% of pts develop respiratory allergies or asthma.
• 80% of occupational skin disease occur in atopics.
• It is rare to see AD after age 50.
Filaggrin
• Filaggrins are filament-associated proteins which bind to keratin fibers in
epithelial cells
• Individuals with truncation mutations in the gene coding for filaggrin are
strongly predisposed to a severe form of dry skin, ichthyosis vulgaris,
and/or eczema
• It has been shown that almost 50% of all severe cases of eczema may have
at least one mutated filaggrin gene.
2

3
Infantile atopic dermatitis
• Infants less than one year old often have widely distributed eczema. The
skin is often dry, scaly and red with small scratch marks made by sharp
baby nails.
• The cheeks of infants are often the first place to be affected by eczema +-
head +- body.
• The diaper area is frequently spared due to the moisture retention of
diapers. Just like other babies, they can develop irritant diaper dermatitis,
if wet or soiled diapers are left on too long.
Toddlers and pre-schoolers
• As children begin to move around, the eczema becomes more localized
and thickened. Toddlers scratch vigorously and the eczema may look very
raw and uncomfortable.
• Eczema in this age group often affects the extensor (outer) aspects of
joints, particularly the wrists, elbows, ankles and knees. It may also affect
the genitals.
• As the child becomes older the pattern frequently changes to involve the
flexor surfaces of the same joints (the creases) with less extensor
involvement. The affected skin often becomes lichenified i.e. dry and
thickened from constant scratching and rubbing,
• In some children the extensor pattern of eczema persists into later
childhood.
Atopic dermatitis in school-age children
• Older children tend to have the flexural pattern of eczema and it most
often affects the elbow and knee creases. Other susceptible areas include
the eyelids, earlobes, neck and scalp.
• Many children develop a 'nummular' pattern of atopic dermatitis. This
refers to small coin-like areas of eczema scattered over the body. These
round patches of eczema are dry, red and itchy and may be mistaken for
ringworm (a fungal infection).
4
• Mostly the eczema improves during school years and it may completely
clear up by the teens, although the barrier function of the skin is never
entirely normal.
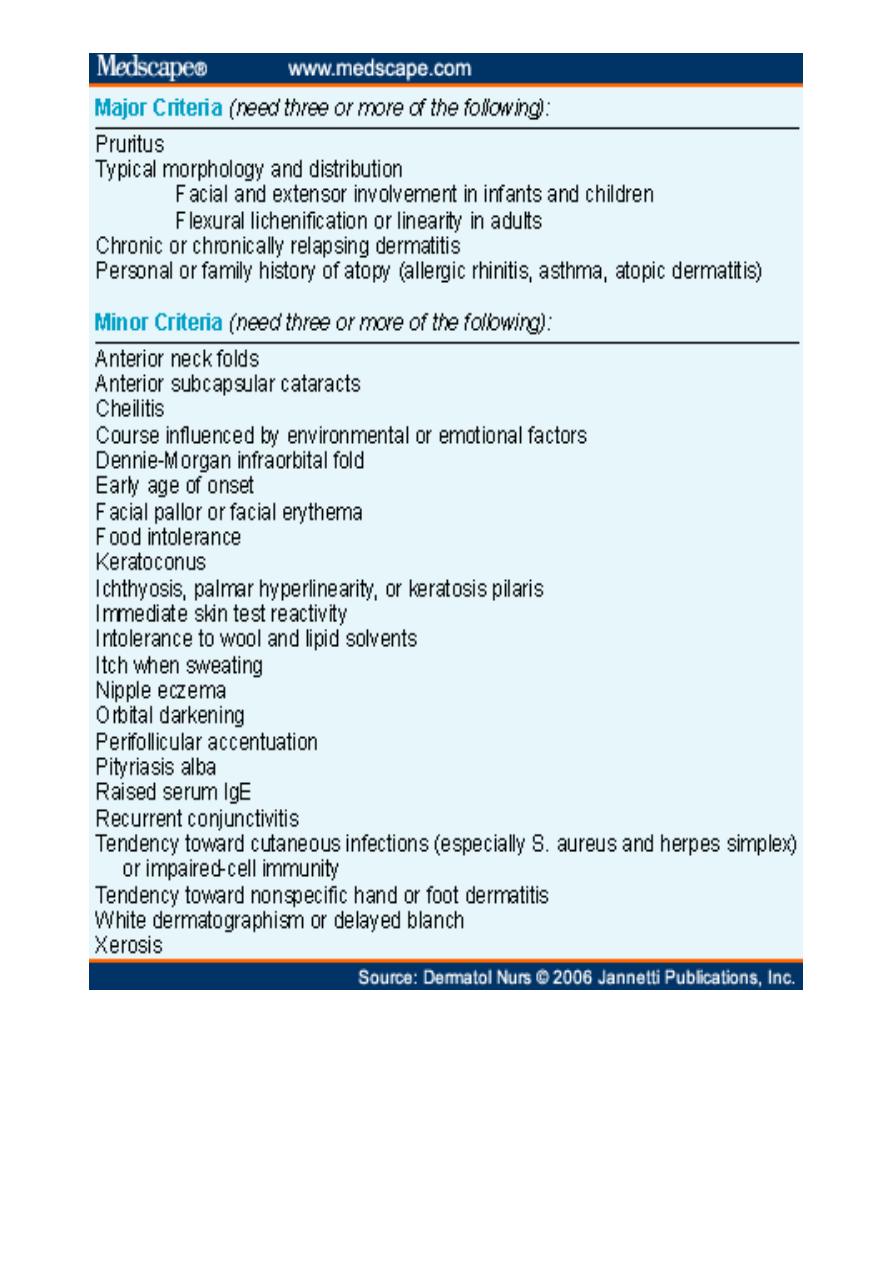
Ichythosis vulgaris
Xerosis (dry skin)
Lichenification
5
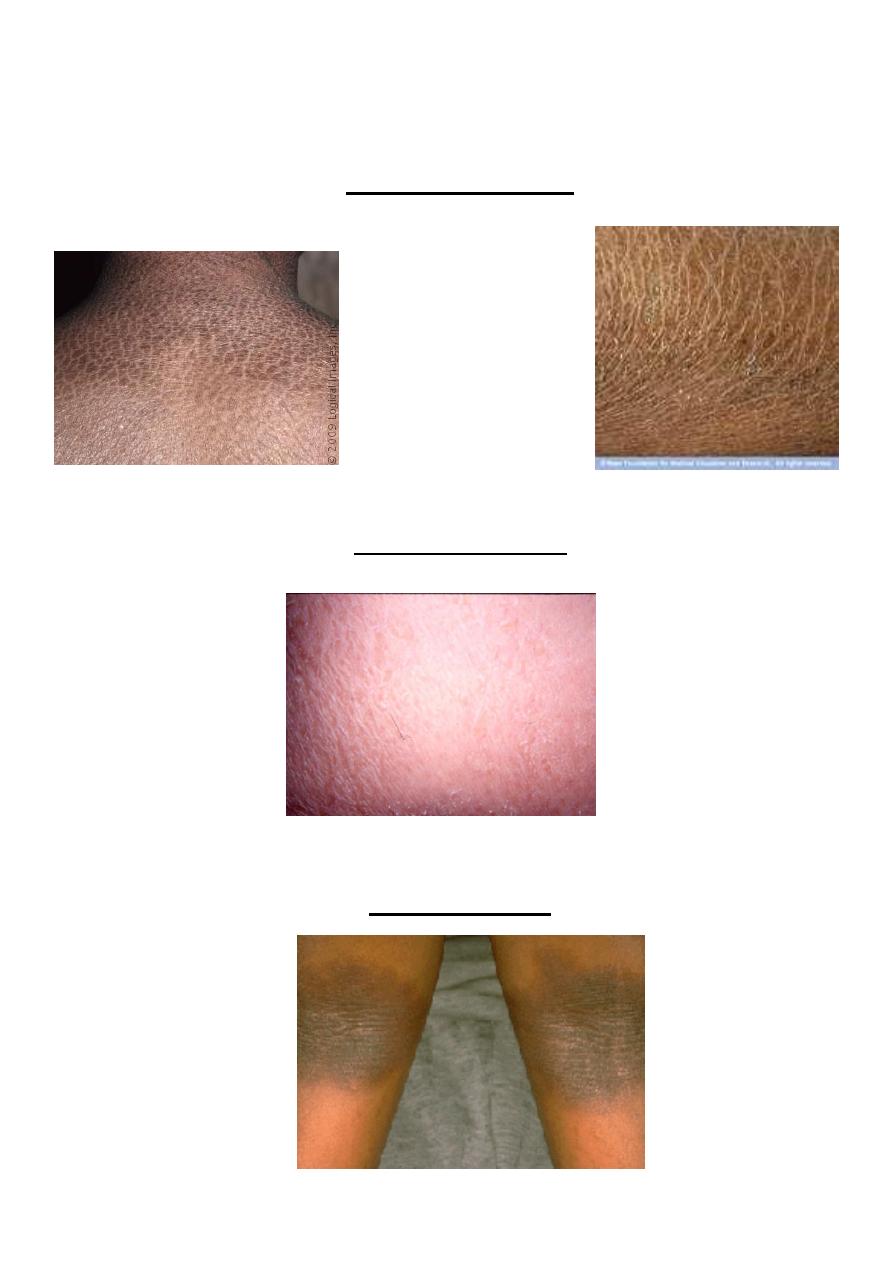
Keratosis pilaris
Palmar hyperlinearity

6
Triggers
• Irritants
Wool
Soaps/detergents
Disinfectants
“Occupational”
Tobacco smoke
• Microbial agents
Staph aureus
Viral infection
?Dermatophytes
Heat/Sweating
Contactants
incl. Dust mites
Psychological
Foods (IgE-induced) vaso-dilatory items
Aeroallergens
Hormones
Climate
(Preventative)
Managing AD
1) Prevent “scratching” or rubbing : apply cold compresses to itchy skin
2) Carefully eliminate all the triggers of itch
a) environmental, occupational, and temperature control
b) bathing – soapless cleansers, Dove
c) LUBRICATION , LUBRICATION , LUBRICATION

7
(Palliation)
Managing AD
Topical anti-inflammatory agent
:
a) corticosteroids (ointments>creams)
more potent - when “acute”
least potent needed for “chronic”
b) Tacrolimus 0.1%, 0.03% ointment
Pimecrolimus 1% Cream
