Dehydration
OBJECTIVES
1-What is state of dehydration.
2-Physiology of fluids in a body of a child.
3-Mechanisms and types of dehydration.
4-Approach to diagnose and correct
dehydration according to degrees and
types .
Dehydration:
It is the most important complication of watery
diarrhea and vomiting .
It is the loss of water and electrolytes due to
diarrhea and vomiting .
Normal Intestinal physiology:
The intestine have an important role in
balancing water and electrolytes and any
abnormality will lead to disturbance.
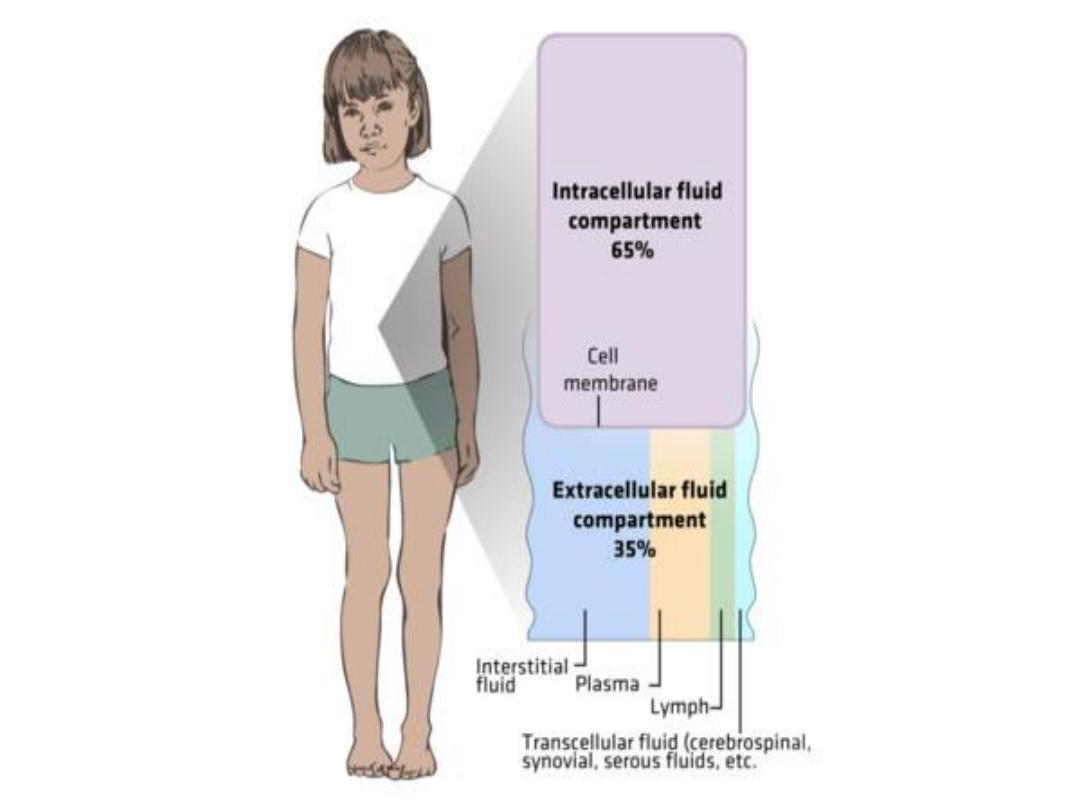
In term baby the total body water is
approximately70%-75% of body Water. Post
nataly the TBW will be adjusted to approx.
65% of the total body wt. This fraction
remains constant until puberty, when the
TBW decreases to 55-60% of the body wt.
*Approximately 2/3 of the TBW is intracellular
& 1/3 is extra cellular.
.
These two fluids are separated by the cell
membranes of the which is water permeable.
*Normally the volume of both ECF & ICF do
not change because the conc. of dissolved
particles are identical on each side of the
membrane
*The normal osmolality is 285 mosm/L.
*Normally Na,Cl &HCO3 ions are primarily
excluded from most of the cellular
environment whereas K ion is maintained
within the cell.
*In addition to the iso-osmolality maintained
between fluid compartments,electronaturality
is also maintained within body fluids so that
the conc. of Cations are equal to the conc.
of the Anions.
Extra cellular fluid includes(ECF):
1-Plasma water (5-7%) of body weight.
2-Interstitial fluid , ISF,(25-30%) of body weight.
3-Trans cellular fluid (1-3%) of body weight. It
includes CSF,GIT, bile, intra-ocular, pleural and
peritoneal fluids.
4-Bone fluids and connective tissue( minimum
amount).
*When the volume of the ISF is depleted poor
skin turger, depressed fontanels and
sunken eyes result.( Signs of dehydration).
*Whereas an expanded ISF volume will result
in edema.
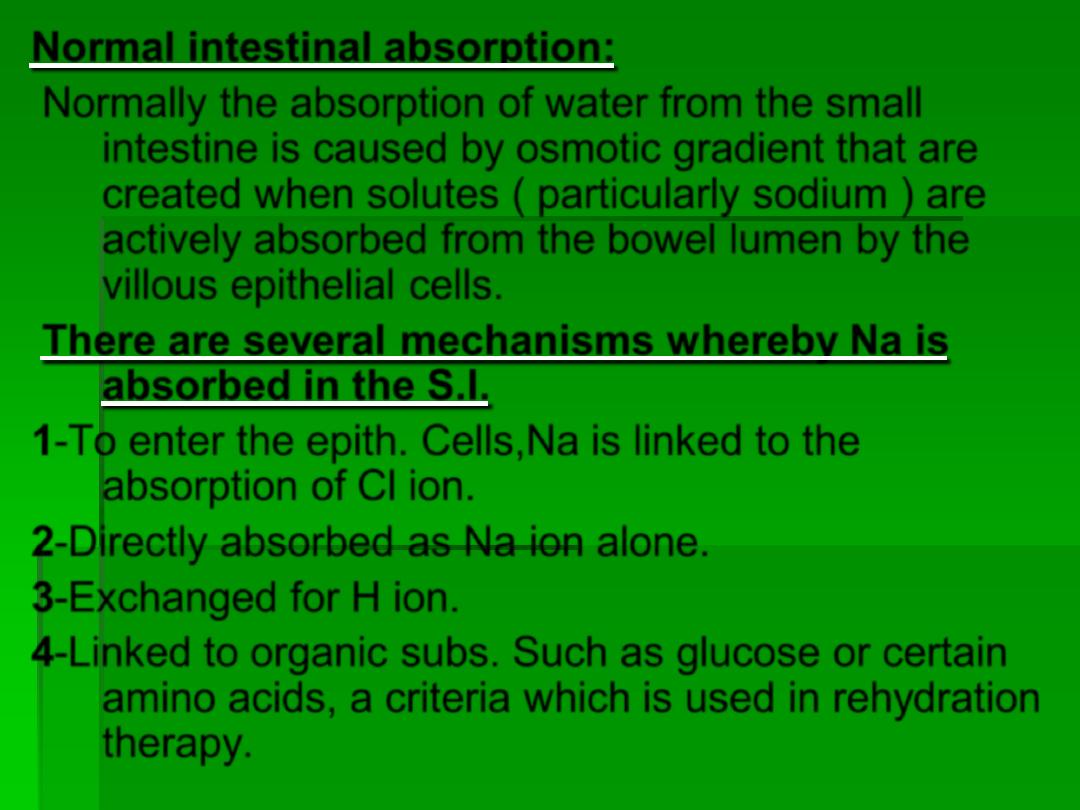
Normal intestinal absorption:
Normally the absorption of water from the small
intestine is caused by
osmotic gradient
that are
created when solutes (
particularly sodium
) are
actively absorbed from the bowel lumen by the
villous epithelial cells.
There are several mechanisms whereby Na is
absorbed in the S.I.
1-To enter the epith. Cells,Na is linked to the
absorption of Cl ion.
2-Directly absorbed as Na ion alone.
3-Exchanged for H ion.
4-Linked to organic subs. Such as glucose or certain
amino acids, a criteria which is used in rehydration
therapy.
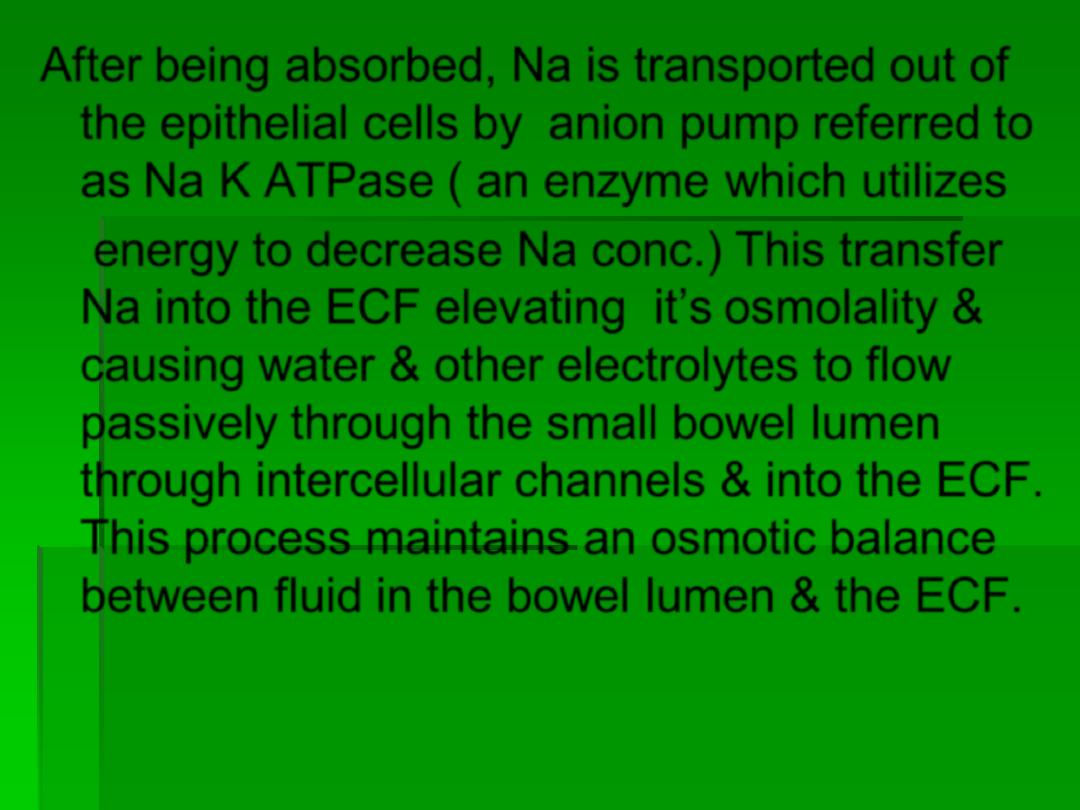
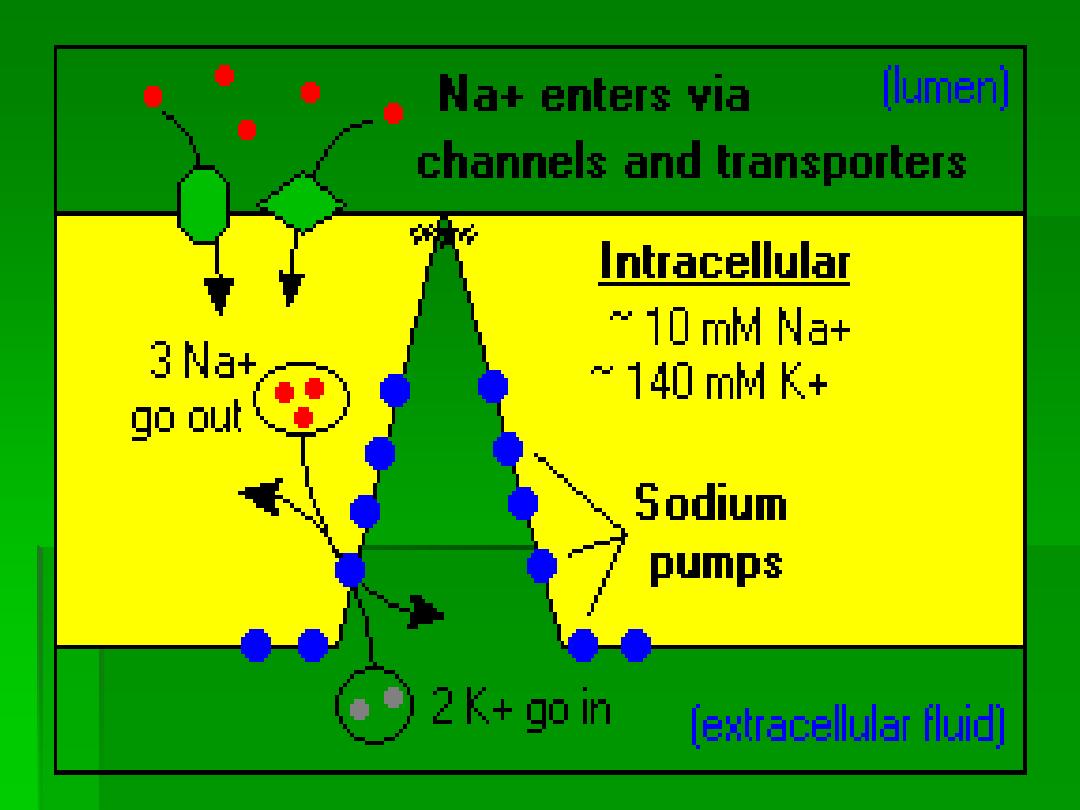
After being absorbed, Na is transported out of
the epithelial cells by
anion pump
referred to
as
Na K ATPase
( an enzyme which utilizes
energy to decrease Na conc.) This transfer
Na into the ECF elevating it’s osmolality &
causing water & other electrolytes to flow
passively through the small bowel lumen
through intercellular channels & into the ECF.
This process maintains an osmotic balance
between fluid in the bowel lumen & the ECF.
Mechanisms of dehydration:
1-There is decrease in the extra cellular fluid
volume ( Incr. loss)---- increase pulse
rate --- increase output in the phase of
the decrease stroke volume.
2-Decrease tissue perfusion leading to:
A-Impair renal function----metabolic acidosis &
uremia.
B-Anaerobic metabolism--- lactic acidosis.
3-Decrease calories intake------ metabolic
acidosis.
Normally:
Absorption & secretion of water & electrolytes
occur throughout the intestine.
E.g.,
Adult drinks 2 liters / day + 7 liters /day saliva,
stomach, panc, liver)
These fluids are delivered to the intestine and
absorbed
by the
villi
and at the same time are
secreted
by the
crypts
of the intestinal epithelium .
This will cause a 2 directional flow of water and
electrolytes between int. lumen & the blood. Since
absorption is normally > than secretion, the net
result is fluid absorption.
Factors that make infants more affected
than adult by dehydration:
1-Total body water in infants is higher than
adult (70-75%) vs.(55%-60)
2-Increase metabolic rate in infancy.
3-Larger body surface area to volume.
4-Fever will increase the fluid loss.
5-Anorexia and decrease fluid intake.
6-Easily compromised renal function.
7-Frequency of gastroenteritis in young infants
is more than adults.
Principles of rehydration therapy:
1-Initial therapy:
a- For rapidly expanding the ECF volume.
b- Improving the circulatory dynamics.
c- To improve renal function.
2- Subsequent therapy:
To replace the remaining
ICF & ECF deficit of
water and electrolytes at
a slower rate with Na first before the K
replacement.
3-Suplemental therapy :return to normal
nutritional status by oral feeding as soon as
possible.
The rehydration has 3 phases:
1-Rehydration phase.
2-Maintenance phase.
3-On going phase.
Oral rehydration solution (ORS):
It is also called ( Dextrolyte) .
1-It is given in acute diarrhea with No dehydration
state to prevent dehydration
.
2-
Also given for rehydration in Some
dehydration (mild to moderate ) state.
3- It is given for the on going loss.
Composition of ORS:
NaCl--------------3.5g/l
NaHCO3---------2.5g/l
KCl---------------1.5g/l
Glucose----------20g/l
This is dissolved in one liter of clean water and is
given by spoon gradually to avoid acute gastric
distention which causes vomiting. It is used for only
24 hours .
Concentration of ORS:
Na------------------90mmol/l
HCO3--------------30mmol/l
K--------------------20mmol/l
Cl-------------------80mmol/l
Glucose------------111mmol/l

Physiological bases of ORS:
Based on the principle that intestinal absorption
of Na (& thus other electrolytes and water ) is
enhanced by active absorption of certain food
molecules such as glucose ( which is derived
from the break down of sucrose or cooked
starches) or a. a.( which are derived from the
breakdown of proteins and peptides. This
process continues to function normally during
secretory diarrhea, whereas other pathways
of intestinal absorption of Na are impaired.
Limitation of ORS:
1-Inappropriate for initial treatment of severe
dehydration.
2-Patients with paralytic ileus and abdominal
distention.
3-Patients with inability to drink. Here we can
introduce the ORS through a nasogastric tube.
ORS is ineffective in :
1-Patients with very high purging rate (>15
ml/kg/hour)
2-Patients with severe intractable vomiting.
3-Glucose malabsorption ( rare).
Indication of IV fluid therapy:
1-Shocked patient.
2-Severe dehydration.
3-High purging rate.
4-Repeated vomiting.
5-Severe gastric distention.
Assessment of dehydration:
By 2 methods:
1-According to the degree of dehydration .No, some
(mild
–moderate) and severe dehydration.
2-According to the type of dehydration.( Iso, hypo or
hypernatremic dehydration) .
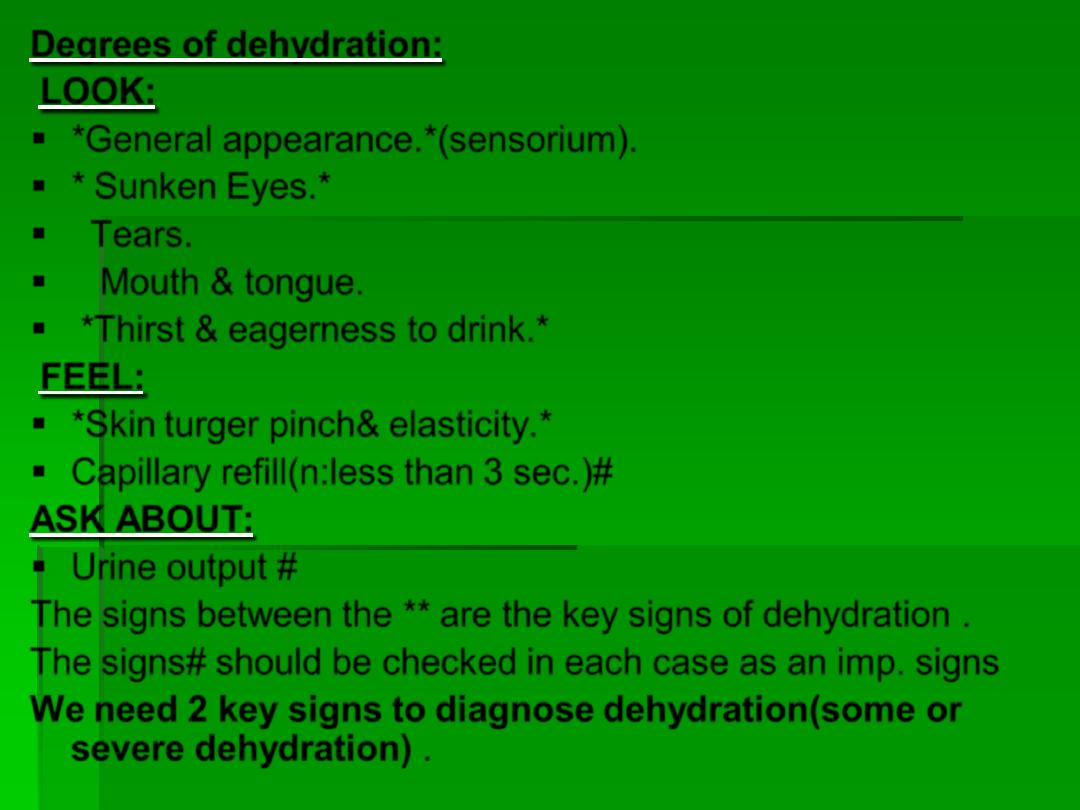
Degrees of dehydration:
LOOK:
*
General appearance.
*
(sensorium).
*
Sunken Eyes.
*
Tears.
Mouth & tongue.
*
Thirst & eagerness to drink.
*
FEEL:
*
Skin turger pinch& elasticity.
*
Capillary refill(n:less than 3 sec.)#
ASK ABOUT:
Urine output #
The signs between the
**
are the key signs of dehydration .
The signs# should be checked in each case as an imp. signs
We need 2 key signs to diagnose dehydration(some or
severe dehydration)
.
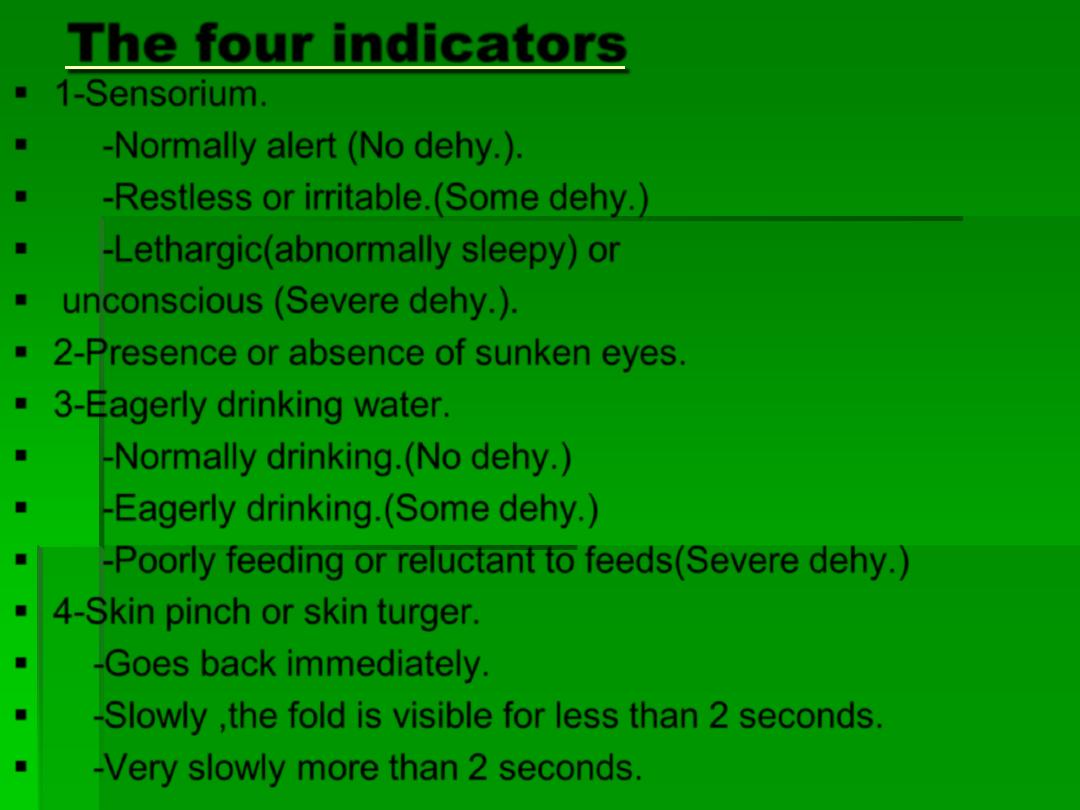
The four indicators
1-Sensorium.
-Normally alert (No dehy.).
-Restless or irritable.(Some dehy.)
-Lethargic(abnormally sleepy) or
unconscious (Severe dehy.).
2-Presence or absence of sunken eyes.
3-Eagerly drinking water.
-Normally drinking.(No dehy.)
-Eagerly drinking.(Some dehy.)
-Poorly feeding or reluctant to feeds(Severe dehy.)
4-Skin pinch or skin turger.
-Goes back immediately.
-Slowly ,the fold is visible for less than 2 seconds.
-Very slowly more than 2 seconds.
Plan A:
1-The child here is not dehydrated, so ORS here is given to
prevent dehydration.
2- Treatment usually at home with no rehydration phase.
3- The maintenance phase is to continue on feeding the baby.
If he is breast fed to continue on feeding him with small
frequent sips & if he is bottle fed to give fewer ounces but
frequent & if he is on diet to give him soft easily digestible
diet in small amount and frequent times.
4- For the on going loss, (and the age is below 24 months) we
give 50-100cc of ORS for each loose bowel motion passed
and if the age 2-10 years , (100-200cc)& if he vomits we wait
for 10 minutes and then continue giving the ORS by spoon
but more slowly .
5- Tell the mother to bring the child to the primary health
center if he is still having diarrhea after 2 days.
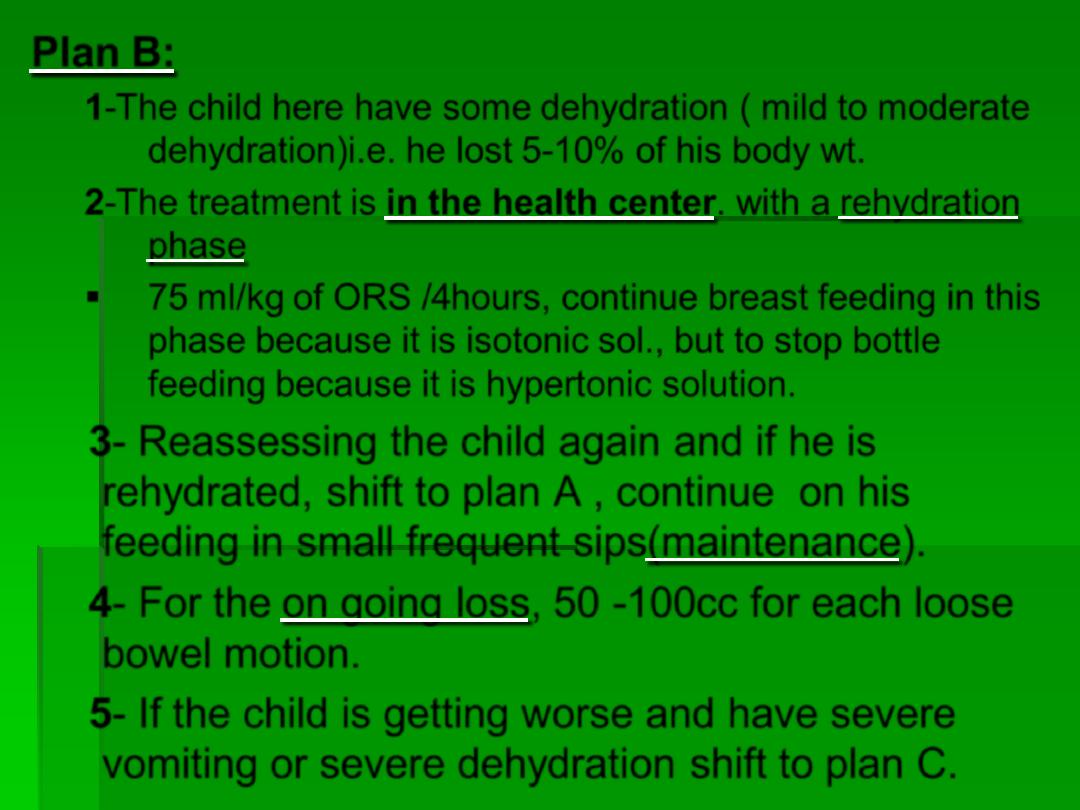
Plan B:
1-The child here have some dehydration ( mild to moderate
dehydration)i.e. he lost 5-10% of his body wt.
2-The treatment is in the health center. with a rehydration
phase
75 ml/kg of ORS /4hours, continue breast feeding in this
phase because it is isotonic sol., but to stop bottle
feeding because it is hypertonic solution.
3- Reassessing the child again and if he is
rehydrated, shift to plan A , continue on his
feeding in small frequent sips(maintenance).
4- For the on going loss, 50 -100cc for each loose
bowel motion.
5- If the child is getting worse and have severe
vomiting or severe dehydration shift to plan C.
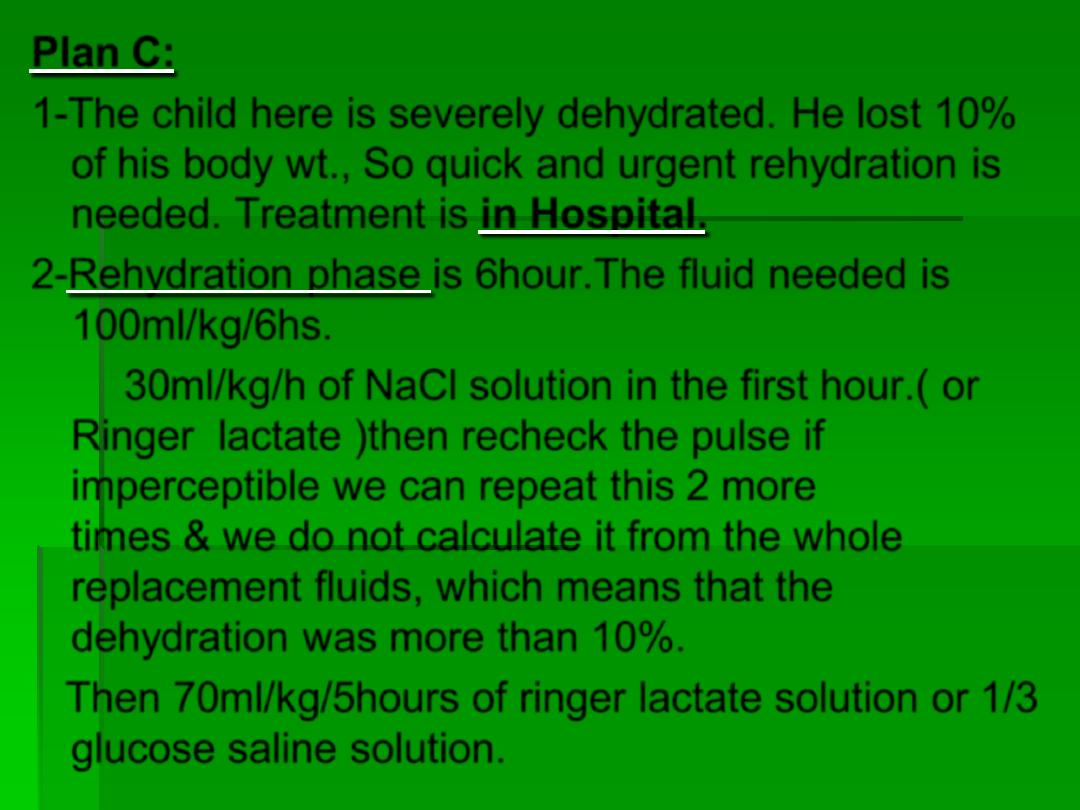
Plan C:
1-The child here is severely dehydrated. He lost 10%
of his body wt., So quick and urgent rehydration is
needed. Treatment is in Hospital.
2-Rehydration phase is 6hour.The fluid needed is
100ml/kg/6hs.
30ml/kg/h of NaCl solution in the first hour.( or
Ringer lactate )then recheck the pulse if
imperceptible we can repeat this 2 more
times & we do not calculate it from the whole
replacement fluids, which means that the
dehydration was more than 10%.
Then 70ml/kg/5hours of ringer lactate solution or 1/3
glucose saline solution.
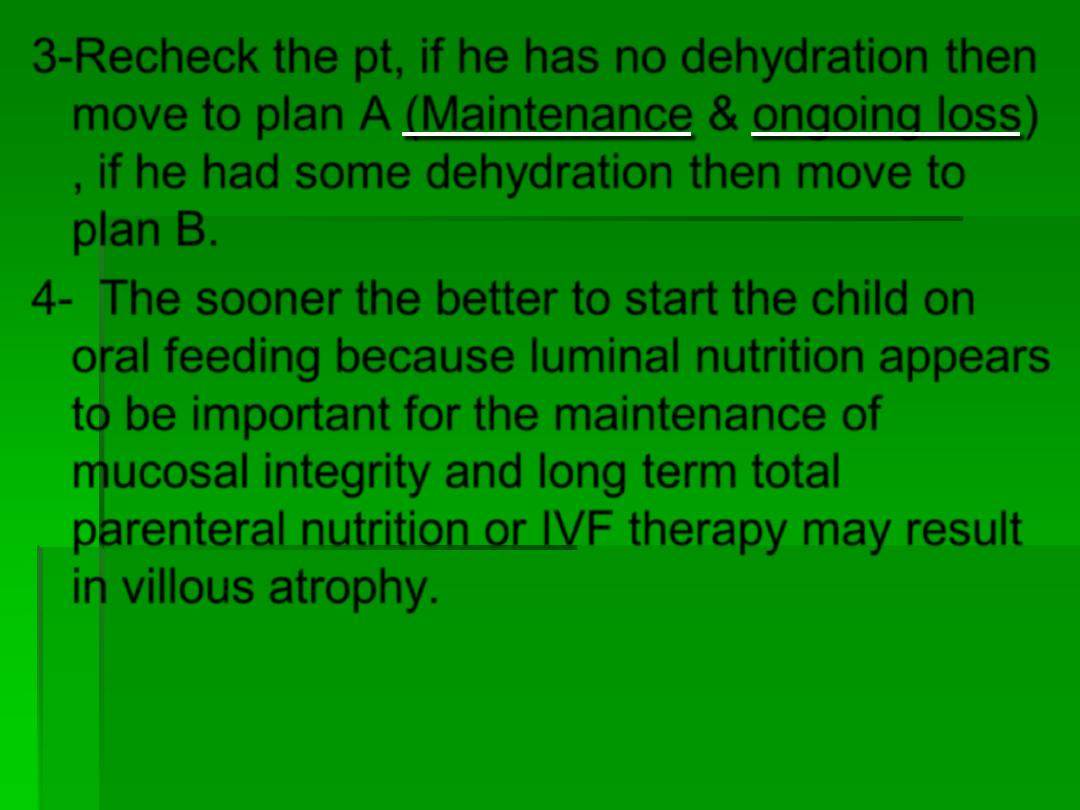
3-Recheck the pt, if he has no dehydration then
move to plan A (Maintenance & ongoing loss)
, if he had some dehydration then move to
plan B.
4- The sooner the better to start the child on
oral feeding because luminal nutrition appears
to be important for the maintenance of
mucosal integrity and long term total
parenteral nutrition or IVF therapy may result
in villous atrophy.
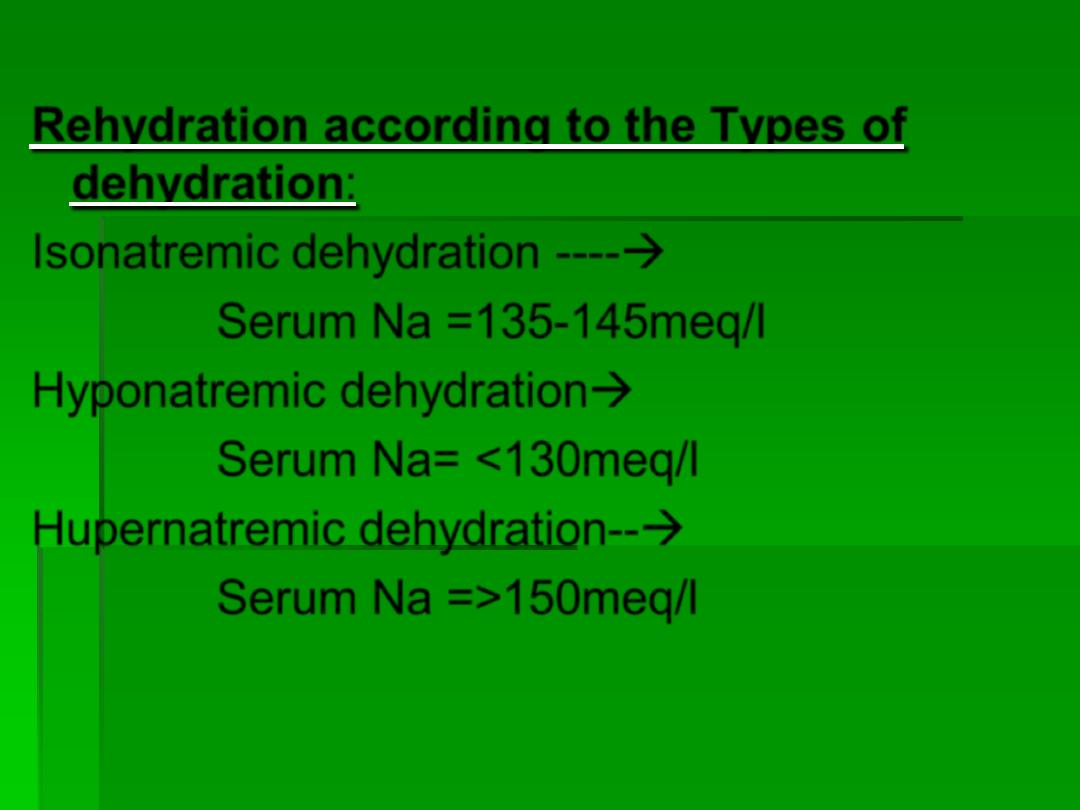
Rehydration according to the Types of
dehydration:
Isonatremic dehydration ----
Serum Na =135-145meq/l
Hyponatremic dehydration
Serum Na= <130meq/l
Hupernatremic dehydration--
Serum Na =>150meq/l
Signs & Symptoms:
Iso & hyponatremic dehydration has the same
S&S :
Lethargy, apathy, disorientation, anorexia, sometimes
agitation or even convulsion when the serum Na
level reaches 120meq/l or below.
Management:
Treatment according to the following equation:
(Normal Na-
Patient’s Na)x0.6xbody wt.= meq. Of Na
needed to raise the level of Na to normal.
The replacement therapy is given over 24-36 hours.

Hypernetremic dehydration:
S&S: The child here is not severely
dehydrated because the dehydration here is
rather intracellular dehydration . There is loss
of water more than Na from the ECF
compartment or excess Na is provided
increasing the osmolality of this fluid &
causing water to move out of the cells ,a
movement that add to the ECF volume so that
the depletion is less obvious.
The child here is irritable, tense fontanels,
crying all the time.Doughy feeling of the skin,
very thirsty, sometimes he presents with
convulsions.
Management of hypernatremic dehydration:
We calculate the same as before for rehydration
phase and then we spread that over 36-48 hours ,
even for the ORS(Slow rehydration) so that the
decrease in serum Na level daily should be 10
– 15
meq/l only.
*Slow rehydration is a must so that to avoid rapid
entry of the fluid to the brain cell causing brain
cell edema, the cell might burst causing
convulsion ,hemorrhage or thrombosis leading to
brain damage .
* Hyponatremic fluid should not be used to avoid
brain edema.
*1/3 glucose saline is the best for slow
rehydration
Hypokalemia:
Signs & symptoms:
The child usually has hypotonia, ms.weakness,
abdominal distention, and sometimes paralytic
ileus& in severe cases cardiac arrhythmias.
Death is possible in severe K depletion.
Management:
* K is added to the IVF only after urination
i.e.after the initial rehydration and the
improvement of the kidney perfusion. We do
not replace K early because of the shift of the
ICF( which Is rich in K) to compensate for the
loss in the ECF in dehydration so the amount
of K will be apparently high, but when we
rehydrate there will be a shift of the K inside
the cell and the level of K will be low.
The dose orally is: 2.5-3.5meq/kg /day.
For IV dose Maximum is 40 meq/l/day(each
ml of KCl=2meqK) .
Metabolic Acidosis:
Signs & symptoms:
In severely dehydrated children, metabolic acidosis
may appear as a result of loss of HCO3 in stool. The
child will have dehydration & deep sighing
respiration (kausmual breathing).
Management:
To treat Acidosis first we have to treat dehydration and
improve the kidney perfusion so that the kidney will
take over and reabsorb the bicarbonate. If the
acidosis remains after rehydration then we have to
investigate the kidney of that child.
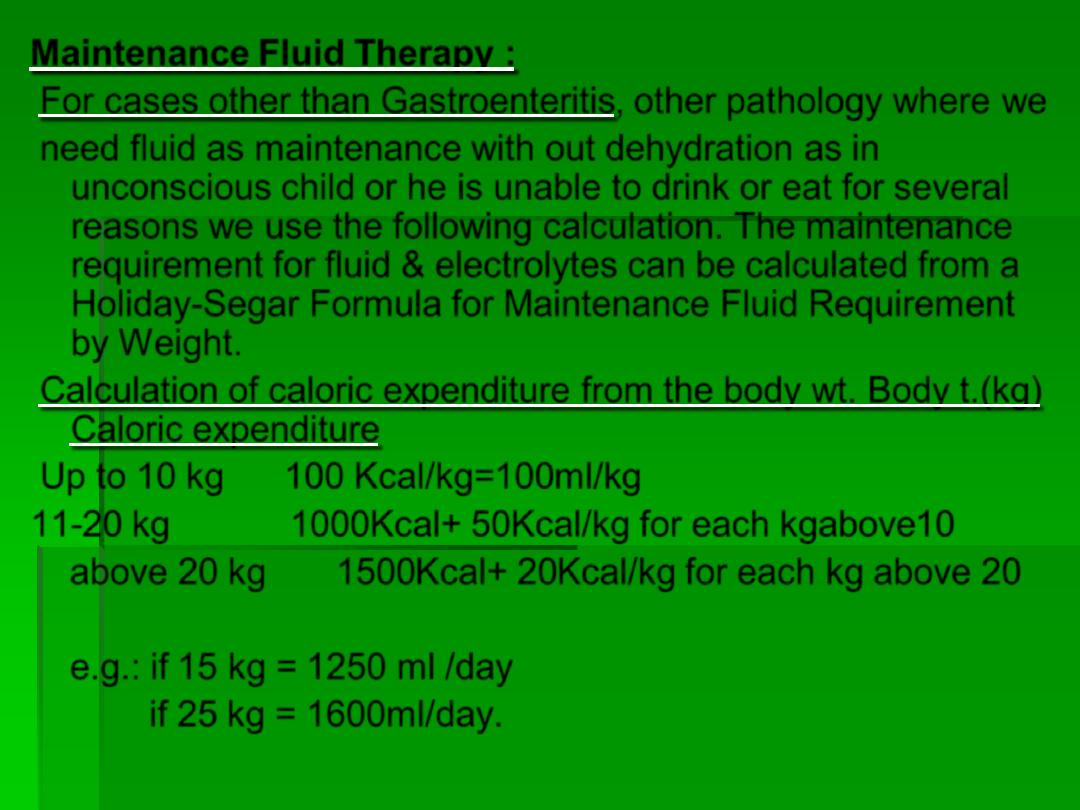
Maintenance Fluid Therapy :
For cases other than Gastroenteritis, other pathology where we
need fluid as maintenance with out dehydration as in
unconscious child or he is unable to drink or eat for several
reasons we use the following calculation. The maintenance
requirement for fluid & electrolytes can be calculated from a
Holiday-Segar Formula for Maintenance Fluid Requirement
by Weight.
Calculation of caloric expenditure from the body wt. Body t.(kg)
Caloric expenditure
Up to 10 kg 100 Kcal/kg=100ml/kg
11-20 kg 1000Kcal+ 50Kcal/kg for each kgabove10
above 20 kg 1500Kcal+ 20Kcal/kg for each kg above 20
e.g.: if 15 kg = 1250 ml /day
if 25 kg = 1600ml/day.
Modification of maintenance therapy as a result
of diseases:
1-Decreased in cases of Anuria or extreme
oliguria,inappropriate ADH secretion such as
in Meningitis, or in congestive heart failure.
2-Increased in cases of Heat stress, Adrenal
insufficiency,Diabetes Mellitus , Diabetes
Insipidus & Burns.