4th stage
MedicineLec-9
Dr.Jasim
1/12/2015
Heart FailureClinical syndrome that develops when the heart cannot maintain adequate output, or
can do so only at the expense of elevated ventricular filling pressure.
Results from any structural or functional abnormality that impairs the ability of the ventricle to eject blood (Systolic Heart Failure) or to fill with blood (Diastolic Heart Failure).
The prevalence of heart failure rises with age.
Almost all forms of heart disease can lead to heart failure.Mechanisms of heart failure :
Reduced ventricular contractility
CAD (segmental dysfunction) ‘cardiomyopathy(global dysfunction)
Ventricular outflow obstruction
Hypertension, aortic stenosis (left heart failure)Pulmonary hypertension, pulmonary stenosis (right heart failure).
Ventricular inflow obstruction
Mitral stenosis,tricuspid stenosis.Ventricular volume overload
Ventricular septal defect.Arrhythmia
Atrial fibrillation ,Tachycardia cardiomyopathy Complete heart block Bradycardia.Diastolic dysfunction
Constrictive pericarditis, Restrictive cardiomyopathy, Cardiac tamponade.Pathophysiology :
Cardiac output is determined by preload (the volume and pressure of blood in the ventricles at the end of diastole) afterload (the volume and pressure of blood in the ventricles during systole) and myocardial contractility.
Fall in cardiac output. activates counterregulatory neurohumoral mechanisms , renin–angiotensin–aldosterone system leads to vasoconstriction, sodium and water retention, and sympathetic nervous system activation.
Activation of the sympathetic nervous system may initially sustain cardiac output through increased myocardial contractility (inotropy)and heart rate (chronotropy).
Prolonged sympathetic stimulation also causes negative effects, including cardiac myocyte apoptosis,hypertrophy and focal myocardial necrosis.
Sympathetic stimulation also causes peripheral vasoconstriction and arrhythmias.
The Vicious Cycle of Congestive Heart Failure :
Types of Heart Failure :Left, right and biventricular heart failure.
Diastolic and systolic dysfunction.
High-output failure.
Acute and chronic heart failure.
Causes of Low-Output Heart Failure (chronic)
Systolic DysfunctionCoronary Artery Disease
Idiopathic dilated cardiomyopathy (DCM)
Hypertension
Valvular Heart Disease
Diastolic Dysfunction
Hypertension
Coronary artery disease
Hypertrophic obstructive cardiomyopathy (HCM)
Restrictive cardiomyopathy
Acute Decompensaated Heart Failure
Causes:Acute MI
Rupture of chordae tendinae/acute mitral valve insufficiency
Volume Overload
Transfusions, IV fluids
Worsening valvular defect
Pulm.embolism
Myocarditis
Factors that may precipitate or aggravate heart failure in pre-existing heart disease :
Myocardial ischaemia or infarctionIntercurrent illness, e.g. infection
Arrhythmia, e.g. atrial fibrillation
Inappropriate reduction of therapy
Administration of a drug with negative inotropic (β-blocker)or fluid-retaining properties (NSAIDs, corticosteroids)Pulmonary embolism
Conditions associated with increased metabolic demand, e.g. pregnancy, thyrotoxicosis, anaemiaIV fluid overload, e.g. post-operative IV infusion
Clinical Presentation of HeartFailure (Acute)Sudden onset of dyspnoea that rapidly progresses to acute respiratory distress, orthopnoea and cough.
The patient appears agitated, pale and clammy. The peripheries are cool to the touch and the pulse is rapid.The BP is usually high, The jugular venous pressure (JVP) is usually elevated.
Auscultation A ‘gallop’rhythm, with a third heart sound,is heard. A new systolic murmur may signify acute mitral regurgitation or ventricular septal rupture. crepitations at the lung bases, or throughout the lungs if pulmonary oedema is severe.
Clinical Presentation of Heart Failure(Chronic)
Due to excess fluid accumulation:Dyspnea (most sensitive symptom
Orthopnea, Paroxysmal Nocturnal Dyspnea (PND)
Edema
Hepatic congestion
Ascites
Due to reduction in cardiac ouput:
Fatigue (especially with exertion)
Weakness
Poor renal perfusion leads to oliguria and uraemia
Chronic heart failure is sometimes associated with marked weight loss (cardiac cachexia).
Physical Examination in Heart Failure
DyspniacCool, pale, cyanotic extremities
Have sinus tachycardia, diaphoresis and peripheral vasoconstriction
Displaced Apex
S3 gallop Low sensitivity, but highly specific
Crackles or decreased breath sounds at bases (effusions) on lung exam
Elevated jugular venous pressure
Lower extremity edema
Ascites
Hepatomegaly
Splenomegaly
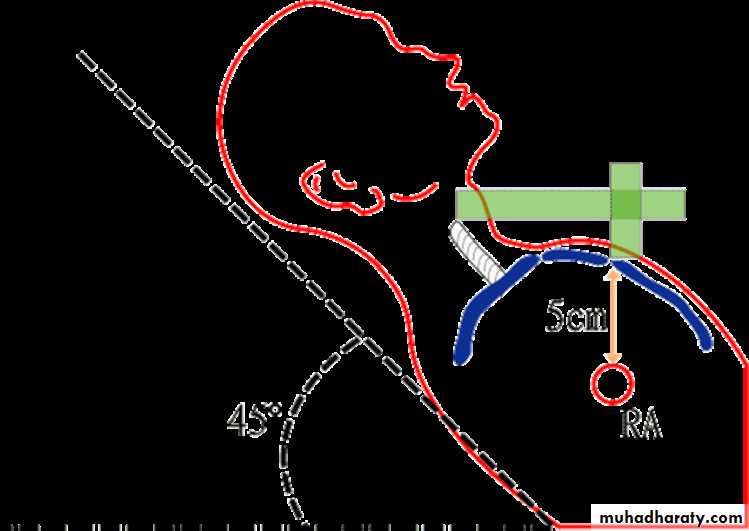
Measuring Jugular Venous Pressure
Complications :
Renal failureHypokalaemia
Hyperkalaemia
Hyponatraemia
Impaired liver function
Thromboembolism
Atrial and ventricular arrhythmias
Impaired liver function
Lab Analysis in Heart Failure:
CBC : Since anemia can exacerbate heart failure
Serum electrolytes and creatinine : before starting high dose diuretics
Fasting Blood glucose : to evaluate for possible diabetes mellitusThyroid function tests : Since thyrotoxicosis can result in A. Fib, and hypothyroidism can results in HF.
Iron studies : to screen for hereditary hemochromatosis as cause of heart failure.
ANA : to evaluate for possible lupusViral studies : If viral mycocarditis suspected
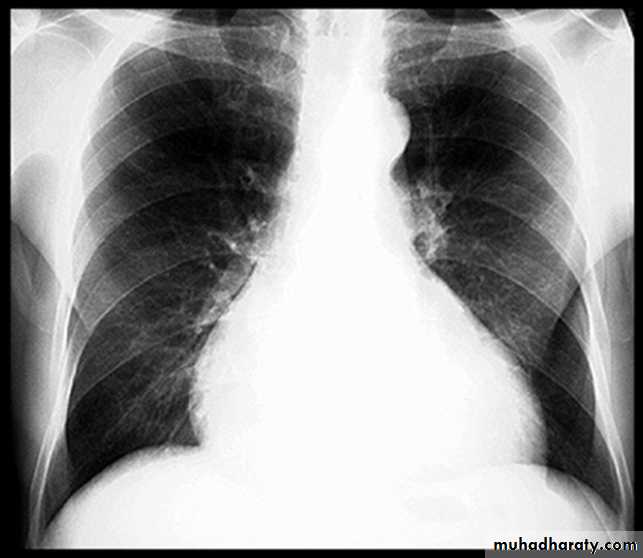
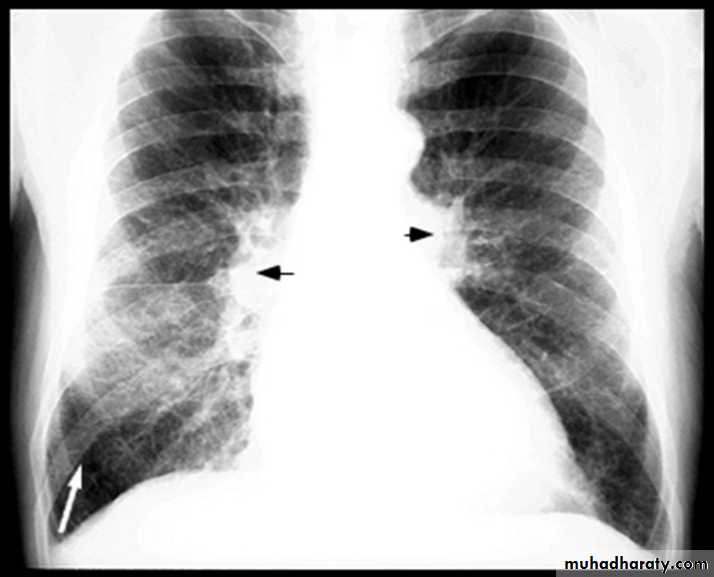
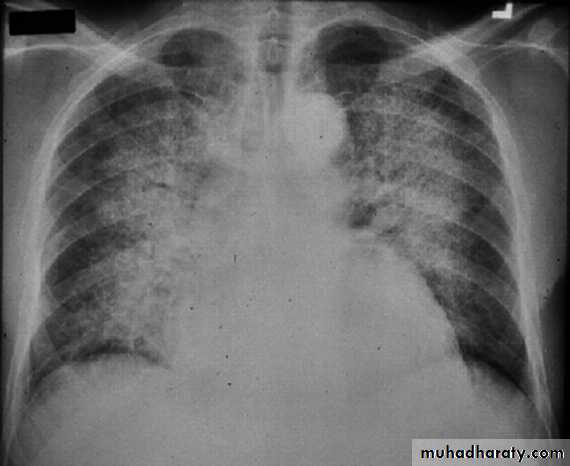
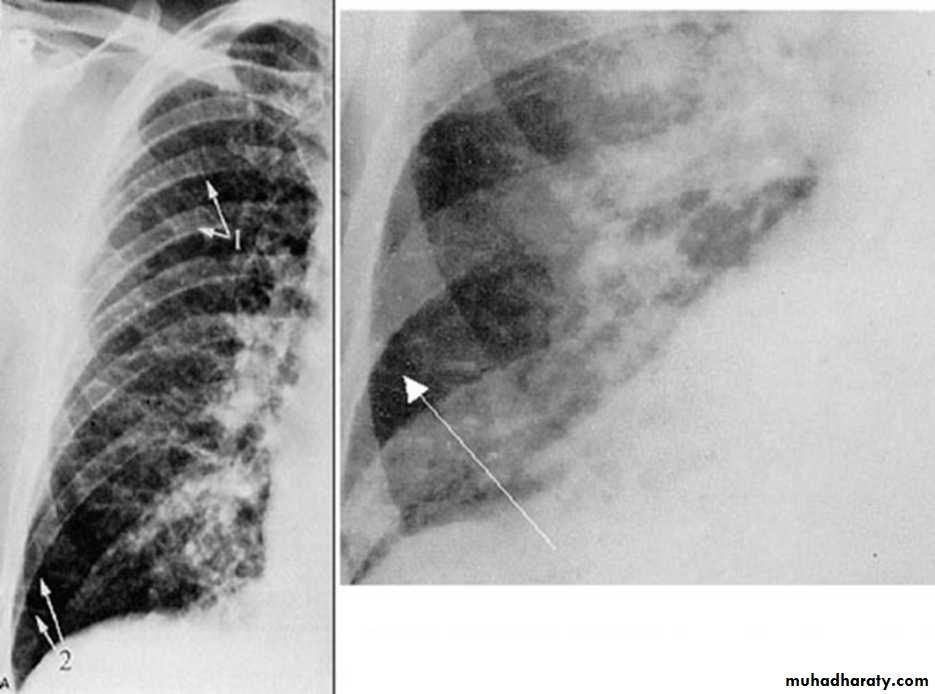
BNP brain natriuretic pepetideChest X-ray in Heart Failure
CardiomegalyCephalization of the pulmonary vessels
Kerley B-lines
Pleural effusions
Cardiomegaly Pulmonary vessel congestion
Pulmonary Edema due to Heart Failure
Kerley B lines
Further Cardiac Testing in Heart Failure
Exercise Testing :Should be part of initial evaluation of all patients with CHF.
Coronary arteriography :
Should be performed in patients presenting with heart failure who have angina or significant ischemia.
Endomyocardial biopsy :
Not frequently used , Really only useful in cases such as viral-induced cardiomyopathyElectrocardiogram:
May show specific cause of heart failure:Ischemic heart disease
Dilated cardiomyopathy: first degree AV block, LBBB, Left anterior fascicular block.
Echocardiogram:
Left ventricular ejection fractionStructural/valvular abnormalities
Management of acute HF ( imp :D )
acute medical emergency:Sit the patient up to reduce pulmonary Congestion.
Give oxygen (high-flow, high-concentration).
IV frusemide 50-100 mg
Administer nitrates, such as IV glyceryl trinitrate until clinical improvement occurs or systolic BP falls.
Continuous monitoring of cardiac rhythm, BP .
Intravenous opiates must be used sparingly in distressed patients.
If these measures prove ineffective, inotropic agents may be required to augment cardiac output , particularly in hypotensive patients ( Dopamine).
Management of chronic heart failure
General measures
Drug therapyDevice therapy
Cardiac transplant
General measures :
EducationDiet
Good general nutrition and weight reduction for the obese
Avoidance of high-salt foods and added salt.
Alcohol
Smoking
Exercise
Regular moderate aerobic exercise within limits of symptoms
Vaccination
Consider influenza and pneumococcal vaccination
Treatment of the underlying cause of heart failure (CAD)
Drug therapy
Loop diureticsACE inhibitor (or ARB if not tolerated)
Beta blockers
Digoxin
Hydralazine, Nitrate
Potassium sparing diuretcs
Ivabradine
Diuretics
Loop diuretics
Furosemide, buteminide
diuretics produce an increase in urinary sodium and water excretion, leading to reduction in blood and plasma volume
Potassium-sparing diuretics
Spironolactone, eplerenone
Help enhance diuresis
Maintain potassium
Shown to improve survival in CHF
ACE Inhibitor
Improve survival in patients with all severities of heart failure.Begin therapy low and titrate up as possible:
Enalapril – 2.5 mg po BID
Captopril – 6.25 mg po TID
Lisinopril – 5 mg po QDaily
If cannot tolerate, may try ARB
Beta Blocker therapy
Certain Beta blockers (carvedilol, metoprolol, bisoprolol) can increase ejection fraction, improve symptoms , reduce the frequency of hospitalisation and reduce mortality.
Contraindicated:
Heart rate <60 bpm
Symptomatic bradycardia
Signs of peripheral hypoperfusion
COPD, asthma
PR interval > 0.24 sec, 2nd or 3rd degree block
Hydralazine plus Nitrates
Dosing:
Hydralazine : Started at 25 mg po TID, titrated up to 100 mg po TID
Isosorbide dinitrate : Started at 40 mg po TID/QID
Decreased mortality, lower rates of hospitalization, and improvement in quality of life.
IvabradineIt reduces hospital admission and mortality rates in patients with heart failure due to moderate or severe left ventricular systolic impairment.
Other medication in Heart Failure :
Digoxin can be used to provide rate control in :patients with heart failure and atrial fibrillation.
patients with severe heart failure, digoxin reduces the likelihood of hospitalisation for heart failure
Statin therapy is recommended in CHF for the secondary prevention of cardiovascular disease.
Some studies have shown a possible benefit specifically in HF with statin therapy.
Meds to AVOID in heart failure :
NSAIDSCan cause worsening of preexisting HF
Thiazolidinediones
Include rosiglitazone (Avandia), and pioglitazone (Actos)
Cause fluid retention that can exacerbate HF
Metformin
People with HF who take it are at increased risk of potentially lethic lactic acidosis.
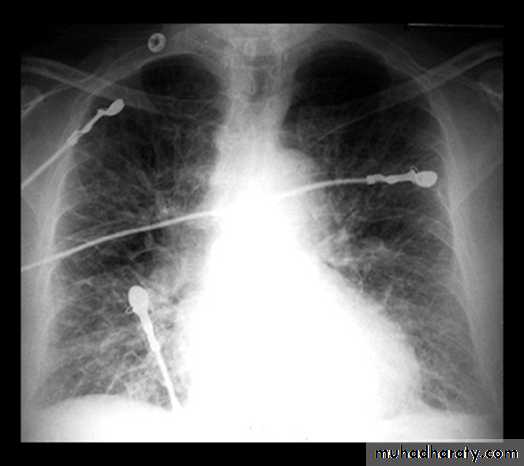
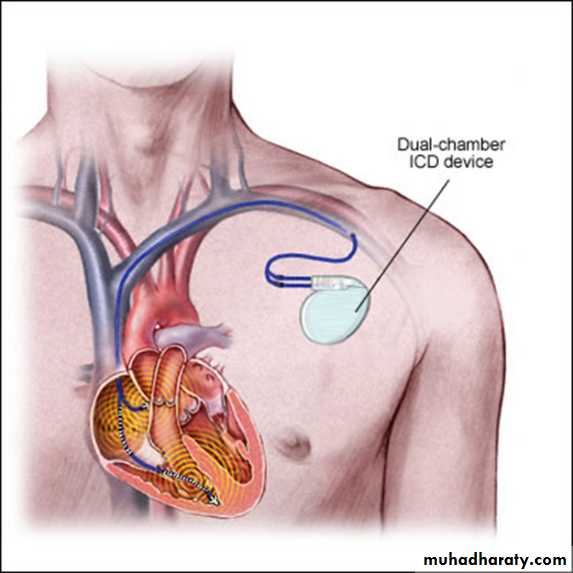
Implantable Cardioverter-Defibrillators for HF( ICD) –CRT
Sustained ventricular tachycardia is associated with sudden cardiac death in HF.
About one-third of mortality in HF is due to sudden cardiac death.Patients with ischemic or nonischemic cardiomyopathy, NYHA class II to III HF, and LVEF ≤ 35% have a significant survival benefit from an implantable cardioverter-defibrillator (ICD) for the primary prevention of SCD.
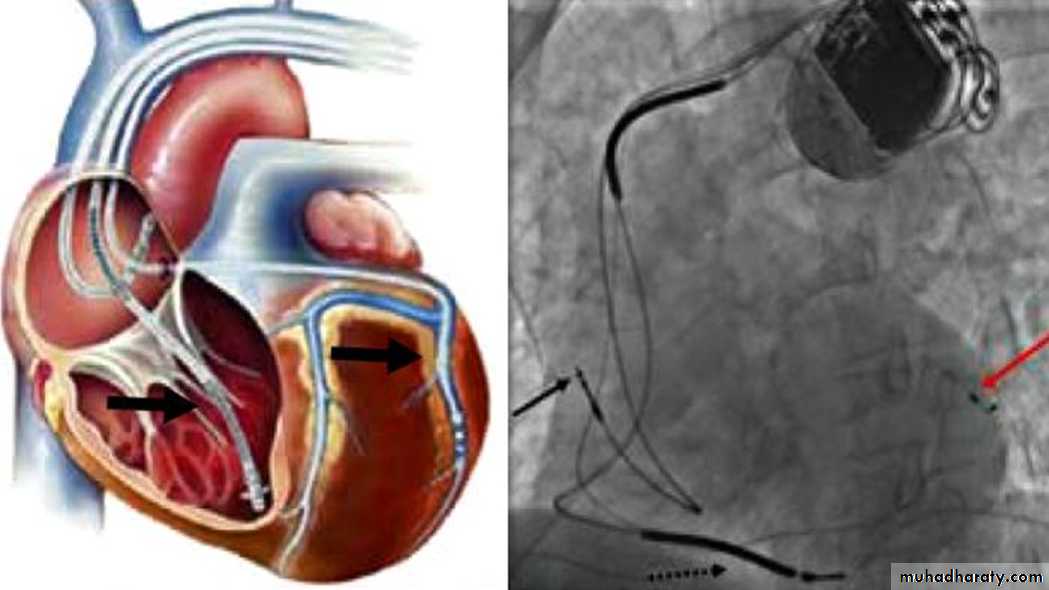
Cardiac-Resynchronization-Therapy
Management of Refractory Heart Failure
Inotropic drugs:Dobutamine, dopamine, milrinone, nitroprusside, nitroglycerin.
Mechanical circulatory support:
Intraaortic balloon pumpLeft ventricular assist device (LVAD).
Cardiac Transplantation