Acyanotic Congenital Heart DiseaseObstructive Lesions:
Pulmonary StenosisAortic Stenosis
Coarctation of the Aorta
PULMONARY STENOSIS
PS accounts for approximately 10% of all congenital heart disease and can be:
Valvular.
Subvalvular.
Supravalvular.
Clinical Manifestations:
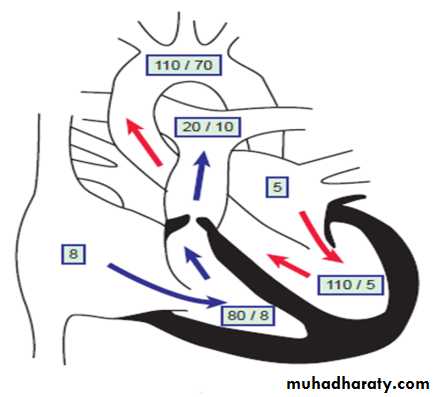
Symptoms depend on the degree of obstruction present:Mild PS: right ventricle to pulmonary artery pressure gradient of ≤30 mm Hg.
Moderate PS: right ventricle to pulmonary artery pressure gradient 30-60 mm Hg.
Severe PS: right ventricle to pulmonary artery pressure gradient >60 mm Hg.
-Mild PS: are asymptomatic.
Moderate to severe PS: results in exertional dyspnea and easy fatigability. If hepatic enlargement and peripheral edema are present, they are an indication of right ventricular failure.
Newborns with severe stenosis may be more symptomatic and even cyanotic because of right-to-left shunting at the atrial level (patent foramen ovale), a condition termed critical pulmonic stenosis.
PS causes a systolic ejection murmur at the second left intercostal space which radiates to the back.
A thrill may be present.
S2 may be widely split.
With more severe pulmonary stenosis, an impulse at the lower left sternal border results from RVH.
Investigations:
Mild PS: normal.
Moderate to severe PS:
ECG: RAD & RVH.
CXR:
the heart size is usually normal (but may shows cardiac enlargement with prominence of the right ventricle and right atrium).
the main PA segment may be prominent because of poststenotic dilation of the main pulmonary artery.
Echo: show the anatomy & pressure gradient
PS: normal heart size but post stenotic dilation of PA
Treatment
Mild PS: usually does not progress.Moderate to severe PS:
Balloon valvuloplasty.
Surgical repair is required if balloon valvuloplasty is unsuccessful.
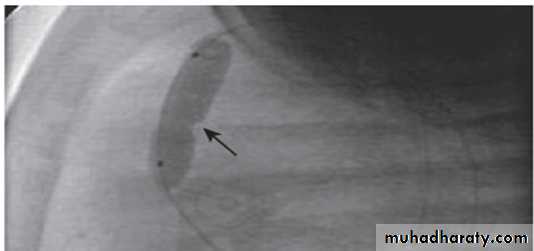
Valvar PS and balloon valvuloplasty
Inflation of the balloon catheter showing the indentation (arrow) made on the balloon from the stenotic valve.
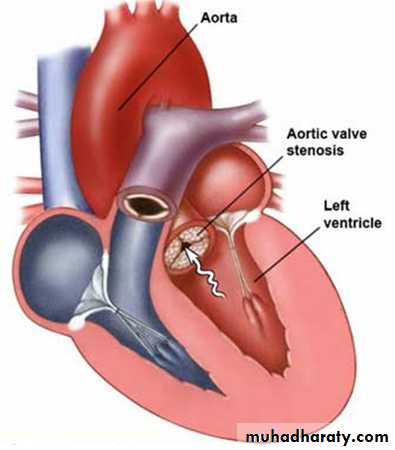
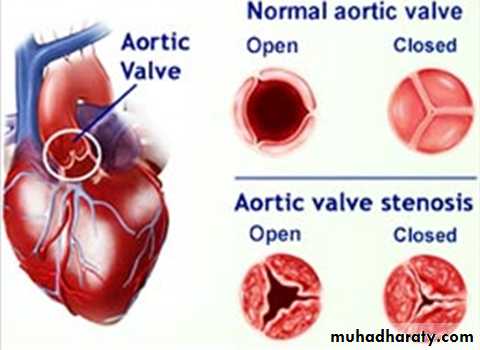
AORTIC STENOSIS
AS represents approximately 5% of all congenital heart disease. It is 3 types:Valvular.
Subvalvular.
Supravalvular.
CLINCAL MANIFESTATIONS
Symptoms depend on the degree of stenosis:
Mild to moderate AS: cause no symptoms.Severe AS: results in easy fatigability, exertional chest pain, and syncope. Sudden death if surgical relief delayed.
Infants with critical AS: may present with symptoms of LHF.
Signs:
Systolic ejection murmur is heard at the right second intercostal space along the sternum and radiating into the neck.
Thrill may be present at the right upper sternal border or in the suprasternal notch.
Investigation:
Mild AS: normal.
Moderate to severe AS:
ECG: LVH.
CXR: poststenotic dilation of the ascending aorta or aortic knob.
Echo: shows the anatomy & pressure gradient.
Treatment:
The degree of aortic stenosis frequently progresses with growth and age.
Balloon valvuloplasty is indicated for children with moderate to severe valvular AS to prevent progressive left ventricular dysfunction & the risk of syncope and sudden death.
Surgical management is necessary when balloon valvuloplasty is unsuccessful.
COARCTATION OF THE AORTA
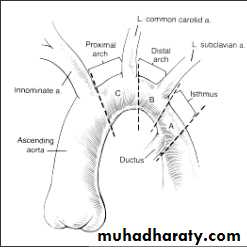
Constrictions of the aorta of varying degrees may occur at any point from the transverse arch to the iliac bifurcation, but 98% occur just below the origin of the left subclavian artery at the origin of the ductus arteriosus (juxtaductal coarctation).
CoA accounts for 10 % of all CHD.
Male: Female ratio 2:1
More common in Turner syndrome.
Pathophysiology:
Developmental factor
1. Underdevelopment or hypoplasia of aortic arch or isthmus.
* Proximal arch
* Distal arch
* Isthmus
2. Presence of ectopic ductal tissue in the aorta.
Hypoplasia of aortic arch & isthmus
Types of coarctation:
Infantile type (preductal CoA).Adult type (juxtaductal CoA) previously known as postductal type.
Preductal CoA Postductal CoA
Pathophysiology (cont..)
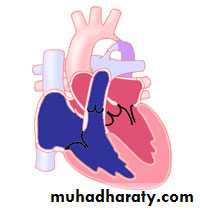
Preductal or infantile-type CoA:CoA associated with aortic arch hypoplasia. right ventricular blood is ejected through the ductus to supply the descending aorta. Perfusion of the lower part of the body is then dependent on right ventricular output.
In this situation, the femoral pulses are palpable, and differential blood pressures may not be helpful in making the diagnosis. The ductal right to- left shunting is manifested as differential cyanosis, with the upper extremities being pink and the lower extremities blue. Such infants may have severe pulmonary hypertension and high pulmonary vascular resistance. Signs of heart failure are prominent.
Coarctation associated with arch hypoplasia was once referred to as infantile type because its severity usually led to recognition of the condition in early infancy.
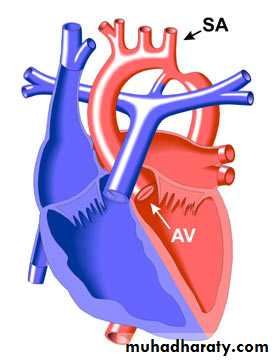
Discrete juxtaductal or adult- type CoA:
Ascending aortic blood flows through the narrowed segment to reach the descending aorta, although left ventricular hypertension and hypertrophy result.
In the 1st few days of life, the PDA may serve to widen the juxtaductal area of the aorta and provide temporary relief from the obstruction. Net left-to-right ductal shunting occurs in these acyanotic infants.
It is called adult type because it is was not usually recognized until later childhood. Blood pressure is elevated in the vessels that arise proximal to the CoA; blood pressure as well as pulse pressure is lower below the constriction.
Clinical Manifestations
Clincal manifestation depend on:
Type of CoA
Associated cardiac lesion as bicuspid aortic valve, subaortic stenosis, mitral valve abnormalities, VSD.
Associated syndroms as turner.
Presence of collateral.
Infant:
Closure of ductus (7-10 days) produces severe HF, poor feeding, respiratory distress, acidosis and shock. Classically the femoral pulses are weaker and delayed compared with the right radial pulse. The blood pressure in the lower extremities is lower than that in the upper extremities.
Ductus remains patent - differential cyanosis.
On examination, the heart is large, and a systolic murmur is heard along the left sternal border.
Older children:
Asymptomatic.
leg discomfort with exercise, headache, or epistaxis.
The classic sign of CoA is a disparity in pulsation and blood pressure in the arms and legs. The femoral, popliteal, posterior tibial, and dorsalis pedis pulses are weak (or absent in up to 40% of patients), in contrast to the bounding pulses of the arms and carotid vessels & hypertension in an upper extremity greater than the 95th percentile for age.
If collateral present, there will be radial-femoral delay.
Systolic murmur is often heard along the left sternal border at the 3rd and 4th intercostal spaces. The murmur is well transmitted to the left infrascapular area and occasionally to the neck.
If significant collaterals have developed, continuous murmurs may be heard throughout the chest.
An abnormal aortic valve is present approximately 50% of the time, causing a systolic ejection click and systolic ejection murmur of aortic stenosis.
Investigation:
Infant: The ECG and chest x-ray show evidence of RVH with marked cardiomegaly and pulmonary edema. Echocardiography shows the site of coarctation and associated lesions.
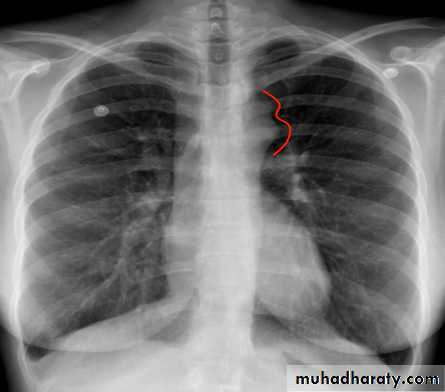
In older children: the ECG and chest x-ray usually show LVH and a mildly enlarged heart. Rib notching may also be seen in older children (>8 years of age) with large collaterals. Echocardiography shows the site and degree of coarctation, presence of LVH, and aortic valve morphology and function.
3 sign of aorta Rib notching
(Post stenotic dilation of aorta)
Treatment:
Management of an infant presenting with cardiac decompensation includes intravenous infusion of prostaglandin E1 (chemically opens the ductus arteriosus), inotropic agents, diuretics, and other supportive care.Balloon angioplasty has been done, especially in critically ill infants, but surgical repair of the coarctation is most commonly performed.
Ballooning and stenting of older patients with coarctation has also been performed, but surgical repair remains the most common form of management.
Prophylaxis against infective endocarditis
Acyanotic Congenital Heart Disease
Regurgitant Lesions
Regurgitant Lesions
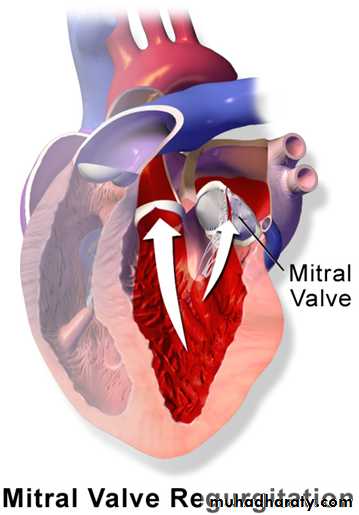
Congenital Mitral Insufficiency.
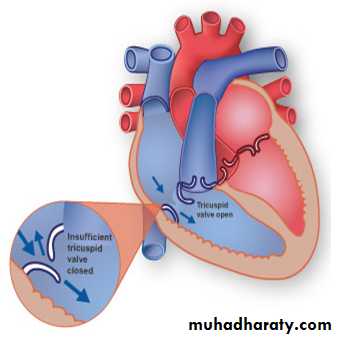
Mitral Valve Prolapse.Tricuspid Regurgitation