Bone tumors
More than 80% of bone tumors are either secondary or its multiple myaloma, and primary bone tumors accounts for less than 20% of all bone tumors.Secondary bone deposits can reach the bone from any body malignancy but most commonly from:
Ca-lung
Ca-thyroid
Ca-breast
Ca-prostate
Ca-kidney
Colo-rectal carcinoma
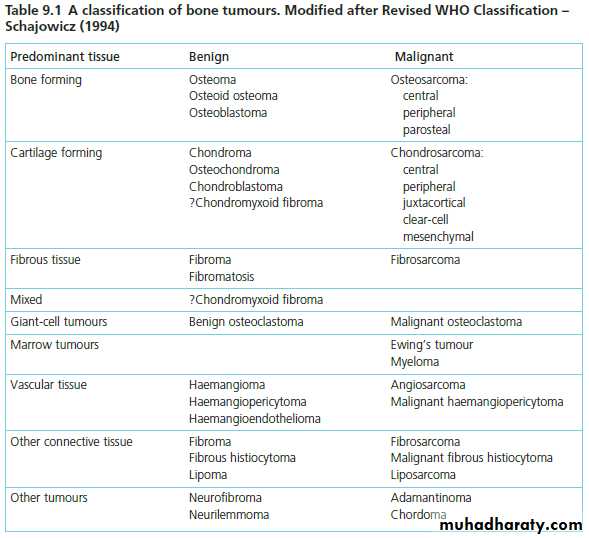
The primary bone tumors are those arising from bony tissues itself and can be classified according to the cell of origin as below:
Diagnosis of bone tumors:
The commenst presenting symptoms are:
Pain
Swelling
Local tenderness
Accidentally diagnosed
Pathological fracture
Signs that may suggest malignancy includes:
Rapid growthWarmth
Tenderness
Ill-defined edges
Important investigations:
Good x-rayCT-scan
MRI
Bone scan
Good biopsy
All must be done before planning for treatment or surgery.
Types of biopsy:
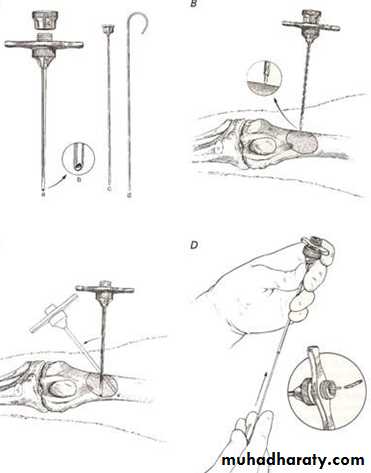
Fine needle aspirate cytology (FNAC): aiming to recover few cells of the suspected tissue and send it for CYTOLOGICAL exam looking for malignant cells.
Wide-bore needle (CORE) biopsy; the wide needle used to recover a tissue piece for HISTOPATHOLOGICAL exam.
Incisional biopsy: via small surgical approach we aim at cutting small pieces of the tumor to e send for histopathology
Excisional biopsy: for small accessible tumors where complete surgical excision is possible and the whole tumor mass send for histopathology
Types of surgical excision of a tumor:
The final decision about type of tumor excision depends on its histopathological appearance whether benign or malignant and if its localized or metastasized. For benign local tumors we use more conservative and limited surgery while for malignant tumors we are more aggressive and may need resection.Tumor excision can be:
Intralesional excision (curettage): for benign lesions we open the capsule and curate the lesion.
Marginal excision (local excision): also for benign lesions where the whole lesion with its capsule and few mm. Of the surrounding tissues is removed.
Wide local excision: for more aggressive tumors, its like marginal excision but here we remove few centimeters of the surrounding tissues EN-BLOCK with the tumor.
Radical resection: it’s used for malignant tumors that are only locally invasive but not metastatized.it means amputation of the limb through the proximal joint???
Malignant tumors also need adjuvant treatment with radiotherapy and/or chemotherapy before and/or after amputation or excision if they are sensitive.
Principles of treatment of bone tumors:
Benign asymptomatic lesions:
Treatment may never needed, if needed we can do curettage or local excision.
Benign symptomatic or enlarging lesions:
Confirm diagnosis by biopsy and do marginal excision.
Suspected malignant tumors:
Properly investigate the patient and exclude distant metastasis
Do proper biopsy
Choose the suitable excision (wide local excision or radical resection) according to tumor type and local extension.
Use adjuvant therapy if its sensitive.
Follow the patient regularly to exclude recurrence or metastasis.
Benign bone tumors
Osteoid osteoma:Benign tumors consist of primitive osteoid tissue with neurovascular tuft (the nidus), its surrounded by a very thick sclerotic bone reaction.
Round or oval in shape, less than 1cm. In size.
Common in metaphysis or diaphysis, usually affects femur or tibia.
Patient age usually below 30.
Pain is the main symptom, mainly at night and can be very severe usually relieved by aspirin.
X-ray shows a small radiolucency (nidus=tumor) surrounded by thick sclerotic bone (bone reaction).
Treatment by local excision of the nidus and surrounding bone.
Osteochondroma (cartilage capped exostosis):
Commonest benign tumor of bone.
Occurs during bone growth in adolescence.
Starts as cartilaginous overgrowth at the edge of the epiphysis and grow outside the bone on the same direction (towards diaphysis), its base later on ossify and show on x-ray as an exostosis (either narrow base-pedanculated or wide base-sessile). Its growth continues with the bone and stops as the bone stops growing, any enlargement after that (especially if associated with pain) considered serious and regarded as malignant transformation until proved otherwise.
It can be single or multiple (multiple familial osteochondrom, congenital achlasis).
Pain or lump is the usual presentation, there is pain due to an overlying bursa or impingement on soft tissues, or it may affect nearby joint or tendon function, sometimes it press on nearby important structures as vessel or nerve. Paraesthesia may due to stretching of an adjacent nerve.
Sometimes accidentally discovered by x-ray
Incidence of malignant transformation is about 1% in single and 6% in multiple osteeochondroma.
X-ray shows well-defined exostosis at the bone ends mainly around the knee.
Any increase in size or pain after puberty must be concederd malignant transformation until proved otherwise. It can change to chodrosarcoma or osteosarcoma.
Treatment is by local excision of the exostosis.
Chondroma:
Benign cartilage tumor.
Single or multiple (Olliers disease).
Occurs most usually in small bones of hands or feet also may occur in long bones.
It may grow inside the bone and called enchondroma or on its outer surface..
Patient may present with pain, swelling or pathological fracture.
X-ray shows well-defined lucent area of bone sometimes expanded and contains specks of calcification which is pathognomonic.
Differential diagnosis includes bone cyst and chondrosarcoma.
It usually affects patients above 30.
Sometimes its multiple (Ollier's disease) and this may be associated with haemangiomas (Maffucci’s syndrome).
Malignanant transformation less than 2 %, up to 30% in Ollier's disease and almost 100% in Maffucci’s syndrome
Treated by excision or curettage +/- bone graft.
Non-ossifying fibroma (fibrous cortical defect):
Lucent fibrous tissue lesion (benign) inside bone cortex.Mostly accidentally discovered by x-ray.
Seen in children and may disappear spontaneously with time during growth.
X-ray shows eccentrically located lucent small defect in the bone cortex, well defined surrounded by sclerosis.
Seen mostly in the cortex of the metaphysis of long bones.
Rarely if large may cause pathological fracture.
Usually does not need treatment unless there is pathological fracture.
Fibrous dysplasia:
Developmental disorder whereby normal bone is replaced by fibrous tissue with flecks of osteoid.
It may affect one bone (monostotic) or multiple bones (polystotic).
The lesion may be very large causes bone expansion and cortical thinning with progressive deformity and sometimes pathological fracture.
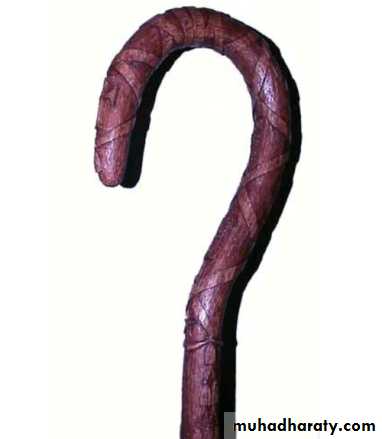
Lesions occur in metaphysis&diaphysis, proximal femur is a common site it gives characteristic deformity called (shepherd’s-crock deformity(عصا الراعي.
X-ray shows lucent cystic lesion sometimes large and multilocular with bone expansion and cortical thinning it contains multiple calcific spots giving the ground-glass appearance, there is always possible deformity or pathological fracture.
About 5-10% of polyostotic forms get malignant, while only rarely occurs in monostotic lesions.
Treatment depends on tumor size and possible deformity;
Small lesions may need no treatment, just follow up.
For larger lesions we do curettage and bone graft or cement.
Sometimes we need internal fixation especially with fractures and larger lesions.
Deformities may need corrective osteotomy.
Always there is tendency for recurrence.
Osteoblastoma (giant osteoid osteoma):
It’s benign and similar to osteoid osteoma but its larger and more cellular.It occurs in young adults, males more than females.
Its commoner in the spine and flat bones& usually presents as pain or muscle spasm.
X-ray shows well-defined lytic lesion surrounded by thin zone of sclerosis, it may contain flecks of calcification.
Treatment consists of excision and bone grafting. With lesions in the vertebral pedicle or the floor of the acetabulum, this is not always easy and removal may be incomplete.
local recurrence is common, and malignant transformation has been reported
000000000000000000
Tumor like conditions
Bone cysts
Simple bone cyst (solitary or unicamerial bone cyst):
It’s not a tumor but it’s a tumor like condition. (also known as a solitary cyst or unicameral bone cyst)Common in upper humerous, femur and tibia.
Seen in children up to the age of puberty.
Presents as local pain or pathological fracture. Sometimes accidentally discovered on X-ray.
Occurs in the metaphysis and directed towards diaphysis. most commonlyin the proximal humerus or femur.
X-ray shows translucent cystic lesion in the metaphysis and shaft of bone often extending up to the physea plate;with bone widening and cortical expansion and thinning with possible pathological fracture.
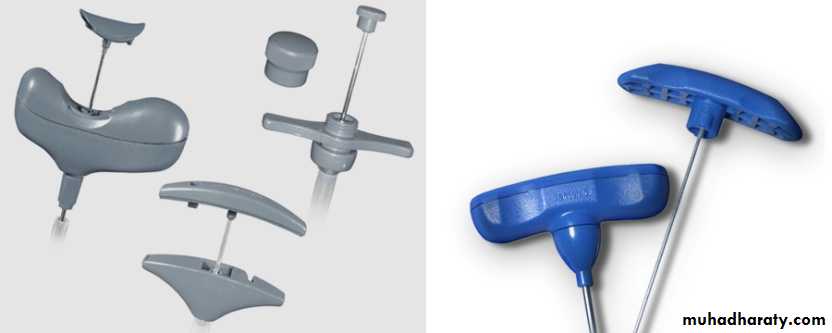
It may show bridges of calcification inside as a result of healing of micro fractures that commonly occurs, by this way it may gradually disappear and heals later in life; sometimes we use this criteria as a method of treatment by frequent aspiration and local steroid injections aiming at induction of such micro fractures that aids healing.
Small cysts treated as above, for larger cysts we do curettage and bone graft.
Aneurismal bone cyst:
Tumor-like cystic lesion forms of multiple cavities full with blood.Mostly seen in spine or eccentrically located in the metaphysis of long bones of young adults.
Clinically With expanding lesions, patients may complain of pain or Occasionally, a large cyst may cause a visible or
palpable swelling of the bone.
X-ray shows well-defined irregular eccentric lucent lesion in the metaphysis that does not reach the articular surface, it may show ballooning, cortical widening and thinning.
Important differential diagnosis is giant cell tumor.
Treatment is by curettage and bone graft or bone cement.
000000000000
Sometimes-malignant tumors
(Intermediate tumors)Giant cell tumor (osteoclastoma):
Pathology:
This tumor contains multinucleated giat cells and large number of stromal cells.
Its soft friable tumor seen in the soft cancellous subarticular bone and never reach the articular surface.
represents 5 per cent of all primary bone tumours, is a lesion of uncertain origin that appears in mature bone, most commonly in the distal femur, proximal tibia, proximal humerus
It’s a tumor of young adults occurs after bone maturity in the epiphysial region.
Its intermediate type of tumor (neither benign nor malignant)
About 1/3 of it remains benign ,
1/3 is locally aggressive,
1/3have distant metastasis.
Clinical features:
Patient aged 20-40.
There is pain or swelling near a joint, 10% presents with pathological fracture.
O/E vague swelling at the bone end and signs of joint irritation.
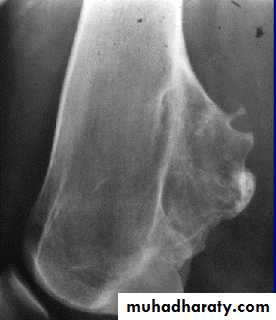
X-ray:
Rarefied area of the bone end reaching just below the articular surface.
Eccentrically situated lesion with bone expansion and ballooning with cortical thinning, sometimes pathological fracture.
There may be calcific trabiculations inside the lesion giving it the commonly known saop-bubble appearance.
Treatment:
For well-defined small and rather benign lesion, we can do curettage and burr-down with bone graft.
Larger more aggressive lesions may need local excision and bone graft or prosthetic replacement.
GCT treated with local excision and bone graft
0000000000000000Differential diagnosisi of radiological appearance of cystic or cyst like bone lesions
oooooooooooooooooooooMalignant bone tumors
Osteosarcoma:Pathology:
Also called osteogenic sarcoma.
It’s a primary malignant bone tumor produces osteoid tissue.
It destroys bone and spread into the surrounding tissues and along the medullay canal.
At the same time it forms abnormal new osteoid in some of its parts, so it destroy bone at the same time it forms new abnormal bone tissue.
It’s easily metastatized via blood and reaches such organs like lung, liver, other bones, …etc.
Clinical features:
It’s seen at the age of 10-20.
It’s a metaphysical lesion usually seen around the knee and in proximal humerus.
50% present with history of trauma.
Pain is a major symptom its usually severe constant and mainly at night.
Sometimes lump is the presenting symptom.
O/E, swollen tender lump without defined margins.
Overlying skin is thin, shiny and warm.
ESR is high.
Imaging:
X-ray shows changes of bone destruction and new bone formation in the metaphysis (rarefaction + sclerosis).
Cortical perforation and soft tissue swelling.
Subperiosteal new bone formation sometimes in the form of Codmen’s triangle and/or sun burst appearance.
CTscan, MRI, and bone scan can show the tumor extent and possible local and distant metastasis.
Pulmonary CTscan can show possible lung metastasis.
Incisional biopsy is essential to establish diagnosis
Treatment of osteosarcoma:
The use of cytotoxic drugs is useful, it increased the 5-year survival of patients up to 50% or even more.Eradication of the primary tumor is essential by radical amputation.
Pre and postoperative cytotoxic drugs are essential especially if there is metastasis, it should go for at least one year.
Irresectable tumors can be treated with combined chemo and radiotherapy.
Chondrosarcoma:
Chondrosarcoma is one of the commonest malignant tumours originating in bone.The highest incidence is in the fourth and fifth decades and men are affected more often than women.
These tumours are slow-growing and are usually present for many months before being discovered.
Patients may complain of a dull ache or a gradually enlarging lump.
Its of two types; primary and secondary.
Primary type:
Its slowly growing form occurs in the flat bones mainly or in the medulla, sometimes mistaken for chondroma.
Rarely seen before the age of forty.
Presents with pain and possible pathological fracture.
X-ray shows destructive medullary tumor with possible flecks of calcification.
Secondary type:
Arises as malignant transformation of a primary chondroma or osteochondroma.
A previously benign tumor and after stop of bone growth starts to increase in size and gets painful.
Sometimes it reaches very large size before being discovered especially in the scapula or pelvis where there is big space for tumor growth.
X-ray shows the original lesion being enlarged and covered with fluffy flecks of irregular calcifications.
Before treatment we investigate the patient with CTscan, MRI and bone scan to establish the diagnosis and see the extent of tumor and its metastasis.
Biopsy is always essential to establish diagnosis.
The tumor metastasis is late, because of that surgical treatment is always useful with wide local excision or amputation,.somtimes we use radithertapy for irresctable tumors.
Fibrosarcoma:
It’s a rare bone tumor.
Usually arises from a previous abnormal lesion like fibrous dysplasia, bone infarct or after irradiation.
Patient usually an adult have pain and swelling rarely pathological fracture.
X-ray may show localized bone destruction, MRI, CTscan can show local extension.
Low-grade tumors can be treated with wide excision and prosthesis.
High-grade tumors needs radical resection or amputation.
Radiotherapy may be useful.
Fibrosarcoma The area of bone destruction in the femoral condyle has no special
distinguishing features.Ewing’s tumor:
Malignant tumor of vascular endothelium of bone marrow.Occur at the diaphysis of long bones commonly tibia, fibula and clavicle.
It causes severe type of periosteal new bone formation.
It’s readily metastasize through blood (sometimes its regarded as blood disease).
Usual age is 10-20.
Pain and swelling is the common presenting features, sometimes there is fever and local lymph node enlargement.
There is tender ill-defined mass which is warm.
Differential diagnosis is acute osteomylitis.
X-ray shows diaphysial lesion with bone destruction and multiple layers of periosteal new bone formation.New bone formation may extend along the shaft and appears as fusiform layers of bone around the lesion – the socalled‘onion-peel’ effect or Onion-Skin appearance. is predominantly in the mid-diaphysis.
Often the tumour extends into the surrounding soft tissues, with radiating streaks of ossification and reactive periosteal bone, these features (the ‘sunray’ appearance and Codman’s triangles) are usually associated with osteosarcoma, but they are just as common in Ewing’s sarcoma.
Bone scan shows increased activity.
Biopsy is highly indicated.
Treatment includes all methods of radical surgery, chemotherapy and radiotherapy.
0000000000000000
Multiple myelomaIt’s a tumor of plasma cells of red marrow wherever it’s found, mainly long bones, pelvis and spine.
Usually its multiple but rarely its localized solitary myeloma lesion and called plasmacytoma.
Clinical features:
Patient aged 45-65, presents with pain or pathological fracture.
Pain is constant, severe mainly backache and possible root pain.
Anemia, cehexia and chronic nephritis with general ill health all may present.
ESR always very high.
Main cause of death is renal failure.
X-ray:
Commonest feature is generalized osteopenia, (osteopenia and high ESR in patient above 50 is MM until proved otherwise).
Sometimes multiple punched-off small defects in more than one bone.
Vertebrae can show compression fractures.
Investigations:
CBP+ESR.
Urine for Benz Jones protein.
Serum&urine protein electrophoresis.
Bone marrow aspirate and biopsy.
Treatment:
Radiotherapy and chemotherapy controls the abnormal growths, relieve pain and pressure and improves survival.
Pathological fractures treated with curettage & internal fixation +/- bone cement.
Spinal lesions and cord or root pressure needs decompression +/- bone fusion.
Multiple Myeloma The characteristic x-ray features are bone rarefaction, vertebral compression fractures, expanding lesions (typically in the ribs and pelvis) and punched-out areas in the skull and the long bones.
Metastatic bone tumors
Its more common than all primary malignant bone tumors together.
The skeleton is one of the commonest sites of secondary cancer; in patients over 50 years bone metastases are seen more frequently than all primary malignant bone tumours together.The commonest source is carcinoma of the breast; carcinomas of the prostate, kidney, lung, thyroid, bladder and gastrointestinal tract.
In about 10 per cent of cases no primary tumour is found.
The commonest sites for bone metastases are the vertebrae, pelvis, the proximal half of the femur and the humerus.
They destroy and replace bone, they grow rapidly and there is no bone reaction.
Clinical features:
Age usually 50-70 years.
Commonly there is pain of long bones spine or pelvis.
Sometimes present as pathological fractures.
We may look for the primary source with clinical exam, imaging, laboratory tests and all possible means.
If primary source is not obvious no need for further effort to find it because it does not affect final treatment a lot.
X-ray:
Pure destructive osteolytic lesion usually in the diaphysis gives a Moth-Eaten appearance without any bone reaction.
Generalized osteopenia is common.
Chest X-ray or pulmonary CTscan can exclude lung metastasis.
Generalized bone scan can show other skeletal lesions.
Metastatic tumours This patient presented with pain in the right upper thigh. X-ray showed what appeared to be a single metastasis in the upper third of the femur. However, the radioisotope scan revealed many deposits in other parts of the skeleton.
Patients over 60 with vertebral compression fractures may simply be very osteoporotic, but they
should always be investigated for metastatic bone disease and myelomatosis.
Treatment:
As metastasis already occurred the prognosis is always poor and treatment is usually palliative.Patient may need radio+/- chemotherapy plus support of the general condition.
A pathological fracture needs curettage, internal fixation +/-bone cement.
Spinal lesions and cord or root compression may need decompression +/- bone fusion.