1
4th stage
جراحة
Lec-2
د.زيد
16/12/2015
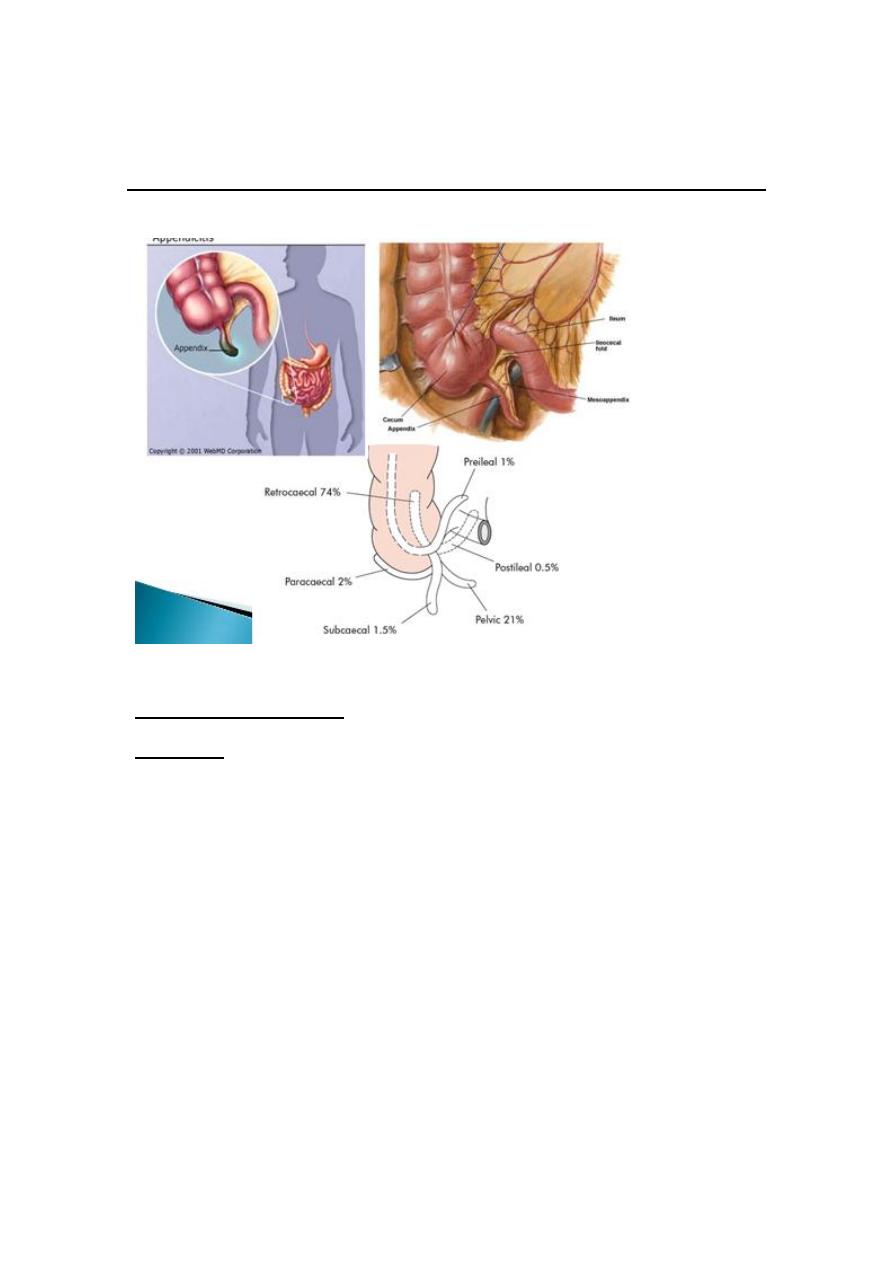
APPENDIX
ACUTE APPENDICITIS
Incidence:
-
rare in infants, increasingly common in childhood and early adult
life, peak incidence in the teens and early 20s.
-
before puberty males = females.
-
In teenagers and young adults the male–female ratio 3:2
-
Thereafter, the greater incidence in males declines.
2
Aetiology
No definite cause
1-Decreased dietary fibre and increased consumption of refined
carbohydrates (low fiber diet)
2-Bacterial proliferation within the appendix,
no single organism is responsible(mixed growth of aerobic and
anaerobic organisms ).
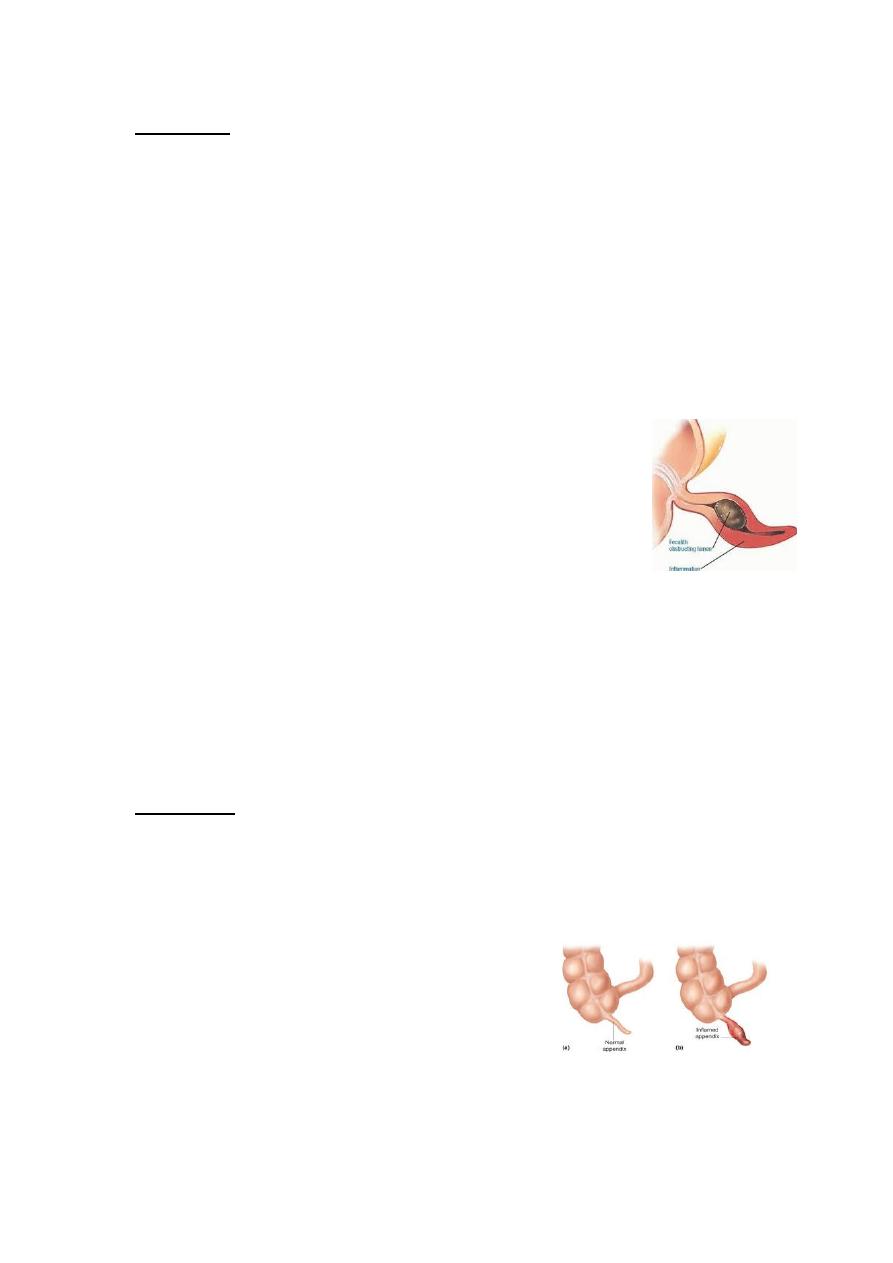
3- Obstruction of the appendix lumen
- Lymphoid hyperplasia
- faecolith (composed of inspissated faecal material,
calcium phosphates, bacteria and epithelial debris
- stricture
- foreign body(rare)
- tumour, particularly carcinoma of the caecum(middle age and
elderly)
- Intestinal parasites, particularly Oxyuris vermicularis
Pathology
-
Lymphoid hyperplasia narrows the lumen luminal obstruction.
-
Continued mucus secretion and inflammatory exudation
increase intraluminal pressure obstructing lymphatic
drainageOedema
- Mucosal ulceration
- Bacterial translocation to the submucosa.

3
Resolution may occur (spontaneously/antibiotic therapy).
or
Condition progresses,more distension venous
obstruction & wall ischaemia bacterial invasion through
the muscularis propria and submucosa, producing acute appendicitis.
Ischaemic necrosis gangrenous appendicitisfree bacterial
contamination of the peritoneal cavity(peritonitis).
Alternatively, the greater omentum and loops of small bowel
become adherent to the inflamed appendix, walling off the spread
of peritoneal contamination, and resulting in a phlegmonous
mass or paracaecal abscess.
Rarely, appendiceal inflammation resolves, leaving a distended
mucus-filled organ termed a ‘mucocoele’ of the appendix .
Diffuse peritonitis is the great threat of acute appendicitis, it ocuurs as a
result of:
-
free migration of bacteria through an ischaemic appendicular wall
-
frank perforation of a gangrenous appendix
-
delayed perforation of an appendix abscess.
4
Factors that promote this process include:
- extremes of age
- immunosuppression
- diabetes mellitus
- faecolith obstruction of the appendix lumen
- free-lying pelvic appendix
- previous abdominal surgery
In these situations, a rapidly deteriorating clinical course is accompanied
by signs of diffuse peritonitis and systemic sepsis syndrome.
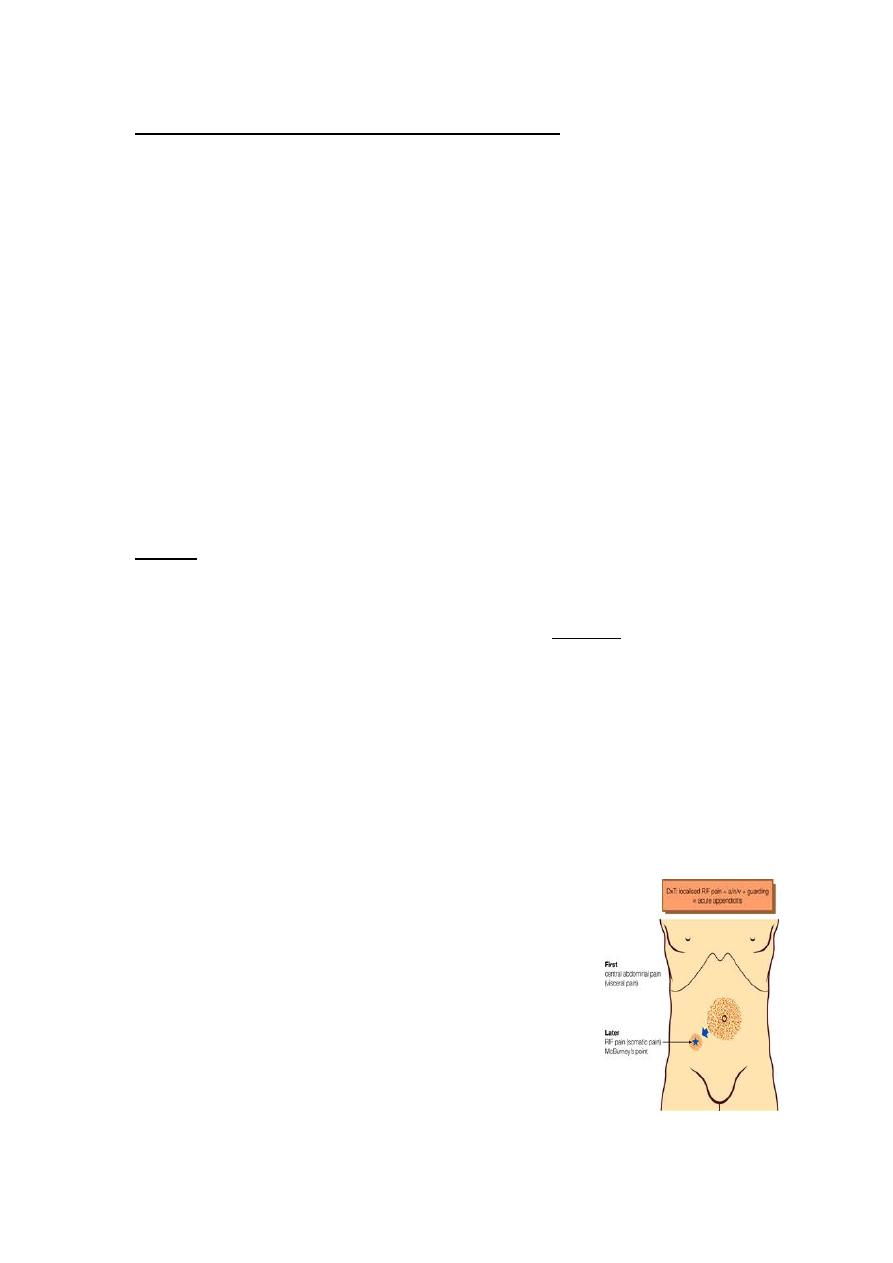
Clinical diagnosis
History
PAIN
-poorly localised, colicky abdominal pain(midgut visceral discomfort in
response to appendiceal inflammation and obstruction).
-The pain in periumbilical region.
- Central abdominal pain + anorexia, nausea and usually one or two
episodes of vomiting that follow the onset of pain.
With progressive inflammation of the appendix:
Shifting of pain: from central abdominal pain to right iliac fossa(irritation
of RIF parietal peritoneum) visceral to somatic pain
which is :
- more intense
- constant
- localised to right iliac fossa
Typically, coughing or sudden movement
exacerbates the right iliac fossa pain.
5
ANOREXIA
-constant clinical feature, particularly in children.
Family history
1/3 of children with appendicitis have a first-degree relative with a
similar history .
One half of acute appendicitis classic visceral–somatic sequence of
pain .
Signs
Temperature and pulse rate:
- After 6 hours, slight pyrexia (37.2–37.7°C) with a corresponding
increase in the pulse rate to 80 or 90 is usual.
-Changes of greater magnitude may indicate complications.
- Unwell patient with low-grade pyrexia
- Inspection of the abdomen limitation of respiratory movement in
the lower abdomen.
- localised abdominal tenderness maximum at McBurney’s point.
- Muscle guarding
-
Rebound tenderness
Asking the patient to cough or gentle percussion over
the site of maximum tenderness will elicit rebound
tenderness .
- Pointing sign: The patient is asked to point to where the
pain began and where it moved .

6
Two clinical syndromes of acute appendicitis:
1- acute catarrhal (non-obstructive) appendicitis
2- acute obstructive appendicitis:
-more acute course(abrupt)
-generalised abdominal pain from the start.
- Temperature normal
- vomiting common.
7
2-Pelvic appendicitis
- More common in children
- Early diarrhoea (inflamed appendix in contact with the rectum).
- Complete absence of abdominal rigidity
- Tenderness over McBurney’s point is also lacking.
- Deep tenderness can be made out just above and to the right of the
symphysis pubis.
- Rectal examination reveals tenderness in the rectovesical pouch or
the pouch of Douglas, especially on the right
side.
- +ve psoas and obturator signs.
- Frequency of micturition (inflamed appendix in contact with the
bladder).
3-Postileal appendicitis
The inflamed appendix lies behind the terminal
Ileum(difficult to diagnose)
- Pain may not shift
- Diarrhea is a feature
- Marked retching
- Tenderness, if any, is ill defined, although it may be
present immediately to the right of the umbilicus.
8
Special features, according to age
Infants
- Rare in infants under 36 months of age.
- The patient is unable to give a history. Diagnosis is often delayed.
- Higher incidence of perforation and postoperative morbidity than
older children.
- Diffuse peritonitis can develop rapidly because of the underdeveloped
greater omentum.
Children
- Vomiting is more common.
- complete aversion to food.
The elderly
- Gangrene and perforation occur much more frequently .
- The abdominal clinical picture is not obvious even in the presence of
gangrenous appendicitis (lax abdominal walls or obesity)
- Clinical picture may simulate subacute intestinal obstruction.
- Higher mortality
(coincident medical conditions plus the previous factors)
The obese
- Obesity can obscure and diminish all the local signs of acute
appendicitis.
- Midline abdominal incision
(Delay in diagnosis + technical difficulty of operating in the obese)
- Laparoscopy is particularly useful in the obese.
9
Pregnancy
Appendicitis is the most common extrauterine acute abdominal
condition in pregnancy.
- Delay in presentation (early non-specific symptoms are often
attributed to the pregnancy).
- The physiologic leukocytosis of pregnancy (high as 16,000 cells/mm3).
Obstetric teaching has been that the caecum and appendix are
progressively pushed to the right upper quadrant of the abdomen as
pregnancy develops during the second and
third trimesters.
- Pain in the right lower quadrant of the abdomen remains the cardinal
feature of appendicitis in pregnancy.
- Fetal loss occurs in 3–5 per cent of cases, increasing to 20 per cent if
perforation is found at operation.
Differential diagnosis
Children
1- Acute gastroenteritis and mesenteric lymphadenitis:
the pain is diffuse, and tenderness is not as sharply localized and
cervical lymph nodes may be enlarged.
2- Meckel’s diverticulitis:
signs may be central or left sided.
history of antecedent abdominal pain or intermittent lower
gastrointestinal bleeding.
3- Intussusception:
Appendicitis is uncommon before the age of two years, whereas the
median age for intussusception is 18 months.
A mass may be palpable in the right lower quadrant,
11
Adults
1- Terminal ileitis
- a doughy mass of inflamed ileum may be felt.
- history of abdominal cramping, weight loss and diarrhoea.
The ileitis may be non-specific, due to Crohn’s disease or Yersinia
infection.
- serum antibody titres are diagnostic, and treatment with
intravenous tetracycline is appropriate.
2- Ureteric colic:
Urinalysis should always be performed, and the presence of red cells
supine abdominal radiograph. Renal ultrasound or intravenous urogram
is diagnostic.
11
3- Right-sided acute pyelonephritis
increased frequency of micturition.
tenderness confined to the loin, fever (temperature 39°C) and possibly
rigors and pyuria.
4- perforated peptic ulcer
the duodenal contents pass along the paracolic gutter to the right iliac
fossa.
- history of dyspepsia
- very sudden onset of pain that starts in the epigastrium and passes
down the right paracolic gutter.
- rigidity is usually greater in the right hypochondrium.
- rigidity and tenderness in the right iliac fossa
- erect chest radiograph gas under the diaphragm in 70 %.
- abdominal (CT) examination in difficult cases.
5- Testicular torsion (teenage or young adult male)
Pain can be referred to the right iliac fossa, and shyness on the part
of the patient may lead the unwary to suspect appendicitis unless the
scrotum is examined in all cases.
6-Acute pancreatitis
should be considered in the differential diagnosis of all
adults suspected of having acute appendicitis and,
when appropriate, should be excluded by serum or
urinary amylase measurement.
12
7- Rectus sheath haematoma
-
relatively rare
-
acute pain and localised tenderness in the RIF
-
after an episode of strenuous physical exercise.
-
Localised pain without gastrointestinal upset is the rule.
Occasionally, in an elderly patient, particularly one taking
anticoagulant therapy, a rectus sheath haematoma may present
as a mass and tenderness in the right iliac fossa after minor
trauma.
Adult female
pelvic disease in women of childbearing age most often mimics acute
appendicitis.
A careful gynaecological history should be taken in all women with
suspected appendicitis, concentrating on:
- menstrual cycle
- vaginal discharge
- possible pregnancy .
The most common diagnostic mimics are
pelvic inflammatory disease (PID), Mittelschmerz, torsion or
haemorrhage of an ovarian cyst and ectopic pregnancy.
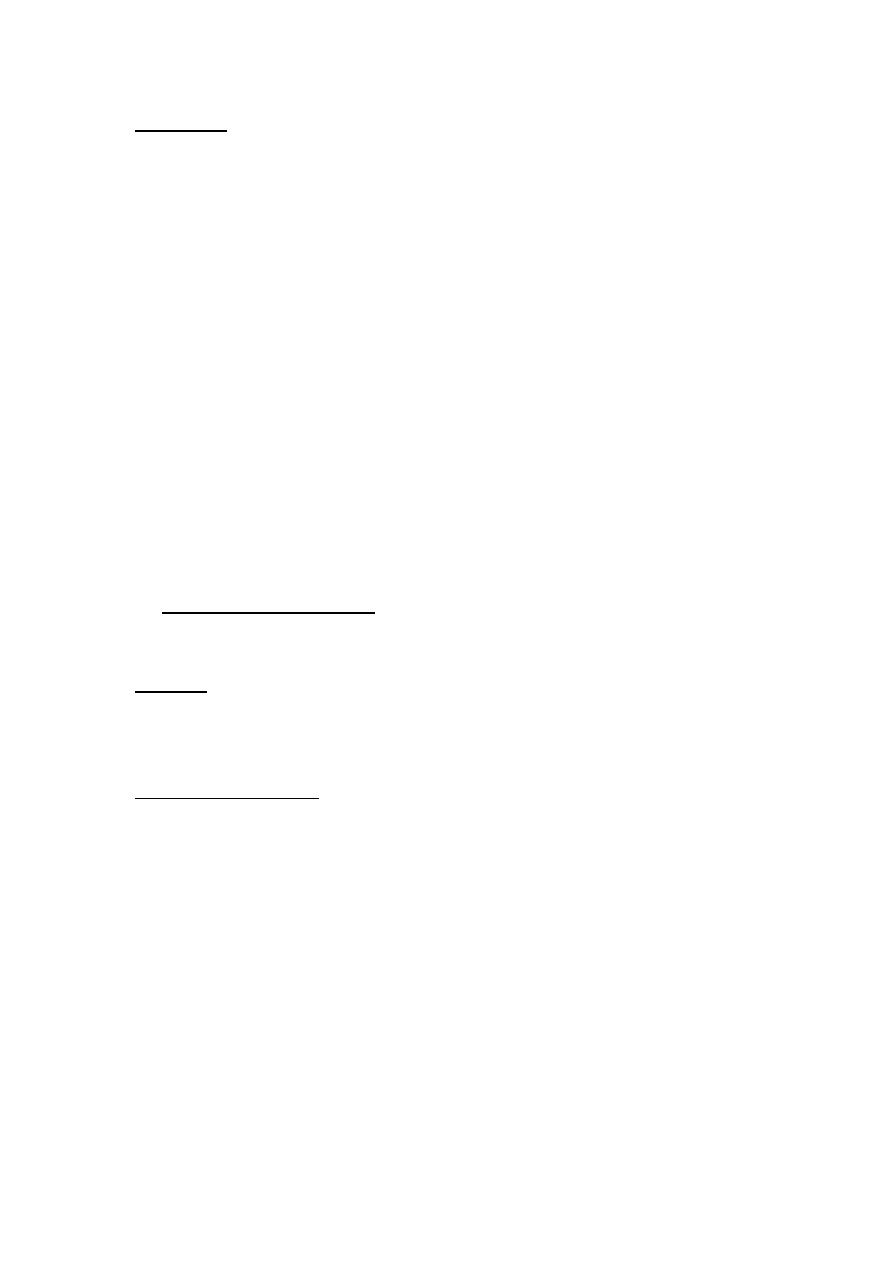
1-Pelvic inflammatory disease
(salpingitis, endometritis and tubo-ovarian sepsis)
- The pain is lower than in appendicitis and is bilateral.
- history of vaginal discharge, dysmenorrhoea and dysurea .
- vaginal examination adnexal and cervical tenderness .
- High vaginal swab & culture Chlamydia trachomatis and Neisseria
gonorrhoeae.
- gynaecologist opinion should be obtained.
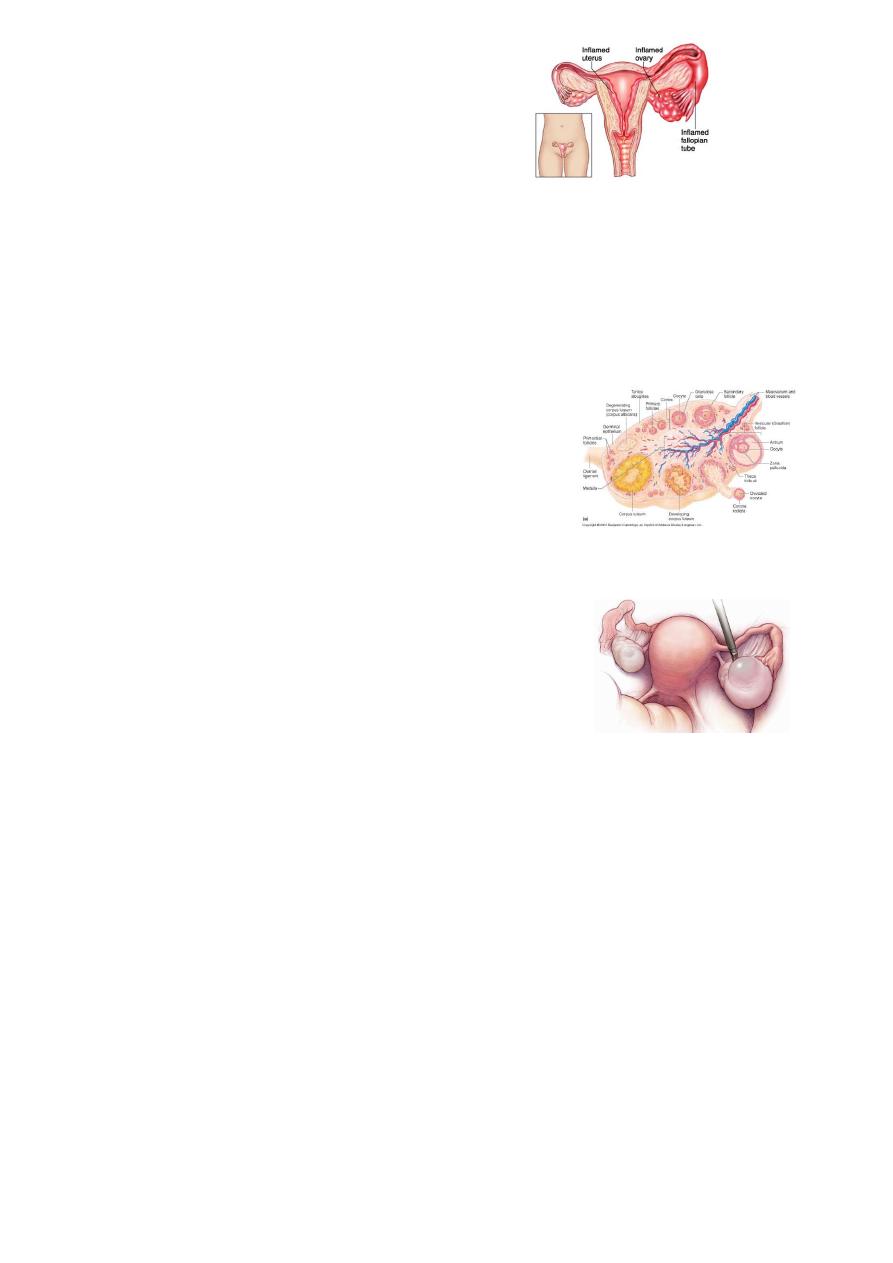
13
- Transvaginal ultrasound
- diagnostic laparoscopy
2- Mittelschmerz
Midcycle rupture of a follicular cyst with bleeding produces lower
abdominal and pelvic pain, typically midcycle.
- No systemic upset
-
Pregnancy test is negative
-
Symptoms usually subside within hours.
-
Occasionally, diagnostic laparoscopy is
required. Retrograde menstruation may
cause similar symptoms.
3- Torsion/haemorrhage of an ovarian cyst
(difficult differential diagnosis)
pelvic ultrasound and a gynaecological opinion
should be sought.
If encountered at operation untwisting of the
involved adnexa and ovarian cystectomy should be performed.
14
4- Ectopic pregnancy
- Ectopic preg. signs of haemoperitoneum
-
right-sided tubal abortion or
right-sided unruptured tubal pregnancy.
Right-sided unruptured tubal pregnancy :
- pain commences on the right side and stays there.
- pain is severe.
- history of a missed menstrual period
- Signs of intraperitoneal bleeding with referred pain in the
shoulder.
- cervical excitation test positive
- urinary pregnancy test may be positive.
- Pelvic ultrasonography.
15
Elderly
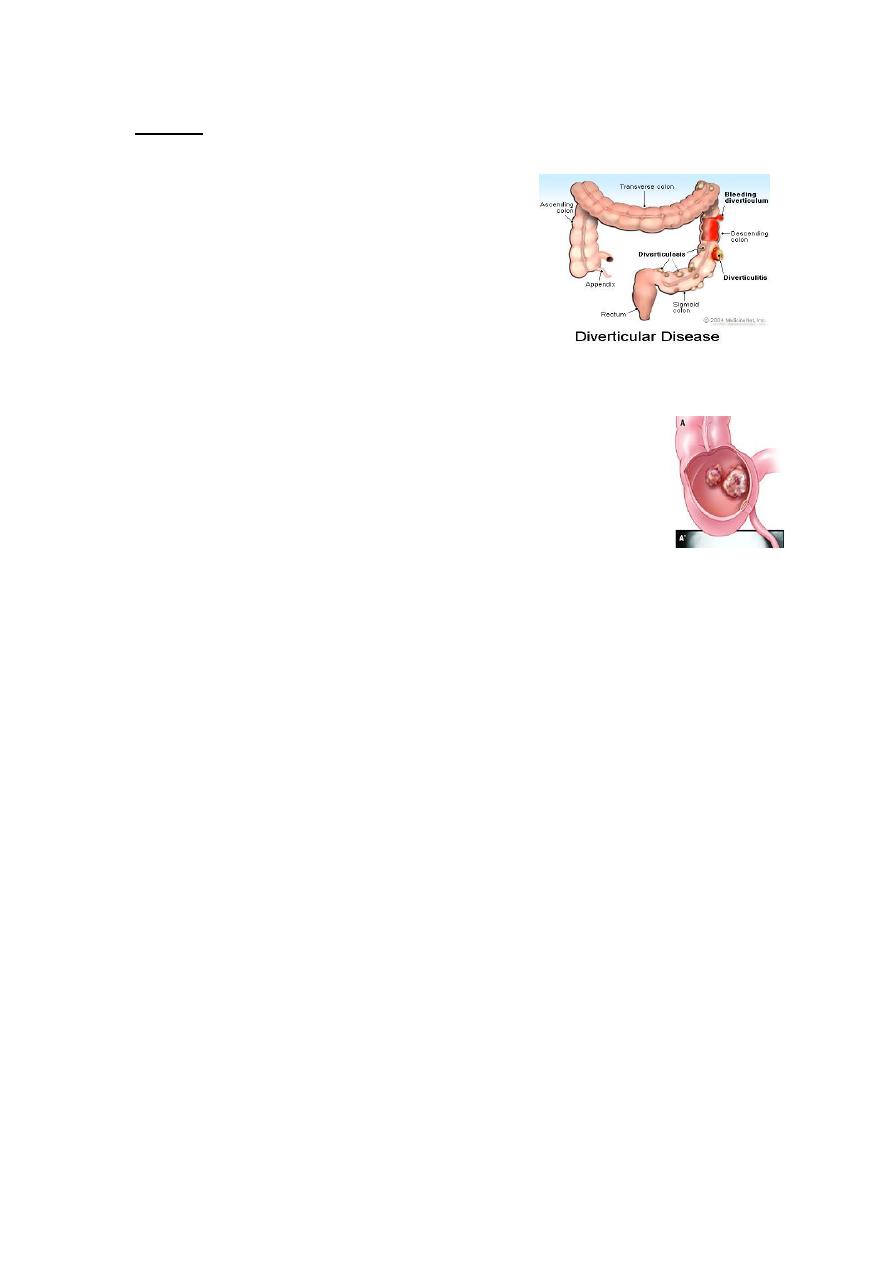
1- Diverticulitis
Abdominal CT scanning is particularly useful
and should be considered in the
management of all patients over the age of
60 years.
Right-sided diverticulitis is unusual and may
be clinically indistinguishable from
appendicitis.
2-Intestinal obstruction
In elderly, occasionally, it may be difficult to differentiate IO
from acute appendicitis
3-Carcinoma of the caecum
-Carcinoma of the caecum when obstructed or locally perforated, may
mimic or cause obstructive appendicitis in adults.
-history of antecedent discomfort, altered bowel habit or unexplained
anaemia.
- mass may be palpable and an abdominal CT scan diagnostic.

16
Rare differential diagnoses
1-Preherpetic pain of the right 10th and 11th dorsal nerves.
- no shift of pain
- marked hyperaesthesia.
- no intestinal upset, no rigidity.
The herpetic eruption may be delayed for 3–8 hours.
2-Tabetic crises.
3-Spinal conditions include tuberculosis of the spine, metastatic
carcinoma, osteoporotic vertebral collapse and multiple myeloma.
4-porphyria and diabetes mellitus
5-Typhlitis or leukaemic ileocaecal syndrome
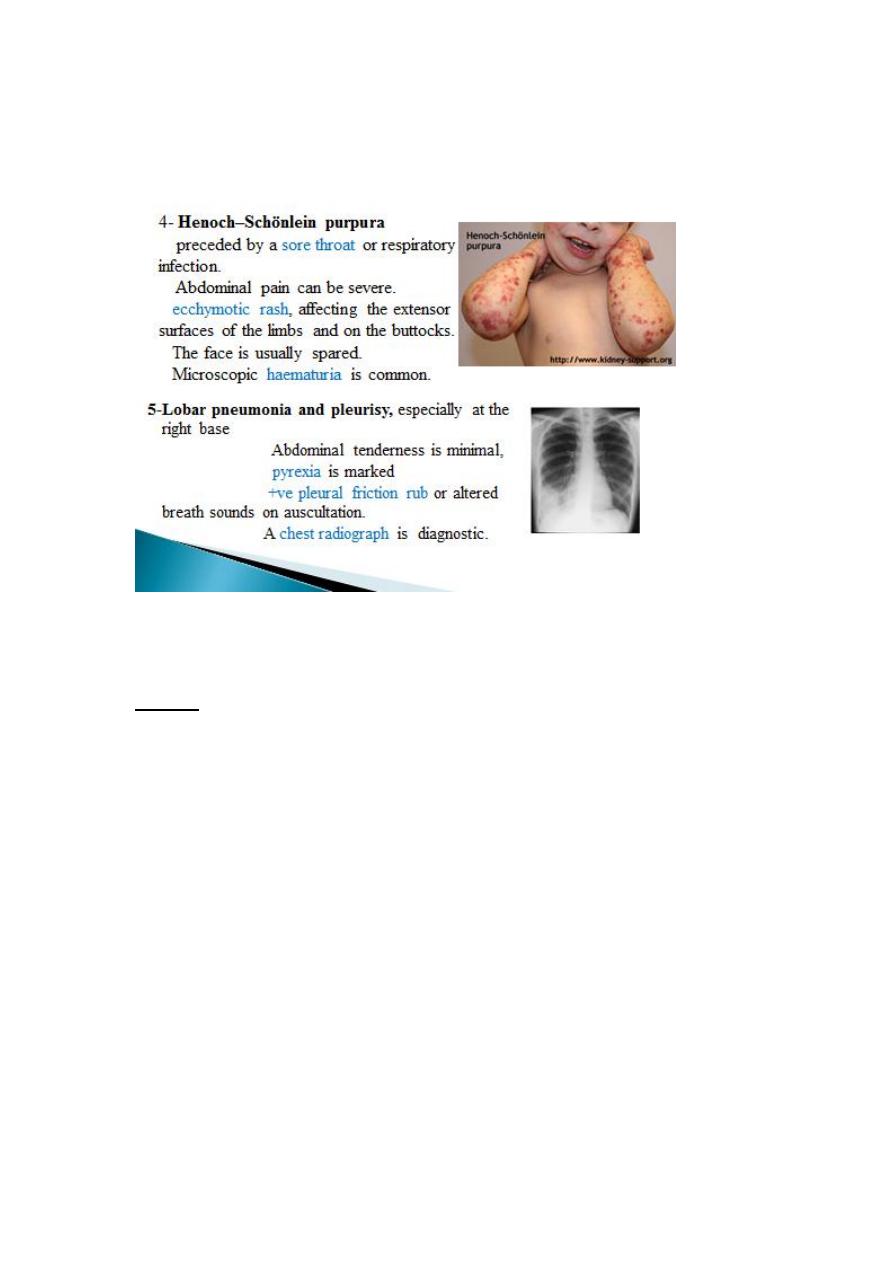
Investigation
The diagnosis of acute appendicitis is essentially clinical
Routine
Full blood count WBC > 10,000
Urinalysis hematuria/ pyuria due to irritation of nearby ureter/
urinary bladder
Selective
Pregnancy test
Urea and electrolytes
Supine abdominal radiograph
Ultrasound of the abdomen/pelvis
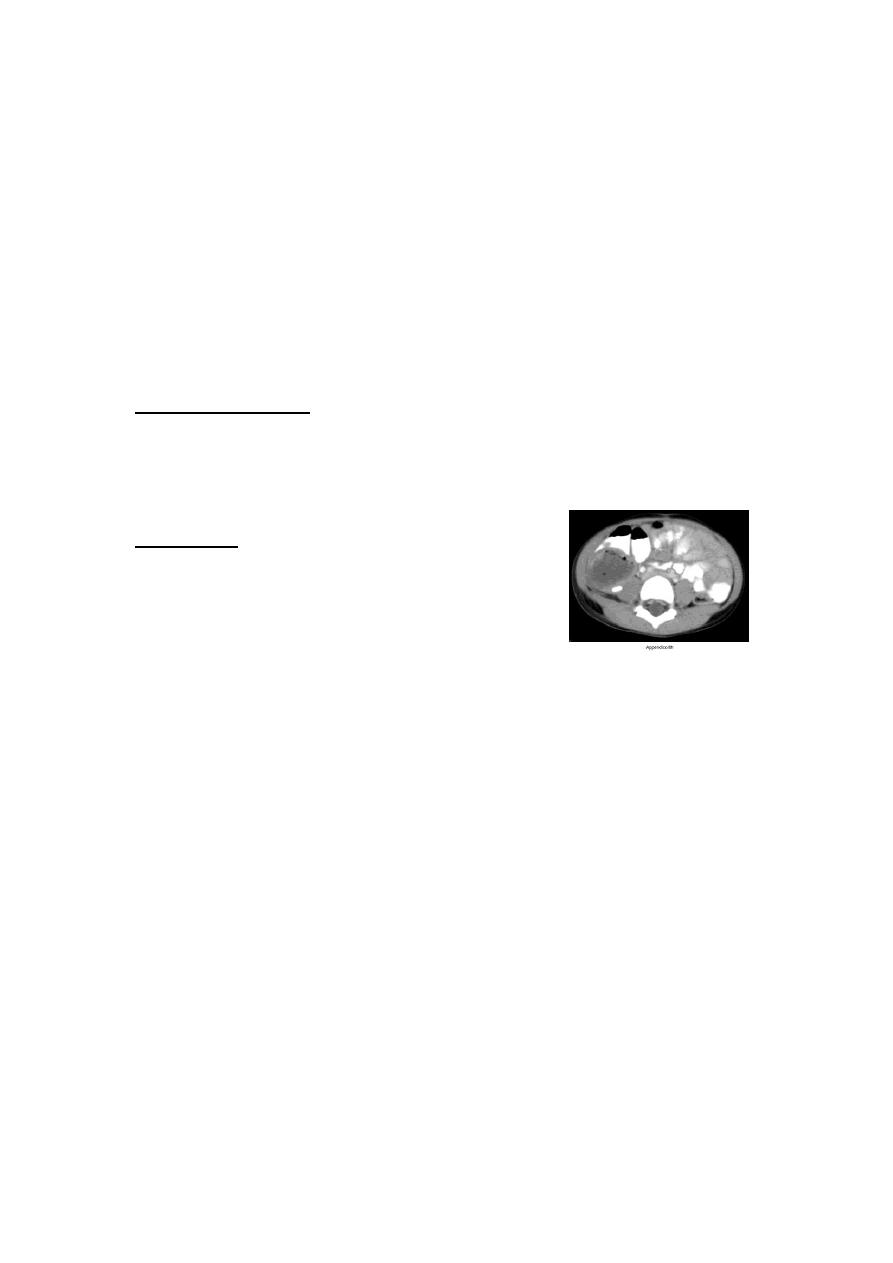
Contrast-enhanced abdomen and pelvic computed tomography scan

17
Alvarado score:
A score of 7 or more is strongly predictive of acute appendicitis
-
Equivocal score (5–6)abdominal ultrasound or contrast-
enhanced CT examination .
Abdominal ultrasound is useful in:
- children and thin adults
- if gynaecological pathology is suspected, with a diagnostic
accuracy >90 %.
Contrast-enhanced CT scan is most useful in:
- diagnostic uncertainty+older patients
- acute diverticulitis, intestinal obstruction and neoplasm
suspected.
18
Treatment
The traditional treatment for acute appendicitis is appendicectomy.
Some research the conservative management in non-obstructive
appendicitis including :
1- bowel rest(NPO)
2- intravenous antibiotics, usually metranidazole and third-generation
cephalosporin
conservative management 80-90% successful, 15 recurrence within
one year.
patients over the age of 40 should be followed up to ensure there is no
underlying malignancy
Appendicectomy:
-
no unnecessary delay
-
short period of intensive preoperative preparation:
1- NPO
2- Intravenous fluids
(catheterisation is needed only in the very ill)
3- IV antibiotics
In the absence of purulant peritonitis give single preoperative dose of
antibiotics .
When peritonitis is suspected, therapeutic intravenous antibiotics to
cover Gramnegative bacilli, as well as anaerobic cocci, should be given.
19
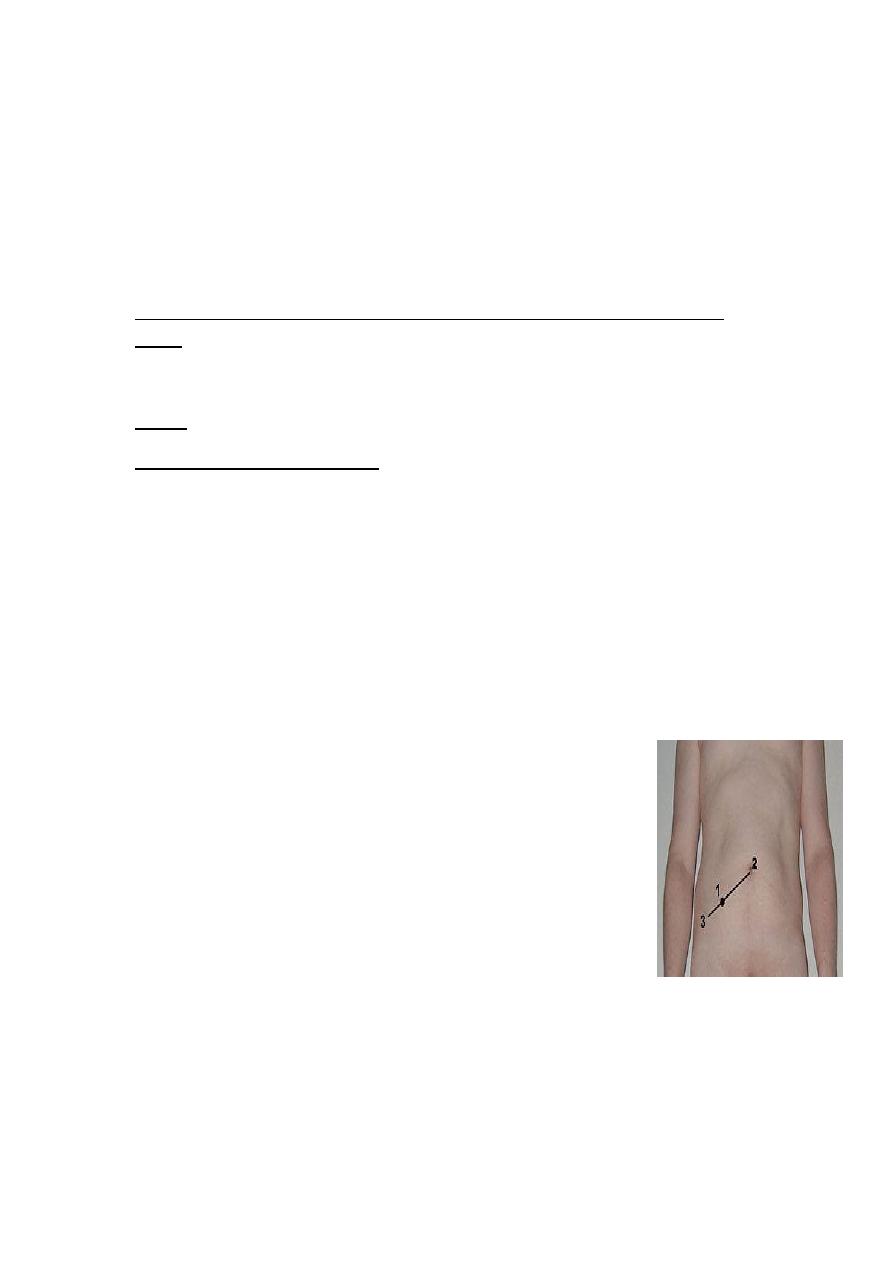
Appendicectomy
- general anaesthetic
-
patient supine on the operating table.
-
When a laparoscopic technique is to be used, the bladder must be
empty
(ensure that the patient has voided before leaving the ward).
palpated for a mass prior to preparing the entire abdomen with an
antiseptic solution.(mass conservative)
Draping of the abdomen
Incisions used:
1- The gridiron incision(most common)
2- Rutherford Morison incision(muscle cutting)
3- Transverse skin crease (Lanz) incision
4- lower midline abdominal incision( doubtful diagnosis)
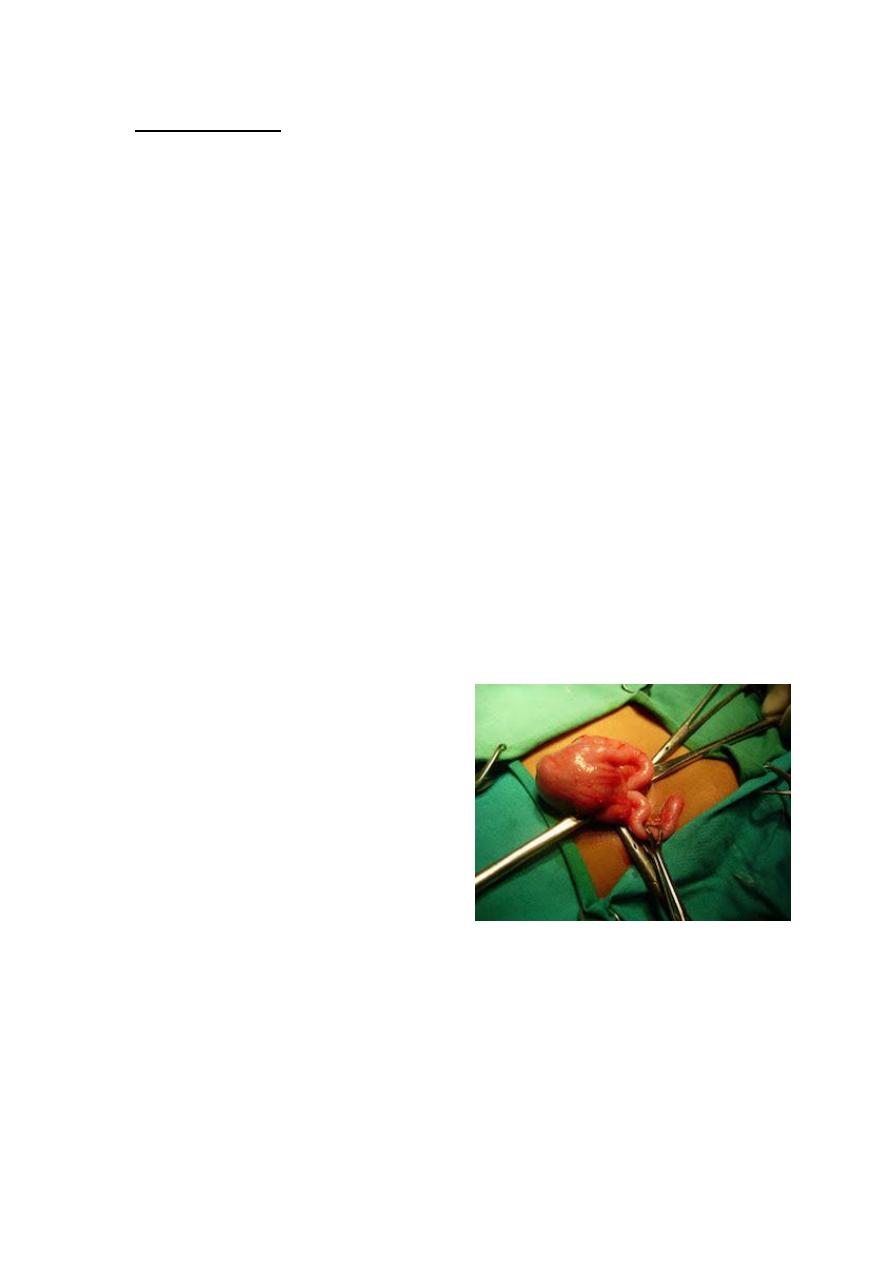
1-The caecum is identified by the
presence of taeniae coli and is
withdrawn.
2- Appendix may be felt at the base
of the caecum.
3- Inflammatory adhesions must be
gently broken with a finger, the
appendix delivered into the wound.
4- Mesoappendix devided between ligature, the base of appendix ligated
and divided.
5- Purse-string to invaginates the stump of the appendix(?????)
21
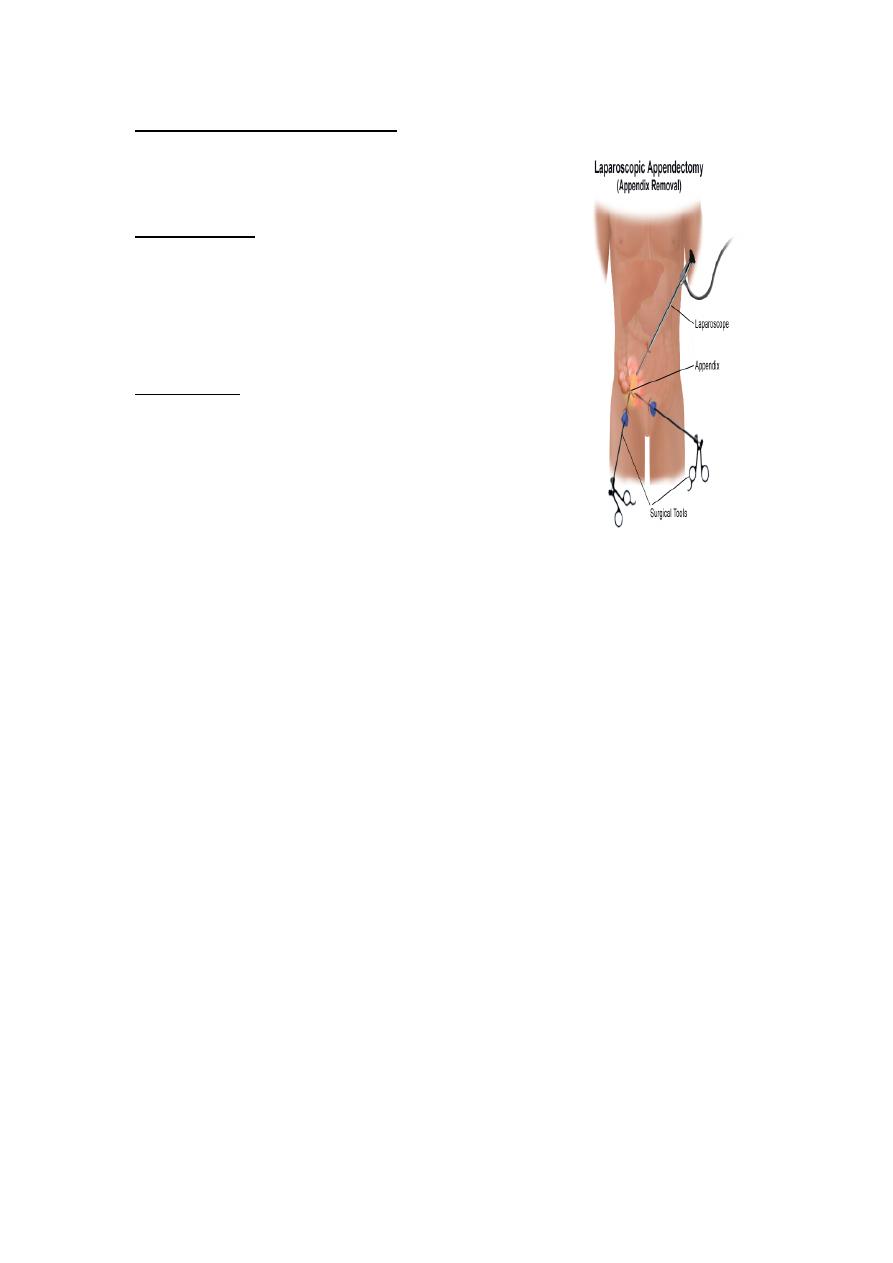
Laparoscopic appendicectomy
Laparoscopy is diagnostic tool(esp. in female)
and therapeutic.
Used more in:
Female (child bearing age)
in obese patients
early pregnancy
Advantages:
less postoperative pain
Early discharge from hospital
Early return to daily activities
NOTES
Natural Orifice Transluminal Endoscopic Surgery
Problems encountered during appendicectomy
1-A normal appendix is found
- exclude other possible diagnoses, particularly terminal ileitis, Meckel’s
diverticulitis and tubal or ovarian causes in women.
- remove the appendix (avoid future diagnostic difficulties)
2-The appendix cannot be found.
The caecum should be mobilised, and the taeniae coli should be traced
to their confluence on the caecum before the diagnosis of ‘absent
appendix’ is made.
3-An appendicular tumour is found.
Small tumours (under 2.0 cm in diameter) can be removed by
appendicectomy.
Larger: right hemicolectomy
21
4- An appendix abscess is found and the appendix cannot be removed
easily.
Preoperatively diagnosed abscessPercutaneous drainage of the
abscess and intravenous antibiotic .
At operationdraine the abscess +intravenous antibiotics.
Frankly necrotic appendix(very rarely) caecectomy or partial right
hemicolectomy .
Appendix abscess
Failure of resolution of an appendix mass or continued spiking pyrexia
usually indicates that there is pus within the phlegmonous appendix
mass.
Treatment :
Ultrasound or abdominal CT scan percutaneous
drain.
If unsuccessful laparotomy through a midline
incision is indicated.
Pelvic abscess
- an occasional complication of acute appendicitis.
-
Presented with spiking pyrexia several days after appendicitis
-
Pelvic pressure or discomfort
-
loose stool or tenesmus is common.
-
Rectal examination mass in the pelvis.
Pelvic ultrasound or CT scan confirm.
Treatment:
- Radiologically guided percutaneous drainage
- Transrectal drainage under general anaesthetic.
22
Postoperative complications
1- Wound infection
most common postoperative complication
usually presents with pain and erythema of the wound on
the 4th or 5th postoperative day.
Treatment: wound drainage + antibiotics.
2- Intra-abdominal abscess
presented with spiking fever, malaise and anorexia developing 5–7
days after operation .
Sites of collection:
Interloop, paracolic, pelvic and subphrenic
Abdominal ultrasonography and CT scanning diagnostic and allow
percutaneous drainage.
Laparotomy in intra-abdominal sepsis without localised collection.
3- slipped ligature
internal bleeding, hypotension, tacchycardia reoperate
4- Ileus
Ileus persisting for more than 4 or 5 days + fevercontinuing intra-
abdominal sepsis investigation.
5- Respiratory
- rare
- Adequate postoperative analgesia and physiotherapy reduce the
incidence.
6- Venous thrombosis and embolism
- rare after appendicectomy
- more in elderly and in women taking the oral contraceptive pill and
prophylactic measures should be considered.
23
7- Portal pyaemia (pylephlebitis)
-
rare
-
complication of gangrenous appendicitis
-
high fever, rigors and jaundice.
-
caused by septicaemia in the portal venous system intrahepatic
abscesses (multiple).
Treatment: systemic antibiotics + percutaneous drainage of hepatic
abscesses.
screen for underlying thrombophilia
8- Faecal fistula
- Rare
- leakage from appendicular stump.
- More in appendicectomy in Crohn’s disease.
Treatment: Conservative management with low-residue enteral
nutrition.
9- Adhesive intestinal obstruction
This is the most common late complication of appendicectomy.
Management of an appendix mass
Conservative Ochsner–Sherren regimen;
A nonoperative programme but to be prepared to operate should
clinical deterioration occur . This includes:

24
Careful recording of the patient’s condition
1- Temperature and pulse rate should be recorded 4-hourly
2- Fluid balance record
3- The abdomen regularly reexamined.
4- The extent of the mass should be made (mark the limits of the mass
on the abdominal wall using a skin pencil)
5- A contrast-enhanced CT examination of the abdomen
6- Antibiotic
7- An abscess, if present, should be drained radiologically.
Criteria for stopping conservative treatment of an appendix
mass
_ A rising pulse rate
_ Increasing or spreading abdominal pain
_ Increasing size of the mass
Clinical deterioration or evidence of peritonitis is an indication for early
laparotomy.
If the mass resolve, Patients over the age of 40 should have colonoscopy
and follow-up imaging to ensure resolution and exclude appendicular or
colonic malignancy.
Recurrent acute appendicitis
- not uncommon
- attacks vary in intensity and may occur every few months.
-
majority of cases ends in severe acute appendicitis.
The appendix in these cases shows fibrosis indicative of previous
inflammation.
25
Neoplasms of the appendix
1-Carcinoid tumours
- arise in argentaffin tissue (Kulchitsky cells of the crypts of Lieberkühn)
-
most common in the vermiform appendix.
- appendix removed because of symptoms of subacute or recurrent
appendicitis.
Treatment:
- Appendectomy .
- Right hemicolectomy is indicated if:
-
caecal wall involvement .
-
2 or more in size.
-
Involved lymph nodes.
2- Goblet cell carcinoid tumour
3- Primary adenocarcinoma of the appendix
extremely rare, presented as appendicitistreated by right
hemicolectomy
Mucinous cystadenoma
- A mucin-secreting adenoma of the appendix
-
rupture into the peritoneal cavity , seeding it with mucussecreting
cells.
-
delayed presentation with gross abdominal distension as a result
of pseudomyxoma peritoneii, which may mimic ascites .
Treatment
radical resection of all involved parietal peritoneal
surfaces and aggressive intraperitoneal chemotherapy.
